Abstract
Objective:
The study was conducted to determine the point prevalence of depression and anxiety in patients suffering from tuberculosis.
Material and Methods:
Total of 100 consecutive cases were included who were already diagnosed with tuberculosis after applying inclusion and exclusion criteria. Tools used were General Health Questionnaire 12 (GHQ-12), Beck Depression Inventory (BDI-II) and Hamilton Anxiety Rating Scale (HARS).
Result:
Out of 100 cases, 74 cases found to be having psychiatric symptoms, in which 35 cases were suffering from depression and 39 were suffering from anxiety.
Conclusion:
Psychiatric morbidity was present in the diagnosed cases of tuberculosis. Proper psycho education, timely intervention in the form of proper diagnosis and specific treatment was required. It should also be evaluated further on a bigger target population.
Keywords: Depression, generalized anxiety disorder, tuberculosis
Introduction
Tuberculosis has been present in human beings since ages. It is caused by the bacteria Mycobacterium tuberculosis (Lishman WA: Organic psychiatry).[1] The prevalence of tuberculosis is more common in India because of poor sanitation and hygiene, overcrowding, low education level, malnutrition, and poor diagnostic and treatment facilities. India is the country with the highest burden of tuberculosis (K Park text book of preventive and social medicine).[2] The World Health Organization statistics for 2014 give an estimated incidence of 2.2 million cases of tuberculosis for India out of a global incidence of 9 million. Still today, tuberculosis is one of the leading causes of morbidity and mortality worldwide (Issa BA et al).[3] As tuberculosis is a chronic illness, it always interferes life physically, psychosocially, and also economically. It can result in unemployment, prolonged hospitalization resulting in abstinence from job, isolation, perception of being infected, significant weight loss, decreased libido, hopelessness, resulting in decreased social interaction. In India, there is always a social stigma associated with the illness. (Bhatia et al)[4,5]
Moffic and Paykel et al (1975)[6] and Stephanie Cavanaugh et al (1983)[7] worked on depression in patients who were admitted to medical wards for general medical conditions. They indicated that 24% of patients meet the criteria for the depression which is less than the depression in tuberculosis patients. Purohit et al.[8] worked on depression in hospitalized tuberculosis patients and observed that approximately 54% of patients had suffered from depression. It was related with the severity and duration of tuberculosis. Moran MG[9] worked on the concept that how emotional stress can predispose to acquire or relapse tuberculosis and how our reactions to the illness affect the recovery process. Bhatia et al[10] studied the psychiatric pattern in tuberculosis patients, attending the outpatient door (OPD) in GTB Hospital, Delhi. They observed that 78% of patients had comorbid psychiatric problems. Duko et al.[11] have also found the prevalence of depression and anxiety among tuberculosis patients were 43.4% and 41.5%, respectively. Depression and anxiety disorders are frequently seen psychiatric disorders in patients with tuberculosis. The presence of depression and anxiety in tuberculosis patients leads to poor compliance to the antitubercular treatment resulting in poor prognosis, ultimately increasing the morbidity and mortality due to tuberculosis. Aghauwa HS et al.[12] found a significance higher prevalence of psychiatric disorder was found in the tuberculosis group (30.2%) than in the orthopedic group (15%) and the apparently healthy control (5%).
Materials and Methods
The study was performed on 100 consecutive cases who were diagnosed with tuberculosis by the Department of Respiratory Medicine and referred to the Department of Psychiatry from February 2015 to November 2015. Patients of age group between 20 and 70 years from both genders, from all communities, from all socioeconomic classes, and willing to participate were included in the study. Patients who were not willing to participate were excluded from the study. Patients with previous psychiatric history were also excluded from the study. General Health Questionnaire-12 (GHQ-12) was applied initially to all 100 cases, out of which those who scored ≥3 were further qualified for application of Beck Depression Inventory-II (BDI-II) and Hamilton Anxiety Rating Scale (HARS) questionnaire to assess the severity of depression and anxiety, respectively. Kaplan HI, Sadock BJ (2003) Synopsis of psychiatry[13]
Results and Discussion
A total of 100 cases were included in this study who were referred from the Department of Respiratory Medicine to the Psychiatry OPD and fulfilled the inclusion/exclusion criteria. Analysis of data revealed that psychiatric symptoms were present in patients suffering from tuberculosis. Seventy-four percent of the cases scored ≥3 in GHQ-12. Aydin IO, et al.,[14] in his study also applied GHQ-12 as a screening tools and found depression and anxiety in patients suffering from tuberculosis & COPD. It could be due to its chronicity, diagnostic dilemmas, long and costly treatments, social stigma associated with it, medical problems (such as infertility, pain, and breathlessness) due to it. Sometimes, poor drug compliance leads to incomplete treatment which results in relapses causing great stress to the patients. Physical weakness associated with the disease leads to frequent abstinence from the workplace, which adds to more stress financially. Poor social support system gives patients a feeling of being neglected, isolated, and worthless. The aim of this study was to define and understand the stresses to which average tuberculosis patients are subject to along with the common ways of dealing with such stresses. Underlying this aim is the hope that such understanding will lead to developing ways of helping the patients to achieve an optimal adjustment. During interview, it was observed that before the diagnosis, patients had apprehension, insomnia, irritability, and restlessness. They had fear of death, decreased sleep, and appetite with decreased interest in interaction with people due to complications of the disease and uncertainty of diagnosis. Once the diagnosis is made and treatment is started, patients feel relaxed and show sense of relief but very soon become anxious, irritable, and depressed due to worry about the nature of disease and its complications and prognosis. Hence, they want more and more information. Intermittent episodes of aggression and irritability were reported by family members. It was felt that emotional maturity and education level were important factors for proper adaptation to treatment. Some researchers have observed that adolescent patients tend to comply less well to drug treatment than adult or older patients. They are irregular in taking medicines; they keep on abusing drugs or alcohol. They are more conscious about the changes in body functions and appearance. They are more hostile and aggressive than the adult patients. Even interview with these patients was difficult. They showed anger and noncooperation toward staff and treating physicians. Compliance to diet is poor. However, suicidal ideation was less prevalent than older patients, may be due to regression. Adult patients are more prone for the depression as they are very much concerned for their job loss, burden of expenses in the treatment, reversal of role in their family from bread earner to dependent one. Bhatia MS et al.[15] found Decreased libido and sexual performance also increases their anxiety and depression. Patients of older age groups are more vulnerable for the psychiatric complications. Mayou R et al.[16] mentioned in his study that they are totally dependent on their family, they feel neglected and isolated. Other medical conditions such as diabetes and hypertension aggravate the condition. Due to poor social support, these patients are more susceptible for the psychiatric complications.
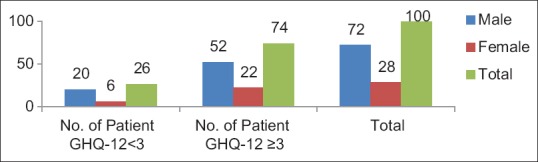
GHQ-12 applied on all 100 cases, out of which 74 patients scored ≥3which shows that 74% of cases were having psychiatric symptoms [Table 1 and Figure 1]
Data in Table 2 show that patients who have psychiatric symptoms, i.e., 74 cases, in which thirty cases belong to 20–40 years of age group, which shows that psychiatric symptoms present more in elderly cases suffering from tuberculosis [Figure 2]
Data in Table 3 indicate that psychiatric symptoms are more in male patients as compared to female, i.e., 70.27% and 29.72%, respectively [Figure 3]
Data in Table 4 suggest that Muslim cases have higher incidence of psychiatric symptoms as compared to Hindu cases, i.e., 55.71% and 44.28%, respectively [Figure 4]
Table 5 indicates that out of 74 cases, 39 cases scored ≥14 on HARS, which shows that 52.71% cases suffering from anxiety disorders [Figure 5]
Data in Table 6 show that out of 74 cases, 35 cases scored ≥13 in BDI-II, which shows 47.29% suffering from depressive disorders [Figure 6].
Table 1.
Number of cases screened using General Health Questionnaire-12
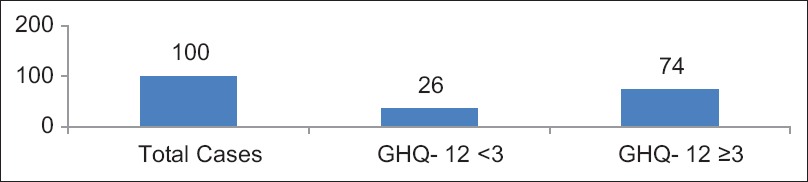
Figure 1.
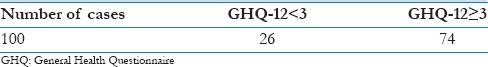
GHQ-12 Score ≥3 OR <3
Table 2.
Distribution of age (years)
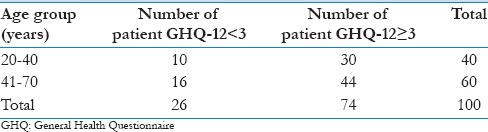
Figure 2.
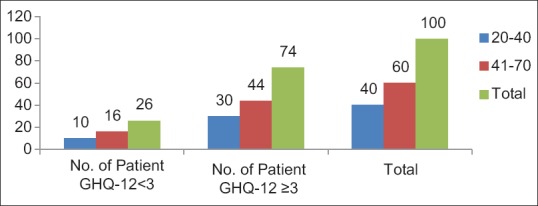
Distribution of age
Table 3.
Distribution of gender
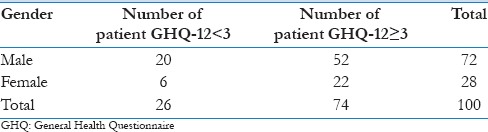
Figure 3.
Distribution of gender
Table 4.
Distribution of religion
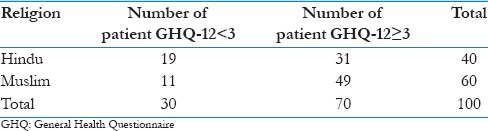
Figure 4.
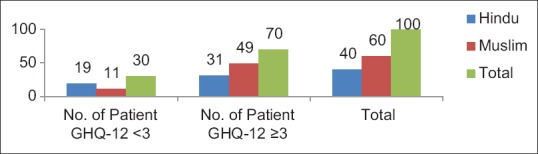
Distribution of religion
Table 5.
Distribution of cases with anxiety disorders
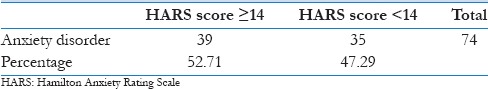
Figure 5.
HARS score< OR ≥14
Table 6.
Distribution of cases with depressive disorders
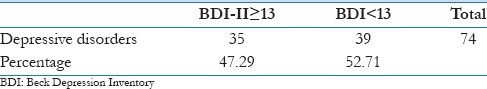
Figure 6.
BDI score <13 OR ≥13
Conclusion
Psychiatric morbidity was present in the diagnosed cases of tuberculosis and it should be evaluated further on a bigger target population
Proper psychoeducation, timely intervention in the form of proper diagnosis, and specific treatment required
Poor compliance to the treatment is most frequently encountered while treating these case due to lack of social and family support and the stigma associated with the illness
Prevention and cure of patient suffering from tuberculosis is a must to eradicate this illness
Comorbid illness should be identified for better prognosis and treatment of the illness
Appropriate referral should be made for comorbid illness if present in a patient suffering from tuberculosis.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Lishman WA. Organic Psychiatry. 3rd ed. Oxford: Blackwell; 1996. pp. 366–7. [Google Scholar]
- 2.K Park's Text Book of Preventive and Social Medicine. 17th ed. Jabalpur Banarsi Das bhanot Publication; 2002. [Google Scholar]
- 3.Issa BA, Yusuf AD, Kuranga SI. Depressive comorbidity among patients with tuberculosis in University teaching hospital outpatient clinic in Nigeria. Ment Health Fam Med. 2009;6:130–8. [PMC free article] [PubMed] [Google Scholar]
- 4.Bhatia MS, Bhasin SK, Dubey KK. Psychosocial dysfunction in tuberculosis patients. Ind J Med. 2000;54:171. [PubMed] [Google Scholar]
- 5.Bhatia MS, Bhasin SK, Dubey KK. Psychological reactions amongst patients, their family members and the community regarding hospitalized tuberculosis patients in Delhi. Psychiatry Today. 1998;11:30. [Google Scholar]
- 6.Moffic HS, Peykel ES. Depression in medical ill patients. Br J Psychiatry. 1975;126:346–53. doi: 10.1192/bjp.126.4.346. [DOI] [PubMed] [Google Scholar]
- 7.Cavanaugh S, Clark DC, Gibbons RD. Diagnosing depression in the hospitalised medically ill. Psychosomatics. 1983;24:809–15. doi: 10.1016/S0033-3182(83)73151-8. [DOI] [PubMed] [Google Scholar]
- 8.Purohit DR, Purohit SD, Dhariwal ML. Incidence of depression in hospitalized tuberculosis patients. Indian J TB. 1978;25:147–51. [Google Scholar]
- 9.Moran MG. Psychiatric aspects of the tuberculosis. Adv Psychosom Med. 1985:109–18. doi: 10.1159/000411840. [DOI] [PubMed] [Google Scholar]
- 10.Bhatia MS, Bhasin SK, Dubey KK, Narendra Sindhi. Psychiatric morbidity in tuberculosis patients. Ind Med Gazette. 2000;134(1):5–6. [Google Scholar]
- 11.Duko B, Gebeyehu A, Ayano G. Correlates of depression and Anxiety among patients with tuberculosis at wolaita Sodo University Hospital and Sodo Health Center, Wolaita Sodo, South Ethiopia, Cross sectional study. BMC Psychiatry. 2015;15:214. doi: 10.1186/s12888-015-0598-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Aghanwa HS, Erhabor GE. Demographic/Socioeconomic factors in mental disorders associated with tuberculosis in South West Nigeria. J psychosom Res. 1998;45:353–60. doi: 10.1016/s0022-3999(98)00006-3. [DOI] [PubMed] [Google Scholar]
- 13.Kaplan HI, Sadock BJ. Synopsis of psychiatry. Philadelphia, Pa: Lippincott Williams & Wilkins; 2003. [Google Scholar]
- 14.Aydin IO, Ulusahin A. Depression, anxiety comorbidity and disability in tuberculosis and chronic obstructive pulmonary disease patients: Applicability of GHQ- 12. Gen. Hosp Psychiatry. 2001;23:77–83. doi: 10.1016/s0163-8343(01)00116-5. [DOI] [PubMed] [Google Scholar]
- 15.Bhatia MS, Bhasin SK, Dubey KK. Impact of Tuberculosis on sexual relationship amongst hospitalized patients. Indian Practitioner. 1999;52:680. [Google Scholar]
- 16.Mayou R, Hawton K. Psychiatric disorders in the general hospital. Br J Psychiatry. 1986;149:172–190. doi: 10.1192/bjp.149.2.172. [DOI] [PubMed] [Google Scholar]


