Background
Obesity is a major threat to the health of the nation. The prevalence of obesity1,2 and its associated health risks are well documented.3,4 Known determinants of obesity include physical activity and dietary behaviors. Public health efforts to increase physical activity and improve nutrition among the general population have traditionally been aimed at individual-level health changes. Such approaches have been found to be minimally effective, costly, and difficult to sustain.5 In 2002, the Institute of Medicine (IOM) endorsed a broad approach to public health problems recommending the adoption of an ecologic model, where individuals and their behavioral choices are situated within and influenced by their broader social and environmental context.6,7 Physical activity and nutrition researchers and practitioners have applied the ecologic model.8 Researchers currently recommend a systems-oriented multilevel framework, which acknowledges the interrelated, dynamic, and adaptive factors that can influence obesity.3,9–11 A national focus on “policy, systems, and environmental change strategies” has emerged in public health, supported by evidence showing that policy has the potential to impact population health.12–15
Leading US public health organizations have led efforts to promote policy, systems, and environmental change (PSE) strategies nationwide and have encouraged practitioners and researchers to implement nutrition and physical activity policies. These public health organizations have provided a rapid infusion of resources to support such attempts.16–18 Collaborative endeavors among philanthropic organizations and government agencies have emerged to focus on accelerating progress on policy changes.19,20 Recent investments by these sectors have supported an increased focus on obesity prevention by public health practitioners and led to the establishment of collaborative groups (e.g. coalitions, networks, partnerships). These groups are actively working to promote PSE strategies at state and local levels.21 Their ability to lead the development of PSE is likely to impact the nation’s progress on obesity prevention. There is a pressing need to increase the familiarity and expertise of those working to promote obesity prevention with the processes and activities that facilitate PSE approaches.13,22,23 The IOM has urged practitioners to familiarize themselves with legal and policy interventions to improve public health.13 A recent assessment of the competencies necessary for obesity prevention and control identified the ability of public health practitioners to understand the process by which laws are developed as a key area in which to build competence.23 Other researchers have noted the importance of studying policy development,24 which is considered a core public health function.25 Yet, public health policymaking processes generally have been understudied and poorly understood.5 There is an urgent need to bring knowledge and skills on advancing PSE to the local and state levels, where practitioners have the greatest potential to exert influence on the decision making of public officials.
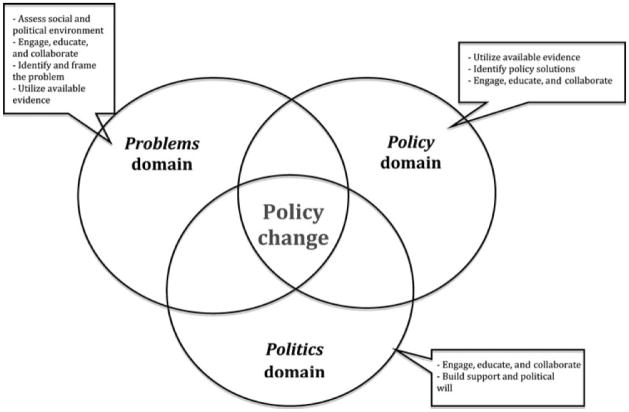
The purpose of this article was to provide guidance for practitioners and collaborative groups on the activities that hold promise for facilitating policy change for obesity prevention. The article first provides an overview of the policy process by describing three domains that influence policymakers in their decisions to adopt one policy instead of another. The problem, policy, and politics domains each, respectively, plays a vital role in determining the fate of most policy proposals. Together, they provide a frame through which the policy-making process can be understood. Next, the article focuses on ways to promote conditions favorable to obesity prevention policies. Collectively, the three domains and six activities presented here represent a framework (Figure 1) to guide advocacy for PSE around obesity prevention. Other aspects of the policy process, such as implementation and evaluation, are beyond the scope of this article and are discussed elsewhere.26,27
FIGURE 1.
Framework for Advancing Policy, System, and Environmental Change Approaches for Obesity Prevention
The development of this article was informed by a literature search for published works that describe or explain the policymaking process. We conducted an assessment of articles on the basis of accepted rules of qualitative inquiry, with the goal of distilling activities identified as having utility in influencing the policy process. The key activities included in this article represent themes that emerged from our review and analysis. Findings are not meant to represent a systematic review. There is much to be studied and learned on the art and science of advocacy for obesity prevention policy. This article seeks to communicate what is currently known about strategies for influencing the policy process. It aims to contribute to public health practice and the building of a knowledge base in this area.
Overview of the Policy Process
The current focus on PSE as an effective approach for obesity prevention prompts a review of the process through which policy is made. The policymaking process has been described as consisting of three domains: problems, policy, and politics.28 In the problem domain, practitioners and collaborative groups must have their issue of interest acknowledged by policymakers as a problem worthy of attention. The issue must be placed on the policy agenda by decision makers. While obesity is a serious public health problem, it is but one problem among many competing for the finite attention of policymakers. The practitioner’s goal in the problems domain is simply to have their issue recognized as a problem and placed on the policy agenda for action. Failure to achieve this goal reduces the odds that desired policies will be considered or implemented.
The second area of focus in the policy process is the policy domain. It is focused on identification of policy solutions that address the problem of focus (i.e. typically a specific determinant of obesity). Many proposals may be put forth. Some are taken seriously by policymakers and others quickly discarded. The policy proposals that survive to ultimately receive serious consideration generally meet several selection criteria, including technical feasibility, congruence with values, and anticipation of future restrains, including fiscal limitations, public acceptability, and politicians’ receptivity. The third point of focus is the politics domain. It represents the prevailing political context. It determines whether or not a policy proposal will be legitimized and adopted. The politics domain is affected by factors, such as national mood, public opinion, changes in administration, shifts in partisan or ideological distributions among politicians, and interest group pressure campaigns. In this domain, practitioners and collaborative groups must work to establish a favorable environment for policies that promote obesity prevention. The adoption of policy proposals is most likely to occur when the three domains become coupled. As the process goes, a problem is recognized, policy proposals are generated, the political climate makes the time right for change, and the constraints do not prohibit action.28 Efforts to implement PSE for obesity prevention are likely to benefit from a clearer presentation of the activities that promote success within each of the three domains. Next, we summarize activities that hold promise for promoting policy change by facilitating the convergence of the three domains.
Key Activities for Policy Change
Our review of the literature suggests that desirable policy change outcomes involve six key activities: (a) assess the social and political environment; (b) engage, educate, and collaborate with key stakeholders; (c) identify and frame the problem; (d) utilize available evidence; (e) identify policy solutions; and (f) build support and political will. The activities focus on addressing issues of interest, facilitating effective policy development and evaluating the existing political and social environment. These activities do not necessarily occur sequentially, and each may take place in the problem, policy, and politics domains of the policy process. We highlight these activities for their potential to facilitate the development and implementation of policy solutions that reshape environments to promote healthy behaviors related to nutrition and physical activity. Supplemental examples and resources for each activity are provided in Table 1.
Table 1.
Key Activities to Facilitate Success in Policy and Environmental Approaches
| Activity and definition | Examples of action | Tools/Resources |
|---|---|---|
|
Identify and frame the problem. Presenting the issue as a problem worthy of action and caused by factors amenable to policy intervention. |
Using media to highlight a problem. | |
| Developing policy briefs that help policymakers understand the problem and possible solutions. Using participatory action research methods, such as Photovoice. |
||
|
Engage and educate key people. Intentional interaction with politicians, public officials, and stakeholders to raise awareness of the problem and initiate public and political engagement. |
Developing a coalition; working collaboratively with stakeholders to develop an action agenda; | |
| Educating policymakers; building public awareness and engagement. | ||
|
Identify policy solutions. Defining policy opportunities and specific levers to influence food systems or physical activity environments |
Review evidence-based recommendations; consider feasibility, acceptability, cost, and reach; | |
|
Utilize available evidence. Using credible sources of evidence to inform policy formulation. |
Review evidence-based recommendations to inform content of policies (CDC, IOM, the Community Guide); consider likelihood of policy adoption, anticipated outcomes. |
|
|
Assess social and political environment. Working to understand the prevailing context in which policy proposals are considered for adoption. |
Conduct a public opinion survey; test reactions to various policy proposals; identify hot issues and how they might connect with obesity prevention; consider how to use elections cycles to promote policy solutions. | |
|
Build support and political will. Encouraging advocates, policymakers, and the general public to support proposed policies |
Educate stakeholders about the problems and possible solutions; support |
Stamatakis KA, McBride TD, Brownson RC. Communicating prevention messages to policy makers: the role of stories in promoting physical activity. J Phys Act Health. 2010; Suppl 1:S99–107.
Community Preventive Services Task Force: http://www.thecommunityguide.org/uses/research.html.
Centers for Disease Control and Prevention. MMWR 2009;58: http://www.cdc.gov/mmwr/pdf/rr/rr5807.pdf.
Swinburn, B; Gill, T; Kumanyika, S (2004). Obesity prevention: a proposed framework for translating evidence into action. Obesity Reviews, 6:23–33.
Klein JD, Dietz W. Childhood obesity: The new tobacco. Health Aff. 2010;29:3,388–392.
Assess the social and political environment
Successful policy change often hinges on understanding how and when the processes of problem recognition, policy development, and political decision making converge. The coupling of these domains is a phenomenon commonly referred to as the opening of a policy window, representing an advantageous context for policy change. The window opens when the problem has been highlighted, decision makers begin seeking solutions, and the political climate is favorable for policy adoption.28 Practitioners and collaborative groups can help create the conditions that promote the coupling of the problem, policy, and political domains by surveying the social and political environment. These actions may include acquiring knowledge about the government structures, processes, and rules that affect policy proposals and identifying powerful political actors and their agenda priorities.31 For example, it is important to understand which unit of the legislative or executive branches has oversight of the issue(s) of concern, which policymakers hold key positions, and what can be learned about their political beliefs and ideologies.32 Elected and appointed officials are often situated within influential networks of political support.33 Developing knowledge of these networks can inform decisions on which policymakers to engage and which policy issue(s) to pursue. Strategies for better understanding these networks might include identifying key decision makers’ colleagues, community and business affiliations; and donors and political supporters.
Public opinion is another factor that should be considered when working to advance policy issues. It reflects the mood, values, and policy preferences of voters. Public opinion has been found to influence political agendas and political decision making.34 It can be a powerful force in persuading policymakers to support, or even champion, obesity prevention policy. Data on public opinion can be acquired through surveys of the public at-large; interviews with key opinion leaders in relevant sectors; or even by reviewing the public’s voting records on related ballot measures. By assessing and understanding the environment, advocates can identify policy opportunities, tailor policy options to the existing political environment, and gauge the likelihood of successful PSE.34
Engage, educate, and collaborate
Successfully promoting obesity prevention policies requires support from a broad coalition of stakeholders that often include politicians, public officials, interest groups, and other parties. Engaging and educating these groups and initiating formal collaboration early in the process can pay dividends when efforts are made to have the problem placed on the agenda, to identify solutions, and to advocate for adoption of desired policies. Politicians and public officials have significant power and influence in shaping governmental policy agendas. To attain agenda status, an issue will need to garner the support of key decision makers, who develop and guard the formal policy agenda.35 It is vital to engage and educate these individuals about obesity and the specific policy strategies that are being pursued to address the problem.
Interest groups also have significant potential to impact policy outcomes.32 Interests groups are organizations that seek to influence public opinion and policy on a particular cause. They can represent stakeholders affected by policy decisions. For example, an effort aimed at physical education policy in schools would benefit from engaging stakeholders, such as physical education teachers, parents, school administrators, and the professional associations representing these constituencies. policymakers often seek information and opinions from these groups in determining whether a problem exists (problems domain) and whether the policy proposal being considered is feasible and acceptable (policy and politics domains). Advocacy efforts that include groups with access to key points of government and decision making are more likely to have their issues placed on an agenda and addressed.35 In a recent study, researchers conducted interviews with legislators across 11 states to examine factors enabling state-level childhood obesity prevention legislation.36 Consistent with previous research,37 legislators identified “support or involvement of stakeholders” and “involvement of senior legislators” as enablers of policy adoption. Establishing broad engagement across a mix of policymakers, stakeholders, and interest groups contributes to the building of a strong coalition, which can exert tremendous influence on future policy decisions.38 Such collaborative groups focused on promoting active living and healthy eating achieve policy change successes in part by soliciting endorsements from community leaders and offering testimony in policy, legal, or judicial hearings.21 A case study illustrating the results of effective engagement and education of key stakeholders is presented in Table 2.
Table 2.
Engage and Educate People: Arkansas Act 1220
The Arkansas case study on obesity prevention policy efforts illustrates the value of engaging and educating key decision-makers. Prior to the passage of Arkansas’s Act 1220 of 2003 a series of events occurred placing a spotlight on the problem of childhood obesity, ultimately catapulting obesity prevention onto the policy agenda.a,b Arkansas policy leaders focused on engaging and educating key decision-makers and stakeholders through various activities. These included:
Collectively, these events and actions focused influential policymakers on the problem of childhood obesity and on possible policy solutions. The initiative promoted by health advocates culminated in the implementation of a comprehensive school-based obesity prevention program. |
Ryan K, Card-Higginson P, McCarthy S, Justus M, Thompson J. Arkansas fights fat: translating research into policy to combat childhood and adolescent obesity. Health Aff. 2006;25(4).
Craig R, Felix H, Walker J, Phillips M. Public health professionals as policy entrepreneurs: Arkansas’s childhood obesity policy experience. Am J Public Health. 2010;100(11):2047–52.
Identify and frame the problem
Recognizing obesity as a problem that merits immediate attention and a place on the public policy agenda is a critical step in promoting the adoption of desired policies. Approaches in this area directly impact the problems domain of the policy process, helping decision makers to recognize the need for policy intervention. Practitioners and collaborative groups who coordinate their efforts to advocate in the public’s interest can “trigger” attention for a problem such as obesity and ultimately get it prominently placed on the policy agenda.35 Available data can serve as a problem indicator (e.g. low student fitness reports) or may highlight a condition demanding action (e.g. obesity prevalence, lack of access to healthy foods). Research indicates that simply providing information about a problem to policymakers is insufficient to change policy.29 Information must be packaged in a persuasive manner.41 Narratives or stories generating empathy and calling attention to external causes of obesity promote support for obesity-related policy change.42 For example, stories about barriers in the built environment that make it difficult or unsafe for children to walk to school have prompted action to create safe routes for walking.29 Participatory action research methods such as Photovoice, which engages residents in documenting their concerns using photography, can further focus the lenses on a problem by illustrating the barriers and enablers of physical activity.43,44
Efforts to identify and frame an obesity-related problem should also utilize media. Media exposure of childhood obesity policy has been identified as an enabler of policy adoption.36 Research shows that community coalitions that frequently use media advocacy are more likely to achieve environmental changes in support of active living.21 Effective media communication can reduce barriers to policy change by addressing any misconceptions and fears associated with proposed legislation.36 Overall, advocates for obesity prevention policies can advance their work by leveraging media, using powerful narratives, and packaging communication tools persuasively.
Utilize available evidence
Efforts to identify and frame obesity occur in the problems domain of the policy process. But there is also a need to carry out work that aims to identify policies that hold promise in addressing obesity (thepolicy domain). In doing so, existing evidence should be used as a guide to determine the most effective policies. Next, we highlight three key factors that can be used to determine the most policy-relevant evidence.45,46 First, it is important to have evidence on the content of the policy. The Guide to Community Preventive Services12 outlines specific intervention topics that, after systematic review, were recommended for obesity prevention. These topics span settings, sectors, and policy levels. While it is important to seek out the best available evidence for content, it may be necessary to include untested yet promising strategies.47 The Center of Excellence for Training and Research Translation48 provides systematic evaluation of evidence-based and emerging interventions and policies in obesity prevention. The Center TRT recognizes the importance of practice-tested initiatives in building the evidence for these strategies and has provided an evaluation framework for policy interventions.49 Credible information can also be found in reports, briefs, or analyses produced by leading philanthropies, not-for-profits, and nongovernmental organizations. Using aggregate policy data sources can also help assess content effectiveness. One such source is Bridging the Gap,50 an annual compilation of school policies related to wellness and obesity prevention; other sources may be topic-specific. Web-based resources for Complete Streets,51 Joint Use Agreements,52 or Farm to School,53 all keep current lists of federal, state, and local policies, including model policy language based on the evidence (when available) or practice-tested content.
The second key factor in determining policy-relevant evidence is to examine evidence related to the likelihood of policy adoption.45,46 Many approaches to obesity prevention have potential in various settings, such as cities, counties, local communities, and states.9 It is important to consider which approaches are more or less likely to be adopted given contextual factors. Kindgon’s policy stream model suggests that factors, such as national mood, public opinion, and interest group pressure, can affect policy adoption.28 For example, in a recent study, Eyler et al54 found that bills containing content about menu labeling or increased tax were more than two times less likely to be enacted than other obesity prevention topics. Conversely, bills containing content about curriculum changes or Safe Routes to School were more likely to be enacted than other topics. Determining the degree of receptiveness among key stakeholders is critical to adoption.
The third key factor in determining policy-relevant evidence is documenting the potential impact of a proposed policy. One approach that is receiving increasing attention in the United States is Health Impact Assessment. Health Impact Assessment is a public engagement and decision-support methodology that can be used to prospectively assess the health impacts of policy proposals and to make recommendations to inform decision making and ultimately improve public health outcomes.55 Several states and cities now offer Health Impact Assessment training, as does the Centers for Disease Control and Prevention and the National Association of County and City Health Officials.56
Existing data and surveillance systems also can be used to assess changes in health outcomes over time.57 These include, the Behavioral Risk Factor Surveillance System, the Youth Risk Behavior Surveillance Survey;58 the National Survey of Children’s Health;59 National Immunization Survey;60 state-specific vital statistics; and census data. The National Collaborative on Childhood Obesity Research developed a catalog of surveillance systems, which provide a unique window on obesity-related policies and environmental factors as well as trends in relevant health behaviors, outcomes, and determinants.20 Using data to inform policies can assist in revealing the extent of the problem, setting targets, and demonstrating improvement.
Identify policy solutions
Identifying the appropriate policy solutions (policy domain) to address obesity requires careful consideration of the wide range of available policy options to influence food systems (Table 3) and physical activity environments (Table 4). Of utmost importance, policy solutions should be practical and suitable. Kingdon28 suggests that a range of factors should be considered in developing policy solutions. Proposed solutions should be technically feasible. Solutions should specify actual mechanisms by which an idea would be brought into practical use. The idea should be compatible with expert opinions and key stakeholders (i.e. reflect shared values). It should be cost-sensitive. Solutions should include information on efficiency and should address whether benefits could be achieved through less costly policy interventions. Cost considerations should also include anticipation of future financial constraints and how they can be addressed. The idea should be compatible with public mood and political climate (i.e. publically acceptable). Information on the number, proportion, and representativeness of individuals that are likely to be affected should be provided (i.e. population reach). Policy solutions should be aimed at a wide audience. The proposed policy should hold promise for altering the environment in a manner that positively influences population-level physical activity or dietary behaviors (i.e. effectiveness). Identification of appropriate policies can be informed by established models that aim to inform the selection of policy solutions by examining many of the factors listed previously.62,63
Table 3.
Policy Areas that Influence the Food Systema
| Sector | Level of Governance | |
|---|---|---|
| Food Production |
Local Land-use management, zoning Community Gardens |
State Production subsidies, taxes |
| Food Processing | Food safety | |
| Distribution | Food transport | |
| Marketing | Laws, regulations regarding marketing unhealthy foods Laws, regulations regarding marketing healthy foods |
Laws, regulations restricting marketing unhealthy foods Laws promoting marketing of healthy foods |
| Retail | Land-use management, zoning Density, location of fresh food retailers Density, location of fast food outlets Food deserts |
Products sold in schools |
| Restaurants and Food Service | Nutrition information in restaurants Food safety |
|
Adapted from:
Sacks G, Swinburn BA, Lawrence MA. A systematic policy approach to changing the food system and physical activity environments to prevent obesity. Aust New Zealand Health Policy. 2008;5:13
Table 4.
Policy Areas that Influence Physical Activity Environmentsa
| Sector | Level of Governance | |
|---|---|---|
|
| ||
| Local | State | |
| Infrastructure and Planning | Land-use management, zoning | Urban planning |
| Walking environment | Roads Public, alternative transportation | |
| Cycling environment | ||
| Play environment | ||
|
| ||
| Education | Physical education in schools Facilities, equipment for physical activity in schools | |
|
| ||
| Employment | Building design standards | |
|
| ||
| Transportation | Public transportation | Public transportation |
| Parking restrictions | Alternative transportation | |
| Traffic control | Traffic control | |
|
| ||
| Sports and Recreation | Facilities for physical activities - built structures | Public liability |
| Facilities for physical activities - parks and open spaces | Access of general community to school physical activity/sports facilities | |
| Public liability | ||
Adapted from:
Sacks G, Swinburn BA, Lawrence MA. A systematic policy approach to changing the food system and physical activity environments to prevent obesity. Aust New Zealand Health Policy. 2008;5:13
It is also important to identify the governing body responsible for passing or adopting the policy of interest (e.g. the town zoning board or the state legislature).62 The recognition of receptive venues for policy increases the likelihood of adoption of desirable policies. While receptive legislatures may adopt policies designed to address obesity,39,40 the executive branch can issue orders by proclamation or through its regulatory agencies or offices.64 By understanding these dynamics, advocates can identify and develop a policy appropriate for the governing body of interest.
Consideration should also be given to the likelihood of sustainability, effects on health equity, and any potential for unintended consequences (e.g. traffic congestion, economic impact, stigmatization).47 It is best to have more than one policy solution available, as devising a short list of ideas will allow for flexibility. Kingdon28 recommends having these solutions “in hand” so that the solution is already developed when a window of opportunity opens.
Build support and political will
Building community and political support has a direct impact on the politics domain, and it is vital to achieving policy change. Public opinion influences the “political will” of policymakers to enact desired policies.34 Garnering support for obesity-related policy among the general public and encouraging the public to voice concerns about obesity to policymakers improves the likelihood that policy change will occur. Advocates can increase awareness, support, and political will to develop obesity-related policy by encouraging participation from local officials, individuals and community groups, and public and private entities.37 Community members, leaders, advocates, and organized groups within communities have a perspective of the local context that helps them recognize unique policy opportunities, build support, and encourage collaboration among interested parties and policymakers.37 Building support ensures that policies will reflect the needs and concerns of community members.65 Coordinating efforts across all levels of government66 and including potential opponents in the discussion67 promotes successful policy initiatives.
Efforts associated with building support and political will should leverage relationships that have been established in the problems domain, where the engage, educate, and collaborate activity (previously presented) is carried out with an eye toward building a broad base of support for the issue of interest. There is an ongoing need to build such support from key stakeholders across the entire policy process. However, as public officials bring the policy proposal of interest under consideration (the politics domain), the collective will of engaged policymakers, interest groups, coalitions, and the public must be galvanized and brought to bear on decision makers. The policy process is not fully sequential. It will usually be necessary to work concurrently on many of the activities recommended here. A relevant case study is highlighted in Table 5.
Table 5.
Build Support and Political Will: Grocery Gap II
| In 2001, the Food Trust, a non-profit organization dedicated to increasing access to healthy food focused its policy change efforts on closing the “grocery gap” and expanding access to healthy, nutritious food in underserved communities. The Food Trust spearheaded a campaign to increase the number of fresh food outlets in underserved communities and worked to unite community and political leaders and other key stakeholders from diverse sectors around its policy goal. |
| Recognizing that building support in the community and among local political leaders was critical to its success, the Food Trust focused its efforts on outreach and education. Its members established a telephone campaign targeting supermarket representatives, children’s health-related non-profit organizations, academic institutions, and public health departments and other governmental organizations. They also organized meetings to gauge the existing understanding of the connection between supermarkets, health, underserved communities and measures that could be implemented to increase access to healthy food. Policy advocates convened local task-force comprised of local organizations and key stakeholders and engaged and educated local decision makers. Building support across a broad, diverse group of stakeholders ultimately led to a successful policy change effort. |
Karpyn A, Manon M, Treuhaft S, Giang T, Harries C, McCoubrey K. Policy solutions to the ‘grocery gap’. Health Aff. 2010 Mar–Apr;29(3):473–80.
Conclusion
Public health efforts to accelerate obesity prevention are increasingly focused on policy, systems, and environmental approaches. Practitioners and collaborative groups at the state and local levels, such as coalitions and other networks, are well positioned to initiate and advance this work. This article has sought to describe the policy process and identify the specific activities that have promise for promoting the adoption of active living and healthy eating policies. A key takeaway is that the policy-making process is multifaceted. It consists of three domains: problems, policy, and politics, which focus on problem identification, developing of policy solutions, and promoting a political context that supports policy change, respectively. Recommended activities in this article to advance obesity prevention policies include the following:
Assess the social and political environment. The social and political environments are powerful forces in constraining policy options. Understanding the environment can inform planning and build an awareness of the types of PSE strategies that may be possible.
Engage, educate, and collaborate. Stakeholders representing diverse constituencies should be engaged to articulate the urgency of the problem, to provide input on appropriate solutions, and to advocate for the adoption of proposed policies. Building broad engagement and support early will be beneficial in advancing other key activities.
Identify and frame the problem. Efforts aimed at PSE should frame the issue of interest in a manner that leads it to be recognized by decision makers and placed on the agenda.
Use available evidence and identify policy solutions. The identification of plausible policy solutions requires consideration of current evidence, feasibility, acceptability, reach, and impact.
Build political will. Policymakers respond positively to policy proposals that carry the support of their constituencies and colleagues, including public officials, community leaders, organized collaborative groups, and the general public (i.e. voters). It is vital to assess the local context and work cooperatively to build support across all stakeholders.
This article has suggested that engaging in these policy activities promotes increased efficiency and effectiveness in advancing policies for obesity prevention. It has also provided various policy and environmental change strategies for nutrition and physical activity (see Tables 3 and 4), although not exhaustive of possible options. Practitioners and collaborative groups should consider the approaches presented here in their planning and stakeholder convening process.
While the development and adoption of policy is important, emerging evidence suggests that policy and environmental change strategies in the absence of intentional efforts to connect people to new opportunities for physical activity and healthy eating may not have the desired impact on behavior. Policies and/or environmental changes undertaken individually are often insufficient to produce desired behavioral and health outcomes.69
Although we have focused on the portion of the policy process leading up to adoption, the process of implementation (i.e. applying and enforcing a policy change) is crucial if the policy is to achieve its intended public health impact. The governing bodies that implement policy usually differ from those that adopt policy.62 A detailed discussion of policy implementation pertaining to obesity prevention is beyond the scope of this article but should be considered in future research. The framework presented here has been guided by the literature. We believe that applications of the framework by practitioners and collaborative groups holds promise for accelerating progress on PSE strategies for obesity prevention.
Acknowledgments
This work was supported through research grants from the US Centers for Disease Control and Prevention (CDC) to the Physical Activity Policy Research Network (#U48/DP001903; 5U48DP001938-02; U48/DP001946; U48-DP000059). The content is solely the responsibility of the authors and does not necessarily represent the official views of CDC.
Footnotes
There are no conflicts of interest on the part of any of the authors.
References
- 1.Flegal K, Carroll M, Ogden C, Curtin LR. Prevalence and trends in obesity among US adults, 1999–2008. JAMA. 2010;303(3):242–249. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 2.Anonymous. [Accessed October 2, 2012];MMWR weekly report: CDC grand rounds: childhood obesity in the United States. http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6002a2.htm. [PubMed]
- 3.Koplan JP, Liverman CT, Kraak VA, editors. Institute of Medicine. Preventing Childhood Obesity: Health in the Balance. Washington, DC: The National Academies Press; 2005. http://www.nap.edu/openbook.php?record_id=11015. [PubMed] [Google Scholar]
- 4.US Department of Health and Human Services. The surgeon general’s call to action to prevent and decrease overweight and obesity. Rockville, MD: US Department of Health and Human Services, Office of the Surgeon General; 2001. Available from US GPO, Washington. [PubMed] [Google Scholar]
- 5.Brownson R, Haire-Joshu D, Luke D. Shaping the context of health: a review of environmental and policy approaches in the prevention of chronic diseases. Annu Rev Public Health. 2006;27:341–370. doi: 10.1146/annurev.publhealth.27.021405.102137. [DOI] [PubMed] [Google Scholar]
- 6.Gebbie K, Rosenstock L, Hernandez LM, editors. Institute of Medicine. Who Will Keep the Public Healthy? Educating Public Health Professionals for the 21st Century. Washington, DC: The National Academies Press; 2003. http://www.nap.edu/openbook.php?record_id=10542. [PubMed] [Google Scholar]
- 7.Stokols D. Establishing and maintaining healthy environments. Toward a social ecology of health promotion. Am Psychol. 1992;47(1):6–22. doi: 10.1037//0003-066x.47.1.6. [DOI] [PubMed] [Google Scholar]
- 8.Sallis JF, Cervero RB, Ascher W, et al. An ecological approach to creating active living communities. Annu Rev Public Health. 2006;27:297–322. doi: 10.1146/annurev.publhealth.27.021405.102100. [DOI] [PubMed] [Google Scholar]
- 9.Kumanyika SK, Parker L, Sim LJ, editors. Institute of Medicine. Bridging the Evidence Gap in Obesity Prevention: A Framework to Inform Decision Making. Washington, DC: The National Academies Press; 2010. http://www.nap.edu/openbook.php?record_id=12847. [PubMed] [Google Scholar]
- 10.Huang T, Drewnosksi A, Kumanyika S, Glass T. A systems-oriented multilevel framework for addressing obesity in the 21st century. Prev Chronic Dis. 2009;6(3):A82. [PMC free article] [PubMed] [Google Scholar]
- 11.Kopelman P, Jebb S, Butland B. Executive summary: Foresight “Tackling Obesities: Future Choices” project. Obes Rev. 2007;8(1):6–9. doi: 10.1111/j.1467-789X.2007.00344.x. [DOI] [PubMed] [Google Scholar]
- 12.The Community Preventive Services Task Force. [Accessed August 30, 2012];The guide to community preventive services (community guide) http://www.thecommunityguide.org.
- 13.Institute of Medicine. For the Public’s Health: Revitalizing Law and Policy to Meet New Challenges. Washington, DC: The National Academies Press; 2011. http://www.nap.edu/openbook.php?record_id=13093. [Google Scholar]
- 14.Mensah GA, Goodman RA, Zaza S, et al. Law as a tool for preventing chronic diseases: expanding the spectrum of effective public health strategies. Prev Chronic Dis. 2004;1(2):A11. [PMC free article] [PubMed] [Google Scholar]
- 15.Heath GW, Parra DC, Sarmiento OL, et al. Evidence-based intervention in physical activity: lessons from around the world. Lancet. 2012;380(9838):272–281. doi: 10.1016/S0140-6736(12)60816-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention. [Accessed October 2, 2012];CDC—community overview—communities putting prevention to work. http://www.cdc.gov/CommunitiesPuttingPreventiontoWork/communities/index.htm.
- 17.Robert Wood Johnson Foundation. [Accessed October 2, 2012];Childhood obesity programs and grants. http://www.rwjf.org/en/about-rwjf/program-areas/childhood-obesity/childhood-obesitygrants.html?s=66.
- 18.National Institutes of Health. [Accessed October 2, 2012];NIH obesity research funding opportunities. http://www.obesityresearch.nih.gov/funding/funding.aspx.
- 19.The Convergence Partnership. [Accessed October 2, 2012]; http://www.convergencepartnership.org/site/c.fhLOK6PELmF/b.3917533/k.F45E/Whats_New.htm.
- 20.The National Collaborative on Childhood Obesity Research (NCCOR) [Accessed October 2, 2012]; http://www.nccor.org.
- 21.Litt J, Reed H, Tabak R, et al. Active living collaboratives in the US; understanding characteristics, activities, and achievement of environment and policy change. Prev Chronic Dis. 2013;10 doi: 10.5888/pcd10.120162. 120162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Monroe J, Collins J, Maier P, et al. Legal preparedness for obesity prevention and control: a framework for action. J Law Med Ethics. 2009;37(suppl 1):15–23. doi: 10.1111/j.1748-720X.2009.00387.x. [DOI] [PubMed] [Google Scholar]
- 23.Perdue W, Ammerman A, Fleischhacker S. Assessing competencies for obesity prevention and control. J Law Med Ethics. 2009;37(suppl 1):37–44. doi: 10.1111/j.1748-720X.2009.00390.x. [DOI] [PubMed] [Google Scholar]
- 24.Schmid TL, Pratt M, Wiltmer L. A framework for physical activity policy research. J Phys Act Health. 2006;3(suppl 1):S20–S29. doi: 10.1123/jpah.3.s1.s20. [DOI] [PubMed] [Google Scholar]
- 25.Turnock M. Public Health, What It Is and How It Works. 5. Sudbury, MA: Jones and Bartlett Publishers; 2012. [Google Scholar]
- 26.Spratt K. Policy Implementation Barriers Analysis: Conceptual Framework and Pilot Test in Three Countries. Washington, DC: Futures Group, Health Policy Initiative, Task Order 1; 2009. [Accessed August 30, 2012]. http://www.aidstarone.com/resources/health_policy_initiative/policy_implementation_barriers_analysis. [Google Scholar]
- 27.Patton MQ. Qualitative Research & Evaluation Methods. 3. Thousand Oaks, CA: Sage Publications, Inc; 2002. [Google Scholar]
- 28.Kingdon J. Agendas, Alternatives, and Public Policies. New York, NY: HarperCollins College Publishers; 1995. [Google Scholar]
- 29.Stamatakis K, McBride T, Brownson R. Communicating prevention messages to policymakers: the role of stories in promoting physical activity. J Phys Act Health. 2010;7(suppl 1):S99–S107. doi: 10.1123/jpah.7.s1.s99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Klein JD, Dietz W. Childhood obesity: the new tobacco. Health Aff. 2010;29(3):388–392. doi: 10.1377/hlthaff.2009.0736. [DOI] [PubMed] [Google Scholar]
- 31.Dodd C. Health Policy. Crisis and Reform in the US Health Care Delivery System. 5. Sudbury, MA: Jones & Barlett Learning; 2008. Play to win: know the rules; pp. 15–26. [Google Scholar]
- 32.Truman D. Classics of Public Policy. New York, NY: Pearson Longman; 2005. The governmental process; pp. 83–87. [Google Scholar]
- 33.Weissert C, Weissert WG. Governing Health: The Politics of Health Policy. 4. Baltimore, MD: The Johns Hopkins University Press; 2012. [Google Scholar]
- 34.Brodie M, Blendon R. Health Politics and Policy. Clifton Park, NY: Delmar Cengage Learning; 2008. Public opinion; p. 223. [Google Scholar]
- 35.Cobb R, Elder C. Classics of Public Policy. New York, NY: Pearson Longman; 1972. The dynamics of agenda-building; pp. 128–136. [Google Scholar]
- 36.Dodson E, Fleming C, Boehmer T, et al. Preventing childhood obesity through state policy: qualitative assessment of enablers and barriers. J Public Health Policy. 2009;30(suppl 1):161–176. doi: 10.1057/jphp.2008.57. [DOI] [PubMed] [Google Scholar]
- 37.Eyler A, Brownson R, Evenson KR, et al. Policy influences on community trail development. J Health Polit Policy Law. 2008;33(3):407–427. doi: 10.1215/03616878-2008-003. [DOI] [PubMed] [Google Scholar]
- 38.Dahl R. The behavioral approach in political science: epitaph for a monument to a successful protest. Am Polit Sci Rev. 1961;55(4):763–772. [Google Scholar]
- 39.Ryan K, Card-Higginson P, McCarthy S, Justus M, Thompson J. Arkansas fights fat: translating research into policy to combat childhood and adolescent obesity. Health Aff. 2006;25(4):992–1004. doi: 10.1377/hlthaff.25.4.992. [DOI] [PubMed] [Google Scholar]
- 40.Craig R, Felix H, Walker J, Phillips M. Public health professionals as policy entrepreneurs: Arkansas’s childhood obesity policy experience. Am J Public Health. 2010;100(11):2047–2052. doi: 10.2105/AJPH.2009.183939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Stone DA. Causal stories and the formation of policy agendas. Polit Sci Q. 1989;104(2):281–300. [Google Scholar]
- 42.Niederdeppe J, Robert S, Kindig D. Qualitative research about attributions, narratives, and support for obesity policy, 2008. Prev Chronic Dis. 2011;8(2):A39. [PMC free article] [PubMed] [Google Scholar]
- 43.Aytur S, Butcher R, Carlson C, Schifferdecker K. Creating safe neighborhoods for obesity prevention: perceptions of urban youth. In: Brennan V, Kumanyika S, Zambrana R, editors. Obesity Interventions in Underserved US Populations: Evidence and Directions. Baltimore, MD: Johns Hopkins University Press; In press. [Google Scholar]
- 44.Nykiforuk C, Vallianatos H, Nieuwendyk L. Photovoice as a method for revealing community perceptions of the built and social environment. Int J Qualitative Methods. 2011;10(2):103–124. doi: 10.1177/160940691101000201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Magnusson R. What’s law got to do with it part 1: a framework for obesity prevention. Aust New Zealand Health Policy. 2008;5:5–10. doi: 10.1186/1743-8462-5-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Magnusson RS. What’s law got to do with it part 2: legal strategies for healthier nutrition and obesity prevention. Aust New Zealand Health Policy. 2008;5:5–11. doi: 10.1186/1743-8462-5-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Swinburn B, Gill T, Kumanyika S. Obesity prevention: a proposed framework for translating evidence into action. Obes Rev. 2005;6(1):23–33. doi: 10.1111/j.1467-789X.2005.00184.x. [DOI] [PubMed] [Google Scholar]
- 48.The Center for Training and Research Translation (Center TRT) [Accessed October 3, 2012]; http://www.centertrt.org/
- 49.Leeman J, Sommers J, Vu M, et al. An evaluation framework for obesity prevention policy interventions. Prev Chronic Dis. 2012;9:E120. doi: 10.5888/pcd9.110322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. [Accessed October 3, 2012];Bridging the Gap: Research Informing Policies and Practices for Healthy Youth. http://www.bridgingthegapresearch.org/
- 51.National Complete Streets Coalition. [Accessed October 3, 2012];Smart Growth America. http://www.smartgrowthamerica.org/complete-streets.
- 52.joint use. [Accessed October 3, 2012]; http://www.jointuse.org/
- 53.Farm to School. [Accessed October 3, 2012]; http://www.farmtoschool.org/
- 54.Eyler AA, Nguyen L, Kong J, Yan Y, Brownson R. Patterns and predictors of enactment of state childhood obesity legislation in the United States: 2006–2009. Am J Public Health. 2012;102(12):2294–2302. doi: 10.2105/AJPH.2012.300763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Dannenberg AL, Bhatia R, Cole BL, et al. Use of health impact assessment in the U.S.: 27 case studies, 1999–2007. Am J Prev Med. 2008;34(3):241–256. doi: 10.1016/j.amepre.2007.11.015. [DOI] [PubMed] [Google Scholar]
- 56.National Association of County & City Health Officials. [Accessed October 3, 2012]; http://www.naccho.org/
- 57.Davis FG, Peterson CE, Bandiera F, Carter-Pokras O, Brownson RC. How do we more effectively move epidemiology into policy action? Ann Epidemiol. 2012;22(6):413–416. doi: 10.1016/j.annepidem.2012.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Centers for Disease Control and Prevention. [Accessed October 3, 2012];CDC—YRBSS—youth risk behavior surveillance system—adolescent and school health. http://www.cdc.gov/HealthyYouth/yrbs/index.htm.
- 59.Resource Center for Child and Adolescent Health. [Accessed October 3, 2012];National Survey of Children’s Health—Data. http://childhealthdata.org/learn/NSCH.
- 60.Centers for Disease Control and Prevention. [Accessed October 3, 2012];NIS—National immunization survey. http://www.cdc.gov/nchs/nis.htm.
- 61.Sacks G, Swinburn BA, Lawrence MA. A systematic policy approach to changing the food system and physical activity environments to prevent obesity. Aust New Zealand Health Policy. 2008;5:13. doi: 10.1186/1743-8462-5-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Jilcott S, Ammerman A, Sommers J, Glasgow R. Applying the RE-AIM framework to assess the public health impact of policy change. Ann Behav Med. 2007;34(2):105–114. doi: 10.1007/BF02872666. [DOI] [PubMed] [Google Scholar]
- 63.Glasgow R, Vogt T, Boles S. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health. 1999;89(9):1322–1327. doi: 10.2105/ajph.89.9.1322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Pomeranz J, Brownell K. Advancing public health obesity policy through state attorneys general. Am J Public Health. 2011;101(3):425–431. doi: 10.2105/AJPH.2010.198697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Salvesen D, Evenson KR, Rodriguez D, Brown A. Factors influencing implementation of local policies to promote physical activity: a case study of Montgomery County, Maryland. J Public Health Manag Pract. 2008;14(3):280–288. doi: 10.1097/01.PHH.0000316487.57512.f6. [DOI] [PubMed] [Google Scholar]
- 66.Sacks G, Swinburn B, Lawrence M. Obesity policy action framework and analysis grids for a comprehensive policy approach to reducing obesity. Obes Rev. 2009;10(1):76–86. doi: 10.1111/j.1467-789X.2008.00524.x. [DOI] [PubMed] [Google Scholar]
- 67.Blouin C, Dube L. Global health diplomacy for obesity prevention: lessons from tobacco control. J Public Health Policy. 2010;31(2):244–255. doi: 10.1057/jphp.2010.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Karpyn A, Manon M, Treuhaft S, Giang T, Harries C, McCoubrey K. Policy solutions to the ‘grocery gap’. Health Aff. 2010;29(3):473–480. doi: 10.1377/hlthaff.2009.0740. [DOI] [PubMed] [Google Scholar]
- 69.Blacksher E, Lovasi G. Place-focused physical activity research, human agency, and social justice in public health: taking agency seriously in studies of the built environment. Health Place. 2012;18(2):172–179. doi: 10.1016/j.healthplace.2011.08.019. [DOI] [PubMed] [Google Scholar]