Abstract
Family meals are associated with a range of positive outcomes among children and adolescents. There is inconsistency, however, in the way in which studies have defined and measured family meals. Therefore, a systematic review of the literature was conducted to determine how studies describe family meals with the use of structural characteristics. The current review focused on studies in the United States that included children ages 2–18 y. A total of 33 studies were identified that characterized family meals with the use of ≥1 of the following structural features: frequency or mean number of family meals per week, length of family meal, people present at meal, and where meals occurred. No study characterized family meals by using all 4 family meal features, whereas most studies (81%) characterized family meals by using frequency or mean number of meals per week. Findings not only provide an initial understanding of the structural features used to define family meals but also point to the importance of developing a more comprehensive, sensitive assessment that can accurately capture the complex and multidimensional nature of family meals.
Keywords: family meal, systematic review, characteristics, child, adolescent
Introduction
Increasing the frequency of family meals has been recommended for weight management in children (1) because more frequent family meals have been associated with improved nutrient intake (2, 3), lower rates of disordered eating (4), as well as lower odds of overweight and obesity (2, 5). Although family meals are frequently recommended, the family meal literature has yet to develop a standard definition of a “family meal” in terms of where meals should take place, who should be present, or how long meals should last to yield the greatest benefit. Instead, research has focused on the frequency of family meals, which are defined inconsistently across studies, such as “most or all family members sharing a meal together” (5) or having “at least 1 parent present” when a child eats (2). The inconsistency and lack of specificity in defining family meals make it difficult to interpret findings across studies and make clear recommendations to families.
Because family meals are activities that include parents and children, to make clear recommendations around family meals it is important to consider family structure (e.g., single-parent household, siblings) as well as a child’s developmental stage. Data suggest that parental modeling of eating behaviors in the preschool years plays an important role in establishing long-term eating behaviors, whereas adolescence is associated with more autonomy and an inclusion of additional factors influencing eating behavior, such as peers, the school environment, and increased exposure to media (6). The mechanism through which family meals affect child and adolescent health may be different for preschoolers (e.g., parental modeling) and adolescents (e.g., parent-adolescent communication); thus, it is important for family meal recommendations to take these developmental stage differences into account.
Historical shifts in family structure, such as a higher percentage of mothers entering the workforce (6, 7) and increases in after-school and weekend activities in which children are involved, are often cited as barriers to sharing a family meal (8). These shifts have resulted in changes in meals and eating behavior for families, such as child care providers being responsible for meals as well as families eating “on the go” or going out to eat more often (6). To provide the best recommendations to families, we need a better understanding of how these shifts in family structure are affecting the structural elements of family meals.
Systematic reviews of family meals have previously focused on the relation between family meals and nutrition and/or weight outcomes (2, 5, 9, 10), with 1 review focusing on intervention strategies that promote family meals (11). Across all of these reviews, measurement variation and inconsistency in defining family meals are continually noted as limitations. This measurement variation stems from the lack of research examining what specific components of family meals are important for promoting child and adolescent health. Identifying how the literature has characterized the family meal environment is an important first step in understanding the mechanism(s) underlying the relation between family meals and health.
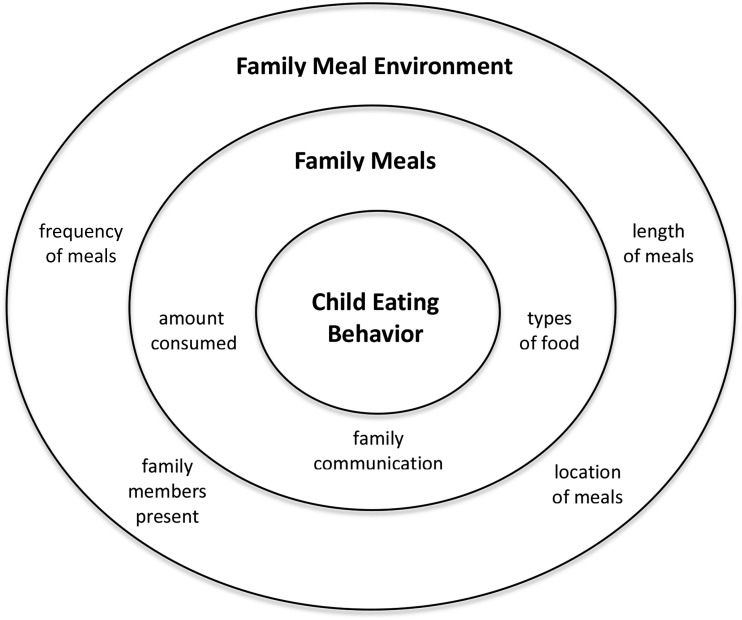
According to a socioecological framework of eating behavior, the eating environment (i.e., structural characteristics) can affect how much is eaten at meals, what kind of food is served, and family communication, which could all contribute to health (12) (Figure 1). Therefore, the purpose of this review is to examine how the family meal environment has been characterized in the existing literature as an initial step in developing specific recommendations for families on how to structure family meals to positively affect health. This fills a gap in the literature because, to our knowledge, the family meal eating environment has yet to be systematically reviewed or synthesized.
FIGURE 1.
Proposed socioecological framework for the family meal environment of child eating behavior.
Grounded in socioecological theory, the structural characteristics of the environment identified as related to child health (12), as well as easily measured, manipulated, and replicated in future studies, were chosen as search terms (i.e., frequency of meals, length of meals, location, and family members present). A systematic literature search was conducted to extract the structural features of the family meal environment (frequency, length, location, and/or family members present) in studies based in the United States that included family meals. Because child developmental stage has been shown to influence eating patterns, this review organized the findings into 3 developmental periods (i.e., early childhood, middle childhood, and adolescence).
Methods
Study criteria.
Studies conducted in the United States with quantitative primary data collection on the structural aspects of the family meal environment (frequency, length, location, and/or family members present) were eligible for this review. Only studies conducted in the United States were included because the structural components related to the family meal environment may differ in countries other than the United States. At the national level, family meals are promoted in the United States and recommendations are provided by the American Academy of Pediatrics on how to structure family meals, such as eating family meals ≥5 times/wk and eating at a table (1). Other countries, even those that are English-speaking, do not have specific recommendations for family meals that align with those in the United States. Findings, therefore, from studies outside the United States are not included in the current review because examining these cultural differences is not within the scope of this article. The inclusion criteria for study selection included the following: the target population of families with children aged 2–18 y, written in English, and primary data collection published through December 2014. Exclusion criteria included investigations focused on children with a medical condition that may affect eating or who have medication requirements that may alter eating (e.g., diabetes) and feeding studies or programs in which food was provided to children outside the home environment (e.g., Head Start), because the nature of these studies may not be a good indication of the natural characteristics in the home environment. No minimum sample size was required for a study to be included in the review.
Search strategy.
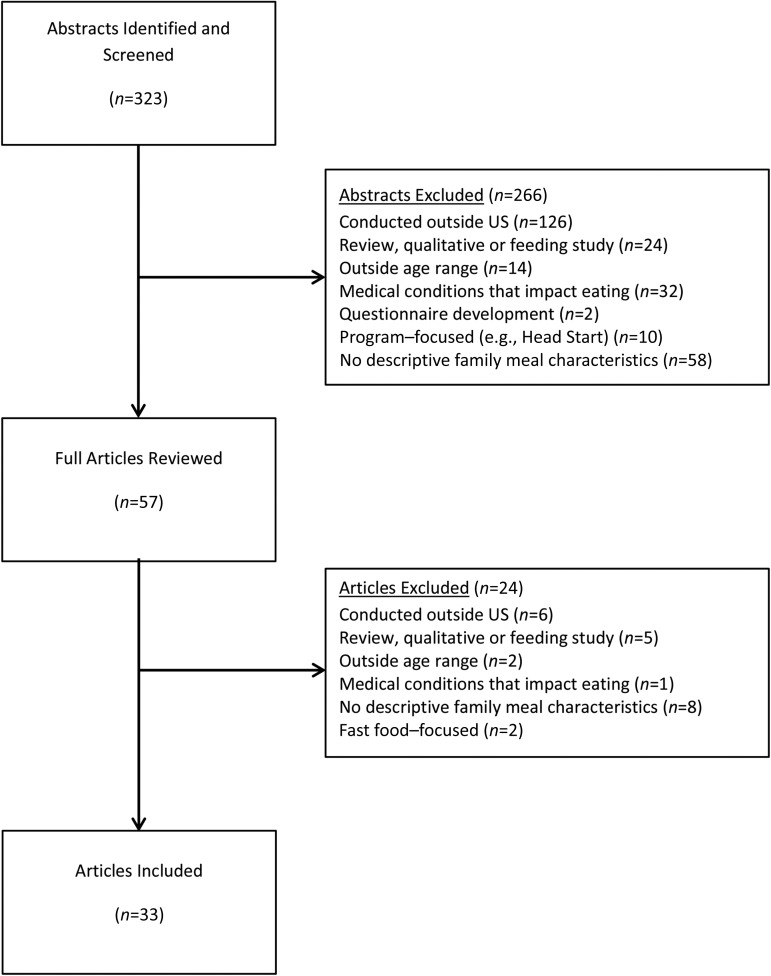
A comprehensive search was conducted in January 2015 by using Medical Subject Headings (MeSH) in PubMed and in January 2016 for search terms in PsycINFO. MeSH and search terms included “child behavior,” “adolescent behavior,” “feeding behavior,” “family relations,” “nuclear family,” and “meals.” Eating is classified as a behavior; thus, behavior was used as a MeSH term to capture eating. Search terms that may be limiting (e.g., overweight) were not included to allow for a more expansive search to fully capture how family meals have been broadly described in the literature. Two independent reviewers (MBM and SMR) screened abstracts of all studies identified by the PubMed and PsycINFO searches to determine potentially relevant studies. Studies excluded in the initial step of screening of abstracts included the following: those conducted outside the United States or outside the age range, reviews, qualitative or feeding investigations, children with medical conditions that affect eating, questionnaire development, program-focused (e.g., Head Start), or those with no information included about structural descriptive characteristics (Figure 2). On the basis of reviewer consensus, articles were selected for full review. Full articles that met all of the inclusion criteria, as agreed upon by both reviewers, were included in the review and select characteristics, determined a priori (see variable categories in Table 1), were extracted independently and confirmed by comparison.
FIGURE 2.
CONSORT (Consolidated Standards of Reporting Trials) diagram of the family meal systematic review.
TABLE 1.
Structural characteristics of family meals by developmental period1
| Characteristics of FM |
||||||||||
| Authors, year (ref) | Sample size, n | Study design, data source | Participant characteristics | FM F, n/wk | Length, min | Location | Who is present | Methodology used to assess FM | Outcome measures | Main findings |
| Early childhood: ages 2–5 y | ||||||||||
| Haines et al., 2013 (30) | 121 | 6-mo RCT; Healthy Habits, Healthy Homes | 4.1 ± 1.12 y, 52.3% female; 33.3% black, 51.4% Hispanic, 15.3% other; BMI %iles: 53.7% <85th, 26.9% ≥85th and <95th, 19.4% ≥95th | 6.3 ± 2.0 | — | — | — | Questionnaire: “How many days did at least some of the family eat a meal together in the past 7 days?” | FMF; child‘s sleep duration; child‘s TV viewing time; presence of TV in child‘s room | No intervention effect for FMF, overall TV viewing time, or TV in child‘s bedroom. Sleep ↑ for families in intervention group, whereas sleep ↓ for control group |
| Goulding et al., 2014 (41) | 295 (parent-child dyads) | Cross-sectional and observational | 5.9 ± 0.6 y, 48% female | — | — | 82% of children always eat at table | 60% of mothers always eat with child | Observation: video-recorded 3 typical dinnertime meals over the course of 1 wk | Maternal depressive symptoms; maternal feeding practices | Mothers with ↑ depressive symptoms reported more pressuring of child to eat and more demandingness; less authority in child-feeding, and less likely to eat with child |
| Kong et al., 2013 (13) | 30 (parent-child dyads) | Cross-sectional and observational | 4.5 ± 0.05 y; 33.3% white, 33.3% black, 33.3% Hispanic; BMI %ile: 44.8% ≥ 85th | — | White, 17.8; black, 18.9; Hispanic, 23.3 | — | White: 1.0 adult, 3 children; black: 1.0 adult, 1.5 children; Hispanic: 1.0 adult, 3 children | Observation: video-recorded family dinners; did not specify how many dinners recorded | Parent-child mealtime interactions; mealtime characteristics | Black families spent significantly more time in behaviors that diverted their attention from eating compared with white and Hispanic families |
| Taveras et al., 2012 (29) | 1213 | 6-mo RCT; Healthy Habits, Healthy Homes | 4.0 ± 1.1 y, 53% female; 34% black/African-American, 52% Hispanic, 14% white/other; BMI %iles 47% ≥85th and <95th, 20% ≥95th | 6.2 ± 2.1, 64% ≥7 | — | — | — | Questionnaire: “How many days did at least some of the family eat a meal together in a typical week?” | Household routines (e.g., family meals, sleep, screen time) and parenting strategies that are preventive of overweight and obesity | 45% of parents reported child watched TV ≥1 d/wk while eating. 50% of children slept <11 h/d; children had 3.8 ± 2.7 h/d of screen time (TV, video, computer) |
| Turer et al., 2013 (31) | 400 (parent-child dyads)3 | Cross-sectional; Kids and Adults Now: Defeat Obesity! | 3.5 ± 1.1 y, 44% female; 75% non-Latino white, 22% African-American, 3% other; BMI %iles: 24% ≥85th, 75% <85th | 2% 0, 9% 1–2, 17% 3–4, 24% 5–6, 49% ≥7 | — | — | — | Questionnaire: “During the past 7 days, how many times did all, or most of your family living in your house, eat a meal together?" | Determine if child and mother meet the AAP-recommended behavioral goals for obesity prevention | 16% of children and 12.5% of mothers reported ≥5 servings fruit and vegetables/d; 50% of children and 12.5% of mothers had ≤2 h/d of screen time; children and adults did not meet exercise guidelines; 41% of children and 35% of mothers ate fast-food meals <1 time/wk |
| Middle childhood: ages 6–11 y | ||||||||||
| Berge et al., 2014 (18) | 120 (children and parent dyads) | Cross-sectional; Family Meals LIVE! | 8.9 ± 3.3 y, 47% female; 18% white, 74% black, 9% Indian, 6% Asian, 3% mixed or other; BMI %ile: 50% ≥85th | 15.7 ± 0.9 | 72% kitchen or dining room, 20% family room, 8% office or bedroom | 85% mother, 34% father/stepfather, 53% sister, 39% brother | Observation: video-recorded family meals for 8 d | Parent- and family-level interpersonal and food-related dynamics (e.g., communication, food control) | Positive family- and parent-level interpersonal dynamics at FMs (e.g., warmth) associated with ↓ risk of child obesity | |
| Fulkerson et al., 2008 (42) | 107 (parents of 8–10-y-olds) | Cross-sectional surveys | Mean age: 43.5 y, 86% mothers, 96% white | Breakfast: 13.1% 0, 43.0% 1–2, 9.3% 3–4, 16.8% 5–6, 17.8% 7; dinner: 0% 0, 1.9% 1–2, 16.8% 3–4, 45.8% 5–6, 35.5% 7 | — | — | ≥1 parent present: 0% never, <1% 1–2 FMs/wk, <1% 3–4 FMs/wk, 16.8% 5–6 FMs/wk, 81.3% 7 FMs/wk | Questionnaire: “How many times did all, or most, of your family living in your home eat dinner or supper/breakfast together?” “Was at least 1 parent present when your child ate his/her evening meal?” | Parent perceptions of mealtime environment in families with school-aged children | Parents reported conversations and togetherness as biggest benefits of FM; barriers: planning and preparing meals; 4.7% of parents reported persistent parent-child conflict during most dinners |
| Fulkerson et al., 2011 (43) | 27 (parents of 8–10-y-olds) | Cross-sectional | 43.1 ± 8.3 y, 81% mothers; 81% white, 7% black, 4% Asian, 8% other | Breakfast: 27% 0, 42% 1–2, 12% 3–4, 15% 5–6, 4% 7; dinner: 0% 0, 22% 1–2, 37% 3–4, 26% 5–6, 15% 7 | — | — | Dinner: 1 parent present: 0% never, 7% 1–2 FMs/wk, 11% 3–4 FMs/wk, 7% 5–6 FMs/wk, 74% 7 FMs/wk | Questionnaire: “How frequently did you or most of your family eat dinner/breakfast together?” | FMF (breakfast and dinner); specific foods served | >50% of parents reported eating FMs (dinner) ≥3 times in the past week; 25% reported never eating FMs (breakfast) |
| Gingold et al., 2013 (14) | 64,076 | Cross-sectional; National Survey of Children‘s Health | 6–17 y, 48.9% female; 57.6% non-Hispanic white, 14.9% non-Hispanic black, 19.2% Hispanic, 3.8% non-Hispanic multiracial, 4.6% non-Hispanic other | 25.6% 0–3, 74.4% 4–7 | — | — | — | Questionnaire: “During the past week, on how many days did all the family members who live in the household eat a meal together?” | Screen-based leisure activity; regular nonscreen activities (e.g., physical activity, FM) | >50% of US youth have TV in their bedroom and 14% have no rules about content; odds of screen time (≥2 h/d) significantly ↑ in households without TV rules; youth with FMs ≤3 times/wk had ↑ odds of screen time of >2 h/d than families with FMs ≥4 times/wk |
| Miller et al., 2012 (32) | 21,400 | Longitudinal; Early Childhood Longitudinal Survey–Kindergarten Cohort | 6.09 ± 0.37 y,4 49% female; 55% white; 15% black; 18% Hispanic; 2% Native American; 10% Asian, Pacific Islander, or other | Breakfast: 4.26 ± 2.46 (kindergarten): 4.43 ± 2.42 (first grade); 4.11 ± 2.42 (third grade); 3.56 ± 2.42 (fifth grade); 3.22 ± 2.29 (eighth grade); dinner: 5.75 ± 1.76 (kindergarten); 5.75 ± 1.73 (first grade); 5.68 ± 1.71 (third grade); 5.46 ± 1.77 (fifth grade); 5.25 ± 1.72 (eighth grade) | — | — | — | Questionnaire: “During the past 7 days, how many times did all or most of your family eat a meal together?” | Child academic and behavioral outcomes (e.g., internalizing and externalizing behaviors) | No significant relations between FMF (breakfast or dinner) and academic or behavioral outcomes |
| Sisson et al., 2011 (25) | 48,687 | Cross-sectional; US National Survey of Children‘s Health | 11.5 ± 8.8 y, 48.9% female; 63.9% non-Hispanic white, 15.4% non-Hispanic black, 11.7% Hispanic, 9% other | 3.9% 0, 21.7% 1–3, 37% 4–6, 37.4% 7 | — | — | — | Questionnaire: “During the past week, on how many days did all the family members who live in the household eat a meal together?” | Demographic factors associated with TV in the bedroom; impact of TV in the bedroom on community involvement, social skills, health habits, and family | 49.3% of youth have a TV in their bedroom; TV in bedroom associated with ↑ odds of problematic social behavior, ↓ odds of having FMs ≥4 d/wk; ↓ engagement in school activities, participation in extracurricular activities, and not getting enough sleep ≥4 d/wk |
| Adolescence: ages 12–18 y | ||||||||||
| Berge et al. 2010 (34) | 4746 | Cross-sectional and longitudinal; Project EAT–I and EAT–II | Middle school: 12.8 ± 0.8 y; high school: 15.8 ± 0.8 y; overall4: 49.8% female; 48.5% white, 19% African-American, 5.8% Hispanic, 3.5% Native American, 19.2% Asian, 3.9% mixed/other | Estimated least squares of regression mean ages: middle school males: 4.4; females: 4.6; high school males: 3.5; females: 3.2 | — | — | — | Questionnaire: “During the past 7 days, how many times did all, or most, of your family living in your house eat a meal together?” | Maternal and paternal parenting style (authoritative, authoritarian, permissive, neglectful); FMF | Authoritative parenting style associated with ↑ FMF. Authoritative parenting predicted ↑ FMF 5 y later for opposite sex parent/child dyads |
| Bauer et al., 2011 (35) | 250 (parent-child dyads) | Cross-sectional; New Moves school-based intervention | Mean age: 15.7 y (range: 12–20.3 y), 100% female; 30% white, 26% black, 11% Hispanic, 24% Asian, 10% mixed/other | 4.64 | — | — | — | Questionnaire: “During the past 7 days, how many times did all, or most, of your family living in your house eat a meal together?” | Family environment (e.g., parental modeling of physical activity, soft-drink consumption) | Higher parent education associated with ↑ FMF. Parents of foreign-born girls reported having ↓ TVs,↓ fast-food and ↑FMF |
| Berge et al., 2013 (19) | 40 (parent-child dyads) | Cross-sectional; Family Meals LIVE! | 14.4 ± 2.0 y, 57.5% female; 35% white, 45% black, 10% Latino, 5% Asian, 2% American Indian, 3% mixed | — | 19 ± 7.3 | 62% kitchen or dining room, 38% family room, bedroom, or office | 1.6 ± 0.74 parents at each meal; 83% mother, 38% father; 2.6 ± 1.2 children at each meal | Observation: 2 family meals video-recorded 1 wk apart. | Mealtime characteristics; interpersonal dynamics (e.g., communication, affect); adolescent BMI; dietary intake | Positive interpersonal dynamics at FMs significantly positively associated with ↓ adolescent BMI and ↑ vegetable intake |
| Berge et al., 2013 (15) | 2793 | Cross-sectional; Project EAT 2010 | 14.4 ± 2.0 y, 53.2% female; 18.8% white, 28.9% black, 16.9% Hispanic, 3.7% Native American, 19.9% Asian, 11.8% mixed/other | Females: 3.8 ± 2.6; males: 4.0 ± 2.6 | — | — | — | Questionnaire: “During the past 7 days, how many times did all, or most, of your family living in your house eat a meal together?” | Family functioning; BMI; FMF; dietary intake; physical activity | Higher family functioning associated with positive health outcomes (e.g., ↓ BMI, ↓ sedentary behavior, ↑ FMF, and ↑ breakfast intake) |
| Eisenberg et al., 2004 (24) | 4746 | Cross-sectional; Project EAT | Mean age: 14.9 y, 55% female; 48.5% white, 19.0% African-American, 5.8% Hispanic, 3.5% Native American, 19.2% Asian American, 4.0% mixed/other | 14.0% 0, 19.1% 1–2, 21.5% 3–4, 18.6% 5–6, 8.8% 7, 18.0% >7 | — | — | — | Questionnaire: “During the past 7 days, how many times did all or most of your family living in your house eat a meal together?” | Associations between FMF and indicators of adolescent health and well-being (substance use, academic performance, self-esteem, depressive symptoms) | Adolescents who had ↑ FMF had significantly ↓ odds of substance use, ↓ GPA, ↓ depressive symptoms, and ↓ suicidal ideation |
| Eisenberg et al., 2008 (22) | 806 | Longitudinal; Project EAT–II | Mean age: 17.2 y (range: 15–18 y), 54.6% female; 47% white, 16.3% African-American, 6.4% Hispanic, 3.7% Native American, 22.9% Asian, 3.8% mixed | Females: 61.2% ≥5; males: 59.5% ≥5 | — | — | — | Questionnaire: “During the past 7 days, how many times did all or most of your family living in your house eat a meal together?” | FMF over 5 y; initiation of substance use during the transition from middle to high school | In females who reported ≥5 FMs/wk, odds of cigarette smoking, alcohol use, and marijuana use 5 y later were approximately half the odds for females who reported <5 FMs/wk; no significant findings for males |
| Eisenberg et al., 2009 (23) | 806 | Cross-sectional; Project EAT–II | Mean age: 17.2 y (range: 15–18 y), 54.6% female; 47% white, 16.3% African-American, 6.4% Hispanic, 3.7% Native American, 22.9% Asian, 3.8% mixed/other | 43.8% <3, 56.1% ≥3 | — | — | — | Questionnaire: “During the past 7 days, how many times did all, or most, of your family living in your house eat a meal together?” | TV viewing during family meals and its relation to substance abuse | Of families who reported regular FMs (≥3 times/wk), 28.6% have meals without TV and 27.5% reported meals with TV; ↓ substance use in females reporting regular FMs vs. no regular FMs |
| Elgar et al., 2014 (20) | 18,834 | Cross-sectional and observational | 15.0 ± 1.7 y, 50.7% female; 70% white, 7.6% black, 6.6% Hispanic, 7.0% mixed, 8.8% Asian/Native American/Middle-Eastern/other | 4.4 ± 2.3 | — | — | — | Questionnaire: “In an average week, how many days do you eat evening meals with your family (0 to 7)?” | Internalizing and externalizing mental health problems; substance use; exposure to cyberbullying | Cyberbullying frequency related to internalizing, externalizing, and substance use; victimization related more closely to rates of problems in adolescents with ↓ FM |
| Fulkerson et al., 2006 (28) | 902 | Cross-sectional; Project EAT–I (subset) | 7th–12th-graders: 47% female; 29% white, 24% African-American, 14% Hispanic, 21% Asian American, 12% other | Adolescents: 13.7% 0, 18.7% 1–2, 20.3% 3–4, 17.8% 5–6, 9.9% 7, 19.6% >7; parents: 6.8% 0, 17.8% 1–2, 18.4% 3–4, 16.5% 5–6, 22% 7, 18.5% >7 | — | — | — | Questionnaire: “During the past 7 days, how many times did all, or most, of your family living in your house eat a meal together?” | Family meal environment as perceived by adolescents and their parents | Parents significantly more likely than youth to report eating ≥5 FMs/wk; youth and parents reported FMs as important and enjoyable; parents more likely to report barriers (e.g., time) to FMs; youth more likely to watch TV at dinner |
| Fulkerson et al., 2006 (39) | 99,462 | Cross-sectional surveys | 6th–12th-graders: 49.8% female; 86% white, <2% African-American, 4% Latino, <2% American Indian, 2% Asian-Pacific Islander, 5% multiracial | Dinner: 20.5% 0–1, 34.7% 2–4, 44.8% 5–7 | — | — | — | Questionnaire: “In an average week, how many times do all of the people in your family who live with you eat dinner together?” | Association of FMF with developmental assets and high-risk behaviors | Prevalence of external (e.g., family support) and internal assets (e.g., engagement in school) ↑ linearly with FMF (dinners); high-risk behaviors inversely associated with FMF (dinners) |
| Fulkerson et al., 2008 (38) | 2516 | Longitudinal; Project EAT–I and EAT–II | 14.9 ± 1.7,4 55.1% female; 48.4% white, 18.7% African-American, 5.8% Latino, 3.6% Native American, 19.2% Asian, 4.3% mixed/other | 13.5% 0, 20.0% 1–2, 66.5% ≥34 | — | — | — | Questionnaire: “During the past 7 days, how many times did all, or most, of your family living in your house eat a meal together?” | Associations between FMF and overweight status over a 5-y period | FMF at time 1 was not associated with overweight status at time 2 in males or females or in the middle or high school cohort |
| Fulkerson et al., 2009 (40) | 145 | Cross-sectional; Team Controlling Overweight and Obesity for Life Study | 17.2 ± 1.2 y, 49% female; 40% white, 31% black, 29% Hispanic/other | 26% 0, 24% 1–4, 50% 5–7 | — | — | — | Questionnaire: ‘‘During the past week, how many days did all, or most of the people you live with eat dinner together?’’ | Dietary practices; healthy and unhealthy weight management; depressive symptoms; substance use; FMF (dinners) | FMF (dinners) positively associated with breakfast consumption and fruit intake and inversely associated with depressive symptoms; adolescents who did not eat FMs (dinners) more likely to be overweight and food insecure than those who ate FMs 5–7 times/wk |
| Hoffmann and Warnick, 2013 (21) | 5419 | Cross-sectional; National Longitudinal Study of Youth | 13 ± 0.015 y, 49% female; 71% white, 15% African-American, 13% Hispanic, 1% mixed race | 5.19 ± 0.035; 14% 0–2, 30% 3–5, 56% 6–7 | — | — | — | Questionnaire: “In a typical week, how many days from 0 to 7 do you eat dinner with your family?” | Alcohol, cigarette, and marijuana use; FMF (dinner) | FMF (dinners) negatively correlated with marijuana frequency |
| Larson et al., 2013 (33) | 2793 | Cross-sectional; Project EAT 2010 | 14.4 ± 2.0 y, 53.2% female; 18.9% white, 29% African-American, 16.9% Hispanic, 3.7% Native American, 19.9% Asian, 11.6% mixed/other | Breakfast: 1.5 ± 2.1; 53% 0, 26.2% 1–2,12.9% 3–6, 7.9% 7; dinner: 4.1 ± 2.6; 14.4% 0, 17.8% 1–2, 35.9% 3–6, 31.9% 7 | — | — | — | Questionnaire: “During the past 7 days, how many times did all, or most, of your family living in your house eat breakfast/dinner together?” | FMF (breakfast and dinner); dietary intake; weight status; family functioning; cohesion | FMF (breakfast) positively associated with being male, ethnic minority, younger age, 2-parent house, better diet quality, and ↓ risk of overweight |
| Neumark-Sztainer et al., 2008 (4) | 2516 | Longitudinal; Project EAT–I and EAT–II | Middle school: 12.8 ± 0.8 y; high school: 15.8 ± 0.8 y; overall4: 49.8% female; 48.5% white, 19% African-American, 5.8% Hispanic, 3.5% Native American, 19.2% Asian, 3.9% mixed/other | Females4: 56% <5, 44% ≥5; males4: 54% <5, 46% ≥5 | — | — | — | Questionnaire: “During the past 7 days, how many times did all, or most, of your family living in your house eat a meal together?” | FMF; disordered eating behaviors; binge-eating with loss of control; chronic dieting | Among girls, regular FMs (≥5/wk) associated with ↓ prevalence of extreme weight-control behaviors 5 y later; no association among boys |
| Neumark-Sztainer et al., 2013 (37) | 30724 | Repeated cross-sectional; Project EAT–I and Project EAT 2010 | 14.6 ± 1.8 y,4 53.3% female; 19.1% white, 28.8% black, 16.7% Hispanic, 3.6% Native American, 20% Asian, 11.8% mixed/other | Mean: 4.034 | — | — | — | Questionnaire: “During the past 7 days, how many times did all, or most, of your family living in your house eat a meal together?” | FMF characterized in 1999 and 2010 | Overall, FMF remained constant from 1999 to 2010; FMF decreased among girls, Asian girls, and youth from lower SES backgrounds |
| Offer, 2013 (26) | 237 (parent-child dyads) | Cross-sectional; 500 Family Study | 15.3 ± 1.6 y, 59.5% female | 2.9 ± 3.5 | 27.8 | — | 39% 2 parents, 36.6%, mother only, 19.9% father only | Self-report: ESM was used; adolescents self-reported what activity they were engaged in when signaled such as “Are you eating a meal right now?” and “Who are you eating with?” adolescents were asked to identify what they were doing 56 times | FMF; family mealtime communication; adolescents’ emotional well-being (e.g., stress) | Family mealtime communication was high when both parents were present at meals; mealtime communication significantly associated with ↑ positive affect and engagement and ↓ negative affect and stress |
| Poulos et al., 2014 (27) | 2895 | Cross-sectional; Central Texas Coordinated Approach to Child Health | Mean age: 13.9 y, 51.6% female; 24.5% white, 13.0% African-American, 52.7% Hispanic, 9.8% other | 4.2 ± 2.8; 35% ≤2, 35% 3–6, 31% ≥7 | — | — | — | Questionnaire: “How many times in the past 7 days did all or most of the family eat a meal together?” | Relation between FMF and parental encouragement of healthy eating | FMF significantly associated with encouragement of healthy eating; ↑ FMF associated with ↑ amount of encouragement |
| Sen, 2010 (44) | 13,558 | Cross-sectional; National Longitudinal Survey of Youth | Females: 14.7 ± 1.4 y; 54% white, 25% black, 21% Hispanic; males: 14.7 ± 1.4 y; 56% white, 24% black, 20% Hispanic | Females: 9% 0, 5% 1, 8% 2, 10% 3, 10% 4, 17% 5, 10% 6, 30% 7; males: 8% 0, 3% 1, 6% 2, 8% 3, 9% 4, 17% 5, 12% 6, 35% 7 | — | — | — | Questionnaire: “How many days in a typical week did your family eat dinner together?” | — | FMF was negatively associated with substance use and running away for females; drinking, physical violence, property destruction, stealing, and running away for males |
| Stewart and Menning, 2009 (36) | 15,537–15,576 | Cross-sectional; National Longitudinal Study of Adolescent Health | Mean age: 16 y, ∼50% female; 57% white, 17% black, 12% Latino/a, 3% Native American, 4% Asian, 7% other | 4.6 ± 0.67 | — | — | — | Questionnaire: “How many days in the past week at least 1 parent was in the room with them when they ate their evening meal?” | Eating patterns of children in nontraditional families | Compared with 2-parent households, youth in 1-parent households ate significantly fewer fruit and vegetables and parents were less likely to be at FMs, except for father-stepmother households |
| Welsh et al., 2011 (16) | 753 | Cross-sectional; baseline data from a 12-mo community-based household weight-gain prevention trial | 12–17 y; BMI %ile: 37% >85th | 5.0 ± 4.4 | — | — | — | Questionnaire: “During the past 7 days, how many times did all or most of your household eat a meal together?” | FMF; family cohesion; individual dietary intake | FMF negatively associated with sweets and sugar-sweetened beverages; these relations were not significant when adjusting for family cohesion |
| Videon and Manning, 2003 (17) | 18,177 | Cross-sectional; National Longitudinal Study of Adolescent Health | 15.9 y, 49% female; 65.9% white, 16.1% black, 12.1% Hispanic, 2.0% Native American, 3.9% Asian | 30.9% ≤3, 20.8% 4–5, 48.3% 6–7 | — | — | — | Questionnaire: “How many times was at least 1 parent present when they ate their evening meal in the past 7 days?” | Parental influence, body weight perceptions, and sociodemographic characteristics on adolescent dietary intake (fruit, vegetables, dairy foods, breakfast) | FMF (dinner) with a parent present significantly associated with ↓ odds of skipping breakfast and poor vegetable, fruit, and dairy consumption; higher parent education associated with ↓ odds of poor vegetable, fruit, and dairy consumption |
AAP, American Academy of Pediatrics; ESM, Experience Sampling Method; FM, family meal; FMF, family meal frequency; GPA, grade point average; Project EAT, Project Eating Among Teens; RCT, randomized controlled trial; ref, reference; SES, socioeconomic status; TV, television; —, data for that category was not reported in the paper; %ile, percentile; ↑, increased; ↓, decreased.
Values are expressed as means ± SDs.
While parent and child demographic information were both included in the referenced articles, only data from the youth sample is presented in this table due to space constraints. Please refer to the individual studies for more information on the parent sample.
Baseline measurement.
Values are expressed as means ± SEs.
Results
The search strategy resulted in 323 records that were screened, and 57 of these abstracts were selected for full-text review. Of these, 24 were excluded; 33 articles met all study inclusion and exclusion criteria and were selected for inclusion in this systematic review (Figure 2). Of the 33 studies that met all of the criteria, 22 focused on adolescents aged 12–18 y, 6 on children aged 6–11 y, and 5 focused on children aged 2–5 y. Sample sizes ranged from 30 parent-child dyads (13) to >64,000 children (14). The majority (n = 26) of studies used a cross-sectional design, whereas others incorporated longitudinal analyses (n = 5) or were intervention-based (n = 2). Twenty-eight of the 32 studies used a questionnaire to assess family meal characteristics, which included the question, “During the past 7 days, how many times did all or most of your household eat a meal together?” Most studies (n = 18) based their family meal questions on Fulkerson et al.’s measure of family meals (28), which has not been validated. Others reported that the questions were part of a larger data source without providing psychometrics for the measure (n = 10). The remaining assessment methods included direct observation (n = 4) and self-report experience method sampling (n = 1), which studies reported were valid and reliable measures. Of note, 12 studies used the same data source to describe family meal characteristics, Project EAT (Eating Among Teens), a large longitudinal study of the dietary patterns of adolescents in Minnesota.
All of the studies reported on ≥1 of the 4 structural features of family meals: 1) frequency or mean number of family meals per week (n = 29), 2) length of family meal in minutes (n = 4), 3) location of family meals (n = 3), and 4) people present at family meals (n = 7). The majority of studies (n = 25) characterized family meals by using 1 category, with no studies characterizing family meals by using all 4 categories. More than half (n = 23) did not specify which family meal (breakfast, lunch, or dinner) participants were reporting. Studies focused on a range of outcomes, including diet quality (n = 8), screen time (n = 8), substance use (n = 6), and risk of overweight and obesity (n = 4), whereas some did not focus on outcomes at all (n = 7). In the studies that examined health outcomes in relation to family meals, a higher frequency of family meals and positive interpersonal dynamics were generally associated with decreased risk of obesity and maladaptive eating behaviors in middle childhood and adolescence (3, 4, 14–19). More frequent family meals were also associated with decreased substance use in adolescence, especially among females (20–25), as well as higher parental support, encouragement, and engagement (26–28).
Because we were interested in the structural characteristics of family meals by age, a summary of family meal characteristics by the following child developmental stages is presented below: early childhood (2–5 y), middle to late childhood (6–11 y), and adolescents (12–18 y). The study design, sample, family meal characteristics, and results of each study are provided in Table 1.
Frequency and mean number of family meals
Early childhood.
Three studies included either frequencies or mean number of family meals per week for children ages 2–5 y. Two of the 3 studies presented the mean number of family meals from the same intervention study, with 1 study focusing on baseline data (mean = 6.2 family meals/wk) (29) and 1 study on outcome data (mean = 6.3 family meals/wk) (30). The percentage of families that reported having ≥7 family meals/wk ranged from 49% (31) to 64% (29). Seventy-three percent of families reported sharing ≥5 family meals/wk (31).
Middle to late childhood.
Five studies included either frequencies or mean number of family meals per week for 6–11 y olds. Miller et al. (32) reported that the mean number of family meals for breakfast and dinner decreased from first to eighth grade. Specifically, the mean number of family breakfasts decreased from 4.4/wk in first grade to 3.2/wk in eighth grade and family dinners decreased from 5.7/wk in first grade to 5.2/wk in eighth grade.
Adolescence.
Relative to early and middle childhood, more studies focused on the frequency of family meals in adolescence (n = 21). Larson et al. (33), the only study to report on family meals for breakfast, reported a mean of 1.5 family breakfasts/wk, whereas the mean values from other studies that reported on dinners and unspecified family meals ranged from 2.9 to 5.1 times/wk (15, 16, 20, 21, 26, 27, 33–37). Frequencies of families sharing ≥3 meals/wk ranged between 56% and 86% (17, 21–23, 27, 33, 38) and for families sharing ≥5 meals/wk ranged between 44% and 61% (4, 22, 24, 28, 39, 40).
Length of meals
Early childhood.
Only 1 study (13) reported meal length in 2–5 y olds. The average time at each meal ranged from 18 to 23 min and differed depending on race and ethnicity, with Hispanic families spending significantly longer on each meal than white and black families.
Middle to late childhood.
Similarly, only 1 study reported meal length in 6–11 y olds (18) and found that the average meal length was ∼15 min.
Adolescence.
Two studies reported meal length in adolescents (19, 26). The mean length of meals for adolescents was slightly higher than for early childhood and middle childhood, ranging from 19 (19) to 27 (26) min.
Location
Early childhood.
One study (41) reported on location of family meals, with parents reporting that 82% of children “always eat at the table.”
Middle to late childhood.
Similar to the early childhood age range, only 1 study reported on where 6–11 y olds eat family meals. Most (72%) reported eating in a kitchen (dining room table) (18), 20% reported eating in a family room, and 8% reported eating in an office or bedroom.
Adolescence.
As with early and middle childhood, 1 study also reported where adolescents eat family meals. In an observational study, Berge et al. (15) found that 62% eat family meals in a kitchen or at a dining room table and 38% eat in a family room, bedroom, or office.
Who is present
Early childhood.
Two studies reported who was present at family meals for 2–5 y olds. One study (41) reported that 60% of mothers “always eat with their child,” whereas the second study showed that the number of children, but not adults, at family meals differed by racial background, with Hispanic and white families having more children present at family meals than African-American families (13).
Middle to late childhood.
Three studies reported on who was present at family meals for 6–11 y olds. At least 1 parent was reported to be present at family meals ≥7 times/wk in 74–81.7% of families (42, 43). Berge et al. (18) were more specific, reporting that of people present at family meals, 85% are mothers, 34% are fathers, 53% are sisters, and 39% are brothers.
Adolescence.
Two studies (16, 21) reported on who was present at family meals in an adolescent population. Both studies specified if the person present was an adult and if the adult was a mother, father, or both and reported that mothers were more likely to be present (83%) than fathers (38%).
Implications for Characterizing Family Meals
This systematic review included 33 studies, of which 29 included information on frequency and/or mean number of family meals per week, 4 included information on length of meal, 3 specified location of the family meal, and 7 provided data on who was present at the family meal. No study included all 4 structural aspects of a family meal. Most studies focused on the developmental stage of adolescence and were cross-sectional in nature, limiting the conclusions to be drawn regarding the important structural aspects of family meals across age groups. Without longitudinal data, it is difficult to assess the structural aspects of family meals that change as shifts occur in family structure over time and as children get older.
This review found that the family meal literature has almost exclusively focused on characterizing family meals by using frequency or mean number of meals per week. Less attention has been paid to examining other structural features that are central to family meals, such as who is present, where families are eating, and how long family meals typically last. Previous work that examined family meals showed that the characteristics of the parent-child relationship, such as parent-adolescent communication as well as positive family- and person-level interpersonal dynamics, are related to a decreased risk of overweight and obesity (19). A recent article by Goldfarb et al. (45) posited that family connectedness mediates the relation between frequent family meals and healthier child adjustment. Family meals may be a means to facilitate family connectedness through the routine aspects of the meal environment that contribute to a positive parent-child relationship, such as exchanging of ideas, engaging in problem-solving, improving family closeness, and discussing issues that are sensitive and emotionally laden. Therefore, going beyond the frequency of family meals to identify who is present, where people are eating, and for how long may help elucidate structural characteristics of meals that can encourage positive parent-child interactions at family meals, which further promotes healthy child behaviors.
At this point, however, it is difficult to ascertain which characteristics of family meals are most important to child health because the definition, measurement, and analysis of family meals are not consistent across studies. For example, although some studies defined a family meal as having ≥1 parent present, others just asked if “most of the family” is present, and most did not specify which meal they were measuring (i.e., breakfast, lunch, or dinner). Studies also differed in how they analyzed family meal frequency, with some studies considering ≥3 family meals/wk and others ≥5 family meals/wk as a cutoff point for “frequent” family meals. In addition, many studies did not report psychometrics for the questionnaires they used to assess family meal questionnaires, which could affect the validity and reliability of the results. Few reliable and validated assessment measures of family meals exist (10). The lack of consistency and specificity in defining, measuring, and analyzing family meals makes it difficult to compare results across studies and to examine differences in these structural characteristics of family meals over the years and across different age groups.
The differences that did emerge across age groups are in line with existing research showing increased autonomy in adolescence and reliance on parents for meals at younger ages (6). Findings showed that the frequency of family meals decreased linearly with each developmental stage, such that families of young children reported higher frequency of family meals than did those with children in middle childhood and adolescence. More children in the early childhood stage ate at the dinner table relative to children in middle childhood or adolescence, whereas children in all age groups reported that their mother was more likely to be present at family meals than their father. These findings suggest that adolescence is a critical period during which family meals are occurring less, which as previous research has shown, can lead to increased risk for health risk behaviors (2, 5). Although we have gained valuable information from this population, particularly from Project EAT (46), it is also important to better understand structural characteristics of family meals that are associated with health among younger populations and with samples from other geographic locations. Examining preventive strategies that can be implemented at younger ages to boost family meal adherence is an area of research that is lacking and in need of future study.
Measuring family meal characteristics by using innovative methods, such as asking families to record numerous aspects of the family meal environment in real-time with the use of cell phones or other handheld devices (47), would allow a more comprehensive and accurate assessment of the family meal environment. This information has the opportunity to be captured through prompted questions, visual images, or video, which can then provide a more inclusive analysis of family meals. In addition, measuring family meals and health at different developmental time points (e.g., early childhood, middle childhood, and adolescence) would provide us with the information needed to develop prevention and intervention programs focused on modifying structural family meal characteristics. It can also provide evidence for clear recommendations on who may be the most important family member, in terms of association with positive eating behaviors, to have at a family meal at different developmental stages, which is likely related to socioemotional characteristics such as parental modeling and family cohesiveness.
Given the sociocultural shift in family context over the past decade, our measurement of family meals needs to include more relevant, specific, and comprehensive questions to account for multiple caregivers in families as well as the changing structure of where children eat and with whom (6). Currently, most studies use a unidimensional approach to assess the frequency of family meals (typically one question on a questionnaire), which is subject to error due to self-reporting and may miss important nuances associated with family meals, such as who is present, where people are eating, and for how long. Characterizing who is present will allow one to further investigate if, for example, the person or persons present (e.g., mother, father, siblings) are affecting child health or if child health is more strongly related to the number of individuals present at the family meal (e.g., parents and siblings). Instead of only asking about the frequency of family meals, our questions should ask where children eat their meals and if this differs from week to week, with whom they eat their meals (i.e., babysitters, siblings), and if caregivers are monitoring their meals or eating with them and therefore modeling eating behaviors, an important component of learned behavior for children (48).
Information gleaned from these questions could be used to better understand what structural characteristics of family meals are the most beneficial to child health and well-being. For example, are children more or less willing to eat healthy foods, such as fruit and vegetables, when 1 parent is sitting at the table as opposed to 2 parents or just siblings? Does the amount of time that families spend eating together affect child health and well-being, and is it important where they spend this time during family meals? Understanding the structural features of family meals can inform the development of specific recommendations for families in the context of where, who, how long, and how many times they should eat together to experience the greatest benefit. Furthermore, a more mechanistic evaluation could be conducted to understand what key structural features affect health.
To our knowledge, no randomized controlled trial has yet explicitly targeted family meals. In 2015 Flattum et al. (49) conducted a community- and home-based intervention that largely focused on increasing the frequency of family meals; however, several other intervention targets were included and family meal frequency did not change from the reported baseline frequency of 5 ± 1.9 meals/wk, limiting conclusions on the impact of family meals in isolation. Dismantling studies may be helpful in determining which structural features of a family meal (e.g., how long they should be, who should be present, and how often they should occur) are most important for child and adolescent health. Furthermore, once sufficient data are collected on the structural aspects of family meals and measured consistently across studies, a meta-analysis could help determine the most important structural aspects of family meals that should be used to develop concrete recommendations for families.
This review provides a first step in understanding the structural components of family meals; however, the findings should be interpreted within the context of the study’s limitations. Narrowing our search to studies conducted in the United States may have limited our understanding of the cultural aspects of the family meal environment; thus, these findings are not generalizable to countries outside the United States. It will be important to extend our search to countries other than the United States in future studies to capture all of the nuances and cultural aspects of the structural characteristics of family meals.
In summary, this review suggests that a more comprehensive assessment of family meals is needed in order to develop a standard definition and to provide concrete recommendations to families. Because family meals are complex, multidimensional, and constantly evolving, the questions assessing them also need to be comprehensive and sensitive enough to capture their nuances. The development of assessment tools that could be easily integrated into the home during family meals, such as an application that records family meals unobtrusively or that asks caregivers to answer multiple open-ended questions during or after the meal, may be one approach to better understanding family meals.
Acknowledgments
All authors read and approved the final manuscript.
References
- 1.Barlow SE; Expert Committee. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics 2007;120:S164–92. [DOI] [PubMed] [Google Scholar]
- 2.Hammons AJ, Fiese BH. Is frequency of shared family meals related to the nutritional health of children and adolescents? Pediatrics 2011;127:e1565–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Larson NI, Neumark-Sztainer D, Hannan PJ, Story M. Family meals during adolescence are associated with higher diet quality and healthful meal patterns during young adulthood. J Am Diet Assoc 2007;107:1502–10. [DOI] [PubMed] [Google Scholar]
- 4.Neumark-Sztainer D, Eisenberg ME, Fulkerson JA, Story M, Larson N. Family meals and disordered eating in adolescents: longitudinal findings from Project EAT. Arch Pediatr Adolesc Med 2008;162:17–22. [DOI] [PubMed] [Google Scholar]
- 5.Fulkerson JA, Larson N, Horning M, Neumark-Sztainer D. A review of associations between family or shared meal frequency and dietary and weight status outcomes across the lifespan. J Nutr Educ Behav 2014;46:2–19. [DOI] [PubMed] [Google Scholar]
- 6.Birch L, Savage JS, Ventura A. Influences on the development of children’s eating behaviours: from infancy to adolescence. Can J Diet Pract Res 2007;68:s1–56. [PMC free article] [PubMed] [Google Scholar]
- 7.Cawley J, Liu F. Maternal employment and childhood obesity: a search for mechanisms in time use data. Econ Hum Biol 2012;10:352–64. [DOI] [PubMed] [Google Scholar]
- 8.Quick BL, Fiese BH, Anderson B, Koester BD, Marlin DW. A formative evaluation of shared family mealtime for parents of toddlers and young children. Health Commun 2011;26:656–66. [DOI] [PubMed] [Google Scholar]
- 9.Valdés J, Rodriguez-Artalejo F, Aguilar L, Jaen-Casquero MB, Royo-Bordonada MA. Frequency of family meals and childhood overweight: a systematic review. Pediatr Obes 2013;8:e1–13. [DOI] [PubMed] [Google Scholar]
- 10.Martin-Biggers J, Spaccarotella K, Berhaupt-Glickstein A, Hongu N, Worobey J, Byrd-Bredbenner C. Come and get it! A discussion of family mealtime literature and factors affecting obesity risk. Adv Nutr 2014;5:235–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dwyer L, Oh A, Patrick H, Hennessy E. Promoting family meals: a review of existing interventions and opportunities for future research. Adolesc Health Med Ther 2015;6:115–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bronfenbrenner U. The ecology of human development: experiments by nature and design. Cambridge (MA): Harvard University Press; (2009). [Google Scholar]
- 13.Kong A, Jones BL, Fiese BH, Schiffer LA, Odoms-Young A, Kim Y, Bailey L, Fitzgibbon ML. Parent-child mealtime interactions in racially/ethnically diverse families with preschool-age children. Eat Behav 2013;14:451–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gingold JA, Simon AE, Schoendorf KC. Excess screen time in US children: association with family rules and alternative activities. Clin Pediatr (Phila) 2014;53:41–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Berge JM, Wall M, Larson N, Loth KA, Neumark-Sztainer D. Family functioning: associations with weight status, eating behaviors, and physical activity in adolescents. J Adolesc Health 2013;52:351–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Welsh EM, French SA, Wall M. Examining the relationship between family meal frequency and individual dietary intake: does family cohesion play a role? J Nutr Educ Behav 2011;43:229–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Videon TM, Manning CK. Influences on adolescent eating patterns: the importance of family meals. J Adolesc Health 2003;32:365–73. [DOI] [PubMed] [Google Scholar]
- 18.Berge JM, Rowley S, Trofholz A, Hanson C, Rueter M, MacLehose RF, Neumark-Sztainer D. Childhood obesity and interpersonal dynamics during family meals. Pediatrics 2014;134:923–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Berge JM, Jin SW, Hannan P, Neumark-Sztainer D. Structural and interpersonal characteristics of family meals: associations with adolescent body mass index and dietary patterns. J Acad Nutr Diet 2013;113:816–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Elgar FJ, Napoletano A, Saul G, Dirks MA, Craig W, Poteat VP, Holt M, Koenig BW. Cyberbullying victimization and mental health in adolescents and the moderating role of family dinners. JAMA Pediatr 2014;168:1015–22. [DOI] [PubMed] [Google Scholar]
- 21.Hoffmann JP, Warnick E. Do family dinners reduce the risk for early adolescent substance use? A propensity score analysis. J Health Soc Behav 2013;54:335–52. [DOI] [PubMed] [Google Scholar]
- 22.Eisenberg ME, Neumark-Sztainer D, Fulkerson JA, Story M. Family meals and substance use: is there a long-term protective association? J Adolesc Health 2008;43:151–6. [DOI] [PubMed] [Google Scholar]
- 23.Eisenberg ME, Neumark-Sztainer D, Feldman S. Does TV viewing during family meals make a difference in adolescent substance use? Prev Med 2009;48:585–7. [DOI] [PubMed] [Google Scholar]
- 24.Eisenberg ME, Olson RE, Neumark-Sztainer D, Story M, Bearinger LH. Correlations between family meals and psychosocial well-being among adolescents. Arch Pediatr Adolesc Med 2004;158:792–6. [DOI] [PubMed] [Google Scholar]
- 25.Sisson SB, Broyles ST, Newton RL Jr, Baker BL, Chernausek SD. TVs in the bedrooms of children: Does it impact health and behavior? Prev Med 2011:52(2):104–8. [DOI] [PubMed] [Google Scholar]
- 26.Offer S. Assessing the relationship between family mealtime communication and adolescent emotional well-being using the experience sampling method. J Adolesc 2013;36:577–85. [DOI] [PubMed] [Google Scholar]
- 27.Poulos NS, Pasch KE, Springer AE, Hoelscher DM, Kelder SH. Is frequency of family meals associated with parental encouragement of healthy eating among ethnically diverse eighth graders? Public Health Nutr 2014;17:998–1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fulkerson JA, Neumark-Sztainer D, Story M. Adolescent and parent views of family meals. J Am Diet Assoc 2006;106:526–32. [DOI] [PubMed] [Google Scholar]
- 29.Taveras EM, McDonald J, O’Brien A, Haines J, Sherry B, Bottino CJ, Troncoso K, Schmidt ME, Koziol R. Healthy Habits, Happy Homes: methods and baseline data of a randomized controlled trial to improve household routines for obesity prevention. Prev Med 2012;55:418–26. [DOI] [PubMed] [Google Scholar]
- 30.Haines J, McDonald J, O’Brien A, Sherry B, Bottino CJ, Schmidt ME, Taveras EM. Healthy Habits, Happy Homes: randomized trial to improve household routines for obesity prevention among preschool-aged children. JAMA Pediatr 2013;167:1072–9. [DOI] [PubMed] [Google Scholar]
- 31.Turer CB, Stroo M, Brouwer RJ, Krause KM, Lovelady CA, Bastian LA, Peterson B, Østbye T. Do high-risk preschoolers or overweight mothers meet AAP-recommended behavioral goals for reducing obesity? Acad Pediatr 2013;13:243–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Miller DP, Waldfogel J, Han WJ. Family meals and child academic and behavioral outcomes. Child Dev 2012;83:2104–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Larson N, MacLehose R, Fulkerson JA, Berge JM, Story M, Neumark-Sztainer D. Eating breakfast and dinner together as a family: associations with sociodemographic characteristics and implications for diet quality and weight status. J Acad Nutr Diet 2013;113:1601–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Berge JM, Wall M, Neumark-Sztainer D, Larson N, Story M. Parenting style and family meals: cross-sectional and 5-year longitudinal associations. J Am Diet Assoc 2010;110:1036–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bauer KW, Neumark-Sztainer D, Fulkerson JA, Story M. Adolescent girls’ weight-related family environments, Minnesota. Prev Chronic Dis 2011;8:A68. [PMC free article] [PubMed] [Google Scholar]
- 36.Stewart SD, Menning CL. Family structure, nonresident father involvement, and adolescent eating patterns. J Adolesc Health 2009;45:193–201. [DOI] [PubMed] [Google Scholar]
- 37.Neumark-Sztainer D, Wall M, Fulkerson JA, Larson N. Changes in the frequency of family meals from 1999 to 2010 in the homes of adolescents: trends by sociodemographic characteristics. J Adolesc Health 2013;52:201–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fulkerson JA, Neumark-Sztainer D, Hannan PJ, Story M. Family meal frequency and weight status among adolescents: cross-sectional and 5-year longitudinal associations. Obesity (Silver Spring) 2008;16:2529–34. [DOI] [PubMed] [Google Scholar]
- 39.Fulkerson JA, Story M, Mellin A, Leffert N, Neumark-Sztainer D, French SA. Family dinner meal frequency and adolescent development: relationships with developmental assets and high-risk behaviors. J Adolesc Health 2006;39:337–45. [DOI] [PubMed] [Google Scholar]
- 40.Fulkerson JA, Kubik MY, Story M, Lytle L, Arcan C. Are there nutritional and other benefits associated with family meals among at-risk youth? J Adolesc Health 2009;45:389–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Goulding AN, Rosenblum KL, Miller AL, Peterson KE, Chen YP, Kaciroti N, Lumeng JC. Associations between maternal depressive symptoms and child feeding practices in a cross-sectional study of low-income mothers and their young children. Int J Behav Nutr Phys Act 2014;11:75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fulkerson JA, Story M, Neumark-Sztainer D, Rydell S. Family meals: perceptions of benefits and challenges among parents of 8- to 10-year-old children. J Am Diet Assoc 2008;108:706–9. [DOI] [PubMed] [Google Scholar]
- 43.Fulkerson JA, Kubik M, Rydell S, Boutelle K, Garwick A, Story M, Neumark-Sztainer D, Dudovitz B. Focus groups with working parents of school-age children: what’s needed to improve family meals? J Nutr Educ Behav 2011;43:189–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sen B. The relationship between frequency of family dinner and adolescent problem behaviors after adjusting for other family characteristics. J Adolesc 2010;33:187–96. [DOI] [PubMed] [Google Scholar]
- 45.Goldfarb SS, Tarver WL, Locher JL, Preskitt J, Sen B. A systematic review of the association between family meals and adolescent risk outcomes. J Adolesc 2015;44:134–49. [DOI] [PubMed] [Google Scholar]
- 46.Neumark-Sztainer D, Larson NI, Fulkerson JA, Eisenberg ME, Story M. Family meals and adolescents: what have we learned from Project EAT (Eating Among Teens)? Public Health Nutr 2010;13:1113–21. [DOI] [PubMed] [Google Scholar]
- 47.Laska MN, Graham D, Moe SG, Lytle L, Fulkerson J. Situational characteristics of young adults’ eating occasions: a real-time data collection using personal digital assistants. Public Health Nutr 2011;14:472–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Birch LL, Fisher J. Development of eating behaviors among children and adolescents. Pediatrics 1998;101:539–49. [PubMed] [Google Scholar]
- 49.Flattum C, Draxten M, Horning M, Fulkerson JA, Neumark-Sztainer D, Garwick A, Kubik MY, Story ME. HOME Plus: program design and implementation of a family-focused, community-based intervention to promote the frequency and healthfulness of family meals, reduce children’s sedentary behavior, and prevent obesity. Int J Behav Nutr Phys Act 2015;12:53. [DOI] [PMC free article] [PubMed] [Google Scholar]