Abstract
Using electronic health record data, we examined longitudinal changes in community health center (CHC) visit rates from 2013 through 2014 in Medicaid expansion versus non-expansion states. Visits from 219 CHCs in five expansion states and four non-expansion states were included. Rates were computed using generalized estimating equation Poisson models. Rates increased in expansion state CHCs for new patient, preventive, and limited-service visits (14%, 41%, and 23%, respectively, P<.01 for all), while these rates remained unchanged in non-expansion states. One year after ACA Medicaid expansions, CHCs in expansion states saw an influx of new patients and provided increased preventive services.
Keywords: Community health centers, Uninsured, Affordable Care Act, Medicaid, Health insurance, Ambulatory care
Introduction
The Patient Protection and Affordable Care Act of 2010 (ACA) was enacted to expand health insurance to all citizens and legal residents, and thus facilitate access to healthcare.(Asplin et al., 2005; Bindman et al., 1995; Burstin, Lipsitz, & Brennan, 1992; Smolderen et al., 2010) The ACA called for Medicaid coverage expansions to individuals in households earning ≤138% of the federal poverty level (FPL). Despite passage of the ACA, in 2012 the Supreme Court ruled that states were not legally required to implement these Medicaid expansions.(Supreme Court of the United States, 2012) As of January 2014, 25 states (and the District of Columbia) had implemented Medicaid expansion, while 25 had not.(Henry J. Kaiser Family Foundation, 2013) An estimated 11.2 million people enrolled in Medicaid programs in the first year after implementation of these new insurance opportunities; states that expanded Medicaid saw a much larger increase in enrollment compared to states that did not expand (a 26% versus 8% increase, respectively).(The Henry J Kaiser Family Foundation, 2015)
Assessing the ACA’s impact is vital for informing future national and state policies. For states still considering expanding Medicaid and those planning for future Medicaid expenditures, a better understanding of the immediate and longer term effects of the ACA is essential.(Rice et al., 2014) Community health centers (CHCs), part of the ambulatory care ‘safety net’, serve the primary health care needs of 23 million people across the United States; the majority of CHC patients are either uninsured (36%) or Medicaid insured (40%).(National Association of Community Health Centers, 2014) Therefore, many are eligible for new coverage under the ACA and CHCs will likely see significant changes in demand for their services.(Morgan, 2012; The White House, 2012) Studies have shown that previous Medicaid expansions significantly impacted CHCs’ payer mix, but these analyses assessed changes in single states only, had limited follow-up periods, did not assess impact on type of CHC visits, or were based on survey data subject to recall bias.(Baicker et al.; McCormick, Sayah, Lokko, Woolhandler, & Nardin; Sommers, Baicker, & Epstein) Angier et al. (2015) describe CHC visit coverage rates in the first six months after implementation of the ACA’s insurance opportunities in a sample of states that expanded Medicaid versus states that did not. They found a 36% increase in Medicaid visit rates and a corresponding 40% decrease in uninsured visits in expansion states the first six months of 2014. Since gains and losses in health insurance are common,(Henry J. Kaiser Family Foundation, 2015a) it remains unknown whether this initial influx of Medicaid visits will persist over time. Moreover, earlier analyses did not assess the impact of Medicaid expansion on different visit types (new patient, preventive services, and mental/behavioral health visits).
To expand on previous work and provide further insight into the ACA’s impact on CHCs in expansion and non-expansion states, this study assesses CHC utilization a full year before and after the implementation of ACA Medicaid expansions (24 months) and describes changes in visit type before and after implementation.
Methods
Data Source and Study Population
We utilized electronic health record (EHR) data from the OCHIN community health information network, a multi-state collaboration of health systems, described elsewhere.(J. DeVoe & Sears, 2013; J. E. DeVoe et al., 2011) In this study ‘CHCs’ represent individual clinic sites; in many cases multiple CHC clinic sites comprise a larger health system (e.g., a county health department). We included a convenience sample of 239 non-dental CHCs ‘live’ on OCHIN’s EHR as of 1/1/2013, located in five Medicaid expansion states (California, Minnesota, Ohio, Oregon, and Washington) and six non-expansion states (Alaska, Indiana, Montana, North Carolina, Texas, and Wisconsin). CHCs in Texas (n=4 CHCs) and Wisconsin (n=16 CHCs) were excluded due to competing state initiatives during the study period.(Angier et al., 2015) We collected all billed visits among non-pregnant adults aged 19–64 from 12 months pre-expansion (1/1/2013–12/31/2013) through 12 months post-expansion (1/1/2014–12/31/2014). Our final sample included 401,988 patients with 2,147,910 visits from 219 CHCs in five Medicaid expansion states and four non-expansion states.
Variables
We assessed rates of uninsured, Medicaid-insured, and commercially-insured CHC visits in the pre- versus post-expansion periods overall and by month across the 24-month study period. We calculated post- versus pre-expansion utilization rate ratios by visit type [new or established patient; primary care, preventive care, mental/behavioral health, or limited-service visits (i.e., nurse-, lab-, immunization-, or imaging-only)]. Visit type categories were identified using the primary Current Procedural Terminology (CPT) code for each visit. We also used the EHR-coded visit type to identify mental/behavioral health and limited-service visits, and clinic type for mental/behavioral health visits. The primary independent variable was expansion status: whether or not a state expanded Medicaid eligibility to ≤138% FPL as of January 1, 2014.
Data Analysis
Patient panel characteristics between patients in expansion versus non-expansion states were compared using chi-square statistics. We calculated visit rates by dividing the number of visits in a given interval (i.e., month or year) by the total number of adult patients seen in a given clinic over the 24-month study period. In a pre- versus post-expansion analysis, we compared each visit rate outcome by state and by expansion versus non-expansion status. Finally, we assessed temporal patterns of visit rates by month across the entire study period, stratified by coverage type, comparing the group of CHCs in expansion states to that in non-expansion states.
To account for differences in the composition of the CHCs’ patient panels, we adjusted for CHC-level proportions of sex, age, race, ethnicity, urban or rural residence, and household income. When comparing expansion versus non-expansion status, we considered potential state-level economic covariates: 2014 minimum wage and unemployment rates,(Bureau of Labor Statistics, 2014; CNN, 2014) 2013 rate of uninsured adults,(Witters, 2014) and insurance exchange type (state-run or federally facilitated).(Henry J. Kaiser Family Foundation, 2014) We fitted generalized estimating equation (GEE) Poisson models with compound symmetry correlation structure and empirical sandwich variance estimator to obtain rates and rate ratios (RRs) for the pre- and post-periods with 95% confidence intervals (CIs), accounting for temporal correlation within CHCs, and adjusting for patient panel and state-level covariates. We fitted similar longitudinal regression models to obtain visit rates by month across the study period; each monthly model was adjusted for patient panel and state-level covariates significant at P<.05.
All statistical analyses were completed using SAS version 9.3 (SAS Institute, Inc.). This study was reviewed and approved by the Oregon Health & Science University Institutional Review Board.
Results
In the composite, CHCs in states that expanded Medicaid had proportionally fewer females, non-white patients, and younger patients compared to CHCs in non-expansion states. They also had more Hispanic patients, patients in urban areas, and patients with incomes ≤138% FPL (P<.001 for all); patient panels in individual states varied (Table 1). Comparing pre- vs. post-expansion years, the total patient volume in expansion state CHCs increased by 6.0% (from 246,852 to 261,574 patients) and visit volume increased 6.2% (from 953,365 to 1,012,370 visits). Both patient and visit volumes decreased in non-expansion states (patients: from 28,950 to 27,699, a 4.3% decrease; visits: from 93,240 to 88,935, a 4.6% decrease; data not shown). Across the two-year study period, patients of CHCs in expansion states had a mean of 5.4 visits per patient versus 4.5 for non-expansion state patients (P<.001, data not shown).
Table 1.
Characteristics of study states and CHCs
| Expansion states | Non-expansion states | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| CA | MN | OH | OR | WA | Expansion states, total |
AK | IN | MT | NC | Non- expansion states, total |
|
| State-level factors | |||||||||||
| Adult Medicaid eligibilitya, pre- (Henry J. Kaiser Family Foundation, 2013a)/post-(Henry J. Kaiser Family Foundation, 2013b) expansion period, % of FPL |
106/138 | 215/205 | 96/138 | 39/138 | 71/138 | - | 78/128 | 24/24 | 54/54 | 47/45 | |
| Minimum wage, 2014, (CNN, 2014) $/hr |
8.00 | 7.25 | 7.95 | 9.10 | 9.32 | - | 7.5 | 7.25 | 7.9 | 7.25 | - |
|
Unemployment rate, 2014, (Bureau of Labor Statistics, 2014) % |
7.6 | 4.6 | 5.5 | 6.9 | 6.1 | - | 6.4 | 5.7 | 4.6 | 6.4 | - |
| Adult uninsured rate, 2013,(Witters, 2014) % |
21.6 | 9.5 | 13.9 | 19.4 | 16.8 | - | 18.9 | 15.3 | 20.7 | 20.4 | - |
| Insurance marketplace (Henry J. Kaiser Family Foundation, 2014) |
State | State | Federal | Stateb | State | - | Federal | Federal | Federal | Federal | - |
| OCHIN CHC characteristics | |||||||||||
| Health systems,No. | 7 | 2 | 3 | 25 | 1 | 38 | 1 | 2 | 1 | 2 | 6 |
| Total CHCs, No. | 44 | 7 | 18 | 123 | 6 | 198 | 1 | 10 | 6 | 4 | 21 |
| Total patients, 2013–2014, No. | 102,536 | 10,394 | 40,655 | 190,376 | 18,324 | 361,811c | 2,632 | 12,700 | 10,990 | 13,896 | 40,216c |
| Female sex, No. (%) | 60,206 (58.7) | 5,777 (55.6) | 22,808 (56.1) | 113,570 (59.7) | 10,853 (59.2) | 212,904 (58.8)d | 1,440 (54.7) | 8,299 (65.3) | 6,494 (59.1) | 8,063 (58.0) | 24,294 (60.4) |
| Age-group, as of last visit, No. (%) | |||||||||||
| 19–25 y | 15,139 (14.8) | 1,738 (16.7) | 7,685 (18.9) | 28,557 (15.0) | 2,850 (15.6) | 55,894 (15.4)d | 417 (15.8) | 1,920 (15.1) | 2,285 (20.8) | 1,728 (12.4) | 6,350 (15.8) |
| 26–39 y | 34,039 (33.2) | 3,947 (38.0) | 13,823 (34.0) | 63,429 (33.3) | 6,033 (32.9) | 121,103 (33.5) | 924 (35.1) | 3,935 (31.0) | 3,218 (29.3) | 3,388 (24.4) | 11,464 (28.5) |
| 40–64 y | 53,358 (52.0) | 4,709 (45.3) | 19,147 (47.1) | 98,390 (51.7) | 9,441 (51.5) | 184,814 (51.1) | 1,291 (49.1) | 6,845 (53.9) | 5,487 (49.9) | 8,780 (63.2) | 22,402 (55.7) |
| Household income, No. (%) | |||||||||||
| ≤138% of FPL | 64,715 (63.1) | 7,572 (72.8) | 33,420 (82.2) | 136,700 (71.8) | 13,965 (76.2) | 255,965 (70.7)d | 955 (36.3) | 9,411 (74.1) | 6,251 (56.9) | 6,922 (49.8) | 23,539 (58.5) |
| >138% of FPL | 13,786 (13.5) | 761 (7.4) | 4,032 (9.9) | 31,859 (1.7) | 4,157 (22.7) | 54,531 (15.1) | 1,253 (47.6) | 1,231 (96.7) | 3,113 (28.3) | 3,271 (23.6) | 8,866 (22.0) |
| Missing/unknown | 24,035 (23.4) | 2,061 (19.8) | 3,203 (7.9) | 21,817 (11.5) | 202 (1.1) | 51,315 (14.2) | 424 (16.1) | 2,058 (16.2) | 1,626 (14.8) | 3,703 (26.6) | 7,811 (19.4) |
| Non-white race, No. (%) | 9,974 (9.7) | 8,075 (77.7) | 21,304 (52.4) | 17,948 (9.4) | 1,332 (7.3) | 58,593 (16.2)d | 784 (29.8) | 6,922 (54.5) | 399 (3.6) | 7,935 (57.1) | 16,040 (39.9) |
| Hispanic ethnicity, No. (%) | 41,627 (40.6) | 187 (1.8) | 5,156 (12.7) | 45,699 (24.0) | 1,853 (10.1) | 94,472 (26.1)d | 257 (9.8) | 1,263 (9.9) | 390 (3.5) | 639 (4.6) | 2,549 (6.3) |
| Urban residence, No. (%) | 98,634 (96.2) | 10,368 (99.7) | 40,628 (99.9) | 180,274 (94.7) | 16,475 (89.9) | 345,960 (95.6)d | 2,594 (98.6) | 12,686 (99.9) | 9,937 (90.4) | 13,190 (94.9) | 38,405 (95.5) |
AK = Alaska; CA = California; CHC = community health center; FPL = federal poverty level; IN = Indiana; MN = Minnesota; MT = Montana; NC = North Carolina; OCHIN = formerly the Oregon Community Health Information Network; OH = Ohio; OR = Oregon; WA = Washington
Eligibility FPL levels may differ between adults with children and without, or those who are working and those who are jobless. The number reported indicates the highest FPL limit for open full Medicaid coverage in a given state among these categories.
Oregon’s state-based exchange uses Federal technology
Expansion group numbers may not sum because an individual can have visits in more than 1 state
Overall percentage differs significantly between expansion states andnon-expansion states by χ2 test (P<.001)
Rates of Medicaid-insured visits increased 46% for total expansion state CHCs post-expansion (post/pre RR=1.46, 95% CI: 1.34–1.60) and 12% in non-expansion state CHCs (RR=1.12, 95% CI: 1.01–1.23). Medicaid visit rates varied by state; expansion states ranged from a non-significant difference in California and Minnesota to a 103% increase in Washington (RR=2.03, 95% CI: 1.35–3.05), while non-expansion states ranged from no significant change in North Carolina and Indiana to a 12% increase in Alaska. Uninsured visit rates were 47% lower in the post-year compared to the pre-year in combined expansion state CHCs (RR=0.53, 95% CI: 0.48–0.59); uninsured rates also dropped in non-expansion state CHCs, but to a lesser degree (RR=0.80, 95% CI: 0.72–0.89). Uninsured visit rates varied by state; expansion states ranged from a non-significant decrease in California to a decrease of 53% in Oregon (RR=0.47, 95% CI: 0.41–0.54). Only one state in this CHC sample saw a significant change in rates of commercially-insured visits: Ohio’s commercial visit rates increased 20% (RR=1.20, 95% CI: 1.08–1.34).
In expansion state CHCs, overall visit rates in the post-expansion year increased by 6%, compared to rates in the pre-expansion year (RR=1.06, 95% CI: 1.02–1.10, Table 2); there was some variation in these rates within the group of expansion states. Overall visit rates remained unchanged across the entire group of CHCs in non-expansion states (RR=0.95, 95% CI: 0.88–1.03), and there were no individual non-expansion states showing an increase in total visit rates.
Table 2.
CHC visit rate ratios by state, post- versus pre-Medicaid expansion
| Expansion states | Non-expansion states | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| CA | MN | OH | OR | WA | Expansion states, total |
AK | IN | MT | NC | Non- expansion states, total |
|
| Adjusteda visit RRs by coverage type, post-expansion period vs pre-expansion periodb | |||||||||||
| Uninsured visits, RR (95% CI) | 0.85 (0.73, 1.00) | 0.57 (0.42, 0.77)c | 0.64 (0.56, 0.72)c | 0.47 (0.41, 0.54)c | 0.55 (0.45, 0.68)c | 0.53 (0.48, 0.59)c | 0.77d | 0.79 (0.63, 1.00) | 0.83 (0.77, 0.89)c | 0.77 (0.62, 0.95)c | 0.80 (0.72, 0.89)c |
| Medicaid visits, RR (95% CI) | 1.07 (0.99, 1.16) | 1.02 (0.89, 1.17) | 1.33 (1.18, 1.50)c | 1.88 (1.67, 2.12)c | 2.03 (1.35, 3.05)c | 1.46 (1.34, 1.60)c | 1.12d | 1.29 (0.97, 1.72) | 1.07 (1.02, 1.13)c | 1.01 (0.89, 1.15) | 1.12 (1.01, 1.23)c |
| Commercially insured visits, RR (95% CI) |
1.14 (0.97, 1.33) | 0.85 (0.71, 1.03) | 1.20 (1.08, 1.34)c | 0.93 (0.81, 1.06) | 0.97 (0.76, 1.24) | 1.00 (0.91, 1.11) | 1.04d | 1.22 (0.96, 1.55) | 1.11 (0.90, 1.37) | 1.03 (0.95, 1.12) | 1.07 (0.98, 1.17) |
| Adjusteda visit RRs by visit type, post-expansion period vs pre-expansion periodb | |||||||||||
| Total visits, RR (95% CI) | 1.04 (0.98, 1.12) | 0.96 (0.87, 1.04) | 1.00 (0.93, 1.07) | 1.07 (1.02, 1.12)c | 1.28 (0.92, 1.79) | 1.06 (1.02, 1.10)c | 0.95d | 0.96 (0.77, 1.19) | 0.96 (0.86, 1.08) | 0.94 (0.83, 1.07) | 0.95 (0.88, 1.03) |
| Primary care office visits, RR (95% CI) |
1.03 (0.96, 1.10) | 1.02 (0.99, 1.06) | 1.01 (0.93, 1.11) | 1.06 (1.01, 1.11)c | 1.39 (0.94, 2.05) | 1.06 (1.02, 1.10)c | 0.91d | 0.96 (0.76, 1.21) | 0.91 (0.80, 1.05) | 0.96 (0.86, 1.07) | 0.94 (0.87, 1.03) |
| New patient visits, RR (95% CI) | 1.01 (0.84, 1.21) | 0.92 (0.90, 0.94)c | 0.99 (0.85, 1.14) | 1.21 (1.07, 1.38)c | 1.69 (1.15, 2.49)c | 1.14 (1.04, 1.25)c | 0.85d | 0.88 (0.63, 1.24) | 1.00 (0.90, 1.11) | 0.84 (0.64, 1.11) | 0.90 (0.75, 1.08) |
| Established patient visits, RR (95% CI) |
1.02 (0.95, 1.09) | 1.01 (0.97, 1.07) | 1.03 (0.94, 1.13) | 1.04 (0.99, 1.09) | 1.35 (0.96, 1.91) | 1.04 (1.00, 1.08) | 0.90d | 0.97 (0.76, 1.23) | 0.94 (0.82, 1.07) | 0.96 (0.88, 1.06) | 0.95 (0.88, 1.03) |
| Preventive visits, RR (95% CI) | 2.93 (1.58, 5.41)c | 1.14 (0.87, 1.50) | 0.81 (0.69, 0.96)c | 1.42 (1.10, 1.82)c | 1.00 (0.67, 1.54) | 1.41 (1.14, 1.73)c | 0.95d | 1.22 (0.89, 1.69) | 1.10 (0.99, 1.21) | 1.04 (0.86, 1.25) | 1.09 (0.99, 1.20) |
| Mental/behavioral health visits, RR (95% CI) |
1.43 (0.97, 2.12) | 0.74 (0.73, 0.76)c | 1.08 (0.98, 1.20) | 1.04 (0.81, 1.34) | 0.94 (0.93, 0.95)c | 1.04 (0.86, 1.25) | 2.00d | 0.78 (0.42, 1.44) | 1.08 (0.92, 1.26) | 1.26 (1.03, 1.55)c | 1.10 (0.96, 1.26) |
| Limited-service visitse, RR (95% CI) |
1.08 (0.94, 1.25) | 1.17 (0.90, 1.53) | 1.15 (1.01, 1.32)c | 1.28 (1.16, 1.41)c | 1.43 (1.00, 2.04) | 1.23 (1.13, 1.33)c | 1.14d | 1.05 (0.73, 1.51) | 1.02 (0.81, 1.28) | 0.97 (0.84, 1.12) | 1.01 (0.91, 1.09 |
AK = Alaska; CA = California; CHC = community health center; CI = confidence interval; FPL = federal poverty level; GEE = generalized estimating equation; IN = Indiana; MN = Minnesota; MT = Montana; NC = North Carolina; OCHIN = formerly the Oregon Community Health Information Network; OH = Ohio; OR = Oregon; RR = rate ratio; WA = Washington
Rates by state: Poisson GEE model adjusted for CHC-level factors (percent female, percent younger than age 40 years, percent nonwhite race, percent Hispanic, percent ≤138% FPL, percent with unknown FPL, percent urban). Rates by expansion status: Poisson GEE model adjusted for all CHC-level factors plus state-level factors (2014 minimum wage, 2014 unemployment rate, 2013 adult uninsurance rate). All GEE models accounted for temporal correlation over time within CHCs.
Pre-expansion period: January 1, 2013 to December 31, 2013; post-expansion period: January 1, 2014 to December 31, 2014.
RR is significantly different from 1.0.
CI cannot be computed because Alaska had only 1 CHC in the sample.
Includes nurse-only, and lab-, imaging-, and immunization-only visits.
Despite some variation between states, utilization of several CHC visit types increased significantly post- versus pre-expansion in the group of expansion state CHCs: new patient [14% (RR=1.14, 95% CI: 1.04–1.25)], primary care [6% (RR=1.06, 95% CI: 1.02–1.10)], preventive care [41% (RR=1.41, 95% CI: 1.14–1.73)], and limited-service [23% (RR=1.23, 95% CI: 1.13, 1.33)], while none of these rates changed significantly in the group of non-expansion state CHCs.
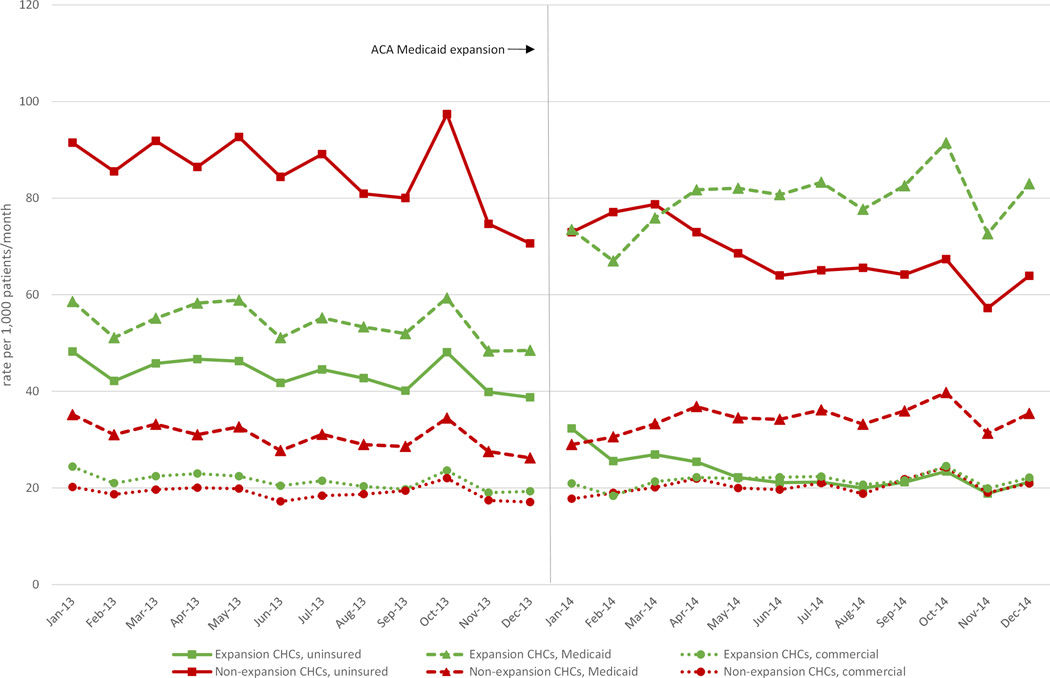
Results of our temporal analysis of coverage status are shown in Figure 1. In the first month post-expansion, Medicaid visit rates increased 52% in the group of expansion state CHCs, or approximately 25 additional Medicaid visits per 1,000 patients per month. Medicaid insured visit rates continued to increase through October, 2014. In the same states, rates of uninsured CHC visits dropped immediately and continued to decline modestly throughout the first six months of the post-expansion period, before leveling off for the remainder of 2014. The group of CHCs in non-expansion states also saw a drop in uninsured visit rates, although it occurred a few months later into the post-expansion year and was smaller in relative scale. Commercially insured visit rates showed a modest increase throughout the post period, particularly in the non-expansion state sample, but this increase was not statistically significant.
Figure 1. Adjusted visit rates by coverage status and month among CHCs in Medicaid expansion and non-expansion states.
Footnote: Rates calculated per 1,000 adult patients across entire study period. GEE Poisson models accounting for temporal correlation within CHCs over time and adjusted for covariates significant at P<.05: percent Hispanic, insurance exchange type, and 2014 minimum wage (uninsured model); percent under age 40, percent non-white race, percent Hispanic, percent ≤138% FPL, and percent with unknown FPL (Medicaid model); percent non-white race, percent Hispanic, percent ≤138% FPL, insurance exchange type, and 2014 minimum wage (commercial model).
Discussion
We used EHR data from a multi-state network of CHCs to measure changes in visit rates by coverage and visit type 12 months before and after ACA health insurance expansions, and compared outcomes in states that expanded Medicaid to those that did not. When taking into account all of the CHCs across the nine states, rates of Medicaid-insured visits increased significantly, while uninsured visit rates declined; these changes were more pronounced among the CHCs in states that expanded Medicaid. The greatest changes in coverage type were seen in the first six months post Medicaid expansion, after which utilization remained relatively stable through the remainder of the year. When assessing changes in overall visit numbers, regardless of payer, CHCs in expansion states saw a modest increase in overall visit rates, while non-expansion states did not.
The most striking pre-post difference in visit type, was in preventive visits: the group of CHCs in expansion states collectively saw a 41% increase in preventive visits, compared to no change in the group of CHCs located in non-expansion states. Expansion state CHCs also saw significant increases in their rates of new patient, primary care, and limited-service visits, while rates of these three visit types remained unchanged in the group of CHCs in non-expansion states. There was variation in the pre-post changes when comparing individual expansion states; however, the expansion states collectively showed increased visit rates overall and changes of larger magnitude than the changes observed in individual non-expansion states, with only a few exceptions. These changes suggest that the ACA’s Medicaid expansions impacted CHCs in several ways. First, the increase in new patient visit rates indicates that patients initiated care at CHCs at which they had not previously been established, likely due to a gain in Medicaid coverage. Second, patients sought and received preventive healthcare services (e.g., preventive visits, immunizations, labs, and imaging) for which they likely were overdue.
These findings are in line with previous studies that found those without insurance received about 50% less healthcare services than insured patients (Hadley, Holahan, Coughlin, & Miller, 2008) and that receipt of preventive services increased for young adults after new insurance coverage opportunities.(Lau, Adams, Park, Boscardin, & Irwin, 2014) The significant increases in new and preventive visit types seen in our study, while overall visit rates rose only modestly, suggest that CHCs in Medicaid expansion states were faced with needing to expand important services and see additional patients post-expansion.
Although millions gained coverage after Medicaid expansions, about 30 million Americans remained uninsured at the end of 2014.(Henry J. Kaiser Family Foundation, 2015a) Of those without insurance, one in ten live below the federal poverty level, but remain uninsured because they live in a state that has not expanded Medicaid.(Henry J. Kaiser Family Foundation, 2015b) CHCs provide recommended healthcare services for vulnerable populations including uninsured, racial/ethnic minority, and rural patients,(National Association of Community Health Centers, 2014) but those in non-expansion states will lack the potential revenue of increased Medicaid-insured visits.(Henry J. Kaiser Family Foundation, 2015b)
Limitations
This study is based on CHCs who are part of the OCHIN network and have a linked EHR; some of the states in our sample are represented by only a few CHCs. Thus, our results may not represent post-Medicaid expansion experiences of all CHCs, states, or expansion status groups. Our analysis is visit-based and does not assess changes in patient-level insurance status or changes in patient panels. We only assessed data from CHC visits in the first 12 months post-expansions; this work provides the foundation for further research that is needed to better understand CHC utilization patterns beyond the first year and to determine the extent of unmet demand for CHCs services (e.g., patients wanting a CHC visit who were unable to obtain CHC visits). We adjusted our multivariable analysis to account for economic differences between expansion and non-expansion states, yet unmeasured confounders could impact our results.
Conclusion
One year after ACA insurance expansions, overall rates of Medicaid-insured CHC visits increased and uninsured visits decreased significantly, with the biggest changes in states that expanded Medicaid. New and preventive visit rates increased in expansion state CHCs suggesting increased demand for CHC services likely among those who gained Medicaid. These results also suggest that expansion state CHCs have increased their capacity to accommodate new patients and provide more preventive care services.
Supplementary Material
Acknowledgements
This work was financially supported by the Patient-Centered Outcomes Research Institute (PCORI) Health Systems Cycle I (2012), the National Cancer Institute (NCI) of the National Institutes of Health, grant number (1 R01 CA181452 01), and the Oregon Health & Science University Department of Family Medicine. We thank the OCHIN practice-based research network (PBRN) and all clinics in the PBRN for making this research possible.
Footnotes
Conflict of Interest: The authors have no conflicts of interest to report.
Contributor Information
Megan J. Hoopes, OCHIN, Inc., 1881 SW Naito Parkway, Portland, OR 97201, hoopesm@ochin.org; phone 503-943-2630; fax 503-943-2501.
Heather Angier, Oregon Health & Science University, Portland, OR.
Rachel Gold, Kaiser Permanente Northwest Center for Health Research, OCHIN, Inc., Portland, OR.
Steffani R. Bailey, Oregon Health & Science University, Portland, OR.
Nathalie Huguet, Oregon Health & Science University, Portland, OR.
Miguel Marino, Oregon Health & Science University, Portland, OR.
Jennifer E. DeVoe, Oregon Health & Science University, OCHIN, Inc., Portland, OR.
References
- Angier H, Hoopes M, Gold R, Bailey S, Cottrell E, Heintzman J, DeVoe JE. An Early Look at Rates of Uninsured Safety Net Clinic Visits After the Affordable Care Act. Ann Fam Med. 2015;13(1):10–16. doi: 10.1370/afm.1741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asplin BR, Rhodes KV, Levy H, Lurie N, Crain AL, Carlin BP, Kellermann AL. Insurance status and access to urgent ambulatory care follow-up appointments. Journal of the American Medical Association. 2005;294(10):1248–1254. doi: 10.1001/jama.294.10.1248. [DOI] [PubMed] [Google Scholar]
- Baicker K, Taubman SL, Allen HL, Bernstein M, Gruber JH, Newhouse JP, Smith J. The Oregon experiment--effects of Medicaid on clinical outcomes. N Engl J Med. 2013;368(18):1713–1722. doi: 10.1056/NEJMsa1212321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bindman AB, Grumbach K, Osmond D, Komaromy M, Vranizan K, Lurie N, Stewart A. Preventable hospitalizations and access to health care. Journal of the American Medical Association. 1995;274(4):305–311. [PubMed] [Google Scholar]
- Bureau of Labor Statistics. Current Unemployment Rates for States and Historical Highs/Lows. [Retrieved May 12, 2015];2014 from http://www.bls.gov/web/laus/lauhsthl.htm.
- Burstin HR, Lipsitz SR, Brennan TA. Socioeconomic status and risk for substandard medical care. Journal of the American Medical Association. 1992;268(17):2383–2387. [PubMed] [Google Scholar]
- CNN. 2014 Minimum Wage, State by State. [Retrieved May 12, 2015];2014 from http://money.cnn.com/interactive/pf/state-minimum-wage/ [Google Scholar]
- DeVoe J, Sears A. OCHIN Community Information Network: Bringing Together Community Health Centers, Information Technology, and Data to Support a Patient-Centered Medical Village. J Am Board Fam Med. 2013;26(3):271–278. doi: 10.3122/jabfm.2013.03.120234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeVoe JE, Gold R, Spofford M, Chauvie S, Muench J, Turner A, Nelson C. Developing a network of community health centers with a common electronic health record: description of the Safety Net West Practice-based Research Network (SNW-PBRN) J Am Board Fam Med. 2011;24(5):597–604. doi: 10.3122/jabfm.2011.05.110052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hadley J, Holahan J, Coughlin T, Miller D. Covering the uninsured in 2008: current costs, sources of payment, and incremental costs. Health Aff (Millwood) 2008;27(5):w399–w415. doi: 10.1377/hlthaff.27.5.w399. [DOI] [PubMed] [Google Scholar]
- Henry J. Kaiser Family Foundation. Medicaid Eligibility for Adults as of January 1, 2014. In: K. C. o. M. a. t. Uninsured, editor. Fact Sheet. Vol. 2014. Menlo Park, C.A.: 2013. [Google Scholar]
- Henry J. Kaiser Family Foundation. State Marketplace Statistics. [Retrieved May 12, 2015];2014 from http://kff.org/health-reform/state-indicator/state-marketplace-statistics/#note-7. [Google Scholar]
- K. C. o. M. a. t. Uninsured, editor. Henry J. Kaiser Family Foundation. Adults who Remained Uninsured at the End of 2014. Menlo Park, C.A.: 2015a. [Google Scholar]
- The Kaiser Commission on Medicaid and the Uninsured, editor. Henry J. Kaiser Family Foundation. The Uninsured: A Primer - Key Facts About Health Insurance and the Uninsured in America. Menlo Park, C.A.: 2015b. [Google Scholar]
- Lau JS, Adams SH, Park MJ, Boscardin WJ, Irwin CE., Jr Improvement in preventive care of young adults after the affordable care act: the affordable care act is helping. JAMA Pediatrics. 2014;168(112):1101–1106. doi: 10.1001/jamapediatrics.2014.1691. [DOI] [PubMed] [Google Scholar]
- McCormick D, Sayah A, Lokko H, Woolhandler S, Nardin R. Access to care after Massachusetts' health care reform: a safety net hospital patient survey. J Gen Intern Med. 2012;27(11):1548–1554. doi: 10.1007/s11606-012-2173-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan D. Health centers for poor, uninsured see ranks swell. [Retrieved January 15, 2015];2012 from http://www.reuters.com/article/2012/05/01/us-usa-healthcare-centers-idUSBRE8401JL20120501?feedType=RSS&feedName=everything&virtualBrandChannel=11563. [Google Scholar]
- National Association of Community Health Centers. Chart Book, 2014. Bethesda, M.D.: 2014. A Sketch Of Community Health Centers. [Google Scholar]
- Rice T, Unruh LY, Rosenau P, Barnes AJ, Saltman RB, van Ginneken E. Challenges facing the United States of America in implementing universal coverage. Bull World Health Organ. 2014;92(12):894–902. doi: 10.2471/BLT.14.141762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smolderen KG, Spertus JA, Nallamothu BK, Krumholz HM, Tang F, Ross JS, Chan PS. Health care insurance, financial concerns in accessing care, and delays to hospital presentation in acute myocardial infarction. Journal of the American Medical Association. 2010;303(14):1392–1400. doi: 10.1001/jama.2010.409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sommers BD, Baicker K, Epstein AM. Mortality and access to care among adults after state Medicaid expansions. N Engl J Med. 2012;367(11):1025–1034. doi: 10.1056/NEJMsa1202099. [DOI] [PubMed] [Google Scholar]
- Supreme Court of the United States. National Federation of Independent Business v Sebelius. [Retrieved January 15, 2015];2012 from http://www.supremecourt.gov/opinions/11pdf/11-393c3a2.pdf.
- T. K. C. o. M. a. t. Uninsured, editor. The Henry J Kaiser Family Foundation. Recent Trends in Medicaid and CHIP Enrollment as of January 2015: Early Findings from the CMS Performance Indicator Project. Menlo Park, CA: 2015. [Google Scholar]
- The White House. The Obama Administration and Community Health Centers. 2012 from http://www.whitehouse.gov/sites/default/files/05-01-12_community_health_center_report.pdf.
- Witters D. Highest Uninsured States Less Likely to Embrace Health Law. [Retrieved May 12, 2015];2014 from http://www.gallup.com/poll/167321/highest-uninsured-states-less-likely-embrace-health-law.aspx. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.