Abstract
Introduction:
Hypertension is a major cause of cardiovascular morbidity and mortality in Kerala. Excess dietary salt, low dietary potassium, overweight and obesity, physical inactivity, excess alcohol, smoking, socioeconomic status, psychosocial stressors, and diabetes are considered as modifiable risk factors for hypertension.
Objectives:
To estimate and compare the distribution of modifiable risk factors among hypertensive (cases) and nonhypertensive (controls) patients and to estimate the effect relationship of risk factors.
Materials and Methods:
Age- and sex-matched case–control study was conducted in a tertiary care hospital in Kerala using a pretested interviewer-administered structured questionnaire based on the WHO STEPS instrument for chronic disease risk factor surveillance. Bivariate and multiple logistic regression analyses were done.
Results:
A total of 296 subjects were included in the study. The mean age of study sample was 50.13 years. All modifiable risk factors studied vis-ΰ-vis obesity, lack of physical activity, inadequate fruits and vegetable intake, diabetes, smoking, and alcohol use were significantly different in proportion among cases and controls. Obesity, lack of physical activity, smoking, and diabetes were found to be significant risk factors for hypertension after adjusting for other risk factors.
Conclusion:
Hypertension is strongly driven by a set of modifiable risk factors. Massive public awareness campaign targeting risk factors is essential in controlling hypertension in Kerala, especially focusing on physical exercise and control of diabetes, obesity, and on quitting smoking.
Keywords: Case–control study, hypertension, Kerala, risk factors of hypertension, WHO STEPS
Introduction
Hypertension is a disease entity of its own. It remains silent being asymptomatic during its clinical course. Because of its asymptomatic appearance, it does immense harm to the body in the form of target organ damage, hence the WHO has named it the “silent killer.” Hypertension is a major cause of cardiovascular morbidity and mortality worldwide.[1] Excess dietary salt, low dietary potassium, overweight and obesity, physical inactivity, excess alcohol, smoking, socioeconomic status, psychosocial stressors, and diabetes are considered as modifiable risk factors for hypertension.[2]
Globally, hypertension is estimated to cause 7.5 million deaths a year which is roughly 12.8% of the total. Hypertension is directly responsible for 57% of all stroke deaths and 24% of all coronary heart disease in India.[3] Studies in Kerala (Criteria: JNC VI) reported 37% prevalence of hypertension among 30–64 age group (43) in 1998 and 55% among the age group of 40–60 years during 2000.[4] A higher prevalence of 69% and 55% was recorded among elderly populations aged sixty and above in the urban and rural areas, respectively, during 2000.[5] Soman[6] in one of his articles in 2007 has demonstrated that only Scotland, among the countries chosen has higher cardiovascular mortality than rural Kerala and that ischemic heart disease (IHD) mortality in Kerala is nearly 3 times higher than that in France and even the United States fare better than Kerala in IHD mortality whereas the differences in stroke mortality are not as striking.[7]
The Government of India launched a flagship program called the National Rural Health Mission (NRHM) in 2005[8] with an objective of expanding access to quality health care to rural populations by undertaking architectural corrections in the institutional mechanism for health care delivery. The Central Government of India started the National Program for Prevention and Control of Cancer, Diabetes, CVD and Stroke (NPCDCS) in the 12th plan period.[9] The NPCDCS program has two components, viz. (i) Cancer and (ii) Diabetes, CVDs and Stroke. These two components have been integrated at different levels as far as possible for optimal utilization of the resources.
Kerala was the first state to start a comprehensive control program even before the formal launch of NPCDCS in the state.[10] The essential component of this program is ASHA service and NRHM machinery working together with state health service system at various levels. This program has been pilot tested in 2008–2009 in a Neyyattinkara Taluk in Trivandrum district and in Wayanad district and was proved successful in improving the efficiency, accessibility, and equity in noncommunicable diseases (NCDs) care in the pilot areas. During 2009–2010, the project was expanded to the whole of Trivandrum district and on April 7, 2010, under the auspices of Health Services department and NRHM, the program was rolled out across the state.
Materials and Methods
The objectives of the study described here, were to understand the prevalence of selected modifiable risk factors associated with hypertension, compare the distribution of these factors among hypertensive patients (cases) and nonhypertensive patients (controls), and estimate the effect relationship of modifiable risk factors and hypertension.
A hospital-based observational study using a matched case–control study design (age group and sex-matched) was conducted in a tertiary care private hospital in the city of Kochi, Kerala, from December 2011 to November 2012. The sampling frame consisted of all patients who came to the outpatient department during the study period. From them, only those who qualified the inclusion criteria as either a case or control were included in the analysis. Purposive sampling was done to match cases and control – both in terms of sex and age group. Sample size was estimated to be 282 as per Fleiss formula.[11]
Cases were defined as patients who were already diagnosed with hypertension by a physician (as per JNC 7 Classification), and/or patients who are already on blood pressure-lowering medication(s) for hypertension. All prevalent cases were included (old and newly diagnosed) in the study. Controls were defined as other patients attending the same outpatient service with no history of hypertension matched by age group and sex and whom the blood pressure recorded on the day of study is normal. All willing patients aged between 35 and 65 years were included in the study. Among cases, those who were known cases of secondary hypertension and antenatal females were excluded while among controls, those patients whose blood pressure was not normal on the day of study were also excluded from the study. They were not included as cases either.
Data was collected by a single researcher with the help of a structured questionnaire. The questionnaire was essentially a modified WHO STEPS instrument (Questionnaire) for chronic disease risk factor surveillance.[12] Data was entered in Microsoft Excel. Ten percent data was re-entered and these were validated. The analysis was performed using SPSS statistical program version 12.0 (SPSS, Inc., Chicago, IL, USA). Simple proportions were done for all the relevant variables studied among cases and control and the overall sample with confidence interval (CI) fixed at 95%. The proportions of relevant risk factors were compared between cases and controls and whether the difference was statistically significant was arrived at. Crude odds ratios (ORs) and adjusted ORs by logistic regression analysis were done to understand the interplay of relevant risk factors as well.
Ethical clearance for this study was obtained from the Institutional Ethics Committee of the hospital. Informed written consent was obtained from all the participants.
Results
Sample characteristics
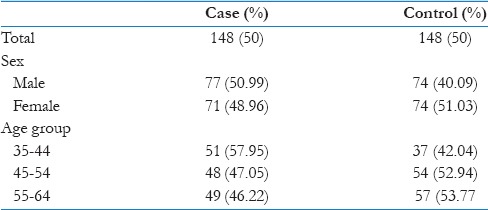
The distribution of study subjects age group and sex-wise is as shown in Table 1. Seven percent were widowed while 3% were unmarried. There were almost equal proportion of cases and controls among the three religious groups of Hindu, Muslim, and Christian. More than one-third reported a monthly income of more than INR 10,000.
Table 1.
Age and sex distribution of subjects
More than 95% were primary school completed and at least a quarter were graduates while 3.38% were having professional qualifications of all the study subjects. Between cases and controls upon classifying into graduates and above versus nongraduates, no significant difference was observed with 33.1% of them being graduates and above among controls and 41.2% among cases. Of the total subjects, 40% of the participants were homemakers and only 3% were unemployed. Most of the males were self-employed while females were mostly homemakers.
Blood pressure
The mean systolic blood pressure among cases and controls were 135.55 and 117.97 mmHg, respectively, while mean diastolic blood pressure were 83.47 and 75.62 mmHg, respectively.
Anthropometric values
Mean body mass index (BMI) of study population was 25.17 kg/m2 with 95% CI range 24.73; 25.61. Females had higher BMI both among cases and controls across all age groups. Hip circumference among study subjects varied between 65 and 143 cm with a mean value 98.28 cm (95% CI: 97.24; 99.31). Among control, the mean value was 96.41 with standard deviation (SD) 7.65 while among cases it was 100.15 with SD 9.97. Among males, hip circumference was 96.66 ± 7.43 cm while in females it was 99.96 ± 10.26 cm.
Family history
A total of 113 cases (76.4%) had family history of both hypertension and diabetes while only 35 controls (23.6%) had both of them together, the difference being statistically significant (P < 0.001).
Modifiable risk factors
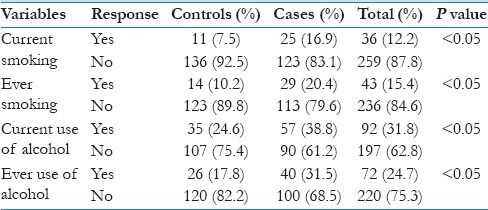
Current smoking and ever smoking were significantly different in proportion among cases and controls; proportion of current smokers among cases was more than double compared to controls (16.9% vs. 7.5%). It was found that close to one-third of the total cases were currently using alcohol of which 97.2% being males, details of which are provided in Table 2.
Table 2.
Smoking and alcohol
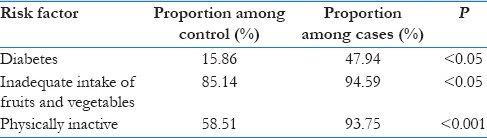
All the study subjects were overweight while more than 50% of study subjects were obese. Obesity varied significantly between cases and control (27.7% among controls vs. 77.7% among cases, P < 0.001). Comparison of other risk factors analyzed is summarized in Table 3.
Table 3.
Diabetes, diet and physical activity
Bivariate and multivariate analyses
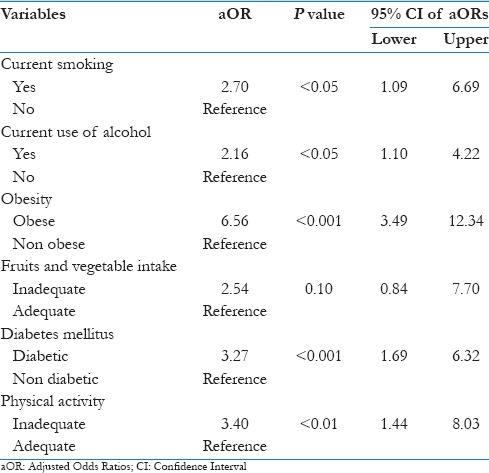
The effect of various risk factors on hypertension was computed in terms of ORs. Crude ORs of all relevant risk factors were analyzed in bivariate analysis, the summary of which is given in Table 4. Variables that were statistically significant in the bivariate analysis were included in the logistic regression model to evaluate the association of selected predictor variables with hypertension. A two-sided P < 0.05 was considered statistically significant.
Table 4.
Results of bivariate analysis
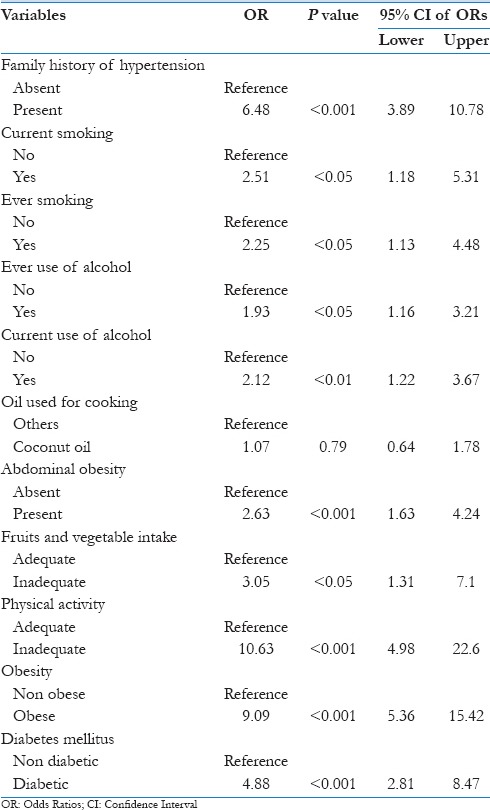
Smoking, alcohol use, physical activity, obesity, abdominal obesity, fruits and vegetable intake, and having food outside home – all were significantly different between cases and controls. The association between risk factors and hypertension explained by ORs showed strong association between hypertension and smoking, alcohol use, physical inactivity, obesity, less fruits and vegetable intake, and abdominal obesity. After adjusting for other variables, diabetes, obesity, physical inactivity, smoking and alcohol emerged as independent risk factors for Hypertension [Table 5].
Table 5.
Results of logistic regression
Discussion
The study reiterates that the current epidemic of hypertension in Kerala can well be linked to known risk factors such as smoking, alcohol use, physical inactivity, obesity, less fruits and vegetable intake, and abdominal obesity. Hypertension study group,[5] which included one of the cities of Kerala, identified a higher BMI and prevalent diabetes mellitus important correlates of the prevalence of hypertension. Findings from the Fletcher Challenge-Auckland University Heart and Health Study[13] by Bullen et al., showed that adjustment for BMI and alcohol consumption almost eliminated ethnic differences in blood pressure, and BMI was found to be the single most important modifiable determinant of raised blood pressure. Efforts to reduce obesity have the potential to significantly reduce raised blood pressure. A study in Kerala by Thankappan et al.[14] however showed that tobacco use was not a risk factor (OR = 0.75) while alcohol users and those who were physically inactive had higher risk of developing hypertension.
Regular physical activity reduces the risk of cardiovascular disease including high blood pressure, diabetes, breast and colon cancer, and depression. People who do not take enough aerobic exercise (such as brisk walking, running, cycling, swimming, or dancing) are more likely to have or to develop hypertension. In this context, it may be noted that due to change in lifestyle with the change in job pattern, even in Kerala physical activity is decreasing among people of all age groups. Information technology-oriented jobs which involve very little physical labor, increasing affordability of two and four wheelers, decreasing availability of playgrounds, decrease in agricultural activities- all would have contributed to the decrease in physical activities among people of Kerala. Blood pressure rises when large amounts of alcohol are consumed, in some cases to dangerous levels– particularly binge drinking.[15] Kerala has the highest per capita alcohol consumption in the country. Alcohol-induced liver diseases and other NCDs are on the rise in Kerala. Binge drinking is on the rise with the availability of relatively cheaper brands through the government-owned outlets itself which is draining the health as well as the economy of the state. Adequate consumption of fruit and vegetables reduces the risk for cardiovascular diseases. Most populations consume much higher levels of salt than recommended by the WHO for disease prevention; high salt consumption is an important determinant of high blood pressure and cardiovascular risk. High consumption of saturated fats and trans-fatty acids is linked to heart disease. An unhealthy diet is rising quickly in lower-resource settings. Available data suggest that fat intake has been rising rapidly in lower-middle-income countries since the 1980s.[16] Fruits and vegetable consumption pattern is swiftly changing in Kerala. Once, vegetables constituted a significant proportion of daily food intake. However, with the fast-food culture emerging faster even in rural areas, intake of fruits and vegetables is coming down. At least 2.8 million people die each year as a result of being overweight or obese.[16] Risks of heart disease, strokes, and diabetes increase steadily with increasing BMI. Raised BMI also increases the risk of certain cancers. Obesity multiplies the risk of developing hypertension about fourfold in men and threefold in women.[17] Kerala men and women are increasingly becoming obese. It was also significant to note that all the study subjects in this study were overweight. Lack of physical activity and unhealthy diet are two important factors pushing this trend.
Hypertension is more prevalent in people with Type 1 and Type 2 diabetes than in the nondiabetic population, whether or not they are overweight. With the much less common Type 1 diabetes, hypertension is mostly a consequence of kidney damage.[17] With Type 2 diabetes, the causative factor is thought to be insulin resistance or “metabolic syndrome,” but the mechanism is not fully understood.[18] Kerala is fast emerging as the diabetic capital of India. Prevalence of diabetes is increasing across the state, rural and urban, men and women alike. Adequate control of diabetes requires suitable medical management including lifestyle interventions - both at individual level and community/state level. Lifestyle interventions are welcomed and are viewed as helpful by patients receiving them. However, potential health gains among high-risk hypertensives are being lost because of poor targeting and coverage of those at greatest risk.[19] So it is important to note that all hospitals where a significant number of Hypertensive patients or other NCD patients is treated should have systematic counseling sessions for these patients in lifestyle modification.
Conclusion
The study finding is consistent with the existing knowledge about risk factors of hypertension. Smoking, alcohol use, physical inactivity, less fruit and vegetable intake, and diabetes all are driving forces behind the rising epidemic of hypertension. Addressing these risk factors is essential in controlling the epidemic of hypertension, which in turn is driving the other major NCDs as well.
Lifestyle changes are the cornerstone in determining how the epidemic of hypertension will move now on. Kerala has achieved a remarkable progress in terms of human development and health of the people. Maternal mortality, child mortality, education status, and immunization status, etc. are all comparable with the most developed nations of the world. The state has achieved these with minimum investments and low-cost interventions. Awareness among the community was the major factor, education being a driving force behind. Kerala is therefore an ideal place to have interventions related to lifestyle modifications which have proved beyond doubt to help control the burden of NCDs, hypertension being one of the most important ones. Therefore, the state should immediately start implementing the core strategies under the national framework to control hypertension. This requires adequate facilities to diagnose and treat hypertension at the earliest.
Recommendations
Diagnosis of hypertension is not complicated and therefore more important is the follow-up and availability of medicines at the lowest point of care itself. Cost of medicines should not lead to interruption in treatment, which may prove fatal. However this is only secondary prevention. Primary prevention should aim at detecting borderline cases of hypertension, which can be achieved by regular screening of people for hypertension. In such people, adequate lifestyle modification at an early stage can prevent hypertension. Primordial prevention should aim at modifying lifestyles in young groups. Young people should be taught about the important of lifestyle diseases from school days itself. The state should promote the formation of health clubs in schools, colleges and panchayat level. There should be adequate facilities in all towns and city residential areas where people can go for walking or exercise. Even though much is known about the risk factors of hypertension, it may be worth undertaking more detailed studies such as prospective cohort studies, which may further increase our knowledge about risk factors and their interplay. Population-based health registries should collect information about risk factors, and the changes in trend in risk factors among various population groups and geographical areas which may help in planning and implementing specific interventions which will help reduce or modify risk factors of hypertension.
Limitations of the study
The study being a case–control design has all the inherent limitation of such a design like the difficulty to establish the temporality between cause and effect, information bias regarding exposure status due to reliance on recall, and potential bias in selection of controls. Because of shortage of time and resources, in the questions regarding fruits and vegetable intake, exact weight of fruits and vegetable intake could not be ascertained and therefore proxy measurements were used for analysis.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.World Health Organization. A global brief on hypertension. Geneva: World Health Organization; 2013. [Google Scholar]
- 2.Institute of Medicine. A Population. Based Policy and Systems Change Approach to Prevent and Control Hypertension. Washington, DC: The National Academies Press; 2010. [Last accessed on 2016 Mar 1]. Available from: http://www.nap.edu/catalog.php?record_id=12819 . [PubMed] [Google Scholar]
- 3.Murray CJ, Lopez AD. Mortality by cause for eight regions of the world: Global Burden of Disease Study. Lancet. 1997;349:1269–76. doi: 10.1016/S0140-6736(96)07493-4. [DOI] [PubMed] [Google Scholar]
- 4.Zachariah MG, Thankappan KR, Alex SC, Sarma PS, Vasan RS. Prevalence, correlates, awareness, treatment, and control of hypertension in a middle-aged urban population in Kerala. Indian Heart J. 2003;55:245–51. [PubMed] [Google Scholar]
- 5.Hypertension Study Group. Prevalence, awareness, treatment and control of hypertension among the elderly in Bangladesh and India: A multicentre study. Bull World Health Organ. 2001;79:490–500. [PMC free article] [PubMed] [Google Scholar]
- 6.Soman CR. Fifty years of primary health care: The Kerala experience. NFI bulletin. Bull Nutr Found India. 2007;28:1–5. [Google Scholar]
- 7.World Health Organization. World Health Statistics. 2007. [Last accessed on 2016 March 1]. pp. 197–99. Available from http://www.who.int/gho/publications/world_health_statistics/whostat2007.pdf?ua=1 .
- 8.National Rural Health Mission. Website of NRHM. [Last accessed on 2015 Sep 18]. Available from: http://www.nrhm.gov.in/
- 9.NCD Alliance. [Last accessed on 2015 Sep 18]. Available from: http://www.ncdalliance.org/node/3497 .
- 10.NRHM Kerala Website. [Last accessed on 2015 Sep 18]. Available from: http://www.arogyakeralam.gov.in .
- 11.Fleiss JL. Statistical Methods for Rates and Proportions. 2nd ed. New York: John Wiley & Sons, Inc; 1981. [Google Scholar]
- 12.Bonita R, de Courten M, Dwyer T, Jamrozik K, Winkelmann R. Surveillance of risk factors for non-communicable diseases: The WHO STEP wise approach. Geneva: World Health Organization; 2002. [Google Scholar]
- 13.Bullen C, Tipene-Leach D, Vander Hoorn S, Jackson R, Norton R, MacMahon S. Ethnic differences in blood pressure: Findings from the Fletcher Challenge-Auckland University Heart and Health Study. N Z Med J. 1996;109:395–7. [PubMed] [Google Scholar]
- 14.Thankappan KR, Shah B, Mathur P, Sarma PS, Srinivas G, Mini GK, et al. Risk factor profile for chronic non-communicable diseases: Results of a community-based study in Kerala, India. Indian J Med Res. 2010;131:53–63. [PubMed] [Google Scholar]
- 15.Marques-Vidal P, Arveiler D, Evans A, Amouyel P, Ferrières J, Ducimetière P. Different alcohol drinking and blood pressure relationships in France and Northern Ireland: The PRIME Study. Hypertension. 2001;38:1361–6. doi: 10.1161/hy1101.095328. [DOI] [PubMed] [Google Scholar]
- 16.Ibrahim MM, Damasceno A. Hypertension in developing countries. Lancet. 2012;380:611–9. doi: 10.1016/S0140-6736(12)60861-7. [DOI] [PubMed] [Google Scholar]
- 17.Nishimura R, LaPorte RE, Dorman JS, Tajima N, Becker D, Orchard TJ. Mortality trends in type 1 diabetes. The Allegheny County (Pennsylvania) Registry 1965-1999. Diabetes Care. 2001;24:823–7. doi: 10.2337/diacare.24.5.823. [DOI] [PubMed] [Google Scholar]
- 18.Lender D, Arauz-Pacheco C, Adams-Huet B, Raskin P. Essential hypertension is associated with decreased insulin clearance and insulin resistance. Hypertension. 1997;29(1 Pt 1):111–4. doi: 10.1161/01.hyp.29.1.111. [DOI] [PubMed] [Google Scholar]
- 19.Foss FA, Dickinson E, Hills M, Thomson A, Wilson V, Ebrahim S. Missed opportunities for the prevention of cardiovascular disease among British hypertensives in primary care. Br J Gen Pract. 1996;46:571–5. [PMC free article] [PubMed] [Google Scholar]


