Abstract
Introduction
This study prospectively examined whether HIV leads to elevated risk for intimate partner violence (IPV) for women, and how this risk varies depending on HIV status disclosure to a partner.
Methods
We ran a series of logistic regression models using data from 1092 pregnant and postpartum women enrolled in an RCT in Durban, South Africa, The first model assessed whether baseline HIV-status predicted 14-week postpartum physical IPV, controlling for baseline physical IPV, disclosure to partner, demographic and study covariates. Model 2 added the interaction between HIV status and disclosure.
Results
HIV was not associated with 14-week physical IPV in the main effects model adjusted odds ratio (AOR) 1.34, 95% CI: .88 - 2.05). However, there was a statistically significant positive interaction between HIV and disclosure, (AOR 0.22, 95% CI: .05-.96). Among women who disclosed their HIV status, HIV was not significantly associated with 14-week IPV (AOR 1.12; 95% CI 0.71-1.89). However, among women who had not disclosed, the odds of reporting IPV at 14 weeks was 5.15 times higher for HIV-positive women as compared to HIV-negative women (95% CI: 1.25-21.00).
Discussion
While we established that HIV does not increase incidence of IPV for all HIV-positive women, we found an elevated risk of IPV among the HIV-positive women who chose not to disclose their status to their partner. Non-disclosure is likely a marker for other problematic aspects of the relationship, and counselors should either find alternative safe options for disclosure or support women’s decisions not to disclose.
INTRODUCTION
Numerous studies have documented an association between intimate partner violence (IPV) victimization and HIV infection among women across a number of different settings (for reviews see, (Kouyoumdjian, Findlay, Schwandt, & Calzavara, 2013; Y. Li et al., 2014). The predominant theoretical perspective driving this research posits that IPV leads to HIV infection either directly, through forced sex with an infected parther, and/or indirectly by, for example, limiting women’s ability to negotiate safe sex (Jewkes, Dunkle, Nduna, & Shai, 2010; S. Maman, Campbell, Sweat, & Gielen, 2000). However, scholars have also acknowledged the possibility for a reverse causal pathway wherein HIV infection may lead to increased risk of experiencing IPV (Campbell et al., 2008; Durevall & Lindskog, 2015; Hatcher et al., 2014). In particular, qualitative research suggests that women who are diagnosed with HIV may experience violence and other negative social outcomes as a result of sharing their HIV positive status with their partner (Gielen, O’Campo, Faden, & Eke, 1997; Hatcher et al., 2014; Medley, Garcia-Moreno, McGill, & Maman, 2004; Mulrenan, Colombini, Howard, Kikuvi, & Mayhew, 2015; Siemieniuk et al., 2013). Further, women who are diagnosed with HIV may experience financial, emotional, physiological stress, depression, and reduced social support that may contribute to relationship conflict and increase vulnerability to IPV (Hand, Phillips, & Dudgeon, 2006). If diagnosis with HIV is a risk factor for IPV, it suggests the importance of developing IPV-prevention programs for HIV-infected women. Yet, to date, nearly all of the studies examining relations between IPV and HIV have been cross-sectional (Kouyoumdjian, Findlay, et al., 2013; Y. Li et al., 2014), precluding the ability to establish temporality of associations, and the few longitudinal studies that have been conducted have examined whether IPV predicts HIV rather than vice-versa (e.g., (Jewkes et al., 2010), (Kouyoumdjian, Calzavara, et al., 2013). A prospective study from Kenya reported that among HIV-positive pregnant women in their cohort the odds of experiencing physical, psychological or financial abuse from a partner two weeks after diagnosis was significantly higher than among HIV-negative women, when controlling for disclosure. (Kiarie et al., 2006). The authors in this study did not examine the interactive effect of disclosure and diagnosis on women’s experiences with IPV.
The current study was designed to address the gaps in the literature using a sample of pregnant South African women. Two primary aims guided the study. The first aim examined the main effects of HIV status, diagnosed during pregnancy on physical IPV victimization at 14 weeks postpartum. We hypothesized that HIV-positive women would be at increased risk for postpartum IPV as compared to HIV-negative women. The second aim investigated the possibility that HIV-disclosure moderated the effect of HIV-status on IPV. Previous research suggests two competing hypotheses concerning the direction of this interaction. On the one hand, as noted above, findings from some qualitative research suggest that disclosure of HIV-positive status may trigger violence. This suggests that HIV may be more strongly related to IPV among women who disclose their status than among women who do not disclose their status. That is, among women who disclose their HIV-status to their partner, disclosure of an HIV-positive diagnosis may be more likely to spark conflict and violence than disclosure of an HIV-negative diagnosis; among women who do not disclose their HIV-status, HIV-infection may be unrelated to IPV.
On the other hand, qualitative research also suggests that women may choose not to disclose that they are HIV-positive to their partner precisely because they fear negative reactions and abuse. Non-disclosure of HIV-positive status may thus be a marker indicating involvement in an unhealthy violence-prone relationship. This line of reasoning suggests that HIV may be more strongly related to IPV among women who do not disclose than among women who do disclose their status. That is, among women who do not disclose, HIV-status may be positively related to IPV because HIV-positive non-disclosers are more likely to be in unhealthy relationships than HIV-negative non-disclosers. In contrast, among women who do disclose, HIV may be unrelated to IPV; HIV-positive women who choose to disclose their HIV-status rightfully anticipate that disclosure will not precipitate violence and thus are at no greater risk for IPV than HIV-negative women who disclose their status.
Methods
Study design and sample
Data for the proposed analyses were collected as part of a randomized control trial, the South Africa HIV/AIDS Antenatal Posttest Support (SAHAPS) study, which was designed to evaluate the efficacy of an enhanced counseling and support intervention for HIV-positive and HIV-negative women during pregnancy and the postpartum period. Participants were women who attended antenatal care at a public primary health clinic in Umlazi township in the province of KwaZulu Natal (KZN). KZN has the highest antenatal prevalence of HIV infection and highest infant mortality in South Africa (Coovadia, Jewkes, Barron, Sanders, & McIntyre, 2009; Karim et al., 2011). Pregnant women who presented to the clinic for their first antenatal visit were eligible for screening. Inclusion criteria were: (1) at least 18 years old, (2) had never tested for HIV or had tested negative for HIV at least 3 months prior to recruitment, (3) attending first antenatal visit when HIV testing was offered; (4) had a primary intimate partner for at least the past 6 months, (5) planned to live in Durban for at least the next year, (6) planned to bring their infant to the clinic for immunization visits, (7) able to communicate in English or Zulu, and; (8) did not need care for a high risk pregnancy since such patients needed to be referred to a tertiary public health facility. Women who consented to participate completed a Computer Assisted Personal Interview (CAPI) in Zulu or in English and were tested for HIV and STIs at baseline (1st antenatal visit) and again at 14 weeks postpartum. Women were not aware of their HIV diagnosis prior to completion of their baseline survey. The interviews were conducted by locally trained data collectors who were fluent in English and Zulu. We screened 3333 women, and determined that 1636 of these women met our eligibility criteria. The most common reasons women were not eligible included that they had previously tested positive for HIV, and they were not planning on being in Durban for the next year. Of the 1636, who met the eligibility criteria, 136 declined to participate and 20 were not tested for HIV as part of our study. We enrolled 1480 women in the trial. Following completion of the baseline interview 733, women were randomized to receive the enhanced counseling intervention (intervention) and 747 were randomized to receive the standard counseling and testing (control).
Among the 1480 women who were enrolled in the study at baseline and eligible for follow-up; 79% (1147) of these women were retained at the 14 week postpartum follow-up. Data for this study come from 1092 women who completed interviews at both at baseline and 14 week follow-up and were not missing data on key variables at follow up. At baseline, participants were, on average, 25.57 years old (range 18-45); 36.90% were HIV-positive; 30.40% had experienced physical IPV in their current relationship prior to or during the current pregnancy, 63.19% reported having had at least one prior pregnancy, and 79.30% reported the current pregnancy was unintended. More details on the study sample and protocol, including intervention and HIV/STI testing procedures are included in prior publications (S. Maman, Moodley, Groves, & Smith, 2007; S. Maman et al., 2014). The research was approved by the institutional review board at the University of North Carolina and the University of KwaZuluNatal.
Measures
Physical IPV
A modified version of the World Health Organization (WHO) Violence Against Women instrument was used to measure physical IPV (Garcia-Moreno, Jansen, Ellsberg, Heise, & Watts, 2006). This instrument has six questions on physical violence that a woman has experienced with her current partner and has been used in numerous South African studies (e.g., (Jewkes et al., 2010); (K. L. Dunkle et al., 2004). A sample item is, “how many times has your current partner pushed or shoved you?” In this study, the stem of the questions was modified to reflect the specific reference period the participants were being asked about (before or during pregnancy, from delivery to 14 weeks postpartum). Each item had five response categories that ranged from never to more than ten times. Responses to the six items were summed and then, due to skew in the distribution of the IPV variable at follow-up, dichotomized to create two binary variables: (1) Baseline Physical IPV assessed the presence or absence of any physical IPV perpetrated by the woman’s partner prior to and/or during pregnancy and; (2) Follow-up Physical IPV assessed the presence of absence of any physical IPV by the woman’s partner between delivery and 14-weeks postpartum.
HIV-status and disclosure
HIV status and HIV disclosure to partner were dichotomized to create binary variables for analysis.
Demographic and study covariates
Participants reported their age, education, and length of their relationship at the baseline visit, which occurred during their first antenatal care visit. Following previous research in South Africa, we created a measure of socioeconomic status by using principal components analysis to derive a linear index from a series of asset ownership indicators and then categorized participants as belong to the poorest 40%, middle 40% or wealthiest 20% on the asset index scale (BERG & Louw, 2004; Blaauw & Penn-Kekana, 2003; Filmer & Pritchett, 2001; Gyekye & Akinboade, 2003). Pregnancy characteristics included gestational age at first antenatal visit (no. of weeks), parity (never, 1 time, 2 or more times) and whether the current pregnancy was intended (yes/no). We also controlled for the amount of time between the completion of the baseline survey and the completion of the 14 week follow up survey (no. of weeks). Sensitivity analysis indicated there were no significant differences in findings across study arms, so study allocation arm was not included as a covariate.
Statistical Analysis
Analyses for the current manuscript proceeded in several phases. First, we conducted bivariate analysis to examine differences in baseline and follow-up IPV, HIV− disclosure, and covariates by HIV status. Next a series of logistic regression models were run to examine study hypotheses regarding the prospective association between HIV and follow-up physical IPV. The first model (main effects) assessed whether baseline HIV-status predicted physical IPV at follow-up, controlling for baseline physical IPV, disclosure to partner, as well as all of the demographic and study covariates described above. Model 2 (full) added the interaction between HIV-status and disclosure. All statistical analyses were performed using SAS software, version 9.3(SAS Institute Inc., 2011).
RESULTS
Descriptive results
HIV positive women in the sample were older on average (26.41 years vs 25.07, p<.0001), of lower socioeconomic status (42.68% vs. 34.40%, p=0.006), and less likely to have completed high school (49.63% vs. 36.43% p<.0001). HIV-positive women had also been in their relationships with their primary partners for a shorter amount of time (3.80 years vs 4.76 years, p<.0001). The HIV-negative women were more likely to be pregnant for the first time (40.64% vs. 30.27%, p=.001), and more likely to have disclosed to their partner (94.63% vs. 76.43%, p<.0001). There were no significant differences in reports of physical IPV at baseline (32.01% vs. 29.46%) and 14 weeks postpartum (14.14% vs 11.47%) among the HIV-positive as compared to the HIV-negative women in the sample. See Table 1.
Table 1. Demographic information on sample at baseline (n=1092).
| HIV+ | HIV− | X2 or t | p-value | |
|---|---|---|---|---|
|
| ||||
| % or mean (SD) |
% or mean (SD) |
|||
|
| ||||
| Age | 26.41 (5.16) | 25.07 (5.56) | −3.92 | <.0001 |
|
| ||||
| SES (ref=high) | ||||
| Low | 42.68 | 34.40 | 7.45 | 0.0060 |
| High | 37.97 | 41.07 | 1.02 | 0.3100 |
|
| ||||
| Education (ref=HS graduate) | ||||
| ≤ Grade 7 | 6.95 | 5.08 | 1.63 | 0.2000 |
| Grades 8-11 (ref) | 49.63 | 36.43 | 18.27 | <.0001 |
|
| ||||
| Length of relationship | 3.80 (3.58) | 4.76 (4.35) | 3.93 | <.0001 |
|
| ||||
| Gestational age (weeks) | 23.43 (5.85) | 24.25 (5.97) | 2.19 | 0.0280 |
|
| ||||
| Pregnancy intended | 19.35 | 21.48 | 0.7 | 0.4000 |
|
| ||||
| Previous pregnancy (ref=2) | ||||
| 0 | 30.27 | 40.64 | 11.75 | 0.0006 |
| 1 | 42.68 | 33.09 | 10.07 | 0.0020 |
|
| ||||
| Disclosed HIV status to partner | 76.43 | 94.63 | 79.29 | <.0001 |
|
| ||||
| Physical IPV | ||||
| Baseline | 32.01 | 29.46 | 0.78 | 0.3800 |
| 14-week postpartum | 14.14 | 11.47 | 1.67 | 0.2000 |
Multivariate results
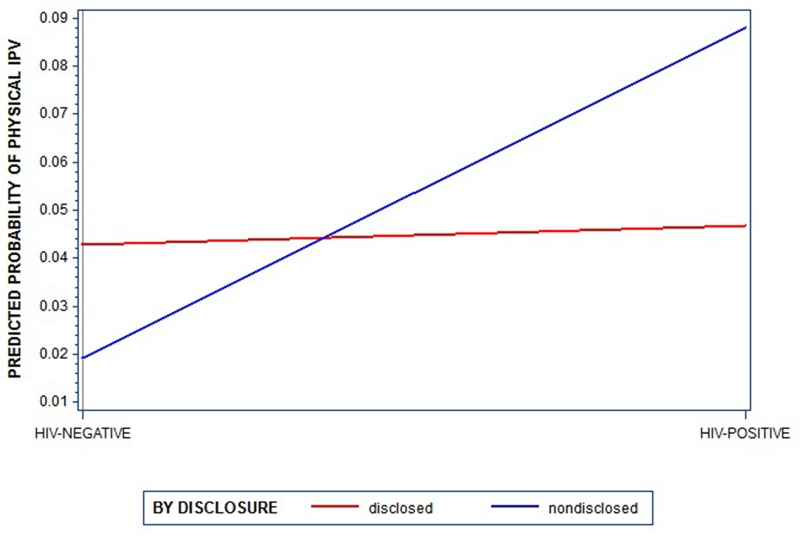
Contrary to expectations, HIV was not associated with physical IPV at follow-up in the main effects model (AOR 1.34, 95% CI: .88 - 2.05). However, there was a statistically significant positive interaction between HIV and disclosure, (AOR 0.22, 95% CI: .05-.96). Following standard recommendations, post-hoc analyses were conducted to determine the simple slopes for the effects of HIV status on physical IPV within each level of the moderator (disclosure). Among women who disclosed their HIV status, HIV was not significantly associated with IPV at follow-up (AOR 1.12; 95% CI 0.71-1.89). However, among women who had not disclosed, the odds of reporting IPV at 14 weeks was 5.15 times higher for HIV positive women as compared to HIV-negative women (95% CI: 1.25-21.20). These findings are depicted graphically in Figure 1 which presents the model-implied predicted probability of IPV at 14 weeks postpartum for HIV positive and HIV negative women who did and did not disclose their HIV-status.
Figure 1.
Interaction of HIV status and disclosure on 14 week IPV
DISCUSSION
We found that HIV diagnosis during pregnancy prospectively predicted postpartum IPV among women who reported that they had not disclosed their HIV status to their partner at the time of follow up. Specifically, HIV-positive women who had not disclosed were approximately five times more likely to report experiencing IPV at 14 weeks postpartum when compared to HIV-negative women who had not disclosed. This finding is consistent with the notion that non-disclosure of HIV-positive status may be a marker indicating involvement in an unhealthy relationship with a violence-prone partner.
On the other hand, HIV was not predictive of IPV among women who did disclose their HIV status; HIV-positive women in our study who disclosed their status to their partners were not at increased risk for IPV when compared to HIV-negative women who disclosed. Prior studies, primarily qualitative, have documented some IPV and other negative social outcomes among HIV-infected women who disclose their status to their partners, however our findings do not support these prior studies (Gielen, McDonnell, Burke, & O’Campo, 2000; Gielen et al., 1997; Murray et al., 2006; Strebel et al., 2006). Another prospective study examined pregnant women’s experiences with IPV following diagnosis in Kenya (Kiarie et al., 2006). Investigators found a greater odds of reporting IPV among HIV-positive women as compared to HIV-negative women, however, the investigators did not examine whether the association between diagnosis and IPV differed by disclosure. They controlled for disclosure in their analysis, making it difficult to compare their results to our findings. In addition, the follow-up assessment in the Kenya study occurred 2 weeks after diagnosis, and not during the postpartum period for women, and the measurement of violence in this study included psychological and financial abuse, further limiting the comparability to our findings.
There is a larger body of research that has explored how IPV may increase women’s risk for HIV. Evidence from these studies have been mixed. Among the many cross-sectional studies, more than half from sub-Saharan Africa reported null findings, while others reported significant associations(Dude, 2011; Kristin L Dunkle et al., 2004; Ketchen, Armistead, & Cook, 2009; Suzanne Maman et al., 2002; Mattson, Settergren, & Sabatier, 2009; Ntaganira, Muula, Siziya, Stoskopf, & Rudatsikira, 2009; Pettifor, Measham, Rees, & Padian, 2004; Sa & Larsen, 2008; Van der Straten et al., 1998). There have been four longitudinal studies from sub-Saharan Africa and two of these studies found that there was a significant association between IPV and incident HIV, and two did not find this association (Jewkes et al., 2010; Kouyoumdjian, Calzavara, et al., 2013; Were et al., 2011; Zablotska et al., 2009). Results of a meta-analysis found significant associations in cohort and cross-sectional studies, but not in case-control studies (Ying Li et al., 2014). Our findings suggest that researchers need to consider not just whether the association exists, but whether this relationship matters more for certain groups of vulnerable women.
Our findings suggest that as part of the HIV post-test counseling session, counselors should assess women’s disclosure plans. For HIV-positive women who feel comfortable disclosing, counselors should encourage them to do so since it is likely that they will not be at any greater risk for IPV than HIV-negative women who disclose. It is certainly possible that some HIV-positive women who disclose their status will experience negative reactions from partners, and counselors should be prepared to provide support and resources to these women.
Almost a quarter (23.6%) of HIV-infected women in our sample had not shared their HIV test result with their partner by 14-weeks postpartum. This rate of non-disclosure is within the range of non-disclosure, 14% to 83.3%, that was reported, in a review of studies among women (Medley et al., 2004). The fact that there continues to be a substantial number of HIV-positive women who opt not to share their diagnosis with their partners, and these women are at greater risk for experiencing IPV, has important implications for practice. Health care providers should be aware that non-disclosure of HIV status is a marker that may indicate involvement in an unhealthy violence-prone relationship. Providers should assess the potential for violence and refer women to counseling or other support services. More generally, the principle of do no harm must continue to inform our counseling and support for women. While disclosure of HIV status is an important public health goal to increase awareness of risk for HIV, this has to be pursued carefully in the case of women who may be at risk for IPV. Before we address disclosure, it is important to address women’s exposure to violence in relationships, and offer women services and support to address the violence. If we focus on disclosure, without assessing risk of violence, we run the risk of putting these women in physical danger if we push women to disclose when it is not safe to do so. We need to explore and test alternative ways to support safe disclosure for women, and accept the fact that disclosure may not always be in the best interest of women and therefore should not be supported until women can insure their own safety. Couples HIV counseling and testing is one approach that may help facilitate the safe disclosure of HIV status. In the couples counseling approach, a counselor is present with the couple as they share their HIV results with each other. The counselor is trained to facilitate the disclosure and mediate conflict between partners. In this model, counselors can also facilitate access to other care and support resources for the couple, enhancing the support that they have to cope with the diagnosis. Couples counseling may not be appropriate in relationships where women are exposed to severe violence from a partner(O’Leary, 2008).
Our prospective design and the enrollment of both HIV-positive and HIV-negative women in our trial are major strengths of this study that enabled us to assess the temporal relationship between HIV diagnosis and IPV victimization, and to assess whether this relationship varied for those who did or did not disclose their HIV status. Other strengths of the trial include the large sample size, and our retention of nearly 80% of women in the trial, which is high in this urban, highly mobile setting. The study was not without limitations. As is the case with all studies that rely on self-reported data, there is the possibility that women may have misreported their experiences with IPV, and whether they disclosed their status to their partner. We included text that was designed to normalize the reporting of IPV for women prior to asking them to report their own experiences, which may have helped women feel more comfortable reporting these sensitive experiences.
CONCLUSION
These findings provide new insight on the relationship between HIV status, disclosure of HIV status to partners and subsequent experiences with IPV. The results from this cohort of women indicate that HIV-positive women who disclose their status are not significantly more likely to experience IPV than HIV-negative women who disclose and therefore that HIV-positive women who feel prepared to disclose should be supported in this decision during HIV counseling and testing. The fact that nearly a quarter of all HIV-positive women reported that they had not shared their HIV test results with their partner, and that these women are at greater risk for experiencing IPV postpartum remains a concern. Among those women who had not disclosed, HIV-positive women were significantly more likely to report violence in the postpartum period than HIV-negative women. For women who do not feel comfortable disclosing their HIV status to their partners, counselors should be prepared to assess their risk for violence and provide services and support to them to address this risk. Disclosure may not be in these women’s best interest and should not be encouraged until women can insure their safety.
Table 2.
Associations between HIV variables, Baseline IPV, sociodemographic characteristics, pregnancy variables, and physical IPV Postpartum
| Model 1 | Model 2 | |||
|---|---|---|---|---|
|
| ||||
| OR | 95% CI | OR | 95% CI | |
|
| ||||
| HIV status | 1.34 | .88-2.05 | 5.15* | 1.25-21.20 |
|
| ||||
| HIV disclosure to partner | .77 | .43-1.37 | .77 | .43-1.37 |
|
| ||||
| Baseline IPV | 5.53*** | 3.71- 8.24 |
5.70*** | 3.82-8.52 |
|
| ||||
| HIV status*disclosure | -- | -- | ||
|
| ||||
| Age | 0.91** | .86-.96 | .91** | .86-.96 |
|
| ||||
| SES (ref=high) | ||||
| Low | .80 | .48-1.36 | .79 | .47-1.34 |
| Middle | .79 | .48-1.30 | .78 | .47-1.28 |
|
| ||||
| Education (ref=HS graduate) |
||||
| ≤ Grade 7 | 1.83 | .75-4.47 | 2.06 | .85-5.04 |
| Grades 8-11 | 1.36 | .90-2.06 | 1.38 | .91-2.09 |
|
| ||||
| Length of relationship | 1.06* | 1.00- 1.13 |
1.07* | 1.00-1.13 |
|
| ||||
| Gestational age | 1.04^ | .99-1.08 | 1.04^ | .99-1.08 |
|
| ||||
| Pregnancy intention | 1.05 | .64-1.74 | 1.09 | .66-1.80 |
|
| ||||
| Previous pregnancy (ref=2) |
||||
| 0 | .91 | .46-1.82 | .97 | .49-1.93 |
| 1 | 1.63^ | .92-2.91 | 1.77^ | .99-3.16 |
All models controlled for the number of week elapsed between baseline and 14-weeks follow up assessment.
p<.10;
p<.05;
p<.01;
p<.001
ACKNOLWEDGEMENTS
We thank the women who partnered with us in conducting this research, and all study participants for their contributions. We also thank study staff in South Africa for their work and dedication.
Source of support: This research was sponsored by the U.S. National Institute of Mental Health (R01HD050134). We also received funds from the Open Society Institute and Elton John Foundation (20020472/20030878).
Footnotes
Conflicts of interest: There are no conflicts of interest to declare.
This study is registered with ClinicalTrials.gov, number NCT01683461
REFERENCES
- BERG S, Louw M. Changing Patterns of South African Income Distribution: Towards Time Series Estimates of Distribution and Poverty1. South African journal of economics. 2004;72(3):546–572. [Google Scholar]
- Blaauw D, Penn-Kekana L. Socio-economic inequalities and maternal health in South Africa; Paper presented at the Exposé présenté à la 22e conference on priorities in perinatal care in South Africa.2003. [Google Scholar]
- Campbell JC, Baty ML, Ghandour RM, Stockman JK, Francisco L, Wagman J. The intersection of intimate partner violence against women and HIV/AIDS: a review. Int J Inj Contr Saf Promot. 2008;15(4):221–231. doi: 10.1080/17457300802423224. doi:10.1080/17457300802423224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coovadia H, Jewkes R, Barron P, Sanders D, McIntyre D. The health and health system of South Africa: historical roots of current public health challenges. Lancet. 2009;374(9692):817–834. doi: 10.1016/S0140-6736(09)60951-X. doi:10.1016/s0140-6736(09)60951-x. [DOI] [PubMed] [Google Scholar]
- Dude AM. Spousal intimate partner violence is associated with HIV and Other STIs among married Rwandan women. AIDS and Behavior. 2011;15(1):142–152. doi: 10.1007/s10461-009-9526-1. [DOI] [PubMed] [Google Scholar]
- Dunkle KL, Jewkes RK, Brown HC, Gray GE, McIntryre JA, Harlow SD. Gender-based violence, relationship power, and risk of HIV infection in women attending antenatal clinics in South Africa. The lancet. 2004;363(9419):1415–1421. doi: 10.1016/S0140-6736(04)16098-4. [DOI] [PubMed] [Google Scholar]
- Dunkle KL, Jewkes RK, Brown HC, Yoshihama M, Gray GE, McIntyre JA, Harlow SD. Prevalence and patterns of gender-based violence and revictimization among women attending antenatal clinics in Soweto, South Africa. Am J Epidemiol. 2004;160(3):230–239. doi: 10.1093/aje/kwh194. doi:10.1093/aje/kwh194. [DOI] [PubMed] [Google Scholar]
- Durevall D, Lindskog A. Intimate partner violence and HIV in ten sub-Saharan African countries: what do the Demographic and Health Surveys tell us? Lancet Glob Health. 2015;3(1):e34–43. doi: 10.1016/S2214-109X(14)70343-2. doi:10.1016/s2214-109x(14)70343-2. [DOI] [PubMed] [Google Scholar]
- Filmer D, Pritchett LH. Estimating wealth effects without expenditure data--or tears: an application to educational enrollments in states of India. Demography. 2001;38(1):115–132. doi: 10.1353/dem.2001.0003. [DOI] [PubMed] [Google Scholar]
- Garcia-Moreno C, Jansen HA, Ellsberg M, Heise L, Watts CH. Prevalence of intimate partner violence: findings from the WHO multi-country study on women’s health and domestic violence. Lancet. 2006;368(9543):1260–1269. doi: 10.1186/1471-2458-11-109. doi:10.1016/s0140-6736(06)69523-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gielen AC, McDonnell KA, Burke JG, O’Campo P. Women’s lives after an HIV-positive diagnosis: disclosure and violence. Matern Child Health J. 2000;4(2):111–120. doi: 10.1023/a:1009522321240. [DOI] [PubMed] [Google Scholar]
- Gielen AC, O’Campo P, Faden RR, Eke A. Women’s disclosure of HIV status: experiences of mistreatment and violence in an urban setting. Women Health. 1997;25(3):19–31. doi: 10.1300/J013v25n03_02. doi:10.1300/J013v25n03_02. [DOI] [PubMed] [Google Scholar]
- Gyekye AB, Akinboade OA. A profile of poverty in the Limpopo province of South Africa. Eastern Africa Social Science Research Review. 2003;19(2):89–109. [Google Scholar]
- Hand GA, Phillips KD, Dudgeon WD. Perceived stress in HIV-infected individuals: physiological and psychological correlates. AIDS Care. 2006;18(8):1011–1017. doi: 10.1080/09540120600568376. doi:10.1080/09540120600568376. [DOI] [PubMed] [Google Scholar]
- Hatcher AM, Woollett N, Pallitto CC, Mokoatle K, Stockl H, MacPhail C, Garcia-Moreno C. Bidirectional links between HIV and intimate partner violence in pregnancy: implications for prevention of mother-to-child transmission. J Int AIDS Soc. 2014;17:19233. doi: 10.7448/IAS.17.1.19233. doi:10.7448/ias.17.1.19233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jewkes RK, Dunkle K, Nduna M, Shai N. Intimate partner violence, relationship power inequity, and incidence of HIV infection in young women in South Africa: a cohort study. Lancet. 2010;376(9734):41–48. doi: 10.1016/S0140-6736(10)60548-X. doi:10.1016/s0140-6736(10)60548-x. [DOI] [PubMed] [Google Scholar]
- Karim QA, Kharsany AB, Frohlich JA, Werner L, Mashego M, Mlotshwa M, Abdool Karim SS. Stabilizing HIV prevalence masks high HIV incidence rates amongst rural and urban women in KwaZulu-Natal, South Africa. Int J Epidemiol. 2011;40(4):922–930. doi: 10.1093/ije/dyq176. doi:10.1093/ije/dyq176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ketchen B, Armistead L, Cook S. HIV infection, stressful life events, and intimate relationship power: the moderating role of community resources for black South African women. Women Health. 2009;49(2-3):197–214. doi: 10.1080/03630240902963648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiarie JN, Farquhar C, Richardson BA, Kabura MN, John FN, Nduati RW, John-Stewart GC. Domestic violence and prevention of mother-to-child transmission of HIV-1. AIDS. 2006;20(13):1763. doi: 10.1097/01.aids.0000242823.51754.0c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kouyoumdjian FG, Calzavara LM, Bondy SJ, O’Campo P, Serwadda D, Nalugoda F, Gray R. Intimate partner violence is associated with incident HIV infection in women in Uganda. AIDS. 2013;27(8):1331–1338. doi: 10.1097/QAD.0b013e32835fd851. doi:10.1097/QAD.0b013e32835fd851. [DOI] [PubMed] [Google Scholar]
- Kouyoumdjian FG, Findlay N, Schwandt M, Calzavara LM. A systematic review of the relationships between intimate partner violence and HIV/AIDS. PLoS One. 2013;8(11):e81044. doi: 10.1371/journal.pone.0081044. doi:10.1371/journal.pone.0081044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y, Marshall CM, Rees HC, Nunez A, Ezeanolue E, Ehiri J. Intimate partner violence and HIV infection among women: a systematic review and meta-analysis. J Int AIDS Soc. 2014;17(1) doi: 10.7448/IAS.17.1.18845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y, Marshall CM, Rees HC, Nunez A, Ezeanolue EE, Ehiri JE. Intimate partner violence and HIV infection among women: a systematic review and meta-analysis. J Int AIDS Soc. 2014;17:18845. doi: 10.7448/IAS.17.1.18845. doi:10.7448/ias.17.1.18845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maman S, Campbell J, Sweat MD, Gielen AC. The intersections of HIV and violence: directions for future research and interventions. Soc Sci Med. 2000;50(4):459–478. doi: 10.1016/s0277-9536(99)00270-1. [DOI] [PubMed] [Google Scholar]
- Maman S, Mbwambo JK, Hogan NM, Kilonzo GP, Campbell JC, Weiss E, Sweat MD. HIV-positive women report more lifetime partner violence: findings from a voluntary counseling and testing clinic in Dar es Salaam, Tanzania. American journal of public health. 2002;92(8):1331–1337. doi: 10.2105/ajph.92.8.1331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maman S, Moodley D, Groves A, Smith E. Integrating health, psychosocial and legal support for pregnant women in South Africa. HIV AIDS Policy Law Rev. 2007;12(2-3):61–63. [PubMed] [Google Scholar]
- Maman S, Moodley D, McNaughton-Reyes HL, Groves AK, Kagee A, Moodley P. Efficacy of enhanced HIV counseling for risk reduction during pregnancy and in the postpartum period: a randomized controlled trial. PLoS One. 2014;9(5):e97092. doi: 10.1371/journal.pone.0097092. doi:10.1371/journal.pone.0097092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mattson C, Settergren S, Sabatier J. Spousal sexual violence, HIV, and sexually transmitted infections: An evaluation of demographic and health survey data-Zimbabwe (2005-2006), Malawi (2004), and Kenya (2003); Paper presented at the Am J Epidemiol.2009. [Google Scholar]
- Medley A, Garcia-Moreno C, McGill S, Maman S. Rates, barriers and outcomes of HIV serostatus disclosure among women in developing countries: implications for prevention of mother-to-child transmission programmes. Bull World Health Organ. 2004;82(4):299–307. [PMC free article] [PubMed] [Google Scholar]
- Mulrenan C, Colombini M, Howard N, Kikuvi J, Mayhew SH. Exploring risk of experiencing intimate partner violence after HIV infection: a qualitative study among women with HIV attending postnatal services in Swaziland. BMJ Open. 2015;5(5):e006907. doi: 10.1136/bmjopen-2014-006907. doi:10.1136/bmjopen-2014-006907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray LK, Haworth A, Semrau K, Singh M, Aldrovandi GM, Sinkala M, Bolton PA. Violence and abuse among HIV-infected women and their children in Zambia: a qualitative study. J Nerv Ment Dis. 2006;194(8):610–615. doi: 10.1097/01.nmd.0000230662.01953.bc. doi:10.1097/01.nmd.0000230662.01953.bc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ntaganira J, Muula AS, Siziya S, Stoskopf C, Rudatsikira E. Factors associated with intimate partner violence among pregnant rural women in Rwanda. Rural Remote Health. 2009;9(3):1153. [PubMed] [Google Scholar]
- O’Leary KD. Couple therapy and physical aggression. Clinical handbook of couple therapy. 2008;4:478–498. [Google Scholar]
- Pettifor AE, Measham DM, Rees HV, Padian NS. Sexual power and HIV risk, South Africa. Emerging infectious diseases. 2004;10(11):1996–2004. doi: 10.3201/eid1011.040252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sa Z, Larsen U. Gender inequality increases women’s risk of HIV infection in Moshi, Tanzania. Journal of biosocial science. 2008;40(04):505–525. doi: 10.1017/S002193200700257X. [DOI] [PubMed] [Google Scholar]
- SAS Institute Inc. SAS® 9.3. Cary, NC; 2011. [Google Scholar]
- Siemieniuk RA, Krentz HB, Miller P, Woodman K, Ko K, Gill MJ. The clinical implications of high rates of intimate partner violence against HIV-positive women. J Acquir Immune Defic Syndr. 2013;64(1):32–38. doi: 10.1097/QAI.0b013e31829bb007. doi:10.1097/QAI.0b013e31829bb007. [DOI] [PubMed] [Google Scholar]
- Strebel A, Crawford M, Shefer T, Cloete A, Henda N, Kaufman M, Kalichman S. Social constructions of gender roles, gender-based violence and HIV/AIDS in two communities of the Western Cape, South Africa. SAHARA J. 2006;3(3):516–528. doi: 10.1080/17290376.2006.9724879. doi:10.1080/17290376.2006.9724879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van der Straten A, King R, Grinstead O, Vittinghoff E, Serufilira A, Allen S. Sexual coercion, physical violence, and HIV infection among women in steady relationships in Kigali, Rwanda. AIDS and Behavior. 1998;2(1):61–73. [Google Scholar]
- Were E, Curran K, Delany-Moretlwe S, Nakku-Joloba E, Mugo NR, Kiarie J, Team P. i. P. H. H. T. S. A prospective study of frequency and correlates of intimate partner violence among African heterosexual HIV serodiscordant couples. AIDS. 2011;25(16):2009. doi: 10.1097/QAD.0b013e32834b005d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zablotska IB, Gray RH, Koenig MA, Serwadda D, Nalugoda F, Kigozi G, Wawer M. Alcohol use, intimate partner violence, sexual coercion and HIV among women aged 15–24 in Rakai, Uganda. AIDS and Behavior. 2009;13(2):225–233. doi: 10.1007/s10461-007-9333-5. [DOI] [PubMed] [Google Scholar]