Abstract
Renal cell carcinoma (RCC) incidence is highest in highly developed countries and it is the seventh most common neoplasm diagnosed. RCC management include nephrectomy and targeted therapies. Type 1 insulin-like growth factor (IGF-1) pathway plays an important role in cell proliferation and apoptosis resistance. IGF-1 and insulin share overlapping downstream signaling pathways in normal and cancer cells. IGF-1 receptor (IGF1R) stimulation may promote malignant transformation promoting cell proliferation, dedifferentiation and inhibiting apoptosis. Clear cell renal cell carcinoma (ccRCC) patients with IGF1R overexpression have 70 % increased risk of death compared to patients who had tumors without IGF1R expression. IGF1R signaling deregulation may results in p53, WT, BRCA1, VHL loss of function. RCC cells with high expression of IGF1R are more resistant to chemotherapy than cells with low expression. Silencing of IGF1R increase the chemosensitivity of ccRCC cells and the effect is greater in VHL mutated cells. Understanding the role of IGF-1 signaling pathway in RCC may result in development of new targeted therapeutic interventions. First preclinical attempts with anti-IGF-1R monoclonal antibodies or fragment antigen-binding (Fab) fragments alone or in combination with an mTOR inhibitor were shown to inhibit in vitro growth and reduced the number of colonies formed by of RCC cells.
Keywords: Renal cell carcinoma (RCC, ccRCC), Insulin-like growth factor-1 (IGF-1), IGF-1 receptor (IGF1R)
Background
Renal cell carcinoma (RCC) comprise 2–3 % of malignant tumors in adults. Clear cell RCC (ccRCC) develops from epithelium of the proximal tubules and is the most common a histological type of RCC – diagnosed in 60-70 % of cases. Initial treatment of RCC is most often partial or radical nephrectomy. Nevertheless one third of patients are diagnosed with synchronous metastases [1]. IGF-1 plays an important role in protection from apoptosis and regulation of cell growth. Deregulation in downstream IGF-1 receptor results in angiogenesis, cell viability, proliferation and invasion. IGF1R expression is poor prognostic factor especially among those presenting with high-grade disease at the initial evaluation. RCC cells with high expression of IGF1R are more resistant to chemotherapy than cells with low expression of that receptor [2]. IGF-1 and insulin share overlapping downstream pathways of cancer cell metabolism. Cell line based studies have shown that down-regulation, knock-out, pharmacological inhibition of IGF-IR may in turn increase in IR signaling and therefore insulin analogs may promote cancerogenesis [3]. On the other hand first preclinical attempts with anti-IGF-1R monoclonal antibodies or fragment antigen-binding (Fab) fragments alone or in combination with an mTOR inhibitor were shown to inhibit in vitro growth and reduced the number of colonies formed by of RCC cells [4, 5]. All these findings suggest that IGF1R expression is significant in ccRCC and understanding of the molecular mechanism of IGF-1 and insulin signaling pathway in RCC may give opportunity to design molecular markers of disease or even finding a new molecular targets for drugs.
Renal cell carcinoma
Renal cell carcinoma is the seventh most common malignancy with expected 5-year survival rate of 72 %. About 64 % of patients are diagnosed with localized disease [6]. RCC has highest incidence in highly developed countries. RCC includes several types of cancer: clear cell RCC, papillary RCC, chromophobe RCC and also rare cancer like, urothelial carcinoma, collecting duct carcinoma and renal medullary carcinoma [7]. The most common type is clear cell RCC that is diagnosed in up to 70 % of cases. Among those up to 60-90 % of sporadic cases of ccRCC exhibit VHL gene loss, silencing, mutation or promoter hypermethylation. The VHL protein (pVHL) is an E3 ubiquitin ligase of hypoxia inducible factor (HIF). It targets HIF for degradation by the proteasome. In the absence of functional pVHL HIF is accumulated in the nucleus where it acts as a transcription factor for vascular endothelial growth factor (VEGF), platelet derived growth factor (PDGF), multidrug resistance pump (MDR-1), cyclin D1 (CCND1), ENOLASE2 (ENO2), Egl-9 Family Hypoxia-Inducible Factor 3/HIF Prolyl Hydroxylase 3 (EGLN3), angiopoietin-like 4 (ANGPTL4), glucose transporter 1 (GLUT1), insulin-like growth factor-binding protein 3 (IGFBP3), and erythropoietin (EPO) [8, 9]. Management of RCC is usually initiated with partial or radical nephrectomy. Ablation procedure is alternative for small renal masses in patients who are ineligible for surgery [10, 11]. Adjuvant therapy has no proven efficacy on management of RCC. Only systemic treatment of metastatic disease has been shown as effective in phase III trials [1, 7]. There are 3 major groups of systematic treatment that are used for metastatic RCC: cytokines, mTOR inhibitors and anti- vascular endothelial growth factor (VEGF) - targeted drugs [7]. Cytokine based immunotherapies included interferon-alpha [12] and high dose interleukin 2 (IL-2) [13], while mTOR inhibitors approved for RCC treatment are everolimus [14] and temsirolimus [15]. VEGF pathway inhibitors used are 1) tyrosine kinase inhibitors as sorafenib [16], sunitinib [17], pazopanib [18], and axitinib [19], and 2) anti-VEGF monoclonal antibody – bevacizumab [20] (Table 1). New drugs that modulate immunological response including anti-CTLA-4 (cytotoxic T lymphocyte antigen 4) antibody and anti-PD-1/PDL-1 (programmed cell death 1) antibody have been developed recently [7, 21, 22]. Anti-CTLA-4 or anti-PD-1 antibodies inhibit the immunosuppression between T cells and APC (antigen presenting cells) including cancer cells which stimulate anti-tumor response [21, 22]. Most recently nivolumab - anti-PD-1 monoclonal antibody - was shown as effective against RCC in trail using everolimus as comparator [23].
Table 1.
Drugs used in RCC therapy
| Group of drug | Drugs | Ref. |
|---|---|---|
| cytokines | 1) Interleukin 2 - overall response rate - 15 %, complete response rate - 5 %, achieved by high dose. Problems with selection of patients who may benefit from treatment. 2) Interferon alfa - inferior to most new agents considering PFS (progression free survival), except in combination with bevacizumab. |
[13, 100] |
| VEGF-targeted drugs | 1) Sorafenib – second and subsequent lines of treatment. 2) Sunitinib – first line treatment for metastatic RCC. 3) Pazopanib – non-inferior to sunitinib 4) Axitinib – treatment refractory RCC. 5) Bevacizumab – used with interferon alfa. Superior PFS when compared with monotherapy of interferon alfa. |
[7, 101, 102] |
| mTOR inhibitors | 1) Temsirolimus – for patient with poor risk as a first line druga
2) Everolimus – used as a second line or third line drug. |
[7, 14, 17] |
athe five Memorial Sloan Kettering Cancer Center (MSKCC) factors plus metastasis in more than one organ
General IGF-1 function
Insulin-like growth factor 1 (IGF-1, somatomedin C) is a natural anabolic peptide hormone produced mainly by hepatocytes. IGF-1 with molecular weight of 7649 Da is built by 70 amino acids and single polypeptide chain with three intramolecular disulfide bridges. Production of IGF-1 is stimulated by growth hormone (GH) secreted by anterior pituitary. IGF-1 production is also stimulated by insulin and has influenced on reduction of lipolysis, glycolysis, inhibition of lipolytic function of adrenaline, embryonic growth and differentiation of cells. IGF-1 may also be released independently of GH. Circulating IGF-1 produced in liver acts in endocrine manner, but locally produced IGF-1 acts also in an autocrine manner. IGF functions therefore both as circulating hormone and tissue growth factor. Circulating IGF-1 forms a complex with two other proteins – the IGF binding protein (IGFBP) and the acid labile subunit (ALS). Six different IGFBPs were characterized, but about 75 % of serum IGFs are bound to IGFBP3 and only 1 % of serum IGF-1 is free-bioactive form [24]. IGFBPs are also mostly synthesized in the liver. Nevertheless IGFs and IGFBPs are also produced in other organs, acting locally in autocrine and paracrine manner and mediating stromal - epithelial cell interactions [25]. IGFBPs acts in a competing manner against IGFR (IGF receptors) and IGFBP proteases. IGF-1 and IGFBP-3 complex play crucial role in mitogenesis, cell differentiation and survival [26]. IGF-1 null mice die shortly after birth [27].
Circulation of IGF-1
High level concentrations of circulating IGF-1 are related with higher risk of prostate, colorectal and breast cancers [28–30]. Circulating concentrations of IGFBP-3 is associated with increased risks of breast cancers in postmenopausal women and prostate cancer in men [28, 29, 31]. Transgenic mouse with deletion in liver-specific IGF-1 that result 75 % reduction in circulating IGF-1 exhibit reduction in development of colon cancer and reduced growth tumor xenografts [31, 32]. Laron syndrome is genetic condition characterized by GH insensitivity and in consequence IGF-1 deficiency [33]. People with Laron syndrome are resistant to cancer what was shown by Steuerman et al. [34]. They found that none of the 230 patients with Laron syndrome developed cancer and that only 1 out of 116 patients with inborn IGF-1 loss was diagnosed with malignancy [34].
IGF-1 receptor and insulin receptor homology
IGFR-1 is a transmembrane receptor with tyrosine kinase activity and is built of two α-subunits (located extracellularly) and two β-subunits (spanning the membrane and activating intracellular signal transduction). Both the α and β subunits are synthesized from a single precursor mRNA. IGF1R shares a high structural homology with the insulin receptor (IR) – has more than 50 % in the overall amino acid sequence and in particular 84 % similarity in the tyrosine kinase domain and 45–65 % in the ligand-binding domain. Moreover ligand-dependent activation of the IGF1R and IR activates almost identical downstream signaling pathways [35]. After IGF-1 binging activation of tyrosine kinase (β-subunits) results in downstream signaling via IR substrate proteins (IRS1-4), Src homology 2 domain containing transforming protein 1 (Shc), GRB2-associated binding protein 1 (Gab-1), Casitas B-lineage Lymphoma proto-oncogene E3 ubiquitin protein ligase (Cbl), Phosphatidyl Inositol 3-Kinase (PIK3), Protein kinase B (Akt), mammalian target of rapamycin (mTOR), mitogen-activated protein kinase (MAPK) and signal regulatory protein family [36]. Insulin and IGFs have a great homology and can have cross-reactivity upon receptors. Moreover hybrid receptors - constituted of IR and IGF1R heterodimers – have been shown to have cellular biological effects resembling those of the IGF1R and were found in colon cancer, thyroid cancer and breast cancer cell lines and tissues [37]. To complicate the interaction even more there are two IR isoforms, arising in the cell by alternative splicing of exon 11 – isoform IR-A, that lacks exon 11, and isoform IR-B – containing exon 11. Insulin does not bind to the hybrid receptors, but binds to IR-A, IR-B, and IGF-1R but binds to the IGF-1R with much lower affinity than to the IR. IGF-I binds to the IGF-1R, hybrid receptors, and IR but has much lower affinity for the IR than IGF-1R [3]. In total insulin and IGF-1 interact with six receptors: the type I IGF receptor (IGF1R), the IRA (IR-A, predominantly expressed in fetal tissue), the IRB (IR-B, predominantly expressed in adult tissue), hybrid receptors of IGF and IR-A, hybrid receptors of IGF and IR-B, and hybrid receptors of IR-A and IR-B [38, 39]. Insulin and IGF-1 while binding to IGF1R, IR-A, IGF1R/IR-A, mediate mostly mitogenic signaling (Ras > MEK > Erk1/2 pathway), while binding to IR-B activate mostly metabolic pathway (PI3K > Akt > mTOR) [24, 36, 40]. As a result both insulin and IGF-1 can act through the hybrid receptors and through the specific receptor for their ligand (Fig. 1). Activation of all receptors (IR, IGF1R, hybrid) which are tyrosine kinase cell-surface receptor result in phosphorylation of IR substrate proteins (IRS 1–4). It activates two key signal-transduction pathways. The GTPase Ras-Raf-MEK-ERK1/2 pathway activates gene expression that result in cells proliferation. The AKT kinase pathway activates mTOR which results in cells proliferation. PI3K induce angiogenesis by activating of hypoxia-inducible factor-1a. Activation of AKT2 promotes GLUT4 translocation leading to the activation of glycogen synthase [31, 41, 42]. Moreover in cancer cells it was shown that GF-1R undergoes nuclear import and both alpha and beta subunits traffic to the nucleus by clathrin-mediated endocytosis. Ligand activated nuclear IGF-1R is phosphorylated and undergoes interaction with chromatin and regulate transcription. This nuclear IGF-1R accumulation is associated with poor prognosis in RCC [43].
Fig. 1.
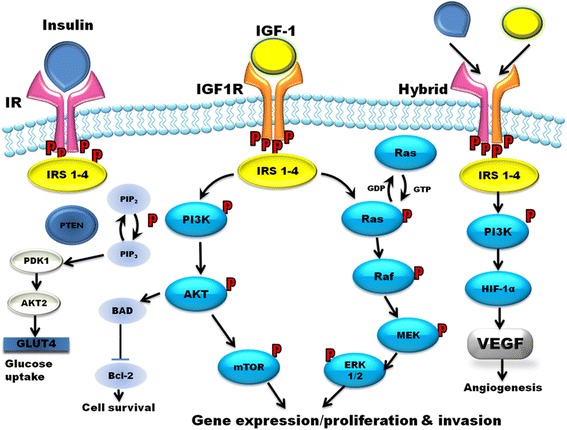
Schematic representation of downstream signaling of IGF1R. AKT, protein kinase B; AMPK, AMP-activated protein kinase; Bcl-2, B-cell lymphoma 2; BAD, B-cell CLL/lymphoma 2 antagonist of cell death; ERK 1/2, extracellular-signal-regulated kinase 1/2, IGF1R, insulin-like growth factor 1 receptor; IR, insulin receptor; IRS1-4, insulin-like receptor substrate 1–4; MEK, mitogen-activated protein kinase kinase; mTOR, mammalian target of rapamycin; PI3K/AKT, phosphatidylinositol 3-kinase/AKT; PDK1, 3-phosphoinositide-dependent protein kinase; PIP2, phosphatidylinositol 4,5-bisphosphate; PIP3, phosphatidylinositol 3,4,5-trisphosphate; PTEN, phosphatase and tensin homolog; GLUT4, Glucose transporter type 4; HIF-1α, Hypoxia-inducible factor 1-alpha, VEGF, Vascular endothelial growth factor
Molecular deregulation of IGF1R pathway and cancerogenesis
IGF-1/insulin pathways were show as significant in cancer research. First of all IGF-1 and insulin share overlapping downstream pathways of cancer cell metabolism. Chronic hyperinsulinemia and diabetes mellitus type 2 were associated with tumor development through the obesity-cancer association [31, 44]. According to the Werner et all. IGF1R activation is pre-requisite for malignant transformation. As oncogenic transformation is initiated, cell survival of transformed cells is strongly dependent on IGF-1 signaling [44]. Further multiple studies confirmed the role of IGF −1 and its receptors on RCC cancerogenesis [41, 45]. Deregulated IGF1R kinase activity and its overexpression was reported in multiple cancers including RCC [46–48]. In particular constitutively active IGF1R leads to salivary and mammary adenocarcinomas in transgenic mice [49]. Transgenic overexpression of IGF1R increases epithelial mammary gland hyperplasia and tumor formation [50]. In the RCC cell lines including Caki-2 (from a primary tumor) and SK-RC-52 (from a metastatic tumor) IGF-1 was shown to enhance transforming growth factor-β (TGF-β) signaling and via TGF-β raise IGF-binding protein 3 (IGFBP-3) levels with growth-promoting effect [51].
Unlike in most genes, promoter sequence lacks TATA and CCAAT boxes that are usually required for efficient transcription initiation. Instead of TATA box, promoter is highly rich in GC base pairs. The initiator (INR) is located approximately 1000 bp upstream of the coding region. Specificity protein 1 (Sp1) is a key transcription activator of the IGF1R gene that binds with high affinity to GC boxes in promoter. The products of tumor suppressor genes like BRCA1, p53, VHL acts through the Sp1 protein [52]. The schematic representation of promoter and other transcription factor shows Fig. 2.
Fig. 2.
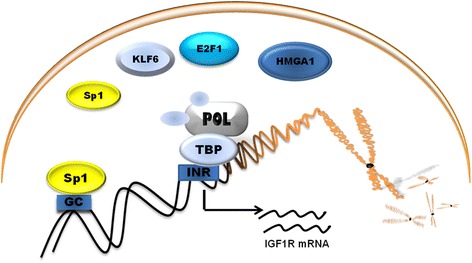
Schematic representation of promoter region of IGF1R and its main transcription factors. Sp1, Specificity protein 1; HMGA1, High mobility group A1; KLF6, Krüppel-like factor 6; E2F1, E2F family of transcription factors; POL, RNA polymerase II; TBP, TATA-binding protein; GC, GC boxes; INR, initiator element
IGF1R activity deregulation is result of loss of tumor suppressor genes or the action of oncogenes [53]. The examples are p53, BRCA1, WT1 genes. p53 is the one of the most frequently mutated tumor suppressor and is well known gene associated with cancerogenesis. Product of p53 gene accumulates in response of DNA demage and results in arrest of cell cycle at G1 phase. Cell can repair DNA or activate apoptotic program. Wild-type p53 supperess the activity of IGF1R promoter whereas mutated p53 enhence promoter activity and accelerate tumor growth [54]. Next antioncogene BRCA1 is linked to the etiology of hereditary of familial breast and ovarian cancer. Wild-type BRCA1 reduce the promoter activity of IGF1R whereas mutated BRCA1 lead to enhance IGF1R promoter activity and expression of protein. BRCA1 and BRCA2 carries have an increased level of IGF1R compared with those with sporadic cancers [55, 56]. WT1 gene which product is a zinc-finger transcription factor is associated with the etiology of Wilms tumor a kind of pediatric kidney cancer [57]. All of these genes products are able to suppress the activity of IGF1R promoter, as well as the endogenous levels of IGF1R mRNA [57–59]. IGF1R expression level is raised in non-BRCA1-mutated ovarian cancer cells compared with normal tissue and additionally IGF1R levels are significantly increased in BRCA1-inactivation ovarian cancer [59]. Moreover investigation in SNP in IGF-1 and IGFR-1 indicate that IGF1-pathway polymorphisms are potential prognostic molecular markers in colorectal cancer and pancreatic cancer. There are significantly associated with progression-free survival and/or overall survival (OS) in these cancers [60, 61]. SNP polymorphisms and mutation of IGF1R that are associated with cancer represents Table 2.
Table 2.
SNP’s and mutations of IGF1R gene associated with cancers
| SNP/mutation | Nucleotide change | Type of cancer | Fuctional feature | Ref. |
|---|---|---|---|---|
| rs8038415 | TT | Breast cancer | BRCA1 carriers with homozigosity TT at this SNP site experience a 40 % higher risk of breast cancer. | [103] |
| rs2272037 | T > C | Colorectal cancer; Glioma |
Significantly related with shorter OS in patients with metastatic colorectal cancer (mCRC). CT and TT associated with increased risk for glioma. | [60] [104] |
| rs2016347 | G > T | Colorectal cancer, glioma | Related to reduced responsiveness to cetuximab treatment. Shorter OS in patients with mCRC. G allele associated with increased risk for Glioma (3’UTR in 3129 site) | [104, 105] |
| rs8038415 | C/T | Non–small cell lung cancer (NSCLC) | Homozygous TT in this SNP had a significantly better OS compared with heterozygous individuals and a trend toward improved survival compared with patients that were homozygous for CC . | [106] |
| CNV in IGF1R gene | Non–small-cell lung cancers (NSCLC) | High IGF1R gene copy number harbors positive prognostic value in NSCLC | [107] | |
| Amplification in 15q26 | High grade glioma | Unkown | [108] | |
| Amplification in 15q25-26 | Alveolar Rhabdomyosarcoma | Related with the rearrangement of PAX7 gene | [109] | |
| A1374V | Lung squamous cell carcinoma | Unknown; mutation occur in the C-terminal lobe of the kinase catalytic domain | [110] | |
| Deletion S1278 | Renal clear cell carcinoma | Unknown; deletion occur in the C-terminal tail region of the receptor | [110] | |
| M1255I | Lung adenocarcinoma | Unknown; mutation occur in in the C-terminal lobe of the kinase catalytic domain | [110] | |
| G596V | Thymic carcinoma | Exonic, Missense | [111] | |
| rs61740868 | C/T | Unknown | Unfavorable substitution Arg1216Cys; showed an increase in energy (less favorable change) in comparison with the native structure. | [112] |
| rs45437300 | A/T | Unknown | Nonsense mutation | [112] |
| rs2229765 | A/G | Unknown | Affect splicing regulation; to be associated with higher plasma concentrations of circulating IGF1R | [112] |
| rs55895813; rs36108138; rs45495500 | A/G; A/C; C/T | Unknown | Splicing site | [112] |
The mechanism of action of P53 and BRCA1 involves interaction with Sp1 to repress the expression of IGF1R [52]. BRCA1 can inhibit IGF1R expression regardless of p53 expression level but not in mutant state of p53. WT1 protein does not involve direct interaction with promoter DNA sequence [62]. Loss-of-function of that genes leads to up-regulation of IGF1R gene. Other tumor suppressor gene VHL, Von Hippel–Lindau tumor suppressor also inhibits IGF1R promoter activity through interaction with Sp1 protein. In RCC inactivation of VHL is associated with IGF1R up-regulation [63]. Schematic representation of main tumor suppressor protein acting on promoter is shown on Fig. 3.
Fig. 3.
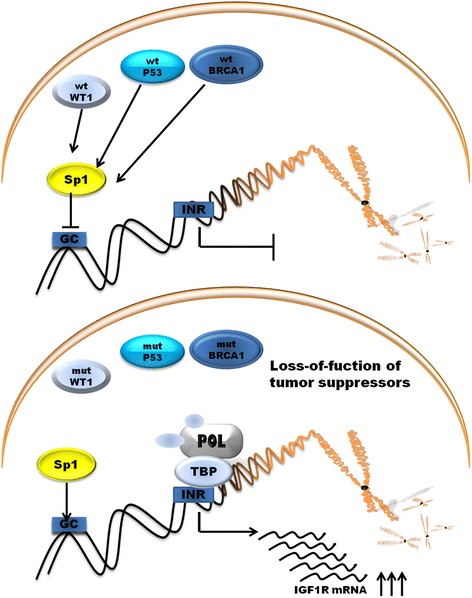
Regulation of promoter activity of IGF1R gene by tumor suppressor genes. POL, RNA polymerase II; TBP, TATA-binding protein; GC, GC boxes; INR, initiator element
Expression of IGF-1 and IGF1R in kidney
Locally synthesize IGF-1 in kidney acts as a paracrine or autocrine factors. Level of IGF-1 in venous renal blood is higher than in renal arterial blood. There are no strong proves on IGF-1 epithelial expression. Studies indicates connective tissue adjacent to epithelial renal cells to be responsible for local synthesis of IGF-1 [64, 65]. Research on human fetal kidney shows no expression of mRNA of IGF-1 in nephrogenic zone but only probably sequestration of IGF-1 peptide in proximal and distal tubules. Studies on rats and mouse shows the IGF-1 (mRNA and peptide) expression (immunolabeling) in collecting ducts. In situ hybridization studies indicate the mRNA expression in medullary thick ascending limb of henle’s loop [64, 66, 67]. IGF- 1 mediated decline in renal vascular resistance, leads to elevated glomerular perfusion, sodium and water resorption leading in turn to soft tissue swelling and glomerular hypertrophy [65, 68]. IGF1R gene expression were detected in whole nephogenic zone including the strong expression in glomeruli and the tubular epithelium of medulla with the least expression in proximal tubules [69]. In contrary Kamenicky et al. shows the strong expression of mRNA of IGF1R in proximal tubule obtained from murine cells by microdissection [65, 70].
Expression of IGF-1 and IGF1R in ccRCC
The type 1 insulin-like growth factor receptor (IGF1R) has an influence on renal cells malignant transformation by induction of cell proliferation, dedifferentiation and anti-apoptotic effect [71, 72]. IGF-1 and IGF1R expression is modulated in kidney development. In mouse model of kidney development IGF-I mRNA is expressed in all cell types with peak in the proximal tubules, peritubular capillaries of the outer medulla and inner cortex one week after birth. The expression of IGF1R in normal proximal tubules was similar to IGF-1 during kidney development until birth [73], but it is poor prognosis factor in RCC [74]. Overexpression of IGF family members was reported observed in oxidative stress (ferric nitrilotriacetate) induced RCC in rats [75]. What is interesting RCC cells with high expression of IGF1R are more resistant to chemotherapy than cells with low expression of that receptor [2]. IGF-I pretreatment levels in RCC patients was predictive to impaired response to interleukin-2 (IL-2) therapy [76]. In SN12K1 cells (cell line derived from metastatic RCC) it was shown that RCC express IGF-I and IGFBP-3, and autocrine IGF-I and IGFBP-3 stimulate and inhibit growth respectively. These cells are also are responsive to exogenous IGF-I stimulation - DNA synthesis is increased. These RCC cells are also responsive to exogenous IGF-I stimulation [77]. Further experiments on RCC cell lines - Caki-2 (primary tumor) and SK-RC-52 (metastatic tumor) – have shown that IGF-I enhances transforming growth factor (TGF)-beta signaling including phosphorylation and nuclear translocation of mothers against decapentaplegic homolog 2 (Smad2). In turn TGF-beta promotes IGFBP-3 production [51]. In mice model injection of MZ-4–71 - growth hormone-releasing hormone antagonist - reduced the IGF-1 induced growth of Caki 1 RCC cell line derived tumors [78].
In first clinical reports high serum IGF-I levels have been associated with an increased risk of developing RCC [77]. At the same time in the analysis of 256 patients serum IGF-1 was not correlated with tumor stage or grade, but was independent favorable prognostic factors in a multivariable analysis [79]. More recently the prospective study of 29 133 Finnish male smokers reported that men with IGF-I levels >113 ng ml(−1) were 59 % less likely to develop RCC than men with levels below or =113 ng ml(−1). Among those 100 men with RCC the IGF binding protein-3 (IGFBP-3) levels did not alter the association [80]. In the study of 90 patients with ccRCC and 20 normal renal tissue samples, hyper-methylation of IGFBP-3 was not found, but in 786–0, ACHN, HRC51 and HRC59 cell lines methylation of IGFBP-3 was observed [81]. Moreover IGF-I and its binding proteins IGFBP-3 and −6 are up-regulated in ccRCC tumor tissues [77]. IGF1R expression was also associated with ccRCC and indicated molecular prognostic marker and potential targets for therapeutic intervention. Data of 280 patients who had ccRCC treated with radical nephrectomy showed that IGF1R expression had a 70 % increased risk of death than patients who had tumors without IGF1R expression [82]. Finally nuclear IGF-1R was detected in primary renal cancer tissues of high proliferation rate and was associated with adverse prognosis [43].
Pathological and clinical grading system and IGF1R status
Fuhrman nuclear grading system correlates with staging of ccRCC. Studies on expression of IGF1R and Furman score in 68 ccRCC showed the statistically significance increasing correlation between Fuhrman grading and IGF1R staining [83]. Also the high serum concentration of IGF1R is associated with the risk of many cancers such as breast, prostate, colorectal, and lung cancers [71]. Overexpression of IGF1R is related with poor prognosis in many human cancers besides the renal cancer also in breast and ovarian cancers [84, 85]. Antisense strategies against the IGF1R suppresses the expression of IGF1R can abolish cell transformation [71, 83]. No correlation was observed between serum IGFBP-3 levels and RCC [79], but high expression of IGFBP-3 was found in ccRCC tumors. Fuhrman grades 3 and 4 ccRCC tumors showed higher IGFBP-3 expression than low grade tumors [80, 86].
Although the IGF1R and Insulin receptor (IR) show great homology and interaction they have different relation to the prognosis in ccRCC. Lkhagvadrj et al. investigated the role of IR expression in 126 ccRCC cases. Researchers showed that there was no differences of total IR protein between tumor and non-tumor but immunoreactivity of IR in tumor was mostly observed in nuclear but in non-tumor tissue in nuclear and cytoplasm. The expression of IR was elevated in low-grade tumor but not in higher-grade. Also the IR expression was inversely correlate with Furman nuclear grade and TNM, pathologic T stage in ccRCC. Higher expression of IR correlated with cystic changes in RCC which is favorable prognostic factor. What is interesting IR expression was not related to the diabetes presence. The authors suggest that although IR and IGF1R share the major down-stream signaling pathway, in RCC there are specific substrates for each receptor [87].
Interaction of VHL and IGF1R
Hereditary RCC is commonly associated loss or mutation of the Von Hippel-Lindau (VHL) tumor suppressor gene. VHL mutation was first discovered in patients with VHL disease by Latif F et al. [88] and VHL mutation or loss is identified in 60-90 % of sporadic RCC cases [7, 89]. Next 20 % of ccRCC show silencing of VHL expression by methylation in promoter region [90]. VHL gene encodes protein with ubiquitin ligase E3 activity directing hypoxia-inducible factor-1α (HIF-1α) for degradation [87]. HIF-1α regulate hypoxia response and promote angiogenesis, cell migration, and metabolism [7, 91] via VEGF, PDGF and TGF [92]. Independently of oxygen status IGF1R activates HIF-1α protein by suppressing VHL and promote RCC development [63]. At the same time IGF-1-mediated signaling is inhibited in the presence of wild-type VHL and VHL decrease stability of IGF-1R [93]. In RCC cells beta-domain of VHL interact with protein kinase C delta (PKCD) and inhibits its association with IGF-IR and subsequent downstream signaling [94]. It was also shown that receptor for activated C kinase 1 (RACK1) serves as a direct mediator between loss of pVHL function and IGF-IR signaling in RCC cells. Upon IGF-1 stimulation, pVHL-deficient RCC cells exhibit high rate of RACK1/IGF-IR binding and up-regulated IGF-1R tyrosine kinase activity, phosphoinositide 3-kinase/serine-threonine kinase Akt (PI3K/Akt) signaling and matrix metalloproteinase-2 (MMP-2) activity and high cellular invasiveness [95]. VHL protein has no influence on ubiquitination of IGF1R. On the contrary the activity of IGF1R expression is regulated by VHL at the transcriptional level and is mediated by Sp1 transcription factor. Sp1 protein is sequestered by VHL and act on promoter of IGF1R. Loss of VHL gene increases therefore IGF1R mRNA stability. The levels of IGF1R is higher in ccRCC samples than in benign renal tumors which could be associated with VHL mutation rate in RCC [63, 96]. At the same time depletion of IGF1R enhance the chemosensitivity of ccRCC, but this effect is significant in cells with no functional VHL. Depletion of IGF1R changed sensitivity to mTOR inhibitors, 5-FU, etoposide but not cisplatin [2].
Conclusions
The role of IGF-1/Insulin pathway in cancerogenesis remain unclear. IGF-1 and insulin share major downstream regulation pathway and both are engaged in cancerogenesis and diabetes [97]. There are evidences that diabetic patients have risk of development of renal cancer. Increase in mortality and incidence of renal cell carcinoma among diabetic patients is linked to hyperinsulinemia and obesity. The interaction of hyperglycemia, hyperinsulinemia causes the insulin resistant state and contribute to central adiposity which result in chronic inflammation. The adipose tissue-derived cytokines like resistin, tumor necrosis factor α (TNF-α) and interleukin 6 (IL-6) promotes persistent inflammation and result in genetic instability, putting cells at risk to malignant transformation. Nuclear factor-kB is strongly activated by TNF-α what is associated with cell proliferation and surviving malignant cells [97]. Associations between hyperinsulinemia and increased circulating levels of IGF-1 is proposed to be involved in carcinogenesis. IR and IGF-1 has a nuclear translocation potential and were postulated to be nonclassical transcription factors. IGF1R physically interact with gDNA and also stimulates itself expression. Study of nuclear IGF1R in primary renal cancer cells revealed that IGF1R expression was associated with poor prognosis in renal cancer [98]. Cell culture experiments have proven that active IGF-IR is necessary for cell transformation by multiple cellular and viral oncogenes. IGF-IR signaling regulate the cell cycle, cell survival/proliferation, cell-cell interactions, ECM attachment, cell motility and metastatic spread. In mice model IGF-IR overexpression promotes tumor growth and metastases development, whereas down-regulation of IGF leads to slower tumor development [3]. In general anti-diabetic treatment may increase the risk of RCC cancer development, but large prospective data is not available at this point of time. Exception is metformin an oral anti-diabetic drug has a RCC-protective effect as it interacts with the IGF signaling pathway which results in inhibition of proliferation and apoptosis regardless the p53 status [99].
Abbreviations
ccRCC, Clear cell renal cell carcinoma; CTLA-4, cytotoxic T lymphocyte antigen 4; IGF-1, Insulin-like growth factor-1; IGF1R, IGF-1 receptor; IGFBPs, IGF-binding proteins; PD-1, programmed cell death 1; PDGFR, Platelet-derived growth factor receptors; RCC, renal cell carcinoma; VEGF, Vascular endothelial growth factor; VHL, Von Hippel–Lindau protein
Acknowledgements
Not applicable.
Funding
This work has been supported by National Science Centre (NCN) grant No. UMO-2012/05/D/NZ5/01844 and Military Institute Medicine Statutory Founding (355).
Availability of data and material
Not applicable.
Authors' contributions
Conceptualizing and refining research ideas - AMC; Literature search - AMC, AT; Creating review design - AMC; Collection of literature data - AMC, AT; Data selection - AT, AMC; Interpreting analyses - AMC, AT, CP, CS; Drafting manuscript AT, AMC; Editing manuscript AMC. All authors read and approved the final manuscript.
Authors' information
AMC is MD PhD - expert in molecular biology and medical doctor - specializes in clinical oncology and has been trained at the Universite degli Studi di Palermo, Paracelsus Medizinische Privatuniversität and Emory University School of Medicine. CS – MD PhD - is professor of clinical oncology specialist since 1986, and has worked at Temple University School of Medicine, Jefferson Cancer Institute at Thomas Jefferson University, and in the last 10 years has participated in major renal cancer treatment clinical trials including AXIS, EU-ARCCS or TARGET and is an expert in renal cancer treatment. AT is specialist in Medical Biotechnology and is MD in training, researcher in the Laboratory of Molecular Oncology, Military institute of Medicine, Warsaw, Poland. CP - Professor of Medical Oncology at the University of Pavia, School of Biotechnology, Responsible of the Laboratory of Pre-Clinical Oncology and Developmental Therapeutics at the IRCCS San Matteo University Hospital in Pavia, Member of ESMO Scientific Committee, involved in Development of new anticancer drugs, e.g., WR2721 (Amifostine), Nolatrexed (Thymitaq), BBR3438, Rampirnase (Onconase), BAY 43–9006 (Sorafenib), SU011248 (Sunitinib), RAD001 (Everolimus), Perifosine, ARQ197, Pazopanib and Satraplatin.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Not applicable.
Contributor Information
Adam F. Tracz, Email: a.f.tracz@gmail.com
Cezary Szczylik, Email: anna.czarnecka@gmail.com.
Camillo Porta, Email: c.porta@smatteo.pv.it.
Anna M. Czarnecka, Phone: +48-607-583-284, Email: cszczylik@wim.mil.pl
References
- 1.Escudier B, Szczylik C, Porta C, Gore M. Treatment selection in metastatic renal cell carcinoma: expert consensus. Nat Rev Clin Oncol. 2012;9(6):327–37. doi: 10.1038/nrclinonc.2012.59. [DOI] [PubMed] [Google Scholar]
- 2.Yuen JS, Akkaya E, Wang Y, Takiguchi M, Peak S, Sullivan M, Protheroe AS, Macaulay VM. Validation of the type 1 insulin-like growth factor receptor as a therapeutic target in renal cancer. Mol Cancer Ther. 2009;8(6):1448–59. doi: 10.1158/1535-7163.MCT-09-0101. [DOI] [PubMed] [Google Scholar]
- 3.Gallagher EJ, LeRoith D. Minireview: IGF, Insulin, and Cancer. Endocrinology. 2011;152(7):2546–51. doi: 10.1210/en.2011-0231. [DOI] [PubMed] [Google Scholar]
- 4.Cardillo TM, Trisal P, Arrojo R, Goldenberg DM, Chang CH. Targeting both IGF-1R and mTOR synergistically inhibits growth of renal cell carcinoma in vitro. BMC Cancer. 2013;13:170. doi: 10.1186/1471-2407-13-170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chang CH, Wang Y, Trisal P, Li R, Rossi DL, Nair A, Gupta P, Losman M, Cardillo TM, Rossi EA, et al. Evaluation of a novel hexavalent humanized anti-IGF-1R antibody and its bivalent parental IgG in diverse cancer cell lines. PLoS One. 2012;7(8):e44235. doi: 10.1371/journal.pone.0044235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.ASCO. http://www.cancer.net/cancer-types/kidney-cancer/statistics. Accessed 28 April 2015.
- 7.Jonasch E, Gao J, Rathmell WK. Renal cell carcinoma. BMJ. 2014;349:g4797. doi: 10.1136/bmj.g4797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cowey CL, Rathmell WK. VHL gene mutations in renal cell carcinoma: role as a biomarker of disease outcome and drug efficacy. Curr Oncol Rep. 2009;11(2):94–101. doi: 10.1007/s11912-009-0015-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhang T, Niu X, Liao L, Cho EA, Yang H. The contributions of HIF-target genes to tumor growth in RCC. PLoS One. 2013;8(11):e80544. doi: 10.1371/journal.pone.0080544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Van Poppel H, Da Pozzo L, Albrecht W, Matveev V, Bono A, Borkowski A, Colombel M, Klotz L, Skinner E, Keane T, et al. A prospective, randomised EORTC intergroup phase 3 study comparing the oncologic outcome of elective nephron-sparing surgery and radical nephrectomy for low-stage renal cell carcinoma. Eur Urol. 2011;59(4):543–52. doi: 10.1016/j.eururo.2010.12.013. [DOI] [PubMed] [Google Scholar]
- 11.Vrdoljak E, Ciuleanu T, Kharkevich G, Mardiak J, Mego M, Padrik P, Petruzelka L, Purkalne G, Shparyk Y, Skrbinc B, et al. Optimizing treatment for patients with metastatic renal cell carcinoma in the Central and Eastern European region. Expert Opin Pharmacother. 2012;13(2):159–74. doi: 10.1517/14656566.2012.647406. [DOI] [PubMed] [Google Scholar]
- 12.Motzer RJ, Bacik J, Murphy BA, Russo P, Mazumdar M. Interferon-alfa as a comparative treatment for clinical trials of new therapies against advanced renal cell carcinoma. J Clin Oncol. 2002;20(1):289–96. doi: 10.1200/JCO.20.1.289. [DOI] [PubMed] [Google Scholar]
- 13.Fyfe G, Fisher RI, Rosenberg SA, Sznol M, Parkinson DR, Louie AC. Results of treatment of 255 patients with metastatic renal cell carcinoma who received high-dose recombinant interleukin-2 therapy. J Clin Oncol. 1995;13(3):688–96. doi: 10.1200/JCO.1995.13.3.688. [DOI] [PubMed] [Google Scholar]
- 14.Motzer RJ, Escudier B, Oudard S, Hutson TE, Porta C, Bracarda S, Grunwald V, Thompson JA, Figlin RA, Hollaender N, et al. Efficacy of everolimus in advanced renal cell carcinoma: a double-blind, randomised, placebo-controlled phase III trial. Lancet. 2008;372(9637):449–56. doi: 10.1016/S0140-6736(08)61039-9. [DOI] [PubMed] [Google Scholar]
- 15.Bellmunt J, Szczylik C, Feingold J, Strahs A, Berkenblit A. Temsirolimus safety profile and management of toxic effects in patients with advanced renal cell carcinoma and poor prognostic features. Ann Oncol. 2008;19(8):1387–92. doi: 10.1093/annonc/mdn066. [DOI] [PubMed] [Google Scholar]
- 16.Escudier B, Eisen T, Stadler WM, Szczylik C, Oudard S, Staehler M, Negrier S, Chevreau C, Desai AA, Rolland F, et al. Sorafenib for treatment of renal cell carcinoma: Final efficacy and safety results of the phase III treatment approaches in renal cancer global evaluation trial. J Clin Oncol. 2009;27(20):3312–8. doi: 10.1200/JCO.2008.19.5511. [DOI] [PubMed] [Google Scholar]
- 17.Hudes G, Carducci M, Tomczak P, Dutcher J, Figlin R, Kapoor A, Staroslawska E, Sosman J, McDermott D, Bodrogi I, et al. Temsirolimus, interferon alfa, or both for advanced renal-cell carcinoma. N Engl J Med. 2007;356(22):2271–81. doi: 10.1056/NEJMoa066838. [DOI] [PubMed] [Google Scholar]
- 18.Sternberg CN, Davis ID, Mardiak J, Szczylik C, Lee E, Wagstaff J, Barrios CH, Salman P, Gladkov OA, Kavina A, et al. Pazopanib in locally advanced or metastatic renal cell carcinoma: results of a randomized phase III trial. J Clin Oncol. 2011;28(6):1061–8. doi: 10.1200/JCO.2009.23.9764. [DOI] [PubMed] [Google Scholar]
- 19.Rini BI, Escudier B, Tomczak P, Kaprin A, Szczylik C, Hutson TE, Michaelson MD, Gorbunova VA, Gore ME, Rusakov IG, et al. Comparative effectiveness of axitinib versus sorafenib in advanced renal cell carcinoma (AXIS): a randomised phase 3 trial. Lancet. 2012;378(9807):1931–9. doi: 10.1016/S0140-6736(11)61613-9. [DOI] [PubMed] [Google Scholar]
- 20.Escudier B, Pluzanska A, Koralewski P, Ravaud A, Bracarda S, Szczylik C, Chevreau C, Filipek M, Melichar B, Bajetta E, et al. Bevacizumab plus interferon alfa-2a for treatment of metastatic renal cell carcinoma: a randomised, double-blind phase III trial. Lancet. 2007;370(9605):2103–11. doi: 10.1016/S0140-6736(07)61904-7. [DOI] [PubMed] [Google Scholar]
- 21.Yang JC, Hughes M, Kammula U, Royal R, Sherry RM, Topalian SL, Suri KB, Levy C, Allen T, Mavroukakis S, et al. Ipilimumab (anti-CTLA4 antibody) causes regression of metastatic renal cell cancer associated with enteritis and hypophysitis. J Immunother. 2007;30(8):825–30. doi: 10.1097/CJI.0b013e318156e47e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Brahmer JR, Tykodi SS, Chow LQ, Hwu WJ, Topalian SL, Hwu P, Drake CG, Camacho LH, Kauh J, Odunsi K, et al. Safety and activity of anti-PD-L1 antibody in patients with advanced cancer. N Engl J Med. 2012;366(26):2455–65. doi: 10.1056/NEJMoa1200694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Motzer RJ, Escudier B, McDermott DF, George S, Hammers HJ, Srinivas S, Tykodi SS, Sosman JA, Procopio G, Plimack ER, et al. Nivolumab versus Everolimus in Advanced Renal-Cell Carcinoma. N Engl J Med. 2015;373(19):1803–13. doi: 10.1056/NEJMoa1510665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mahesh S, Kaskel F. Growth hormone axis in chronic kidney disease. Pediatr Nephrol. 2008;23(1):41–8. doi: 10.1007/s00467-007-0527-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Brahmkhatri VP, Prasanna C, Atreya HS. Insulin-like growth factor system in cancer: novel targeted therapies. BioMed Research International. 2015;2015:538019. doi: 10.1155/2015/538019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Renehan AG, Zwahlen M, Minder C, O'Dwyer ST, Shalet SM, Egger M. Insulin-like growth factor (IGF)-I, IGF binding protein-3, and cancer risk: systematic review and meta-regression analysis. Lancet. 2004;363(9418):1346–53. doi: 10.1016/S0140-6736(04)16044-3. [DOI] [PubMed] [Google Scholar]
- 27.Baker J, Liu JP, Robertson EJ, Efstratiadis A. Role of insulin-like growth factors in embryonic and postnatal growth. Cell. 1993;75(1):73–82. doi: 10.1016/S0092-8674(05)80085-6. [DOI] [PubMed] [Google Scholar]
- 28.Roddam AW, Allen NE, Appleby P, Key TJ, Ferrucci L, Carter HB, Metter EJ, Chen C, Weiss NS, Fitzpatrick A, et al. Insulin-like growth factors, their binding proteins, and prostate cancer risk: analysis of individual patient data from 12 prospective studies. Ann Intern Med. 2008;149(7):461–71. doi: 10.7326/0003-4819-149-7-200810070-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Key TJ, Appleby PN, Reeves GK, Roddam AW. Insulin-like growth factor 1 (IGF1), IGF binding protein 3 (IGFBP3), and breast cancer risk: pooled individual data analysis of 17 prospective studies. Lancet Oncol. 2010;11(6):530–42. doi: 10.1016/S1470-2045(10)70095-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rinaldi S, Cleveland R, Norat T, Biessy C, Rohrmann S, Linseisen J, Boeing H, Pischon T, Panico S, Agnoli C, et al. Serum levels of IGF-I, IGFBP-3 and colorectal cancer risk: results from the EPIC cohort, plus a meta-analysis of prospective studies. Int J Cancer. 2010;126(7):1702–15. doi: 10.1002/ijc.24927. [DOI] [PubMed] [Google Scholar]
- 31.Clayton PE, Banerjee I, Murray PG, Renehan AG. Growth hormone, the insulin-like growth factor axis, insulin and cancer risk. Nat Rev Endocrinol. 2011;7(1):11–24. doi: 10.1038/nrendo.2010.171. [DOI] [PubMed] [Google Scholar]
- 32.Olivo-Marston SE, Hursting SD, Lavigne J, Perkins SN, Maarouf RS, Yakar S, Harris CC. Genetic reduction of circulating insulin-like growth factor-1 inhibits azoxymethane-induced colon tumorigenesis in mice. Mol Carcinog. 2009;48(12):1071–6. doi: 10.1002/mc.20577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Laron Z. Laron syndrome (primary growth hormone resistance or insensitivity): the personal experience 1958–2003. J Clin Endocrinol Metab. 2004;89(3):1031–44. doi: 10.1210/jc.2003-031033. [DOI] [PubMed] [Google Scholar]
- 34.Steuerman R, Shevah O, Laron Z. Congenital IGF1 deficiency tends to confer protection against post-natal development of malignancies. Eur J Endocrinol. 2011;164(4):485–9. doi: 10.1530/EJE-10-0859. [DOI] [PubMed] [Google Scholar]
- 35.Weinstein D, Sarfstein R, Laron Z, Werner H. Insulin receptor compensates for IGF1R inhibition and directly induces mitogenic activity in prostate cancer cells. Endocrine Connections. 2014;3(1):24–35. doi: 10.1530/EC-13-0086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Singh P, Alex JM, Bast F. Insulin receptor (IR) and insulin-like growth factor receptor 1 (IGF-1R) signaling systems: novel treatment strategies for cancer. Med Oncol. 2014;31(1):805. doi: 10.1007/s12032-013-0805-3. [DOI] [PubMed] [Google Scholar]
- 37.Vigneri PG, Tirro E, Pennisi MS, Massimino M, Stella S, Romano C, Manzella L. The Insulin/IGF System in Colorectal Cancer Development and Resistance to Therapy. Frontiers in Oncology. 2015;5:230. doi: 10.3389/fonc.2015.00230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Frasca F, Pandini G, Scalia P, Sciacca L, Mineo R, Costantino A, Goldfine ID, Belfiore A, Vigneri R. Insulin receptor isoform A, a newly recognized, high-affinity insulin-like growth factor II receptor in fetal and cancer cells. Mol Cell Biol. 1999;19(5):3278–88. doi: 10.1128/MCB.19.5.3278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Belfiore A, Frasca F, Pandini G, Sciacca L, Vigneri R. Insulin receptor isoforms and insulin receptor/insulin-like growth factor receptor hybrids in physiology and disease. Endocr Rev. 2009;30(6):586–623. doi: 10.1210/er.2008-0047. [DOI] [PubMed] [Google Scholar]
- 40.De Meyts P, Whittaker J. Structural biology of insulin and IGF1 receptors: implications for drug design. Nat Rev Drug Discov. 2002;1(10):769–83. doi: 10.1038/nrd917. [DOI] [PubMed] [Google Scholar]
- 41.Tao Y, Pinzi V, Bourhis J, Deutsch E. Mechanisms of disease: signaling of the insulin-like growth factor 1 receptor pathway--therapeutic perspectives in cancer. Nat Clin Pract Oncol. 2007;4(10):591–602. doi: 10.1038/ncponc0934. [DOI] [PubMed] [Google Scholar]
- 42.Chitnis MM, Yuen JS, Protheroe AS, Pollak M, Macaulay VM. The type 1 insulin-like growth factor receptor pathway. Clin Cancer Res. 2008;14(20):6364–70. doi: 10.1158/1078-0432.CCR-07-4879. [DOI] [PubMed] [Google Scholar]
- 43.Aleksic T, Chitnis MM, Perestenko OV, Gao S, Thomas PH, Turner GD, Protheroe AS, Howarth M, Macaulay VM. Type 1 insulin-like growth factor receptor translocates to the nucleus of human tumor cells. Cancer Res. 2010;70(16):6412–9. doi: 10.1158/0008-5472.CAN-10-0052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Werner H. Tumor suppressors govern insulin-like growth factor signaling pathways: implications in metabolism and cancer. Oncogene. 2012;31(22):2703–14. doi: 10.1038/onc.2011.447. [DOI] [PubMed] [Google Scholar]
- 45.Gualberto A, Pollak M. Emerging role of insulin-like growth factor receptor inhibitors in oncology: early clinical trial results and future directions. Oncogene. 2009;28(34):3009–21. doi: 10.1038/onc.2009.172. [DOI] [PubMed] [Google Scholar]
- 46.Ouban A, Muraca P, Yeatman T, Coppola D. Expression and distribution of insulin-like growth factor-1 receptor in human carcinomas. Hum Pathol. 2003;34(8):803–8. doi: 10.1016/S0046-8177(03)00291-0. [DOI] [PubMed] [Google Scholar]
- 47.Hartog H, Wesseling J, Boezen HM, van der Graaf WT. The insulin-like growth factor 1 receptor in cancer: old focus, new future. Eur J Cancer. 2007;43(13):1895–904. doi: 10.1016/j.ejca.2007.05.021. [DOI] [PubMed] [Google Scholar]
- 48.Pollak M. Insulin and insulin-like growth factor signalling in neoplasia. Nat Rev Cancer. 2008;8(12):915–28. doi: 10.1038/nrc2536. [DOI] [PubMed] [Google Scholar]
- 49.Carboni JM, Lee AV, Hadsell DL, Rowley BR, Lee FY, Bol DK, Camuso AE, Gottardis M, Greer AF, Ho CP, et al. Tumor development by transgenic expression of a constitutively active insulin-like growth factor I receptor. Cancer Res. 2005;65(9):3781–7. doi: 10.1158/0008-5472.CAN-04-4602. [DOI] [PubMed] [Google Scholar]
- 50.Jones RA, Campbell CI, Gunther EJ, Chodosh LA, Petrik JJ, Khokha R, Moorehead RA. Transgenic overexpression of IGF-IR disrupts mammary ductal morphogenesis and induces tumor formation. Oncogene. 2007;26(11):1636–44. doi: 10.1038/sj.onc.1209955. [DOI] [PubMed] [Google Scholar]
- 51.Rosendahl AH, Forsberg G. IGF-I and IGFBP-3 augment transforming growth factor-beta actions in human renal carcinoma cells. Kidney Int. 2006;70(9):1584–90. doi: 10.1038/sj.ki.5001805. [DOI] [PubMed] [Google Scholar]
- 52.Werner H, Sarfstein R. Transcriptional and epigenetic control of IGF1R gene expression: implications in metabolism and cancer. Growth Horm IGF Res. 2014;24(4):112–8. doi: 10.1016/j.ghir.2014.03.006. [DOI] [PubMed] [Google Scholar]
- 53.Werner H, Shalita-Chesner M, Abramovitch S, Idelman G, Shaharabani-Gargir L, Glaser T. Regulation of the insulin-like growth factor-I receptor gene by oncogenes and antioncogenes: implications in human cancer. Mol Genet Metab. 2000;71(1–2):315–20. doi: 10.1006/mgme.2000.3044. [DOI] [PubMed] [Google Scholar]
- 54.Werner H, Karnieli E, Rauscher FJ, LeRoith D. Wild-type and mutant p53 differentially regulate transcription of the insulin-like growth factor I receptor gene. Proc Natl Acad Sci U S A. 1996;93(16):8318–23. doi: 10.1073/pnas.93.16.8318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Maor S, Yosepovich A, Papa MZ, Yarden RI, Mayer D, Friedman E, Werner H. Elevated insulin-like growth factor-I receptor (IGF-IR) levels in primary breast tumors associated with BRCA1 mutations. Cancer Lett. 2007;257(2):236–43. doi: 10.1016/j.canlet.2007.07.019. [DOI] [PubMed] [Google Scholar]
- 56.Maor S, Papa MZ, Yarden RI, Friedman E, Lerenthal Y, Lee SW, Mayer D, Werner H. Insulin-like growth factor-I controls BRCA1 gene expression through activation of transcription factor Sp1. Horm Metab Res. 2007;39(3):179–85. doi: 10.1055/s-2007-970415. [DOI] [PubMed] [Google Scholar]
- 57.Werner H, Rauscher FJ, 3rd, Sukhatme VP, Drummond IA, Roberts CT, Jr, LeRoith D. Transcriptional repression of the insulin-like growth factor I receptor (IGF-I-R) gene by the tumor suppressor WT1 involves binding to sequences both upstream and downstream of the IGF-I-R gene transcription start site. J Biol Chem. 1994;269(17):12577–82. [PubMed] [Google Scholar]
- 58.Ohlsson C, Kley N, Werner H, LeRoith D. p53 regulates insulin-like growth factor-I (IGF-I) receptor expression and IGF-I-induced tyrosine phosphorylation in an osteosarcoma cell line: interaction between p53 and Sp1. Endocrinology. 1998;139(3):1101–7. doi: 10.1210/endo.139.3.5832. [DOI] [PubMed] [Google Scholar]
- 59.Liu B, Li D, Guan YF. BRCA1 regulates insulin-like growth factor 1 receptor levels in ovarian cancer. Oncol Lett. 2014;7(5):1733–7. doi: 10.3892/ol.2014.1929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Winder T, Zhang W, Yang D, Ning Y, Bohanes P, Gerger A, Wilson PM, Pohl A, Mauro DJ, Langer C, et al. Germline polymorphisms in genes involved in the IGF1 pathway predict efficacy of cetuximab in wild-type KRAS mCRC patients. Clin Cancer Res. 2010;16(22):5591–602. doi: 10.1158/1078-0432.CCR-10-2092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Dong X, Javle M, Hess KR, Shroff R, Abbruzzese JL, Li D. Insulin-like growth factor axis gene polymorphisms and clinical outcomes in pancreatic cancer. Gastroenterology. 2010;139(2):464–73. doi: 10.1053/j.gastro.2010.04.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Sarfstein R, Belfiore A, Werner H. Identification of Insulin-Like Growth Factor-I Receptor (IGF-IR) Gene Promoter-Binding Proteins in Estrogen Receptor (ER)-Positive and ER-Depleted Breast Cancer Cells. Cancers (Basel) 2010;2(2):233–61. doi: 10.3390/cancers2020233. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 63.Yuen JS, Cockman ME, Sullivan M, Protheroe A, Turner GD, Roberts IS, Pugh CW, Werner H, Macaulay VM. The VHL tumor suppressor inhibits expression of the IGF1R and its loss induces IGF1R upregulation in human clear cell renal carcinoma. Oncogene. 2007;26(45):6499–508. doi: 10.1038/sj.onc.1210474. [DOI] [PubMed] [Google Scholar]
- 64.Clemmons DR. Modifying IGF1 activity: an approach to treat endocrine disorders, atherosclerosis and cancer. Nat Rev Drug Discov. 2007;6(10):821–33. doi: 10.1038/nrd2359. [DOI] [PubMed] [Google Scholar]
- 65.Kamenicky P, Mazziotti G, Lombes M, Giustina A, Chanson P. Growth hormone, insulin-like growth factor-1, and the kidney: pathophysiological and clinical implications. Endocr Rev. 2014;35(2):234–81. doi: 10.1210/er.2013-1071. [DOI] [PubMed] [Google Scholar]
- 66.Chin E, Zhou J, Bondy C. Anatomical relationships in the patterns of insulin-like growth factor (IGF)-I, IGF binding protein-1, and IGF-I receptor gene expression in the rat kidney. Endocrinology. 1992;130(6):3237–45. doi: 10.1210/endo.130.6.1375897. [DOI] [PubMed] [Google Scholar]
- 67.Han VK, Hill DJ, Strain AJ, Towle AC, Lauder JM, Underwood LE, D'Ercole AJ. Identification of somatomedin/insulin-like growth factor immunoreactive cells in the human fetus. Pediatr Res. 1987;22(3):245–9. doi: 10.1203/00006450-198709000-00001. [DOI] [PubMed] [Google Scholar]
- 68.Guler HP, Schmid C, Zapf J, Froesch ER. Effects of recombinant insulin-like growth factor I on insulin secretion and renal function in normal human subjects. Proc Natl Acad Sci U S A. 1989;86(8):2868–72. doi: 10.1073/pnas.86.8.2868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Chin E, Bondy C. Insulin-like growth factor system gene expression in the human kidney. J Clin Endocrinol Metab. 1992;75(3):962–8. doi: 10.1210/jcem.75.3.1381376. [DOI] [PubMed] [Google Scholar]
- 70.Kamenicky P, Viengchareun S, Blanchard A, Meduri G, Zizzari P, Imbert-Teboul M, Doucet A, Chanson P, Lombes M. Epithelial sodium channel is a key mediator of growth hormone-induced sodium retention in acromegaly. Endocrinology. 2008;149(7):3294–305. doi: 10.1210/en.2008-0143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Furstenberger G, Senn HJ. Insulin-like growth factors and cancer. Lancet Oncol. 2002;3(5):298–302. doi: 10.1016/S1470-2045(02)00731-3. [DOI] [PubMed] [Google Scholar]
- 72.Valentinis B, Baserga R. IGF-I receptor signalling in transformation and differentiation. Mol Pathol. 2001;54(3):133–7. doi: 10.1136/mp.54.3.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Lindenbergh-Kortleve DJ, Rosato RR, van Neck JW, Nauta J, van Kleffens M, Groffen C, Zwarthoff EC, Drop SL. Gene expression of the insulin-like growth factor system during mouse kidney development. Mol Cell Endocrinol. 1997;132(1–2):81–91. doi: 10.1016/S0303-7207(97)00123-8. [DOI] [PubMed] [Google Scholar]
- 74.Parker AS, Cheville JC, Blute ML, Igel T, Lohse CM, Cerhan JR. Pathologic T1 clear cell renal cell carcinoma: insulin-like growth factor-I receptor expression and disease-specific survival. Cancer. 2004;100(12):2577–82. doi: 10.1002/cncr.20322. [DOI] [PubMed] [Google Scholar]
- 75.Tanaka T, Kondo S, Iwasa Y, Hiai H, Toyokuni S. Expression of stress-response and cell proliferation genes in renal cell carcinoma induced by oxidative stress. Am J Pathol. 2000;156(6):2149–57. doi: 10.1016/S0002-9440(10)65085-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Lissoni P, Barni S, Ardizzoia A, Frigerio F, Paolorossi F, Cazzaniga M, Tancini G, Rocco F, Aapro M. Clinical efficacy of cancer subcutaneous immunotherapy with interleukin-2 in relation to the pretreatment levels of tumor growth factor insulin-like growth factor-1. Tumori. 1995;81(4):261–4. doi: 10.1177/030089169508100409. [DOI] [PubMed] [Google Scholar]
- 77.Cheung CW, Vesey DA, Nicol DL, Johnson DW. The roles of IGF-I and IGFBP-3 in the regulation of proximal tubule, and renal cell carcinoma cell proliferation. Kidney Int. 2004;65(4):1272–9. doi: 10.1111/j.1523-1755.2004.00535.x. [DOI] [PubMed] [Google Scholar]
- 78.Jungwirth A, Schally AV, Pinski J, Groot K, Armatis P, Halmos G. Growth hormone-releasing hormone antagonist MZ-4-71 inhibits in vivo proliferation of Caki-I renal adenocarcinoma. Proc Natl Acad Sci U S A. 1997;94(11):5810–3. doi: 10.1073/pnas.94.11.5810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Rasmuson T, Grankvist K, Jacobsen J, Olsson T, Ljungberg B. Serum insulin-like growth factor-1 is an independent predictor of prognosis in patients with renal cell carcinoma. Acta Oncol. 2004;43(8):744–8. doi: 10.1080/02841860410017260. [DOI] [PubMed] [Google Scholar]
- 80.Major JM, Pollak MN, Snyder K, Virtamo J, Albanes D. Insulin-like growth factors and risk of kidney cancer in men. Br J Cancer. 2010;103(1):132–5. doi: 10.1038/sj.bjc.6605722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Perks CM, Holly JM. Epigenetic regulation of insulin-like growth factor binding protein-3 (IGFBP-3) in cancer. J Cell Communication and Signaling. 2015;9(2):159–66. doi: 10.1007/s12079-015-0294-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Parker A, Cheville JC, Lohse C, Cerhan JR, Blute ML. Expression of insulin-like growth factor I receptor and survival in patients with clear cell renal cell carcinoma. J Urol. 2003;170(2 Pt 1):420–4. doi: 10.1097/01.ju.0000071474.70103.92. [DOI] [PubMed] [Google Scholar]
- 83.Ahmad N, Keehn CA, Coppola D. The expression of insulin-like growth factor-I receptor correlates with Fuhrman grading of renal cell carcinomas. Hum Pathol. 2004;35(9):1132–6. doi: 10.1016/j.humpath.2004.05.012. [DOI] [PubMed] [Google Scholar]
- 84.Belfiore A, Frasca F. IGF and insulin receptor signaling in breast cancer. J Mammary Gland Biol Neoplasia. 2008;13(4):381–406. doi: 10.1007/s10911-008-9099-z. [DOI] [PubMed] [Google Scholar]
- 85.Beauchamp MC, Yasmeen A, Knafo A, Gotlieb WH. Targeting insulin and insulin-like growth factor pathways in epithelial ovarian cancer. J Oncol. 2008;2010:257058. doi: 10.1155/2010/257058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Chuang ST, Patton KT, Schafernak KT, Papavero V, Lin F, Baxter RC, Teh BT, Yang XJ. Over expression of insulin-like growth factor binding protein 3 in clear cell renal cell carcinoma. J Urol. 2008;179(2):445–9. doi: 10.1016/j.juro.2007.09.106. [DOI] [PubMed] [Google Scholar]
- 87.Lkhagvadorj S, Oh SS, Lee MR, Jung JH, Chung HC, Cha SK, Eom M. Insulin receptor expression in clear cell renal cell carcinoma and its relation to prognosis. Yonsei Med J. 2014;55(4):861–70. doi: 10.3349/ymj.2014.55.4.861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Latif F, Tory K, Gnarra J, Yao M, Duh FM, Orcutt ML, Stackhouse T, Kuzmin I, Modi W, Geil L, et al. Identification of the von Hippel-Lindau disease tumor suppressor gene. Science. 1993;260(5112):1317–20. doi: 10.1126/science.8493574. [DOI] [PubMed] [Google Scholar]
- 89.Nickerson ML, Jaeger E, Shi Y, Durocher JA, Mahurkar S, Zaridze D, Matveev V, Janout V, Kollarova H, Bencko V, et al. Improved identification of von Hippel-Lindau gene alterations in clear cell renal tumors. Clin Cancer Res. 2008;14(15):4726–34. doi: 10.1158/1078-0432.CCR-07-4921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Banks RE, Tirukonda P, Taylor C, Hornigold N, Astuti D, Cohen D, Maher ER, Stanley AJ, Harnden P, Joyce A, et al. Genetic and epigenetic analysis of von Hippel-Lindau (VHL) gene alterations and relationship with clinical variables in sporadic renal cancer. Cancer Res. 2006;66(4):2000–11. doi: 10.1158/0008-5472.CAN-05-3074. [DOI] [PubMed] [Google Scholar]
- 91.Finley DS, Pantuck AJ, Belldegrun AS. Tumor biology and prognostic factors in renal cell carcinoma. Oncologist. 2011;16(Suppl 2):4–13. doi: 10.1634/theoncologist.2011-S2-04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Dorff TB, Goldkorn A, Quinn DI. Targeted therapy in renal cancer. Ther Adv Med Oncol. 2009;1(3):183–205. doi: 10.1177/1758834009349119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Kim DS, Choi YB, Han BG, Park SY, Jeon Y, Kim DH, Ahn ER, Shin JE, Lee BI, Lee H, et al. Cancer cells promote survival through depletion of the von Hippel-Lindau tumor suppressor by protein crosslinking. Oncogene. 2011;30(48):4780–90. doi: 10.1038/onc.2011.183. [DOI] [PubMed] [Google Scholar]
- 94.Datta K, Nambudripad R, Pal S, Zhou M, Cohen HT, Mukhopadhyay D. Inhibition of insulin-like growth factor-I-mediated cell signaling by the von Hippel-Lindau gene product in renal cancer. J Biol Chem. 2000;275(27):20700–6. doi: 10.1074/jbc.M909970199. [DOI] [PubMed] [Google Scholar]
- 95.He X, Wang J, Messing EM, Wu G. Regulation of receptor for activated C kinase 1 protein by the von Hippel-Lindau tumor suppressor in IGF-I-induced renal carcinoma cell invasiveness. Oncogene. 2011;30(5):535–47. doi: 10.1038/onc.2010.427. [DOI] [PubMed] [Google Scholar]
- 96.Gnarra JR, Tory K, Weng Y, Schmidt L, Wei MH, Li H, Latif F, Liu S, Chen F, Duh FM, et al. Mutations of the VHL tumour suppressor gene in renal carcinoma. Nat Genet. 1994;7(1):85–90. doi: 10.1038/ng0594-85. [DOI] [PubMed] [Google Scholar]
- 97.Gristina V, Cupri MG, Torchio M, Mezzogori C, Cacciabue L, Danova M. Diabetes and cancer: A critical appraisal of the pathogenetic and therapeutic links. Biomed Rep. 2014;3(2):131–6. doi: 10.3892/br.2014.399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Sarfstein R, Werner H. Minireview: nuclear insulin and insulin-like growth factor-1 receptors: a novel paradigm in signal transduction. Endocrinology. 2013;154(5):1672–9. doi: 10.1210/en.2012-2165. [DOI] [PubMed] [Google Scholar]
- 99.Sarfstein R, Friedman Y, Attias-Geva Z, Fishman A, Bruchim I, Werner H. Metformin downregulates the insulin/IGF-I signaling pathway and inhibits different uterine serous carcinoma (USC) cells proliferation and migration in p53-dependent or -independent manners. PLoS One. 2013;8(4):e61537. doi: 10.1371/journal.pone.0061537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.MRCRC Collaborators. Interferon-alpha and survival in metastatic renal carcinoma: early results of a randomised controlled trial. Medical Research Council Renal Cancer Collaborators. Lancet. 1999;353(9146):14–7. [PubMed]
- 101.Motzer RJ, Hutson TE, Cella D, Reeves J, Hawkins R, Guo J, Nathan P, Staehler M, de Souza P, Merchan JR, et al. Pazopanib versus sunitinib in metastatic renal-cell carcinoma. N Engl J Med. 2013;369(8):722–31. doi: 10.1056/NEJMoa1303989. [DOI] [PubMed] [Google Scholar]
- 102.Rini BI, Halabi S, Rosenberg JE, Stadler WM, Vaena DA, Ou SS, Archer L, Atkins JN, Picus J, Czaykowski P, et al. Bevacizumab plus interferon alfa compared with interferon alfa monotherapy in patients with metastatic renal cell carcinoma: CALGB 90206. J Clin Oncol. 2008;26(33):5422–8. doi: 10.1200/JCO.2008.16.9847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Neuhausen SL, Brummel S, Ding YC, Singer CF, Pfeiler G, Lynch HT, Nathanson KL, Rebbeck TR, Garber JE, Couch F, et al. Genetic variation in insulin-like growth factor signaling genes and breast cancer risk among BRCA1 and BRCA2 carriers. Breast Cancer Res. 2009;11(5):R76. doi: 10.1186/bcr2414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Lonn S, Rothman N, Shapiro WR, Fine HA, Selker RG, Black PM, Loeffler JS, Hutchinson AA, Inskip PD. Genetic variation in insulin-like growth factors and brain tumor risk. Neuro Oncol. 2008;10(4):553–9. doi: 10.1215/15228517-2008-026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Diorio C, Brisson J, Berube S, Pollak M. Genetic polymorphisms involved in insulin-like growth factor (IGF) pathway in relation to mammographic breast density and IGF levels. Cancer Epidemiol Biomarkers Prev. 2008;17(4):880–8. doi: 10.1158/1055-9965.EPI-07-2500. [DOI] [PubMed] [Google Scholar]
- 106.Reinmuth N, Kloos S, Warth A, Risch A, Muley T, Hoffmann H, Thomas M, Meister M. Insulin-like growth factor 1 pathway mutations and protein expression in resected non-small cell lung cancer. Hum Pathol. 2014;45(6):1162–8. doi: 10.1016/j.humpath.2014.01.010. [DOI] [PubMed] [Google Scholar]
- 107.Dziadziuszko R, Merrick DT, Witta SE, Mendoza AD, Szostakiewicz B, Szymanowska A, Rzyman W, Dziadziuszko K, Jassem J, Bunn PA, Jr, et al. Insulin-like growth factor receptor 1 (IGF1R) gene copy number is associated with survival in operable non-small-cell lung cancer: a comparison between IGF1R fluorescent in situ hybridization, protein expression, and mRNA expression. J Clin Oncol. 2010;28(13):2174–80. doi: 10.1200/JCO.2009.24.6611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Bax DA, Mackay A, Little SE, Carvalho D, Viana-Pereira M, Tamber N, Grigoriadis AE, Ashworth A, Reis RM, Ellison DW, et al. A distinct spectrum of copy number aberrations in pediatric high-grade gliomas. Clin Cancer Res. 2010;16(13):3368–77. doi: 10.1158/1078-0432.CCR-10-0438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Lynn M, Shah N, Conroy J, Ennis S, Morris T, Betts D, O'Sullivan M. A Study of Alveolar Rhabdomyosarcoma Copy Number Alterations by Single Nucleotide Polymorphism Analysis. Diagn Mol Pathol. 2014. [DOI] [PubMed]
- 110.Craddock BP, Miller WT. Effects of somatic mutations in the C-terminus of insulin-like growth factor 1 receptor on activity and signaling. J Signal Transduct. 2012;2012:804801. doi: 10.1155/2012/804801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Shitara M, Okuda K, Suzuki A, Tatematsu T, Hikosaka Y, Moriyama S, Sasaki H, Fujii Y, Yano M. Genetic profiling of thymic carcinoma using targeted next-generation sequencing. Lung Cancer. 2014;86(2):174–9. doi: 10.1016/j.lungcan.2014.08.020. [DOI] [PubMed] [Google Scholar]
- 112.de Alencar SA, Lopes JC. A comprehensive in silico analysis of the functional and structural impact of SNPs in the IGF1R gene. J Biomed Biotechnol. 2010;2010:715139. doi: 10.1155/2010/715139. [DOI] [PMC free article] [PubMed] [Google Scholar]


