Abstract
Infections by Carbapenem-Resistant Enterobacteriaceae (CRE), in particular, carbapenem-resistant Klebsiella pneumoniae (CRKp), are a significant public health challenge worldwide. Resistance to carbapenems in enterobacteriaceae is linked to different mechanisms, including the production of the various types of enzymes like KPC, VIM, IMP, NDM, and OXA-48. Despite several attempts to control the spread of these infections at the local and national level, the epidemiological situation for CRKp had worsened in the last years in the Mediterranean area. The rate and types of CRKp isolates greatly differ in the various Mediterranean countries. KPC-producing K. pneumoniae is diffused particularly in the European countries bordering the Mediterranean Sea and is endemic in Greece and Italy. On the contrary, OXA-48-producing K. pneumoniae is endemic in Turkey and Malta and diffused at inter-regional level particularly in some
North African and Middle East countries. The spread of these multiresistant pathogens in the world and the Mediterranean countries has been related to various epidemiological factors including the international transfer of patients coming from endemic areas.
Introduction
Infections by Carbapenem-Resistant Enterobacteriaceae (CRE), in particular carbapenem-resistant Klebsiella pneumoniae (CRKp), are a significant public health challenge worldwide.1–4 These pathogens are characterized by multiantibiotic resistance which involves penicillins, all cephalosporins, monobactams, carbapenems, and even β-lactamase inhibitors. They are generally only susceptible to a few antibiotics, and there is high mortality among patients with bloodstream infections caused by these organisms. Many CRKp isolates remain susceptible to colistin, tigecycline, and one or more aminoglycoside, but some are resistant even to these drugs.5,6 Moreover, only a few drugs are in development against CRE.7 The prognosis of infections by CRKp is particularly poor in high risk immunocompromised populations as intensive care unit (ICU), solid organ transplant (SOT), hematological malignancies (HEM) and stem cell transplant (SCT) patients.8–15
Resistance to carbapenems in enterobacteriaceae is linked to different mechanisms, in particular the production of strong carbapenemases, but also of beta-lactamases that possess weak carbapenemase activity when combined with decreased permeability due to porin loss or alteration. Strong carbapenemases that are responsible for nonsusceptibility to carbapenems, without additional permeability defects, belong to Ambler molecular class A, B, or D. These enzymes are carried either on chromosome or acquired via plasmids.16,17
K. pneumoniae carbapenemase (KPC) enzymes are currently the most clinically significant enzymes among the class A carbapenemases. KPC producing K. pneumoniae had the widest dissemination in the last few years being diffused with important regional, interregional and endemic spread in several countries. To date, more than 20 different KPC variants have been described, even though KPC-2 and -3 remain the most commonly identified variants.18 The class B beta-lactamases or metallo-beta-lactamases (MBLs) have also been identified in various enterobacterial species, including K. pneumoniae.19 They are mainly New Delhi metallo-beta-lactamase (NDM-1), Verona integron-encoded metallo-beta-lactamase (VIM), and Imipenemase (IMP) type enzymes, with the first group being the most commonly identified worldwide. Carbapenem-hydrolysing oxacillinase-48 (OXA-48) is the most frequently reported class D beta-lactamase and microorganisms producing this enzyme have almost reached the same spread of KPC-producing K. pneumoniae.17,19,20
In 2012, the European Centre for Disease Prevention and Control (ECDC) launched the ‘European survey of carbapenemase-producing Enterobacteriaceae (EuSCAPE)’ project to gain insights into the occurrence and epidemiology of CRE and to increase the awareness of the spread of CRE, in Europe.21 The epidemiological situation for CRKp had worsened since 2010 and CRKp continued to spread in European hospitals, particularly in the Mediterranean area.
The aim of this review is to describe the recent epidemiological data on the diffusion of CRKp infections in Mediterranean countries.
Epidemiology of CRKp in Mediterranean countries
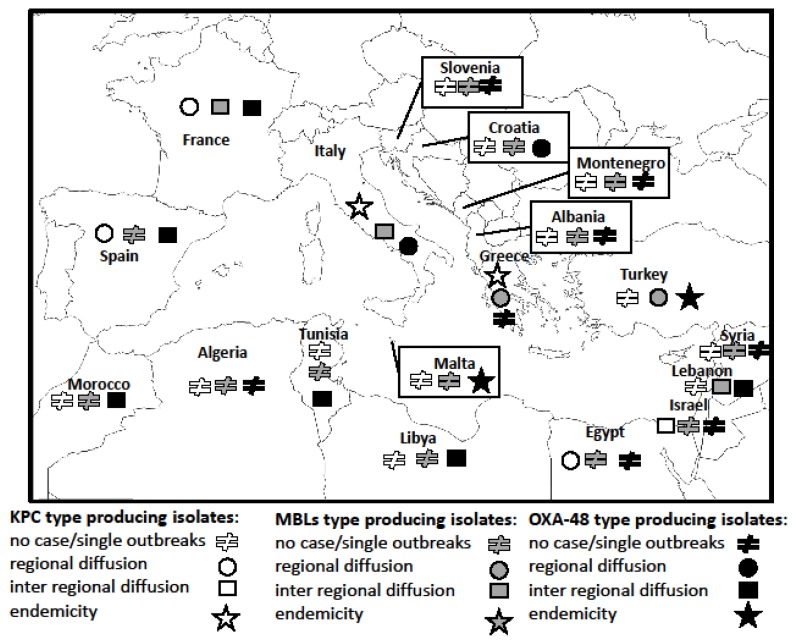
The epidemiology of the various types of CRKp is characterized by a distribution which does not necessarily overlap in the different countries (Figure 1). It is well defined in Europe and Israel where several national and multinational epidemiological surveys have been performed in the last years, on the contrary, the data from North African and Middle East regions, other than Israel, are less accurate.22
Figure 1.
Current epidemiological stages of carbapenem-resistant Klebsiella pneumoniae by type of carbapenemase in the Mediterranean countries
Class A KPC type producing K. pneumoniae
KPC was initially reported from K. pneumoniae strains isolated in the United States in the late 1990s. KPC producing K. pneumoniae has since spread across the United States and the overall prevalence of carbapenem resistance among Klebsiella spp. isolates causing hospital-acquired infections in U.S. hospitals was approximately 12% between 2009 and 2010.23–29 KPC-producing K. pneumoniae has since spread worldwide. The first country besides the United States that experienced a nationwide outbreak was Israel in late 2005 where the pathogen rapidly became endemic.30,31 It was the first outbreak of KPC-producing K. pneumoniae in the Mediterranean area, presumably coming from U.S. Hospital-level interventions were implemented but were unable to contain its spread, therefore in 2007 the Israeli Ministry of Health launched a nationwide intervention, which in few months was able to contain the outbreak nationally, with a 79% relative reduction in the incidence compared with its peak the previous year. In Israel KPC-positive K. pneumoniae was declared as an endemic phenomenon until 2010, while, thanks to the nationwide infection-control intervention, since 2011 the epidemiological scale downgraded to inter-regional spread.32
Since the Israeli epidemic, several sporadic cases and outbreaks of KPC type K. pneumoniae isolates have been reported in many European countries. In 2007 two cases of KPC-2 positive K. pneumoniae infection were diagnosed in France and Sweden, respectively, but both cases were documented in patients transferred from Greece.33,34 In the same year an outbreack of KPC-2-positive K. pneumoniae was reported from a tertiary hospital in Crete and within 2 years of these reports, the multiresistant pathogen disseminated into all Greek tertiary-care hospitals, not only in Intensive Care Units, but also in medical and surgical wards.35–41 According to the data of the European Antimicrobial Resistance Surveillance Network (EARS-Net) of the European Centre for Disease Prevention and Control (ECDC) the epidemiology of KPC-positive K. pneumoniae in Greece was considered at an endemic stage since 2010, and since 2011 the rate of resistance to carbapenems (mainly due to KPC production) was constantly over 60% in invasive K. pneumoniae isolates.42
In Italy, the first KPC-positive K. pneumoniae strains were isolated in 2008 from an inpatient with a complicated intra-abdominal infection in Florence and in 2009 from two patients admitted to a teaching hospital in Rome.43,44 Since then several cases and outbreaks by KPC-2 and KPC-3 K. pneumoniae strains were reported as a consequence of a rapid dissemination in almost all hospitals in the north, middle and south regions of the country.8,9,13,14,45–51 KPC-positive K. pneumoniae have spread rapidly and extensively in Italy, with a sharp increase reported by the EARS-Net surveillance system for bacteraemia isolates, from 1–2% carbapenem resistance in 2006–09 to 26.7% in 2011 and 32.9% in 2014. Since 2013, in Italy the epidemiology of KPC-positive K. pneumoniae was declared at an endemic stage.42
The first two KPC positive K. pneumoniae clinical isolates (one KPC-2 and one KPC-3) in France were found in 2005.52,53 They were recovered from two patients with a recent hospital admission in New York City (USA). A further case was described two years later from a patient transferred from a Greek hospital (see above).33 Subsequently, other nosocomial clusters have been reported, generally related to patients transferred from other European endemic areas.54,55
In 2012, a national reference centre was established to examine all carbapenem-resistant Enterobacteriaceae in France. Throughout 7 months, out of 160 carbapenemase-positive Enterobacteriaceae identified, 19 (11.9%) KPC-producing K. pneumoniae cases were documented.1 Five of these 19 cases were linked to recent stays in Israel, Italy, Kuwait, and China, none was community acquired. According to the EARS-Net data, in 2014 less than 1% of the invasive K. pneumoniae isolates in France were resistant to carbapenems and sporadic hospital outbreaks with no autochthonous inter-institutional transmission have been reported.42,56
The first eight cases of KPC-3-positive K. pneumoniae colonizations reported in Spain have been documented in 2009.57 These patients were in five different wards in a hospital in Madrid, and none had recently travelled to KPC-endemic countries. Since then, sporadic KPC-positive isolates have been identified in the same hospital and in other hospitals in Valencia. A slight increase of KPC-positive K. pneumoniae invasive isolates was observed in the following years in Spain as documented by the EARS-Net surveillance (from 0.3% in 2011 to 2,3% in 2014). In a multicentre prospective epidemiological study carried out in 83 Spanish hospitals from February to May 2013, out of 374 K. pneumoniae isolates 282 (74.4%) were carbapenemase producers but in only 3 (0.1%) cases the carbapenem resistance was related to KPC production.58,59 In the period 2014–2015, KPC-positive K. pneumoniae was reported at regional stage almost exclusively in the territory of Madrid and Valencia.56
To date, only sporadic epidemiological data on KPC-positive K. pneumoniae isolates have been reported in other European countries bordering the Mediterraneum. Forty-eight KPC-2 producing K. pneumoniae isolates, collected during a period from February 2011 to August 2013, were recorded in 9 of 40 centers in Croatia, limited to the northwest region of the country.60,61 According to the EARS-Net data, in 2014 0.9% of the invasive K. pneumoniae isolates in Croatia and Slovenia were resistant to carbapenems.42
A KPC-3 positive K. pneumoniae strain was isolated in Albania in 2014 in an ICU patient with no history of recent travel to endemic areas.62 According to the EuSCAPE data no case of KPC-positive K. pneumoniae has been reported in 2014–2015 from Montenegro, Malta and Turkey.
With regard to North African and the Middle East regions (excluding Israel), in most of the countries, there is no description or only single cases of KPC producers K. pneumoniae isolates.22 A case of KPC-3-producing K. pneumoniae meningitis in a 6-month-old child has been reported in Algeria.63 Three studies from tertiary care hospitals in Egypt showed a high prevalence of KPC related carbapenem non-susceptible K. pneumoniae (70% in one study) isolates suggesting an underestimated epidemiological phenomenon in that country.64–66
Class B MBLs type producing K. pneumoniae
Class B MBLs are mostly of the VIM and IMP types and, more recently, of NDM-1 type.67 IMP-type beta-lactamases were the first acquired MBLs to be identified. They have been detected in a series of clinically relevant Gram-negative bacilli including K. pneumoniae but with a much lower frequency compared all other carbapenemases. IMP producing K. pneumoniae, which is dominant in the Asian continent and Australia, has been only sporadically detected in Europe and the Mediterranean area.22
The VIM type MBL is the most commonly found class B carbapenemase which has been identified in all continents.19,68 Italy was the first Mediterranean country to report acquired MBLs, with sporadic isolates of VIM-4-producing K. pneumoniae.69 Since then, single or sporadic hospital outbreaks caused by VIM-1 like enzymes were described from various regions in this country.70,71 VIM producing K. pneumoniae have not undergone wide dissemination in the other Mediterranean countries, with the exception of Greece where several cases and outbreaks have been reported in the last years.67,72 Finally, single reports and local outbreaks of VIM- type producers have been reported in other countries of the Mediterranean area, such as France,73 Spain,58 Morocco,74 Egypt,75 Algeria,76 and Tunisia.77
The NDM-1 enzyme is a more recently reported class B carbapenemase identified mostly in E.coli and K. pneumoniae and to a lesser extent in other enterobacteriaceae. NDM-1 producers have been reported in the environment and in the community. It arose from India in 2008 and spread rapidly over Indian subcontinent in the following few years and international travel has a significant impact on its rapid worldwide spread.19,78,79 The European epidemiology for CRE changed between 2013 and 2015 for NDM-producing Enterobacteriaceae with several countries reporting regional or inter-regional spread but with no endemic situation. Single or sporadic hospital outbreaks caused by NDM-1 producing K. pneumoniae strains were reported from many countries in the Mediterranean area: France,80 Italy,81 Spain,82,83 Morocco84 Tunisia in a patient transferred from Libya,85 and Egypt.86 In these countries the dissemination of NDM-producing CRE, including K. pneumoniae, was still limited and cases were mostly acquired abroad. Finally, an emergence of autochthonous and imported NDM-1 producing K. pneumoniae was reported in Turkey, especially in hospitals from cities close to the Syrian border, and in Greece.87–90 Sporadic cases or single hospital outbreaks by NDM-1 positive K. pneumoniae have been observed in Lebanon (imported from Iraq), Israel and other Middle East Mediterranean countries.91–93
Class D OXA-48 type producing K. pneumoniae
Class D beta-lactamases, also named OXAs for oxacillinases, have more than 440 known variants with 232 of them showing carbapenemase activity. OXA-48 represents the main enzyme isolated around the world.17 It was initially identified in K. pneumoniae in a strain from Istambul, Turkey in 2001.94 The OXA-48-positive K. pneumoniae strains rapidly diffused in Turkey with hospital outbreaks in the main cities of the country.95 The epidemic was under controlled and in 2015 OXA-48 K. pneumoniae was considered endemic in Turkey.56
Identification of this novel and powerful resistance determinant outside of Turkey indicated that spread was larger than expected. OXA-48 producing isolates disseminated to the Middle East, North Africa and Europe and several nosocomial outbreaks were reported from many Mediterranean countries including France, Spain, Lebanon, Israel, Tunisia and Morocco.97–108 Several cases of OXA-48 K. pneumoniae infections in Libyan refugees transferred to hospitals of European countries have been reported, suggesting that the epidemiology of such multiresistant microorganisms in Libya, and probably in other north African countries, is underestimated.109–113 Dramatic epidemiological findings occurred in Malta where dissemination of OXA-48-producing Enterobacteriaceae had changed the country’s epidemiological level from rare sporadic occurrence before 2010 to an endemic situation by 2013.42,56 Presumably, the influx of injured Libyan war victims to the country’s only tertiary care hospital in 2011 contributed to the first outbreak and spread of OXA-48-producing Enterobacteriaceae in the country. Despite initial control of the outbreak, the situation rapidly became endemic in this hospital and OXA-48-producing K. pneumoniae and other enterobacteria spread to other health and residential care entities on the Maltese islands. EARS-Net data for Malta showed an increase in the percentage of invasive OXA-48–producing K. pneumoniae in Malta, from 3.8% in 2011, to 5.8% in 2013 and 9.9% in 2014.42
In summary, in 2014–2015 the epidemiological stage for the spread of OXA-48 producing K. pneumoniae in the Mediterranean area was: endemic level in Turkey and Malta, inter-regional diffusion in France, Spain, Lebanon, Tunisia, Morocco and Libya, regional diffusion in Italy and Croatia, single or sporadic hospital outbreaks in Israel, Slovenia, Albania, single cases or never reported in Greece, Albania, Montenegro, Syria, Egypt and Algeria.
Conclusions
Despite several attempts to control the spread of CRKp at the local and national level, the epidemiological situation for these multiresistant pathogens had worsened in the last years in the Mediterranean area. The rate and types of CRKp isolates greatly differ in the various countries being the diffusion of these multiresistant pathogens related to various geographic and epidemiological factors including the international transfer of patients coming from endemic areas.
The political and economic relationship and the increasing phenomenon of migration in the Mediterranean basin should lead to a continuous epidemiological survey of multiresistant bacteria in order to define and plan appropriate infection-control intervention at national and international level.
Footnotes
Competing interests: The authors have declared that no competing interests exist.
References
- 1.Munoz-Price LS, Poirel L, Bonomo RA, et al. Clinical epidemiology of the global expansion of Klebsiella pneumoniae carbapenemases. Lancet Infect Dis. 2013;13:785–96. doi: 10.1016/S1473-3099(13)70190-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tzouvelekis LS, Markogiannakis A, Psichogiou M, et al. Carbapenemases in Klebsiella pneumoniae and other Enterobacteriaceae: an evolving crisis of global dimensions. Clin Microbiol Rev. 2012;25:682–707. doi: 10.1128/CMR.05035-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cantón R, Akóva M, Carmeli Y, et al. Rapid evolution and spread of carbapenemases among Enterobacteriaceae in Europe. Clin Microbiol Infect. 2012;18:413–31. doi: 10.1111/j.1469-0691.2012.03821.x. [DOI] [PubMed] [Google Scholar]
- 4.Nordmann P, Poirel L. The difficult-to-control spread of carbapenemae producers in Enterobacteriaceae worldwide. Clin Microbiol Infect. 2014;20:821–30. doi: 10.1111/1469-0691.12719. [DOI] [PubMed] [Google Scholar]
- 5.van Duin D, Doi Y. Outbreak of Colistin-Resistant, Carbapenemase-Producing Klebsiella pneumoniae: Are We at the End of the Road? J Clin Microbiol. 2015;53:3116–7. doi: 10.1128/JCM.01399-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Monaco M, Giani T, Raffone M, et al. Colistin resistance superimposed to endemic carbapenem-resistant Klebsiella pneumoniae: a rapidly evolving problem in Italy, November 2013 to April 2014. Euro Surveill. 2014;19(42) doi: 10.2807/1560-7917.ES2014.19.42.20939. [DOI] [PubMed] [Google Scholar]
- 7.Syue LS, Chen YH, Ko WC, Hsueh PR. New drugs for the treatment of complicated intra-abdominal infections in the era of increasing antimicrobial resistance. Int J Antimicrob Agents. 2016;47:250–8. doi: 10.1016/j.ijantimicag.2015.12.021. [DOI] [PubMed] [Google Scholar]
- 8.Bergamasco MD, Barroso Barbosa M, de Oliveira Garcia D, et al. Infection with Klebsiella pneumoniae carbapenemase (KPC)-producing K. pneumoniae in solid organ transplantation. Transpl Infect Dis. 2012;14:198–205. doi: 10.1111/j.1399-3062.2011.00688.x. [DOI] [PubMed] [Google Scholar]
- 9.Taglietti F, Di Bella S, Galati V, et al. Carbapenemase-producing Klebsiella pneumoniae-related mortality among solid organ-transplanted patients: do we know enough? Transpl Infect Dis. 2013;15:E164–5. doi: 10.1111/tid.12085. [DOI] [PubMed] [Google Scholar]
- 10.Kalpoe JS, Sonnenberg E, Factor SH, et al. Mortality associated with carbapenem-resistant Klebsiella pneumoniae infections in liver transplant recipients. Liver Transpl. 2012;18:468–74. doi: 10.1002/lt.23374. [DOI] [PubMed] [Google Scholar]
- 11.Clancy CJ, Chen L, Shields RK, et al. Epidemiology and molecular characterization of bacteremia due to carbapenem-resistant Klebsiella pneumoniae in transplant recipients. Am J Transplant. 2013;13:2619–33. doi: 10.1111/ajt.12424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Satlin MJ, Jenkins SG, Walsh TJ. The Global Challenge of Carbapenem-Resistant Enterobacteriaceae in Transplant Recipients and Patients With Hematologic Malignancies. Clin Infect Dis. 2014;58:1274–83. doi: 10.1093/cid/ciu052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pagano L, Caira M, Trecarichi EM, et al. Carbapenemase-producing Klebsiella pneumoniae and hematologic malignancies. Emerg Infect Dis. 2014;20:1235–6. doi: 10.3201/eid2007.130094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Girmenia C, Rossolini GM, Piciocchi A, et al. Infections by carbapenem-resistant Klebsiella pneumoniae in stem cell transplant recipients: a nationwide retrospective survey from Italy. Bone Marrow Transplant. 2015;50:282–8. doi: 10.1038/bmt.2014.231. [DOI] [PubMed] [Google Scholar]
- 15.Girmenia C, Viscoli C, Piciocchi A, et al. Management of carbapenem resistant Klebsiella pneumoniae infections in stem cell transplant recipients: an Italian multidisciplinary consensus statement. Haematologica. 2015;100:e373–6. doi: 10.3324/haematol.2015.125484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nordmann P. Carbapenemase-producing Enterobacteriaceae: overview of a major public health challenge. Med Mal Infect. 2014;44:51–6. doi: 10.1016/j.medmal.2013.11.007. [DOI] [PubMed] [Google Scholar]
- 17.Pitout JD, Nordmann P, Poirel L. Carbapenemase-Producing Klebsiella pneumoniae, a Key Pathogen Set for Global Nosocomial Dominance. Antimicrob Agents Chemother. 2015;59:5873–84. doi: 10.1128/AAC.01019-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Walther-Rasmussen J, Hoiby N. Class A carbapenemases. J Antimicrob Chemother. 2007;60:470–482. doi: 10.1093/jac/dkm226. [DOI] [PubMed] [Google Scholar]
- 19.Nordmann P, Naas T, Poirel L. Global spread of carbapenemase producing Enterobacteriaceae. Emerg Infect Dis. 2011;17:1791–1798. doi: 10.3201/eid1710.110655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jean SS, Lee WS, Lam C, Hsu CW, Chen RJ, Hsueh PR. Carbapenemase-producing Gram-negative bacteria: current epidemics, antimicrobial susceptibility and treatment options. Future Microbiol. 2015;10:407–25. doi: 10.2217/fmb.14.135. [DOI] [PubMed] [Google Scholar]
- 21.Glasner C, Albiger B, Buist G, et al. European Survey on Carbapenemase-Producing Enterobacteriaceae (EuSCAPE) Working Group. Carbapenemase-producing Enterobacteriaceae in Europe: a survey among national experts from 39 countries, February 2013. Euro Surveill. 2013;18(28) doi: 10.2807/1560-7917.ES2013.18.28.20525. [DOI] [PubMed] [Google Scholar]
- 22.Djahmi N, Dunyach-Remy C, Pantel A, Dekhil M, Sotto A, Lavigne JP. Epidemiology of carbapenemase-producing Enterobacteriaceae and Acinetobacter baumannii in Mediterranean countries. Biomed Res Int. 2014;2014:305784. doi: 10.1155/2014/305784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rasmussen BA, Bush K. Carbapenem-hydrolyzing β-lactamases. Antimicrob Agents Chemother. 1997;41:223–232. doi: 10.1128/aac.41.2.223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Martínez-Martínez L, Pascual A, Hernández-Allés S, et al. Roles of β-lactamases and porins in activities of carbapenems and cephalosporins against Klebsiella pneumoniae. Antimicrob Agents Chemother. 1999;43:1669–1673. doi: 10.1128/aac.43.7.1669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yigit H, Queenan AM, Anderson GJ, et al. Novel carbapenem-hydrolyzing β-lactamase, KPC-1, from a carbapenem-resistant strain of Klebsiella pneumoniae. Antimicrob Agents Chemother. 2001;45:1151–1161. doi: 10.1128/AAC.45.4.1151-1161.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bradford PA, Bratu S, Urban C, et al. Emergence of carbapenem-resistant Klebsiella species possessing the class A carbapenem-hydrolyzing KPC-2 and inhibitor-resistant TEM-30 β-lactamases in New York City. Clin Infect Dis. 2004;39:55–60. doi: 10.1086/421495. [DOI] [PubMed] [Google Scholar]
- 27.Bratu S, Landman D, Haag R, et al. Rapid spread of carbapenem-resistant Klebsiella pneumoniae in New York City: a new threat to our antibiotic armamentarium. Arch Intern Med. 2005;165:1430–1435. doi: 10.1001/archinte.165.12.1430. [DOI] [PubMed] [Google Scholar]
- 28.Kitchel B, Rasheed JK, Patel JB, et al. Molecular epidemiology of KPC-producing Klebsiella pneumoniae isolates in the United States: clonal expansion of multilocus sequence type 258. Antimicrob Agents Chemother. 2009;53:3365–3370. doi: 10.1128/AAC.00126-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gupta N, Limbago BM, Patel JB, Kallen AJ. Carbapenem-resistant Enterobacteriaceae: epidemiology and prevention. Clin Infect Dis. 2011;53:60–67. doi: 10.1093/cid/cir202. [DOI] [PubMed] [Google Scholar]
- 30.Samra Z, Ofir O, Lishtzinsky Y, Madar-Shapiro L, Bishara J. Outbreak of carbapenem-resistant Klebsiella pneumoniae producing KPC-3 in a tertiary medical centre in Israel. International Journal of Antimicrobial Agents. 2007;30:525–529. doi: 10.1016/j.ijantimicag.2007.07.024. [DOI] [PubMed] [Google Scholar]
- 31.Kitchel, Rasheed JK, J Patel JB, et al. Molecular epidemiology of KPC-producing Klebsiella pneumoniae isolates in the United States: clonal expansion of multilocus sequence type 258. Antimicrobial Agents and Chemotherapy. 2009;53:3365–3370. doi: 10.1128/AAC.00126-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schwaber MJ, Lev B, Israeli A, et al. Containment of a countrywide outbreak of carbapenem-resistant Klebsiella pneumoniae in Israeli hospitals via a nationally implemented intervention. Clin Infect Dis. 2011;52:848–55. doi: 10.1093/cid/cir025. [DOI] [PubMed] [Google Scholar]
- 33.Cuzon G, Naas T, Demachy MC, Nordmann P. Plasmid-mediated carbapenem-hydrolyzing beta-lactamase KPC-2 in Klebsiella pneumoniae isolate from Greece. Antimicrob Agents Chemother. 2008;52:796–97. doi: 10.1128/AAC.01180-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tegmark WK, Haeggman S, Gezelius L, et al. Identification of Klebsiella pneumoniae carbapenemase in Sweden. Euro Surveill. 2007;12:E071220. doi: 10.2807/esw.12.51.03333-en. http://ecdc.europa.eu/en/publications/Publications/antimicrobial-resistance-europe-2014.pdf. [DOI] [PubMed] [Google Scholar]
- 35.Maltezou HC, Giakkoupi P, Maragos A, et al. Outbreak of infections due to KPC-2-producing Klebsiella pneumoniae in a hospital in Crete (Greece) J Infect. 2009;58:213–19. doi: 10.1016/j.jinf.2009.01.010. [DOI] [PubMed] [Google Scholar]
- 36.Pournaras S, Protonotariou E, Voulgari E, et al. Clonal spread of KPC-2 carbapenemase-producing Klebsiella pneumoniae strains in Greece. J Antimicrob Chemother. 2009;64:348–52. doi: 10.1093/jac/dkp207. [DOI] [PubMed] [Google Scholar]
- 37.Souli M, Galani I, Antoniadou A, et al. An outbreak of infection due to beta-lactamase Klebsiella pneumoniae carbapenemase 2-producing K pneumoniae in a Greek University Hospital: molecular characterization, epidemiology, and outcomes. Clin Infect Dis. 2010;50:364–73. doi: 10.1086/649865. [DOI] [PubMed] [Google Scholar]
- 38.Kontopoulou K, Protonotariou E, Vasilakos K, et al. Hospital outbreak caused by Klebsiella pneumoniae producing KPC-2 beta-lactamase resistant to colistin. J Hosp Infect. 2010;76:70–73. doi: 10.1016/j.jhin.2010.03.021. [DOI] [PubMed] [Google Scholar]
- 40.Zarkotou O, Pournaras S, Tselioti P, et al. Predictors of mortality in patients with bloodstream infections caused by KPC-producing Klebsiella pneumoniae and impact of appropriate antimicrobial treatment. Clin Microbiol Infect. 2011;17:1798–803. doi: 10.1111/j.1469-0691.2011.03514.x. [DOI] [PubMed] [Google Scholar]
- 41.Bathoorn E, Tsioutis C, da Silva Voorham JM, et al. Emergence of pan-resistance in KPC-2 carbapenemase-producing Klebsiella pneumoniae in Crete, Greece: a close call. J Antimicrob Chemother. 2016;71:1207–12. doi: 10.1093/jac/dkv467. [DOI] [PubMed] [Google Scholar]
- 42.Spyropoulou A, Papadimitriou-Olivgeris M, Bartzavali C, et al. A ten-year surveillance study of carbapenemase-producing Klebsiella pneumoniae in a tertiary care Greek university hospital: predominance of KPC- over VIM- or NDM-producing isolates. J Med Microbiol. 2016;65:240–6. doi: 10.1099/jmm.0.000217. [DOI] [PubMed] [Google Scholar]
- 43.Giani T, D’Andrea MM, Pecile P, et al. Emergence in Italy of Klebsiella pneumoniae sequence type 258 producing KPC-3 carbapenemase. J Clin Microbiol. 2009;47:3793–94. doi: 10.1128/JCM.01773-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fontana C, Favaro M, Sarmati L, et al. Emergence of KPC-producing Klebsiella pneumoniae in Italy. BMC Res Notes. 2010;3:40. doi: 10.1186/1756-0500-3-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Giani T, Pini B, Arena F, et al. Epidemic diffusion of KPC carbapenemase-producing Klebsiella pneumoniae in Italy: results of the first countrywide survey 15 May to 30 June 2011. Euro Surveill. 2013;18(22) [PubMed] [Google Scholar]
- 46.Tumbarello M, Viale P, Viscoli C, et al. Predictors of mortality in bloodstream infections caused by Klebsiella pneumoniae carbapenemase-producing K. pneumoniae: importance of combination therapy. Clin Infect Dis. 2012;55:943–50. doi: 10.1093/cid/cis588. [DOI] [PubMed] [Google Scholar]
- 47.Giannella M, Trecarichi EM, De Rosa FG, et al. Risk factors for carbapenem-resistant Klebsiella pneumoniae bloodstream infection among rectal carriers: a prospective observational multicentre study. Clin Microbiol Infect. 2014;20:1357–62. doi: 10.1111/1469-0691.12747. [DOI] [PubMed] [Google Scholar]
- 48.Giacobbe DR, Del Bono V, Trecarichi EM, et al. Risk factors for bloodstream infections due to colistin-resistant KPC-producing Klebsiella pneumoniae: results from a multicenter case-control-control study. Clin Microbiol Infect. 2015;21:1106.e1–8. doi: 10.1016/j.cmi.2015.08.001. [DOI] [PubMed] [Google Scholar]
- 49.Monaco M, Giani T, Raffone M, Arena F, Garcia-Fernandez A, Pollini S Network EuSCAPE-Italy. Grundmann H, Pantosti A, Rossolini GM. Colistin resistance superimposed to endemic carbapenem-resistant Klebsiella pneumoniae: a rapidly evolving problem in Italy, November 2013 to April 2014. Euro Surveill. 2014;19(42) doi: 10.2807/1560-7917.ES2014.19.42.20939. [DOI] [PubMed] [Google Scholar]
- 50.Aschbacher R, Giani T, Corda D, et al. Carbapenemase-producing Enterobacteriaceae during 2011–12 in the Bolzano area (Northern Italy): increasing diversity in a low-endemicity setting. Diagn Microbiol Infect Dis. 2013;77:354–6. doi: 10.1016/j.diagmicrobio.2013.08.029. [DOI] [PubMed] [Google Scholar]
- 51.Tumbarello M, Trecarichi EM, De Rosa FG, et al. Infections caused by KPC-producing Klebsiella pneumoniae: differences in therapy and mortality in a multicentre study. J Antimicrob Chemother. 2015;70:2133–43. doi: 10.1093/jac/dkv200. [DOI] [PubMed] [Google Scholar]
- 52.Naas T, Nordmann P, Vedel G, Poyart C. Plasmid-mediated carbapenem-hydrolyzing beta-lactamase KPC in a Klebsiella pneumoniae isolate from France. Antimicrob Agents Chemother. 2005;49:4423–24. doi: 10.1128/AAC.49.10.4423-4424.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Dortet L, Radu I, Gautier V, Blot F, Chachaty E, Arlet G. Intercontinental travels of patients and dissemination of plasmid-mediated carbapenemase KPC-3 associated with OXA-9 and TEM- 1. J Antimicrob Chemother. 2008;61:455–57. doi: 10.1093/jac/dkm455. [DOI] [PubMed] [Google Scholar]
- 54.Cuzon G, Naas T, Demachy MC, Nordmann P. Nosocomial outbreak of Klebsiella pneumoniae harbouring bla(KPC-3) in France subsequent to a patient transfer from Italy. Int J Antimicrob Agents. 2012;39:448–49. doi: 10.1016/j.ijantimicag.2012.01.008. [DOI] [PubMed] [Google Scholar]
- 55.Naas T, Cuzon G, Babics A, et al. Endoscopy-associated transmission of carbapenem-resistant Klebsiella pneumoniae producing KPC-2 beta-lactamase. J Antimicrob Chemother. 2010;65:1305–06. doi: 10.1093/jac/dkq117. [DOI] [PubMed] [Google Scholar]
- 56.Albiger B, Glasner C, Struelens MJ, Grundmann H, Monnet DL European Survey of Carbapenemase-Producing Enterobacteriaceae (EuSCAPE) working group. Carbapenemase-producing Enterobacteriaceae in Europe: assessment by national experts from 38 countries, May 2015. Euro Surveill. 2015;20(45) doi: 10.2807/1560-7917.ES.2015.20.45.30062. [DOI] [PubMed] [Google Scholar]
- 57.Curiao T, Morosini MI, Ruiz-Garbajosa P, et al. Emergence of bla KPC-3-Tn4401a associated with a pKPN3/4-like plasmid within ST384 and ST388 Klebsiella pneumoniae clones in Spain. J Antimicrob Chemother. 2010;65:1608–14. doi: 10.1093/jac/dkq174. [DOI] [PubMed] [Google Scholar]
- 58.Oteo J, Ortega A, Bartolomé R, et al. Prospective multicenter study of carbapenemase-producing Enterobacteriaceae from 83 hospitals in Spain reveals high in vitro susceptibility to colistin and meropenem. Antimicrob Agents Chemother. 2015;59:3406–12. doi: 10.1128/AAC.00086-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Palacios-Baena ZR, Oteo J, Conejo C, et al. Comprehensive clinical and epidemiological assessment of colonisation and infection due to carbapenemase-producing Enterobacteriaceae in Spain. J Infect. 2016;72:152–60. doi: 10.1016/j.jinf.2015.10.008. [DOI] [PubMed] [Google Scholar]
- 60.Bedenic B, Mazzariol A, Plecko V, Bošnjak Z, Barl P, Vraneš J, Cornaglia G. First report of KPC-producing Klebsiella pneumoniae in Croatia. J Chemother. 2012;24:237–9. doi: 10.1179/1973947812Y.0000000017. [DOI] [PubMed] [Google Scholar]
- 61.Jelic M, Butic I, Plecko V, et al. KPC-Producing Klebsiella pneumoniae Isolates in Croatia: A Nationwide Survey. Microb Drug Resist. 2015 Dec 28; doi: 10.1089/mdr.2015.0150. [DOI] [PubMed] [Google Scholar]
- 62.Kostyanev T, Tafaj S, Skenduli I, et al. First detection of KPC-3-producing Klebsiella pneumoniae in Albania. New Microbes New Infect. 2015;4:11–2. doi: 10.1016/j.nmni.2015.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Bakour S, Sahli F, Touati A, Rolain JM. Emergence of KPC-producing Klebsiella pneumoniae ST512 isolated from cerebrospinal fluid of a child in Algeria. New Microbes New Infect. 2014;8:34–6. doi: 10.1016/j.nmni.2014.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Metwally L, Gomaa N, Attallah M, Kamel N. High prevalence of Klebsiella pneumoniae carbapenemase-mediated resistance in K. pneumoniae isolates from Egypt. East Mediterr Health J. 2013;19:947–52. [PubMed] [Google Scholar]
- 65.Helal SF, El-Rachidi NG, AbdulRahman EM, Hassan DM. The presence of blaKPC-mediated resistance in Enterobacteriaceae in Cairo University hospitals in Egypt and its correlation with in vitro carbapenem susceptibility. J Chemother. 2014;26:125–8. doi: 10.1179/1973947813Y.0000000099. [DOI] [PubMed] [Google Scholar]
- 66.Abdulall AK, El-Mahallawy HA, Abdo sa, Aly NK. Emergence of Klebsiella pneumoniae clinical isolates harboring Klebsiella pneumoniaecarbapenemase and metallo-β-lactamase in two hospitals in Egypt. New Egyptian Journal of Microbiology. 2014;39 [Google Scholar]
- 67.Walsh TR, Toleman MA, Poirel L, Nordmann P. Metallo-β-lactamases: the quiet before the storm? Clin Microbiol Rev. 2005;18:306–325. doi: 10.1128/CMR.18.2.306-325.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Vatopoulos A. High rates of metallo-β-lactamase-producingpneumoniae in Greece—a review of the current evidence. Euro Surveillance. 2008;13(4) [PubMed] [Google Scholar]
- 69.Luzzaro F, Docquier JD, Colinon C, Endimiani A, Lombardi G, Amicosante G, Rossolini GM, Toniolo A. Emergence in Klebsiella pneumoniae and Enterobacter cloacae clinical isolates of the VIM-4 metallo-beta-lactamase encoded by a conjugative plasmid. Antimicrob Agents Chemother. 2004;48:648–50. doi: 10.1128/AAC.48.2.648-650.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Aschbacher R, Doumith M, Livermore DM, Larcher C, Woodford N. Linkage of acquired quinolone resistance (qnrS1) and metallo-beta-lactamase (blaVIM-1) genes in multiple species of Enterobacteriaceae from Bolzano, Italy. J Antimicrob Chemother. 2008;61:515–23. doi: 10.1093/jac/dkm508. [DOI] [PubMed] [Google Scholar]
- 71.Aschbacher R, Pagani L, Doumith M, et al. Metallo-β-lactamases among Enterobacteriaceae from routine samples in an Italian tertiary-care hospital and long-term care facilities during 2008. Clin Microbiol Infect. 2011;17:181–9. doi: 10.1111/j.1469-0691.2010.03225.x. [DOI] [PubMed] [Google Scholar]
- 72.Cantón R, Akóva M, Carmeli Y, et al. Rapid evolution and spread of carbapenemases among Enterobacteriaceae in Europe. Clin Microbiol Infect. 2012;18:413–31. doi: 10.1111/j.1469-0691.2012.03821.x. [DOI] [PubMed] [Google Scholar]
- 73.Lartigue M-F, Poirel L, Nordmann P. First detection of a carbapenem-hydrolyzing metalloenzyme in an Enterobacteriaceae isolate in France. Antimicrob Agents Chemother. 2004;48:4929–4930. doi: 10.1128/AAC.48.12.4929-4930.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Barguigua A, El Otmani F, El Yaagoubi FL, Talmi M, Zerouali K, Timinouni M. First report of a Klebsiella pneumoniae strain coproducing NDM-1, VIM-1 and OXA-48 carbapenemases isolated inMorocco. APMIS. 2013;121:675–677. doi: 10.1111/apm.12034. [DOI] [PubMed] [Google Scholar]
- 75.Poirel L, Abdelaziz MO, Bernabeu S, Nordmann P. Occurrence of OXA-48 and VIM-1 carbapenemase-producing Enterobacteriaceae in Egypt. Intern J Antimicrob Agents. 2013;41:90–91. doi: 10.1016/j.ijantimicag.2012.08.015. [DOI] [PubMed] [Google Scholar]
- 76.Robin F, Aggoune-Khinache N, Delmas J, Naim M, Bonnet R. Novel VIM metallo-β-lactamase variant from clinical isolates of Enterobacteriaceae from Algeria. Antimicrob Agents Chemother. 2010;54:466–470. doi: 10.1128/AAC.00017-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ktari S, Arlet G, Mnif B, et al. Emergence of multidrugresistant Klebsiella pneumoniae isolates producing VIM-4 metallo-β-lactamase, CTX-M-15 extended-spectrum β-lactamase, and CMY- 4 AmpC β-lactamase in a Tunisian University Hospital. Antimicrob Agents Chemother. 2006;50:4198–4201. doi: 10.1128/AAC.00663-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Nordmann P, Poirel L, Toleman MA, Walsh TR. Does broad-spectrum β-lactam resistance due to NDM-1 herald the end of the antibiotic era for treatment of infections caused by Gram-negative bacteria? J Antimicrob Chemother. 2011;66:689–692. doi: 10.1093/jac/dkq520. [DOI] [PubMed] [Google Scholar]
- 79.Kumarasamy KK, Toleman MA, Walsh TR, et al. Emergence of a new antibiotic resistance mechanism in India, Pakistan, and the UK: a molecular, biological, and epidemiological study. Lancet Infect Dis. 2010;10:597–602. doi: 10.1016/S1473-3099(10)70143-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Birgy A, Doit C, Mariani-Kurkdjian P, et al. Early detection of colonization by VIM-1-producing Klebsiella pneumoniae and NDM-1-producing Escherichia coli in two children returning to France. J Clin Microbiol. 2011;49:3085–3087. doi: 10.1128/JCM.00540-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Giani T, Pini B, Arena F, et al. Epidemic diffusion of KPC carbapenemase-producing Klebsiella pneumoniae in Italy: results of the first countrywide survey. Eurosurveillance. 2013;18:22. [PubMed] [Google Scholar]
- 82.Gil-Romero Y, Sanz-Rodriguez N, Almagro-Molto M, Gomez-Garces GM. New description of a NDM-1 carbapenemase producing Klebsiella pneumoniae carrier in Spain. Enferm Infec Microb Clin. 2013;31:418–419. doi: 10.1016/j.eimc.2012.10.009. [DOI] [PubMed] [Google Scholar]
- 83.Oteo J, Domingo-Garcia D, Fernandez-Romero S, et al. Abdominal abscess due to NDM-1-producing Klebsiella pneumoniae in Spain. J Med Microbiol. 2012;61:864–867. doi: 10.1099/jmm.0.043190-0. [DOI] [PubMed] [Google Scholar]
- 84.Poirel L, Benouda A, Hays C, Nordmann P. Emergence of NDM-1-producing Klebsiella pneumoniae in Morocco. J Antimicrob Chemother. 2011;66:2781–2783. doi: 10.1093/jac/dkr384. [DOI] [PubMed] [Google Scholar]
- 85.Nasr AB, Decre D, Compain F, Genel N, Barguellil F, Arlet G. Emergence of NDM-1 in association with OXA- 48 in Klebsiella pneumoniae from Tunisia. Antimicrob Agents Chemother. 2013;57:4089–4090. doi: 10.1128/AAC.00536-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Abdelaziz MO, Bonura C, Aleo A, Fasciana T, Mammina C. NDM-1-and OXA-163-producing Klebsiella pneumoniae isolates in Cairo, Egypt, 2012. J Glob Antimicrob Resist. 2013;1:213–5. doi: 10.1016/j.jgar.2013.06.003. [DOI] [PubMed] [Google Scholar]
- 87.Poirel L, Ozdamar M, Ocampo-Sosa AA, Turkoglu S, Ozer UG, Nordmann P. NDM-1-producing Klebsiella pneumoniae now in Turkey. Antimicrob Agents Chemother. 2012;56:2784–2785. doi: 10.1128/AAC.00150-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Alp E, Percin D, Colakoglu S, et al. Molecular characterization of carbapenem-resistant Klebsiella pneumoniae in a tertiary university hospital in Turkey. J Hosp Infect. 2013;84:178–180. doi: 10.1016/j.jhin.2013.03.002. [DOI] [PubMed] [Google Scholar]
- 89.Giakkoupi P, Tryfinopoulou K, Kontopidou F, et al. Emergence of NDM-producing Klebsiella pneumonia in Greece. Diagn Microbiol Infect Dise. 2013;77:382–384. doi: 10.1016/j.diagmicrobio.2013.09.001. [DOI] [PubMed] [Google Scholar]
- 90.Psichogiou M, Tassios PT, Avlamis A, et al. Ongoing epidemic of blaVIM-1-positive Klebsiella pneumoniae in Athens, Greece: a prospective survey. J Antimicrob Chemother. 2008;61:59–63. doi: 10.1093/jac/dkm443. [DOI] [PubMed] [Google Scholar]
- 91.Baroud M, Dandache I, Araj GF, et al. Underlying mechanisms of carbapenem resistance in extended-spectrum β-lactamase-producing Klebsiella pneumoniae and Escherichia coli isolates at a tertiary care centre in Lebanon: role of OXA-48 and NDM-1 carbapenemases. Intern J Antimicrob Agents. 2013;41:75–79. doi: 10.1016/j.ijantimicag.2012.08.010. [DOI] [PubMed] [Google Scholar]
- 92.Bialvaei AZ, Kafil HS, Leylabadlo HE, Asgharzadeh M. Aghazadeh M Dissemination of carbapenemases producing Gram negative bacteria in the Middle East. Iran J Microbiol. 2015;7:226–246. [PMC free article] [PubMed] [Google Scholar]
- 93.Gefen-Halevi S, Hindiyeh MY, Ben-David D, Smollan G, Gal-Mor O, Azar R, et al. Isolation of genetically unrelated bla(NDM-1)- positive Providencia rettgeri strains in Israel. J Clin Microbiol. 2013;51:1642–3. doi: 10.1128/JCM.00381-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Poirel L, H’eritier C, Tolün V, Nordmann P. Emergence of oxacillinase-mediated resistance to imipenem in Klebsiella pneumoniae. Antimicrob Agents Chemother. 2004;48:15–22. doi: 10.1128/AAC.48.1.15-22.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Carrer A, Poirel L, Eraksoy H, Cagatay AA, Badur S, Nordmann P. Spread of OXA-48-positive carbapenem-resistant Klebsiella pneumoniae isolates in Istanbul, Turkey. Antimicrob Agents Chemother. 2008;52:2950–4. doi: 10.1128/AAC.01672-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Aktas Z, Kayacan CB, Schneider I, Can B, Midilli K, Bauernfeind A. Carbapenem-hydrolyzing oxacillinase, OXA-48, persists in Klebsiella pneumoniae in Istanbul, Turkey. Chemother. 2008;54:101–6. doi: 10.1159/000118661. [DOI] [PubMed] [Google Scholar]
- 97.Cuzon G, Ouanich J, Gondret R, Naas T, Nordmann P. Outbreak of OXA-48-positive carbapenem-resistant Klebsiella pneumoniae isolates in France. Antimicrob Agents Chemother. 2011;55:2420–2423. doi: 10.1128/AAC.01452-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Potron A, Poirel L, Rondinaud E, Nordmann P. Intercontinental spread of OXA-48 beta-lactamase-producing Enterobacteriaceae over a 11-year period, 2001 to 2011. Eurosurveillance. 2013;18:31. doi: 10.2807/1560-7917.ES2013.18.31.20549. [DOI] [PubMed] [Google Scholar]
- 99.Benouda A, Touzani O, Khairallah MT, Araj GF, Matar GM. First detection of oxacillinase-mediated resistance to carbapenems in Klebsiella pneumoniae from Morocco. Ann Trop Med Parasitol. 2010;104:327–330. doi: 10.1179/136485910X12743554760108. [DOI] [PubMed] [Google Scholar]
- 100.Voulgari E, Zarkotou O, Ranellou K, et al. Outbreak of OXA-48 carbapenemase-producing Klebsiella pneumoniae in Greece involving an ST11 clone. J Antimicrob Chemother. 2013;68:84–88. doi: 10.1093/jac/dks356. [DOI] [PubMed] [Google Scholar]
- 101.Adler A, Shklyar M, Schwaber MJ, et al. Introduction of OXA-48-producing enterobacteriaceae to israeli hospitals by medical tourism. J Antimicrob Chemother. 2011;66:2763–2766. doi: 10.1093/jac/dkr382. [DOI] [PubMed] [Google Scholar]
- 102.Matar GM, Dandache I, Carrër A, et al. Spread of OXA-48-mediated resistance to carbapenems in Lebanese Klebsiella pneumoniae and Escherichia coli that produce extended spectrum β-lactamase. Ann Tropic Med Parasitol. 2010;104:271–274. doi: 10.1179/136485910X12647085215651. [DOI] [PubMed] [Google Scholar]
- 103.Matar GM, Cuzon G, Araj GF, et al. Oxacillinase mediated resistance to carbapenems in Klebsiella pneumoniae from Lebanon. Clin Microbiol Infect. 2008;14:887–888. doi: 10.1111/j.1469-0691.2008.02059.x. [DOI] [PubMed] [Google Scholar]
- 104.Pirš M, Andlovic A, Cerar T, et al. A case of OXA-48 carbapenemase-producing Klebsiella pneumoniae in a patient transferred to Slovenia from Libya, November 2011. Euro Surveillance. 2011;16:50. [PubMed] [Google Scholar]
- 105.Oteo J, Hern’andez JM, Espasa M, et al. Emergence of OXA-48-producing Klebsiella pneumoniae and the novel carbapenemases OXA-244 and OXA-245. in Spain. J Antimicrob Chemother; 2013. pp. 317–321. [DOI] [PubMed] [Google Scholar]
- 106.Ktari S, Mnif B, Louati F, et al. Spread of Klebsiella pneumoniae isolates producing OXA-48 β-lactamase in a Tunisian university hospital. J Antimicrob Chemother. 2011;66:1644–1646. doi: 10.1093/jac/dkr181. [DOI] [PubMed] [Google Scholar]
- 107.Hays C, Benouda A, Poirel L, Elouennass M, Nordmann P. Nosocomial occurrence of OXA-48-producing enterobacterial isolates in a Moroccan hospital. Intern J Antimicrob Ag. 2012;39:545–547. doi: 10.1016/j.ijantimicag.2012.03.002. [DOI] [PubMed] [Google Scholar]
- 108.Barguigua A, El Otmani E, Talmi M, Zerouali K, Timinouni M. Emergence of carbapenem-resistant Enterobacteriaceae isolates in the Moroccan community. Diagn Microbiol Infect Dis. 2012;73:290–291. doi: 10.1016/j.diagmicrobio.2012.03.011. [DOI] [PubMed] [Google Scholar]
- 109.Kraiem AG, Zorgani A, Elahmer O, Hammami A, Chaaben BM, Ghenghesh KS. New Delhi metallo-β-lactamase and OXA-48 carbapenemases in Gram-negative bacilli isolates in Libya. Libyan J Med. 2015;10:29206. doi: 10.3402/ljm.v10.29206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Lafeuille E, Decré D, Mahjoub-Messai F, Bidet P, Arlet G, Bingen E. OXA-48 carbapenemase-producing Klebsiella pneumoniae isolated from Libyan patients. Microb Drug Resist. 2013;19:491–7. doi: 10.1089/mdr.2012.0219. [DOI] [PubMed] [Google Scholar]
- 111.Kocsis E, Savio C, Piccoli M, Cornaglia G, Mazzariol A. Klebsiella pneumoniae harbouring OXA-48 carbapenemase in a Libyan refugee in Italy. Clin Microbiol Infect. 2013;19:E409–11. doi: 10.1111/1469-0691.12232. [DOI] [PubMed] [Google Scholar]; Pirš M, Andlovic A, Cerar T, Žohar-Cretnik T, Kobola L, Kolman J, Frelih T, Prešern-Štrukelj M, Ružic-Sabljic E, Seme K. A case of OXA-48 carbapenemase-producing Klebsiella pneumoniae in a patient transferred to Slovenia from Libya, November 2011. Euro Surveill. 2011;16:20042. [PubMed] [Google Scholar]
- 112.Hammerum AM, Larsen AR, Hansen F, Justesen US, Friis-Møller A, Lemming LE, Fuursted K, Littauer P, Schønning K, Gahrn-Hansen B, Ellermann-Eriksen S, Kristensen B. Patients transferred from Libya to Denmark carried OXA-48-producing Klebsiella pneumoniae, NDM-1-producing Acinetobacter baumannii and meticillin-resistant Staphylococcus aureus. Int J Antimicrob Agents. 2012;40:191–2. doi: 10.1016/j.ijantimicag.2012.05.003. [DOI] [PubMed] [Google Scholar]
- 113.Pirš M, Andlovic A, Cerar T, Žohar-Èretnik T, Kobola L, Kolman J, Frelih T, Prešern-Štrukelj M, Ružiæ-Sabljiæ E, Seme K. A case of OXA-48 carbapenemase-producing Klebsiella pneumoniae in a patient transferred to Slovenia from Libya, November 2011. Euro Surveill. 2011;16:20042. [PubMed] [Google Scholar]