Abstract
Background/Aims
Recruitment of subjects is critical to the success of any clinical trial, but achieving this goal can be a challenging endeavor. Volunteer nurse and student enrollers are potentially an important source of recruiters for hospital-based trials; however, little is known of either the efficacy or cost of these types of enrollers. We assessed volunteer clinical nurses and health science students in their rates of enrolling family members in a hospital-based, pragmatic clinical trial of cardiopulmonary resuscitation education, and their ability to achieve target recruitment goals. We hypothesized that students would have a higher enrollment rate and are more cost-effective compared to nurses.
Methods
Volunteer nurses and student enrollers were recruited from eight institutions. Participating nurses were primarily bedside nurses or nurse educators while students were pre-medical, pre-nursing, and pre-health students at local universities. We recorded the frequency of enrollees recruited into the clinical trial by each enroller. Enrollers’ impressions of recruitment were assessed using mixed methods surveys. Cost was estimated based on enrollment data. Overall enrollment data were analyzed using descriptive statistics and generalized estimating equations.
Results
From 02/2012 to 11/2014, 260 hospital personnel (167 nurses and 93 students) enrolled 1,493 cardiac patients’ family members, achieving target recruitment goals. Of those recruited, 822 (55%) were by nurses, while 671 (45%) were by students. Overall, students enrolled 5.44 (95% CI: 2.88, 10.27) more subjects per month than nurses (p<0.01). After consenting to participate in recruitment, students had a 2.85 (95% CI 1.09, 7.43) increased chance of enrolling at least one family member (p=0.03). Among those who enrolled at least one subject, nurses enrolled a mean of 0.51(95% CI 0.42, 0.59) subjects monthly, while students enrolled 1.63 (95%CI: 1.37, 1.90) per month (p<0.01). Of 198 surveyed hospital personnel (127 nurses, 71 students), 168/198 (85%) felt confident conducting enrollment. The variable cost per enrollee recruited was $25.38 per subject for nurses and $23.30 per subject for students.
Conclusions
Overall, volunteer students enrolled more subjects per month at a lower cost than nurses. This work suggests that recruitment goals for a pragmatic clinical trial can be successfully obtained using both nurses and students.
Keywords: Pragmatic clinical trial, enrollment or recruitment, nurse and student enrollers, cost of enrollers
Introduction
Investigations have highlighted challenges and financial constraints with clinical trial recruitment.1–4 Furthermore, the high cost of recruiting for clinical trials impacts enrollment goals.4,5 Systematic reviews have identified barriers to subject participation, but strategies to improve the process of enrollment for clinical trials to achieve recruitment goals require additional investigation.2,5,6
Previous studies have explored the use of various types of enrollers to improve study recruitment.1,3,4 An investigation in the Journal of Clinical Epidemiology examined the use of nurses and urologists to enroll subjects into a prostate cancer trial and found that nurses were as effective and cost less than physicians.7 Additionally, studies have examined enrollers for clinical trials in non-clinical environments;6,8 for example, the Women’s Health Initiative in Arizona assessed using trained, Hispanic lay advocates and found that the trained lay advocates enrolled adequately.8 It is unclear whether it is feasible to reach target recruitment goals using both volunteer hospital bedside nurses and students or whether one enroller-type is preferred when comparing average recruitment numbers and costs between cohorts. Given the growing trend towards practical or pragmatic approaches to clinical trial study design,9 evaluating the use of volunteer nurses or students to enroll subjects into a clinical trial could inform future use of this model.
We conducted a multicenter, pragmatic randomized clinical trial (RCT) designed to assess cardiopulmonary resuscitation education dissemination strategies to family members of hospitalized cardiac patients. We sought to prospectively evaluate whether nurses and students could recruit family members for this pragmatic clinical trial and maintain recruitment goals. We hypothesized that students would have a higher enrollment rate and would cost less compared to nurses when calculated over the duration of the study.
Methods and study design
The Cardiopulmonary resuscitation Hospital-Initiated Project (CHIP)
Nurses and students were sought to conduct enrollment in a multicenter prospective trial of hospital-based cardiopulmonary resuscitation education for families (the CHIP study) in which family members of high-risk cardiac patients were recruited to learn cardiopulmonary resuscitation before hospital discharge through one of two modalities of cardiopulmonary resuscitation education. Details of the primary investigation are reported elsewhere.10,11 Cardiopulmonary resuscitation was taught through a validated video self-instruction program (Cardiopulmonary resuscitation Anytime Family and Friends, American Heart Association, Dallas, TX, and Laerdal Medical, Stavanger, Norway), which includes an instructional DVD and inflatable practice manikin.12–14 Hospitals were block randomized to training strategies; recruitment materials and RCT transitions were maintained by the research personnel.
Study population and setting
This study was conducted on the inpatient wards at eight acute care hospitals in Southeastern Pennsylvania (Hospital of the University of Pennsylvania, Penn Presbyterian Medical Center, Pennsylvania Hospital, Crozer-Chester Medical Center, Albert Einstein Medical Center Philadelphia, Temple University Hospital, Chester County Hospital, and Taylor Hospital).
Our prospective multicenter observational cohort study was approved by the Institutional Review Boards with jurisdiction over the study sites (University of Pennsylvania (three sites), Crozer-Keystone Health System (two sites), Albert Einstein Healthcare Network, Temple University, and the Chester County Hospital and Health System). Enrollment was conducted using a standard written informed consent process. Bedside nurses and students elected to participate in this research study and enrolled family members of cardiac patients from 2/2012 to 11/2014. The goal for enrollment was 1,450 family members by 12/2014. Participating nurses were staff of cardiology service lines, telemetry wards, step down units, and observation units while students were pre-medical, nursing, and pre-health students at local universities.
Subject recruitment and training
Nurse and student enrollers
Nurses and students at each hospital were recruited to participate in this project through referral from key stakeholders. Nursing personnel were identified by nurse educators, clinical nurse specialists, and nurse managers at participating hospital sites. Students were recruited using pre-medical and pre-health email lists and were screened by study staff through in-person interviews. Interested nurses and students were invited to attend a 30-minute informational session where study personnel presented a general overview of the training program. Upon completion of the informational session, interested nurses and students signed a written informed consent form. Subsequently, the consented nurses and students were referred to as enrollers.
Once consented, enrollers were required to participate in a 30-minute training session. The enrollers were oriented through the study recruitment manual, which included instructions on how to identify and approach a potential family member (inclusion/exclusion criteria), how to consent an individual, how to set up the training materials, and how to collect study forms. Additionally, enrollers went through mock enrollment scenarios with sample study forms. Select enrollers (nurses and students) shadowed “senior” enrollers as a final step to complete the training process.
Once formally trained, all enrollers were asked to integrate the research enrollment process into their weekly routine. During their clinical shifts, nurse enrollers periodically approached potential family members and offered them the opportunity to enroll before their loved one was discharged. Student enrollers were scheduled under a shift-work model and were asked to take at least one two-hour shift per week offering enrollment to eligible family members on approved hospital floors. Student enrollers were not required to conduct any additional responsibilities on the hospital floors or wards.
Research personnel routinely collected completed family member enrollment packets from each study site and recorded which enroller recruited the specified family member. Additionally, demographics such as age, race, gender and classification within the institution were obtained from each enroller. To encourage continued enrollment, various incentives were provided to the nurses and students who participate in this study including opportunities for authorship on academic publications, team lunches, and $25 gift cards (as approved by the IRB).
Enrollment rate and enrollers perspective
To measure enrollment frequency, we tracked individual recruitment by enrollers from time of their consent into the study. We analyzed the recruitment numbers by month and examined the frequency of recruitment by enrollers over time. Further analysis was conducted on the proportion of enrollers who enrolled at least one subject and the average number of enrollees recruited per month by enrollers who enrolled at least one enrollee.
Lastly, enrollers completed a post-training survey to measure their perspectives on the research project. This survey was structured using mixed quantitative and qualitative metrics including Likert scale questions such as “I am comfortable conducting this study” (1=not comfortable at all, 5=extremely comfortable). The survey was administered three months after initial participation in the program.
Cost of enrollment
In order to estimate the cost of enrollment for each approach, we assumed the same fixed costs (training materials, e.g.) and quantified the variable costs for nurses and students. We estimated the number of person-hours of nurse and student time required to enroll one enrollee. Students were asked to record the number of hours worked, number of enrollees approached and recruited. We then used this information to estimate the person-hours of student time required to enroll one enrollee and the ratio of enrolled to declined enrollees. Per conversations with key nurse enrollers, we assumed nurses used 0.25 hours to recruit one enrollee and had a 1:1 enrolled to declined ratio. Nurses were assumed to take 5 minutes to approach a subject who declined enrollment, while a student was assumed to take 10 minutes. Nurse wages were based on the national mean registered nurse wages plus 30% benefits.15 The student opportunity cost was assumed to be 33% of the nurse’s wages and benefits based on the median pay of a medical assistants wage provided by the Bureau of Labor statistics.16
Statistical approach and analysis
All data were compiled in a secure, internet-based database application (REDCap Software Version 5.2.1, Vanderbilt University, Nashville, TN) and analyzed using a statistical software package (STATA 13, Statacorp, College Station, TX). Demographic data were examined using a chi-square test (categorical variables) or, a Student’s t-test (continuous variables). We noted that enrollers generally did not participate in each month of the study; we used Kaplan-Meier survival estimates to assess the difference in active months between nurses and students. A log-rank test was used to examine whether there was a difference in enrollers remaining active in the study. We examined the rates of enrollment per month by all consented enrollers and compared nurses to students using generalized estimating equations to account for repeated enrollment periods (months) and duration of enrollers active participation in the study (active time). To assess frequency of enrollment, a negative binomial distribution was employed to account for over-dispersion in the data. We tested whether age, gender, race, and classification within the institution were associated with the model, and all items were not significant. The final model included hospital site and season of enrollment, specifically winter (November, December, January), spring (February, March, April), summer (May, June, July), and fall (August, September, October). We used generalized estimating equations with a logit link to estimate the proportion of enrollers who enrolled at least one subject to participate in the study. We used generalized estimating equations with a Gaussian distribution to estimate the average number of enrollees recruited per month by enrollers who enrolled at least one subject. All generalized estimating equations models used the same covariates and fixed effects. We conducted a sensitivity analysis examining the frequency of enrollment using four sites with a significant number of both nurse and student enrollers; the relationship was similar to our findings using the larger cohort. Likert scale survey responses were compared between nurses and students using a nonparametric trend test of proportions. Cost modeling was conducted and reported using descriptive statistics.
Results
Enroller demographics
From 02/2012 to 11/2014, 260 hospital personnel were recruited to conduct the Family cardiopulmonary resuscitation training program at eight study hospitals. Among the enrollers, 167 (64%) were nurses and 93 (36%) were students. Descriptive characteristics, demographics, and description of missing demographic covariates of the enroller population are detailed in Table 1.
Table 1.
Enroller Demographics
| Nurse n=167 |
Students n=93 |
p-value | |
|---|---|---|---|
| A. Trainer Demographics: | |||
| Agea | 39±17 | 20±12 | <0.01 |
| Racea | |||
| White | 64 (73%) | 31(49%) | 0.01 |
| Black | 13 (15%) | 6 (10%) | |
| Other | 11 (12%) | 26 (41%) | |
| Gender | |||
| Female | 149 (89%) | 59 (63%) | <0.01 |
| Classification | |||
| Beside Staff Nurse | 149 (90%) | <0.01 | |
| Nurse Educator | 9 (5%) | ||
| Other Nursing Profession | 9 (5%) | ||
| Pre-Med/Health Student | 79 (85%) | ||
| EMTs | 11 (12%) | ||
| Other Student | 3 (3%) | ||
| Hospitalb | |||
| A | 4 (2%) | 39 (42%) | <0.01 |
| B | 44 (27%) | 0 (0%) | |
| C | 19 (11%) | 9 (10%) | |
| D | 19 (11%) | 0 (0%) | |
| E | 36 (22%) | 10 (11%) | |
| F | 10 (6%) | 10 (11%) | |
| G | 35 (21%) | 2 (2%) | |
| H | 0 (0%) | 23 (24%) |
The results are presented as a mean (SD) or frequency (%)
Age - missing 83 data points for nurses and 32 for students; Race – missing 79 nursing data points and 30 student data points.
Hospital names- A: Hospital of the University of Pennsylvania, B: Penn Presbyterian Medical Center, C: Pennsylvania Hospital, D: Crozer- Chester Medical Center, E: Einstein Medical Center, F: Temple Hospital, G: The Chester County Hospital, H: Taylor Hospital
Of the nurses, 149/167 (90%) were bedside nurses, 9/167 (5%) were nurse educators, and 9/167 (5%) were another nursing profession, while 79/93 (85%) of the students were premedical or pre-health, 11/93 (12%) were student EMTs, and 3/93 (3%) were another type of student. Subject cohort demographics differed by age and gender. Nursing enrollers’ mean age was 39±17, while students’ mean age was 20±12 (p<0.01). Additionally, 149/167 (89%) of the nurses were female compared to 59/93 (63%) of the students (p<0.01). Furthermore, 64/88(73%) of the nurses were White, compared to 31/63(49%) of the students. The distribution of the overall race category comparing nurses to students was statistically significant (p=0.01).
Enrollment patterns of nurses and students
From 02/2012 to 11/2014, volunteer nurses and students enrolled 1,493 subjects or 48 subjects per month. The original recruitment goal was 1,450 by 12/2014; this goal was achieved prior to the target date. Of those enrolled, 822/1493(55%) were by nurses, while 671/1493(45%) were by students (Table 2). The mean unadjusted monthly enrollment by all enrollers was 0.25 (95% CI: 0.21, 0.29) by nurses and 1.20 (95% CI: 0.99, 1.41) by students (p<0.01). Of the nurses, 35/167(21%) enrolled at least one enrollee in the study, while 43/93(46%) of the students enrolled at least one enrollee (p<0.01). The mean unadjusted monthly enrollment by enrollers who participated in the study (enrolled > 1 person) was 0.51(95% CI: 0.42, 0.59) by nurses and 1.63 (95% CI: 1.37, 1.90) by students (p<0.01). (Table 2)
Table 2.
Overall enrollment patterns of nurses and students
| Nurses n=167 (95% CI) |
Students n=93 (95% CI) |
p-value | |
|---|---|---|---|
| Enrollees enrolled | 822 (55%) | 671 (45%) | <0.01 |
| Mean monthly enrollment of all enrollers | 0.25 (0.21, 0.29) | 1.20 (0.99, 1.41) | <0.01 |
| Proportion of enrollers who enrolled at least one trainee | 0.21(21%) | 0.46 (46%) | <0.01 |
| Mean monthly enrollment among those who enrolled at least one trainee | 0.51(0.42, 0.59) | 1.63 (1.37, 1.90) | <0.01 |
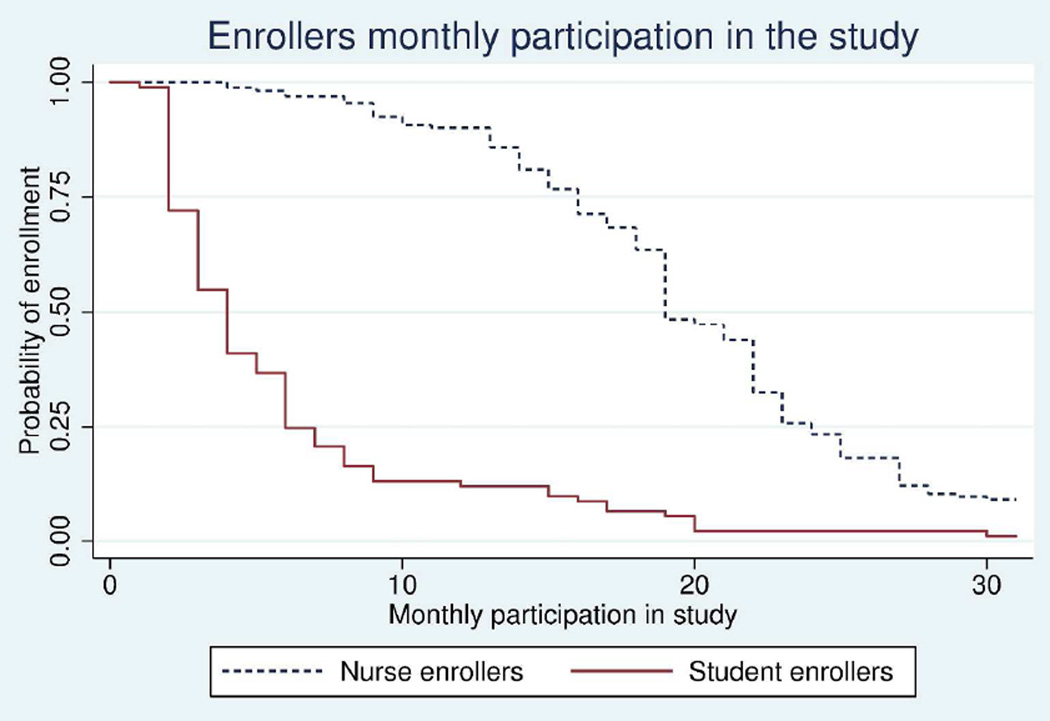
We examined the enrollers’ active time in the study. The median active time for nurses was 19 (95% CI: 19, 22) months, while the median active time for students was 4 (95% CI: 3, 5) months. Nurses had a statistically significant longer active time than students (p<0.01). (Figure 1)
Figure 1. Enrollers monthly participation in the study.
Active participation and probability of enrollment by enroller cohort.
When accounting for all enrollers’ active time in the study using a generalized estimating equations model, students enrolled 5.44 (95% CI: 2.88, 10.27) more subjects monthly than nurses (p<0.01) (Table 3). Over time, mean monthly enrollment decreased (0.95 (95% CI: 0.92, 0.99), p=0.01). Seasonality was significantly related to enrollment; specifically, individuals enrolled 1.77 (95%CI: 1.34, 2.35) more subjects in the spring than winter months (p<0.01). This relationship was still statistically significant when considering the effect of time on this relationship in a generalized estimating equations model (p<0.01). Students had a 2.85 (95% CI: 1.09, 7.43) increased odds of enrolling at least one subject in the project (p=0.03). Seasonality was not statistically significant in this model (p=0.35), however, hospital site was (p=0.02). (Table 4) Among those who enrolled at least one subject, the mean rate of enrollment per month differed by 2.00 (95% CI: 1.29, 2.71) with students enrolling more than nurses. Seasonality and hospital site were statistically related to enrollment in this model. (Table 5)
Table 3.
Ratio of monthly enrollment of subjects per students versus nurses adjusted for key covariates.* Values shown are rate ratios (RR) with 95% CI. Baseline categories are identified for each categorical covariate.
| RRa (95% CI) | Global p-value | Individual p-value | ||
|---|---|---|---|---|
| Title | Nurses (baseline) | na | - | |
| Students | 5.44 (2.88, 10.27) | <0.01 | ||
| Active Time | 0.95 (0.92, 0.99) | 0.01 | ||
| Season | Winter (baseline) | na | <0.01 | - |
| Spring | 1.77 (1.34, 2.35) | <0.01 | ||
| Summer | 0.97 (0.72, 1.31) | 0.86 | ||
| Fall | 0.98 (0.69, 1.39) | 0.92 | ||
| Hospitalb | A(baseline) | na | 0.15 | - |
| B | 0.96 (0.27, 3.41) | 0.95 | ||
| C | 1.45 (0.77, 2.71) | 0.25 | ||
| D | 1.25 (0.27, 5.74) | 0.77 | ||
| E | 1.58 (0.78, 3.21) | 0.21 | ||
| F | 0.76 (0.34, 1.68) | 0.50 | ||
| G | 1.03 (0.32, 3.24) | 0.97 | ||
| H | 0.39 (0.17, 0.92) | 0.03 |
RR: Rate Ratio which is the frequency of enrollment occurring by month over the duration of enrollers participating in the study;
Hospital names- see prior figure.
The model assumed a negative bionomial distribution and was fit using generalized estimating equations
Table 4.
Proportion of those who enrolled; modeled using generalized estimating equations with a logit distribution.
| Odds Ratio (95% CI) | Global p-value | Individual p-value | ||
|---|---|---|---|---|
| Title | Nurses (baseline) | - | - | |
| Students | 2.85 (1.09, 7.43) | 0.03 | ||
| Time from initial enrollment | - | - | ||
| Season | Winter (baseline) | - | 0.35 | - |
| Spring | 1.69 (0.56, 5.15) | 0.35 | ||
| Summer | 2.41 (0.85, 6.84) | 0.10 | ||
| Fall | 1.27 (0.34, 4.75) | 0.72 | ||
| Hospitala | A(baseline) | - | 0.02 | |
| B | 0.59 (0.15, 2.24) | 0.44 | ||
| C | 0.29 (0.78, 1.08) | 0.06 | ||
| D | 0.92 (0.18, 4.80) | 0.92 | ||
| E | 1.83 (0.61, 5.51) | 0.29 | ||
| F | 1.23 (0.36, 4.20) | 0.74 | ||
| G | 0.37 (0.09, 1.59) | 0.18 | ||
| H | 0.33 (0.11, 0.99) | 0.05 | ||
Hospital names- see prior figure
Table 5.
The mean rate of enrollment per nurse or student per month among those who enrolled at least one subject; modeled using generalized estimating equations with a gaussian distribution.
| Coef (95% CI) | Global p-value | Individual p-value | ||
|---|---|---|---|---|
| Title | Nurses (baseline) | - | - | |
| Students | 2.00 (1.29, 2.71) | <0.01 | ||
| Time from initial enrollment | −0.10 | 0.12 | ||
| Season | Winter (baseline) | - | <0.01 | |
| Spring | 1.15 (0.01, 2.30) | 0.05 | ||
| Summer | 0.75 (−0.45, 1.96) | 0.22 | ||
| Fall | −0.61 (−1.35, 0.15) | 0.72 | ||
| Hospitala | A(baseline) | - | <0.01 | |
| B | 0.95 (−0.68, 2.57) | 0.25 | ||
| C | 0.72 (0.13, 1.31) | 0.02 | ||
| D | 1.77 (0.14, 3.40) | 0.03 | ||
| E | 0.38 (−0.15, 0.91) | 0.16 | ||
| F | 1.92 (0.88, 2.95) | <0.01 | ||
| G | 1.29 (0.05, 2.52) | 0.04 | ||
| H | 0.63 (−0.27, 1.53) | 0.17 | ||
Hospital names- see prior figure.
Enroller surveys
Of the 260 enrollers, 198 (76%) participated in the enrollers surveys (127 nurses, 71 students). Overall, 187/198 (94%) of the enrollers felt they were the appropriate individual to enroll family members for the CHIP study. Additionally, 53/198 (27%) of the enrollers reported encountering challenges while implementing the enrollment process. Regarding comfort conducting enrollment, 168/198 (85%) felt confident conducting the research project, while the mean Likert scale response (1=not confident, 5=extremely confident) among the nursing cohort was 4.2±1.2 compared to 4.7±0.7 among the student cohort (p<0.01). Furthermore, regarding whether the recruitment process impacted the enroller’s daily workload, the mean Likert scale response (1=do not agree, 5=strongly agree) among the nurses was 3.5±1.5 compared to 3.1±1.7 among the students (p=0.04).
Cost of enrollment for a nurse or student
The cost per enrollee instructed was $25.38 for nurses and $23.30 for students. This was mostly due to student’s lower opportunity cost, or hourly wages and benefits. Even though students took a longer time to recruit an enrollee (0.86 vs. 0.25 hours) and had lower recruitment success rate (0.2 vs 0.5), the cost was comparable. The ratio of enrolled to declined enrollees for students were estimated to be 1:4, while the ratio for nurses was estimated to be 1:1. Other costs that may be varied through this model include the cost of the cardiopulmonary resuscitation training curriculum and the cost for research personnel to train nurses and students; these costs were assumed to be similar in our model. Additional fixed costs included the research personnel’s wages, transportation, and research supplies.
Discussion
In our current work, we found that achieving recruitment goals for an education-based pragmatic RCT was attainable using both volunteer bedside nurse and student enrollers. Additionally, students on average enrolled more trainees monthly over the duration of the study when compared to nurses. Furthermore, there are cost and implementation considerations for using nurse or student enrollers that should be considered when preparing for future investigations.
Enrollment rate variation
Recruitment varied significantly between the nurse and student enroller cohorts with students enrolling on average 5.44 (95% CI: 2.88, 10.27) more subjects monthly, while nurses recruited more subjects overall compared to students. This initial variation may be due to a small number of nurses contributing to the majority of the overall nursing enrollment. The higher student enrollment rate may be due to proportionally more students attempting initial enrollment, whereas fewer nurses initially recruited for the study. That nurses were found to have a significantly longer active time of enrollment but a lower average recruitment rate constitutes an interesting finding, and suggests that motivations and barriers to enrollment is likely to vary in type and extent according to enroller type.
Since this was an observational study, variation could be influenced by a variety of unmeasured environmental factors. Specifically, nurses were recruiting family members for this research project while balancing multiple work-related demands which may have influenced their overall enrollment rate. To support this notion, a recent study examined barriers to research among nurses and found that nurses struggle finding time to engage in research.17 In contrast, students were exclusively enrolling for this project, meaning they did not have competing tasks to balance while recruiting. Future work may consider the process variables related to enrollment by site while assessing whether there are motivational factors that may influence enrollment.
Motivation to voluntarily participate in the RCT
The variation in the enrollment rate suggests there were environmental factors and individual motivational factors that may have influenced the enrollers. While this study was not designed to capture motivation for participating in the RCT, other studies have explored using students to recruit subjects in various hospital settings including the emergency department.18–20 Hollander et al examined using students and suggested that the student’s motivation for participation was the opportunity to become an author on publications and participate in national meetings.19,20 Through participation in our study, students and nurses had the opportunity to obtain letters of recommendation from faculty and members of our team.
Additionally, we provided various incentives for the nurses and students to participate in this study including opportunities for authorship on academic publications, team lunches, and $25 gift cards (as approved by the IRB). Studies have demonstrated that establishing a research culture is important for engagement in clinical research.21,22 Future work may be conducted to explore both student and nurse motivation for participating in clinical research, to help maximize this model for future implementation.
Enroller cost implications
Through our cost analysis, we found that the student-only enroller model was equivalent to the nurse-only model. This is largely due to nursing time being more costly than student time, thus roughly compensating for the lower success rates achieved by students participating in clinical research. Given the similar cost difference per enrollee, both recruitment models are viable options. Since this was a low-risk study, we do not perceive any associated risks with using students in the role as an enroller – studies deemed higher-risk may reconsider the use of a student enroller. Implementation of these recruitment models should also consider location and available resources. For example, a location with more limited access to academic institutions or teaching hospitals may be less ideal to implement the student-only recruitment model.
Future items for evaluation
Given our finding that the use of nurses and students to enroll in a clinical trial is feasible, a more robust analysis of enroller motivation for participation may be warranted. Understanding what motivates enrollers who are not primarily compensated to participate in a clinical research study would be beneficial for future implementation of research projects that use nurses or students to conduct enrollment. Additionally, the significance of individual hospital sites varied by statistical model. Future work should examine the administration and environmental-factors within hospitals to help inform future implementation. Understanding this model may serve as a foundation to establish more robust pragmatic clinical trials. Specifically, this study may have important implications for prospective observational studies and low risk RCTS, serving as a model for a hospital-based enrollment platform.
Limitations
Several limitations to this project should be noted. First, since this was a secondary analysis of a larger prospective randomized controlled trial, the cost analysis was based on many assumptions and estimates. In addition, we did not include the costs associated with orienting volunteers that are levied by other institutions such as preventative screenings for new volunteers and the labor associated with volunteer orientation. Second, we were unable to obtain demographics, specifically age and race from many of our enrollers, and there was site enrollment variation, and previously discussed unmeasured environmental confounding. Furthermore, we were unable to obtain recruitment logs from the nurses resulting in our estimation of the length of enrollment time for nurses. Despite these limitations, the data suggest enrollment variation between volunteer nurse and student enrollers within our cohort. These data may be useful for future recruitment considerations of pragmatic clinical trials.
Conclusion
This work suggests that implementation of an education-based, pragmatic RCT with fixed recruitment goals using nurse or student enrollers is feasible. Additionally, this work demonstrates that students can effectively recruit more subjects at a similar cost as nurses. Investigators considering executing a pragmatic or low risk RCT may consider their available resources and hospital environment before deciding upon nurse or student enrollers.
Acknowledgments
Financial Support: This work was supported by a grant from the National Institutes of Health (R18HL107217).
We would like to thank the nurse and student volunteers at the Hospital of the University of Pennsylvania, Penn Presbyterian Medical Center, Pennsylvania Hospital, Crozer-Chester Medical Center, Taylor Hospital, Temple University Hospital, Einstein Medical Center, and The Chester County Hospital. We would also like to thank Russell Localio, PhD for his review of the enroller rate biostatistical methods and Andrew Murray for his review of the manuscript.
Conflict of interest disclosures
Ms. Blewer has research funding through the American Heart Association. Ms. Leary has research funding through the American Heart Association and Laerdal Medical Foundation. Ms. Leary has received in-kind support from Laerdal and Physio-Control. Dr. Abella has received research funding and honoraria from Philips Healthcare, in-kind research support from Laerdal Medical Corporation and research funding from Medtronic Foundation.
Footnotes
Clinical Trial Registration: NCT01514656
References
- 1.Caldwell PH, Hamilton S, Tan A, et al. Strategies for increasing recruitment to randomised controlled trials: systematic review. PLoS Med. 2010;7:e1000368. doi: 10.1371/journal.pmed.1000368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ross S, Grant A, Counsell C, et al. Barriers to participation in randomised controlled trials: a systematic review. J Clin Epidemiol. 1999;52:1143–1156. doi: 10.1016/s0895-4356(99)00141-9. [DOI] [PubMed] [Google Scholar]
- 3.Page MJ, French SD, McKenzie JE, et al. Recruitment difficulties in a primary care cluster randomised trial: investigating factors contributing to general practitioners' recruitment of patients. BMC Med Res Methodol. 2011;11:35. doi: 10.1186/1471-2288-11-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Eapen ZJ, Vavalle JP, Granger CB, et al. Rescuing clinical trials in the United States and beyond: a call for action. Am Heart J. 2013;165:837–847. doi: 10.1016/j.ahj.2013.02.003. [DOI] [PubMed] [Google Scholar]
- 5.Fletcher B, Gheorghe A, Moore D, et al. Improving the recruitment activity of clinicians in randomised controlled trials: a systematic review. BMJ Open. 2012;2:e000496. doi: 10.1136/bmjopen-2011-000496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Watson JM, Torgerson DJ. Increasing recruitment to randomised trials: a review of randomised controlled trials. BMC Med Res Methodol. 2006;6:34. doi: 10.1186/1471-2288-6-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Donovan JL, Peters TJ, Noble S, et al. Who can best recruit to randomized trials? Randomized trial comparing surgeons and nurses recruiting patients to a trial of treatments for localized prostate cancer (the ProtecT study) J Clin Epidemiol. 2003;56:605–609. doi: 10.1016/s0895-4356(03)00083-0. [DOI] [PubMed] [Google Scholar]
- 8.Larkey LK, Staten LK, Ritenbaugh C, et al. Recruitment of Hispanic women to the Women's Health Initiative. the case of Embajadoras in Arizona. Control Clin Trials. 2002;23:289–298. doi: 10.1016/s0197-2456(02)00190-3. [DOI] [PubMed] [Google Scholar]
- 9.Tunis SR, Stryer DB, Clancy CM. Practical clinical trials: increasing the value of clinical research for decision making in clinical and health policy. JAMA. 2003;290:1624–1632. doi: 10.1001/jama.290.12.1624. [DOI] [PubMed] [Google Scholar]
- 10.Blewer AL, Leary M, Decker CS, et al. Cardiopulmonary resuscitation training of family members before hospital discharge using video self-instruction: a feasibility trial. J Hosp Med. 2011;6:428–432. doi: 10.1002/jhm.847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Blewer AL, Li J, Leary M, et al. Video-only cardiopulmonary resuscitation education for families before hospital discharge: a multicenter pragmatic clinical trial. Circulation. 2015;132:A15569. doi: 10.1161/CIRCOUTCOMES.116.002493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Roppolo LP, Pepe PE, Campbell L, et al. Prospective, randomized trial of the effectiveness and retention of 30-min layperson training for cardiopulmonary resuscitation and automated external defibrillators: The American Airlines Study. Resuscitation. 2007;74:276–285. doi: 10.1016/j.resuscitation.2006.12.017. [DOI] [PubMed] [Google Scholar]
- 13.Einspruch EL, Lynch B, Aufderheide TP, et al. Retention of CPR skills learned in a traditional AHA Heartsaver course versus 30-min video self-training: a controlled randomized study. Resuscitation. 2007;74:476–486. doi: 10.1016/j.resuscitation.2007.01.030. [DOI] [PubMed] [Google Scholar]
- 14.Potts J, Lynch B. The American Heart Association CPR Anytime Program: the potential impact of highly accessible training in cardiopulmonary resuscitation. J Cardiopulm Rehabil. 2006;26:346–354. doi: 10.1097/00008483-200611000-00002. [DOI] [PubMed] [Google Scholar]
- 15.Bureau of Labor Statistics, U.S. Department of Labor. Occupational Outlook Handbook, 2014–2015 Edition. [accessed 6 October 2015];2014 http://www.bls.gov/ooh/healthcare/registered-nurses.htm.
- 16.Bureau of Labor Statistics, U.S. Department of Labor. Occupational Outlook Handbook, 2014–2015 Edition. [accessed 6 October 2015];2014 http://www.bls.gov/ooh/healthcare/medicalassistants.htm.
- 17.Atkinson M, Turkel M, Cashy J. Overcoming barriers to research in a Magnet community hospital. J Nurs Care Qual. 2008;23:362–368. doi: 10.1097/01.NCQ.0000336675.48466.37. [DOI] [PubMed] [Google Scholar]
- 18.Steadman PE, Crudden J, Naranian T, et al. The effectiveness of a student volunteer program for research in a pediatric Emergency Department. J Emerg Med. 2015;48:19–25. doi: 10.1016/j.jemermed.2014.06.039. [DOI] [PubMed] [Google Scholar]
- 19.Hollander JE, Singer AJ. An innovative strategy for conducting clinical research: the academic associate program. Acad Emerg Med. 2002;9:134–137. doi: 10.1111/j.1553-2712.2002.tb00230.x. [DOI] [PubMed] [Google Scholar]
- 20.Hollander JE, Valentine SM, Brogan GX., Jr Academic associate program: integrating clinical emergency medicine research with undergraduate education. Acad Emerg Med. 1997;4:225–230. doi: 10.1111/j.1553-2712.1997.tb03747.x. [DOI] [PubMed] [Google Scholar]
- 21.Higgins I, Parker V, Keatinge D, et al. Doing clinical research: the challenges and benefits. Contemp Nurse. 2010;35:171–181. doi: 10.5172/conu.2010.35.2.171. [DOI] [PubMed] [Google Scholar]
- 22.Wilkes L, Cummings J, McKay N. Developing a culture to facilitate research capacity building for clinical nurse consults in generalist pediatric practice. Nurs Res Pract. 2013;2013:709025. doi: 10.1155/2013/709025. [DOI] [PMC free article] [PubMed] [Google Scholar]