Abstract
Neuroleptic malignant syndrome (NMS) is a life-threatening emergency that is often seen as a complication of antipsychotic agents. It is characterized by a tetrad of motor, behavioral, autonomic, and laboratory abnormalities. We report a case of a 34-year-old man with a history of newly diagnosed Type 2 diabetes mellitus, mental retardation, and behavioral abnormalities who developed NMS after starting on antipsychotic agents. He presented with high temperature, muscle rigidity, tachycardia, and elevated blood pressure. After a week of hospital treatment in the general ward of a secondary care unit, he was discharged in a hemodynamically and mentally stable state.
Keywords: Antipsychotic agents, family physician, neuroleptic malignant syndrome
Introduction
Neuroleptic malignant syndrome (NMS) is a rare but life-threatening complication to antipsychotic agents. It was initially reported in 1960s[1] and since then many cases have been recognized worldwide. NMS is associated with a significant mortality rate and requires early recognition and prompt treatment. Early diagnosis of NMS can be a clinical challenge to family physicians who treat patients with both medical and psychiatric conditions. With increasing the use of antipsychotic agents in primary and secondary care setting, NMS can be missed if not suspected in patients on antipsychotics presenting in general practice with hyperthermia and muscle rigidity. We report a case of NMS diagnosed in a patient with poorly controlled diabetes in the Urban Health Center at Vellore, Tamil Nadu, India.
Case Report
A 34-year-old male with history of Type 2 diabetes mellitus on oral hypoglycemic agents was hospitalized twice with symptoms of ketosis. He was treated with Insulin, intravenous fluids, and supportive therapy. He was discharged on twice daily dosing of mixtard insulin. Poor drug compliance, poor motivation regarding diabetes care, and psychomotor agitation were noted during hospitalization. Psychiatry consultation was sought for behavioral abnormalities. On psychiatry evaluation, the patient was diagnosed to have mental retardation with psychotic features. He was started on risperidone at a dose of 1 mg twice daily.
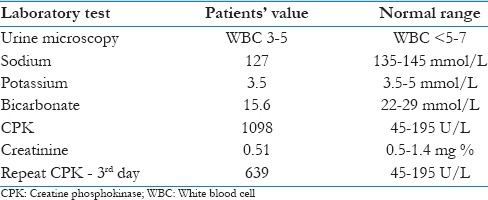
One week after starting on antipsychotics, he presented with extrapyramidal symptoms of dystonia, parkinsonian gait, fine tremors, high spiking fever, altered sensorium, and muscle rigidity. He was hospitalized and started on supportive therapy. Blood counts, urine microscopy, and renal function were normal except for low sodium [Table 1]. Creatine phosphokinase (CPK) was ordered in view of muscle rigidity that was very high (1543). A diagnosis of NMS was made according to Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) criteria. Imaging and lumbar puncture were deferred as the initial reports were suggestive of NMS.
Table 1.
Laboratory abnormalities in our patient
Risperidone was stopped immediately, and he was treated with lorazepam, trihexyphenidyl, paracetamol, and intravenous fluids in consultation with psychiatrist. Within 48 h of hospitalization, his symptoms improved and CPK level gradually came down. The patient was afebrile on the 3rd day and his glycemic control improved. Family was informed of the diagnosis and the need for close monitoring of his glycemic control. Psychiatrists decided not to restart antipsychotic drugs. His behavioral abnormalities were to be managed with counseling sessions. He was discharged without further complications.
Discussion
NMS is a rare condition as reported in the two studies done in neurology and psychiatric units of teaching hospitals in India with an incidence of 1.40–1.41/1000 cases treated with antipsychotics.[2,3] Among the risk factors, some studies report older age as high-risk due to the associated medical morbidities, nutritional deficiencies, dehydration and electrolyte abnormalities, male gender, and genetic predisposition.[4] Other studies report more cases in the age group of 20–50 years associated with high antipsychotic dosage as seen in our patient.[5]
The antidopaminergic activity of antipsychotic drugs is associated with the symptoms of muscle rigidity, hyperthermia, autonomic dysfunction, and mental status change. These symptoms are recognized as diagnostic according to the American Psychiatric Associations’ DSM-IV.[6] The signs and symptoms develop during a 24–72 h period following the administration of antipsychotic drug; however, it can develop later as seen in our patient. Newer antipsychotic agents such as risperidone block serotonin receptors more than dopamine receptors; however, NMS has been reported with their use as in our case study. Anti-emetics such as metoclopramide and droperidol have been linked to NMS by their dopaminergic blocking activity.
No single laboratory test result is diagnostic. Laboratory abnormalities may include leukocytosis, electrolyte disturbances, and elevated CPK secondary to muscle damage. Diagnostic tests for fever may include urine analysis, chest radiography, and lumbar puncture. Imaging studies of brain are not diagnostic of NMS, however, may rule out other causes of altered mental status. Possible complications include dehydration from poor oral intake, renal failure secondary to rhabdomyolysis, and coagulation abnormalities. Mortality in NMS has decreased from 76% to between 10% and 20%, however, complete recovery is noted in most patients.[7] Mortality is caused by complications such as respiratory failure, cardiovascular collapse, renal failure, arrhythmias, and thromboembolism.
Treatment depends on the severity of symptoms. Patients who are hemodynamically unstable are to be transferred to higher centers for intensive monitoring. Mild cases can be managed at the secondary care setting in consultation with a psychiatrist. Supportive therapy involves discontinuation of antipsychotic agents, correction of electrolyte imbalances, nutritional deficiencies and monitoring of airway, breathing, and circulation. Our patient was managed at the urban health center by the team of family physicians. Specific dopaminergic agents such as bromocriptine, dantrolene, and electroconvulsive therapy as an option are considered for more severe cases by psychiatrists. Iron deficiency should be corrected as low iron levels may aggravate movement disorders.[8]
Complete resolution of symptoms takes around 2 days to 2 weeks. Symptoms may last for a month in patients who were on depot preparations. Restarting antipsychotics in patients with history of NMS if needed is done on consultation with psychiatrist. Depot preparations are generally not recommended, however, a 2 weeks interval is to be considered between recovery and restarting antipsychotic agents.[9] No complications with anesthesia have been reported in post-NMS patients.
Early detection and management of side effects caused by neuroleptic agents are of particular consideration to family physicians who attend to the early symptoms. Decreasing risk factors that aggravate rigidity include avoiding dehydration, minimal use of restraints and intramuscular injections, adequate nutrition, screening for history of NMS in the patient, or other family members.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We gratefully acknowledge Dr. Dheeraj Kuttala, Assistant Professor, Department of Psychiatry, Christian Medical College, Vellore, for his support in the management of our patient.
References
- 1.Delay J, Pichot P, Lemperiere T, Elissalde B, Peigne F. A non-phenothiazine and non-reserpine major neuroleptic, haloperidol, in the treatment of psychoses. Ann Med Psychol (Paris) 1960;118:145–52. [PubMed] [Google Scholar]
- 2.Chopra MP, Prakash SS, Raguram R. The neuroleptic malignant syndrome: An Indian experience. Compr Psychiatry. 1999;40:19–23. doi: 10.1016/s0010-440x(99)90071-8. [DOI] [PubMed] [Google Scholar]
- 3.Panagariya A, Sharma B, Singh R, Agarwal V, Dev A. The neuroleptic malignant syndrome: A report of 14 cases from North India. Neurol India. 2007;55:166–8. doi: 10.4103/0028-3886.32793. [DOI] [PubMed] [Google Scholar]
- 4.Waldorf S. AANA journal course. Update for nurse anesthetists. Neuroleptic malignant syndrome. AANA J. 2003;71:389–94. [PubMed] [Google Scholar]
- 5.Gupta S, Nihalani ND. Neuroleptic Malignant Syndrome: A Primary Care Perspective. Prim Care Companion J Clin Psychiatry. 2004;6:191–194. doi: 10.4088/pcc.v06n0502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Association; 1994. American Psychiatric Association. [Google Scholar]
- 7.Shalev A, Hermesh H, Munitz H. Mortality from neuroleptic malignant syndrome. J Clin Psychiatry. 1989;50:18–25. [PubMed] [Google Scholar]
- 8.Gold R, Lenox RH. Is there a rationale for iron supplementation in the treatment of akathisia? A review of the evidence. J Clin Psychiatry. 1995;56:476–83. [PubMed] [Google Scholar]
- 9.Pope HG, Jr, Aizley HG, Keck PE, Jr, McElroy SL. Neuroleptic malignant syndrome: Long-term follow-up of 20 cases. J Clin Psychiatry. 1991;52:208–12. [PubMed] [Google Scholar]


