Abstract
Background:
Deliberate self-harm (DSH) is a major under-recognized epidemic in the low- and middle-income countries. This is a large retrospective study form the Emergency Department (ED) of Tertiary Care Center of South India to describe the clinicodemographic features of DSH cases.
Materials and Methods:
This is a retrospective study conducted at ED of Christian Medical College, Vellore, India from January 01, 2011 to December 31, 2013. All cases of DSH were included in the study. The demographic details, mode of DSH and clinical outcome were extracted from the electronic medical record. Descriptive statistics are presented. Chi-square test was used to compare categorical variables. For all tests, a two-sided P ≤ 0.05 was considered statistically significant.
Results:
Total of 1228 patients were admitted to ED for DSH during the study period. Male and female occurred in equal ratio. More than half of the cases occurred among age group below 30 years. Consumption of pesticides (agricultural chemicals) was the single most common mode of DSH (46%), especially among men, followed by medication overdose (29.8%). Consumption of plant poison and tablet overdose was higher among women. Overall mortality due to DSH was low (1.5%) in our study.
Conclusion:
DSH is under-recognized major public health problem in low-middle income countries like India. Most cases occur among young and productive age group and in equal frequencies among men and women. Timely and the appropriate institution of treatment can decrease the morbidity and mortality due to DSH remarkably.
Keywords: Deliberate self-harm, Emergency Department, profile, suicide
Introduction
Deliberate self-harm (DSH) is one of the commonest cause of death in the world with a higher rate noted in the low- and middle-income countries.[1] Soman et al. from South India reported that DSH was responsible for 6.6% of all deaths.[2] The average age was 42 years for males and 34 years for females and half of all suicides occurred in the age group of 15–44 years.[2] Nojomi et al. from Iran reported that women had frequent DSH attempts and the mean age was 24.5 (±9) years.[3] DSH attempts are one of the commonest reasons for Emergency Department (ED) admissions.[4] Self-poisoning was the most common method used for DSH in a study done across eight low- and middle-income countries.[5] Suicide attempts were common among those from low socioeconomic status, and the common modes were self-poisoning with organophosphorus compounds and overdosage of tablets.[6] The suicide rate was high among the elderly according to a study done in South India, and the common modes were hanging and organo-phosphorous poisoning.[7] Insecticide poisoning and self-immolation were associated with high mortality rate in India while in a South American country hanging and jumping from heights had a bad outcome.[8,9,10] A wide variety of poisons like insecticides, pesticides, plant poisons, rodenticides is freely available across the country. Even drugs such as benzodiazepines, barbiturates, and antidepressants are easily accessible. There is a wide variation in the method of DSH used across different states of India and varies with the socioeconomic status. This study was done to describe the profile of DSH attempts and outcome of patients presenting to the adult ED of our tertiary care hospital in South India.
Materials and Methods
This is a retrospective study, of patients, presenting with DSH to the adult ED of Christian Medical College, Vellore, which is a 45-bed department in South India with an average of 200 admissions daily. All patients more than 15 years old presenting with a history of alleged DSH from January 01, 2011 to December 31, 2013, were included in the study. The patients were identified using the triage register of the ED. A retrospective chart review was performed on all the above said patients using the hospital's electronic medical database. The following were extracted: Demographics, age, sex, date of admission, type of DSH used, discharge status, and duration of admission.
Statistical analysis was performed using SPSS for Windows, Version 16.0. Chicago, SPSS Inc. Released 2007. Mean (standard deviation) were calculated for the continuous variables. The categorical variables were expressed in proportion and Chi-square test or Fisher exact test was used to compare dichotomous variables. For all tests, a two-sided P < 0.05 was considered statistically significant.
This study was approved by the Institutional Review Board, and patient confidentiality was maintained using unique identifiers and by password protected data entry software with restricted users.
Results
During the study period of 3 years, the ED attended to 130,164 patients. Eighty-seven percent of those were medical/surgical emergencies, and 13% were trauma related cases. The prevalence of patients presenting with DSH was 1.08% (1228/1,13,243) [Figure 1]. There was a slight female predominance (51.8%) which was consistent over the study period of 3 years [Table 1]. The mean age of the patients was 20 (±11) years. Majority of the patients (82.7%) were <40 years old. Almost half of the patients (48.1%) were in the age group between 20 and 29 years of age. Elderly population (≥60 years) constituted 3.5% of the study population [Table 1]. The month-wise distribution of DSH cases over a 3-year period is shown in Figure 2. The time of DSH admissions were as follows, 37.1% (456/1228) were at nights (2100–0500 h, the following day), 29% (356/1228) were at afternoons (1200–1700 h), 18.9% (232/1228) at evenings (1700–2100 h), and 15% (184/1228) during morning hours (0500–1700 h).
Figure 1.
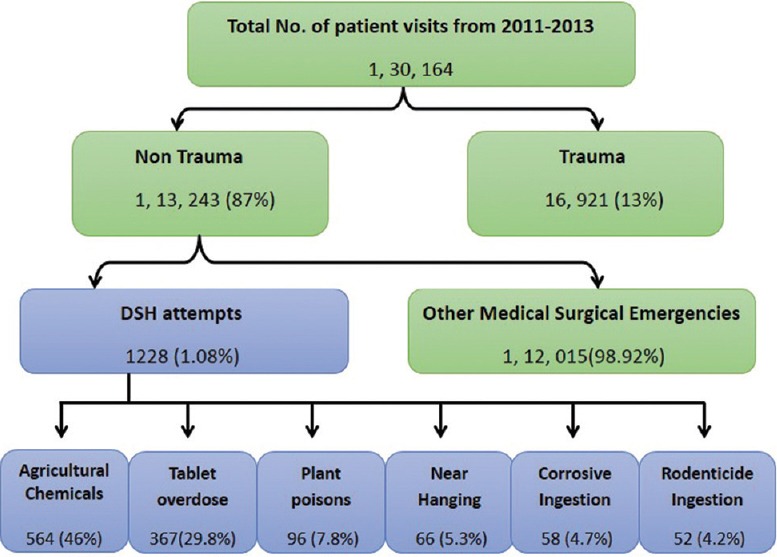
Patient flow in emergency department with classification of DSH
Table 1.
Baseline characteristics
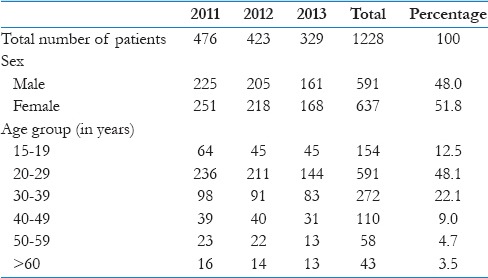
Figure 2.
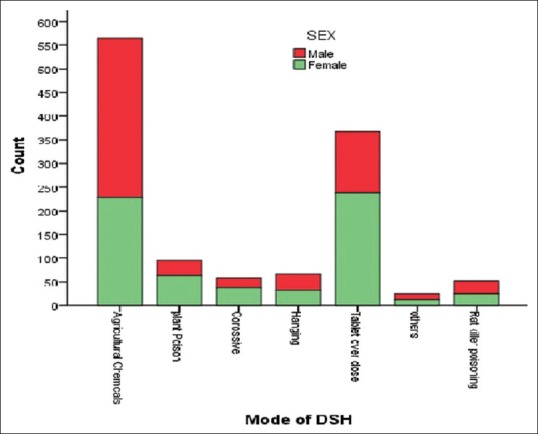
Mode of Deliberate Self-Harm among men and women
Consumption of pesticide chemicals (agricultural chemicals) (46%) was the most common mode of DSH followed by tablet overdosing (29.8%). Consumption of plant poisons (7.8%), near hanging (5.3%), corrosive chemical ingestion (4.7%), and ingestion of rodenticides (4.2%) were the other common modalities of DSH. Two wild plants of our locality which were consumed for DSH were oleander (52/96) and oduvanthalai (42/96). The other plants that were used for DSH were henna and eucalyptus with one case each of the leaves being consumed. Rare modes of DSH (2%) were hydrocarbon ingestion (12), hair dye ingestion (5), self-infliction with sharp objects (4), ingestion crushed glass pieces (2), burns (1), and ingestion of copper oxychloride (1) [Table 2]. The method of DSH more preferred by women were plant poisons (66.3% vs. 33.7%, P = 0.006), corrosives (63.8% vs. 36.2%, P = 0.047) and tablet overdose (64.9% vs. 34.1%, P = 0.001) while agricultural chemicals were more likely to be consumed by men (59.5% vs. 40.5%, P = 0.001) for DSH. The preferred mode of DSH by the males and females is shown in Figure 3.
Table 2.
Mode of deliberate self-harm
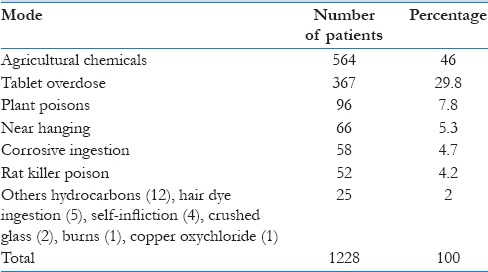
Figure 3.
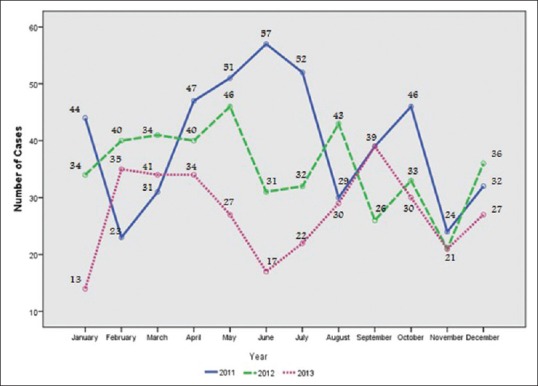
Month wise distribution of the number of patients with DSH for 3 years
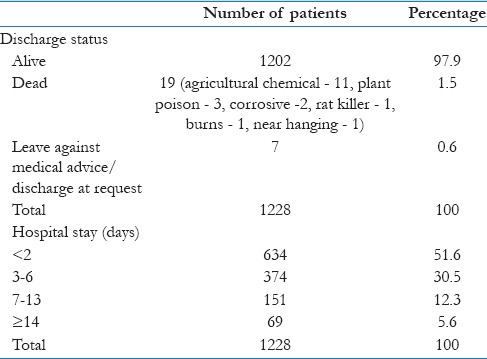
The outcome was studied by the condition at discharge from hospital and the number of days in hospital. Majority (97.9%) of the patients were discharged alive from the hospital while 19 (1.5%) died in the hospital. The discharge status of 7 patients was mentioned as either left against medical advice or discharged at request. The length of hospital stay was ≤2 days among 634 (51.6%) patients, between 3 and 6 days among 374 (30.5%), between 7 and 13 days among 151 (12.3%) and 2 weeks or more in 69 (5.6%) patients, respectively [Table 3].
Table 3.
Outcome of patients
Discussion
The objective of this study was to describe the demographic features, mode of DSH and outcome of patients presenting with DSH to a tertiary care hospital in South India. Nearly, 1% of our admission in the ED is related to DSH. In our study, the male: Female ratio was 0.93 with a slight female predominance (51.8%), while a study done in a low socioeconomic country reported a male to female suicide ratio of 1.7.[2] A study conducted in a middle-income country showed that women had frequent DSH attempts than men.[3] A similar study revealed the average age was 42 years for males and 34 years for females with half of all suicides occurring in the age group of 15–44 years.[2] The average age commonly resorting to DSH was 24.5 (±9) years as reported by Nojomi et al.[3] In our study, DSH was common among the young with 82.7% patients being <40 years of age. Almost half of the patients (48.1%) were in the age group between 20 and 29 years of age. It was found that 12.5% of DSH attempts were committed by teenage individuals. DSH attempts affect the younger population in their more productive years of life. Patients ≥60 years constituted 3.5% of the DSH attempts reported, and DSH was not uncommon among the elderly.[7]
DSH attempts usually present to the ED and self-poisonings were the common mode of DSH according to a study done in eight low- and middle-income countries.[4,5] In this study on an average, at least, one DSH presented to ED every day. Self-poisoning was the most common method of DSH, and agricultural chemicals (46%) were commonly used to commit DSH. Overdosing with tablets (29.8%) was the second most common method used. Other studies from India also reported insecticide poisoning and tablet overdosage as the frequent modes of DSH.[6,8] The other modes of DSH reported were near hanging, self-immolation, jumping from heights, self-infliction, inhalation of automobile gases, etc.[6,8,9,10] The less frequently reported modes of DSH in this study were consumption of plant poisons (7.8%), near hanging (5.3%), corrosive chemical ingestion (4.7%), and ingestion of rat killer poisons (4.2%). Multiple modes of DSH were observed in 3 patients, one patient presented with near hanging after consuming insecticide poison, the second patient consumed a combination of kerosene, insecticide and paint and the third patient consumed zinc phosphide along with paracetamol tablets. Since the hospital in which the study was done has a separate triage and resuscitation policy for burns, exact numbers could not be presented.
Bose et al. study on suicides in the same geographical area reported a total mortality rate of 82.2/100000 population. As the age group affected was from 15 to 40 years the total years of life lost was also high (26.9 years).[9] However, in this study, of the total 1228 patients with attempted DSH 1202 (97.9%) patients were discharged alive from the hospital, while 19 (1.5%) died in the hospital. This reflects that though suicide attempts posed a high risk for death, hospitalization and aggressive treatment can positively affect the outcome. On further analysis, it was found that of the adult DSH attempts 51.6% were discharged from hospital by 2 days. The length of hospital stay was between 3 and 6 days for 30.5% of patients, between 7 and 13 days for 12.3% and 2 weeks or more 5.6% of the study population.
Psychiatric illness such as depression and personality disorders were found in majority of first attempters of DSH.[11] Alcohol abuse, ethnicity, low income, marital discord, loss of job, and change in weather conditions were also associated with DSH.[12,13,14,15] All patients with DSH attempt should receive a psychiatric evaluation and follow-up should be arranged with a general practitioner or a psychiatrist. Preventive health activities such as psychiatric screening and follow-up, socioeconomic upliftment, counseling regarding difficult times in life such as loss of job, marital discord, and alcohol abuse will result in decreased DSH attempts. Banning and restricting the use of fatal agricultural chemicals will reduce the morbidity and mortality associated with DSH in low socioeconomic countries. Hazard classification of agricultural chemicals should also include their DSH potential and warnings issued accordingly.
Conclusion
ED doctors should be geared to handle a variety of DSH attempts. Hospital care of DSH attempts can positively influence their outcome. Since still a large number of DSH attempts are with agricultural chemicals, political will, and legal changes regarding the sale of poisonous chemicals can indirectly lead to a decrease in mortality and morbidity associated with DSH attempts.
Limitations
The retrospective nature of this study did not provide information into the risk factors and co-morbid conditions associated with DSH. The lack of follow-up information is another limitation to the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.WHO | Suicide Data. WHO. [Last cited on 2015 Oct 06]. Available from: http://www.who.int/mental_health/prevention/suicide/suicideprevent/en/
- 2.Soman CR, Shahulhameed S, Ramankutty V, Vijayakumar K, Kunjukrishnapillai R, Ajayan K, et al. Cohort profile: The PROLIFE study in Kerala, India. Int J Epidemiol. 2011;40:10–4. doi: 10.1093/ije/dyp275. [DOI] [PubMed] [Google Scholar]
- 3.Nojomi M, Malakouti SK, Bolhari J, Hakimshooshtari M, Fleischmann A, Bertolote JM. Epidemiology of suicide attempters resorting to emergency departments in Karaj, Iran, 2003. Eur J Emerg Med. 2008;15:221–3. doi: 10.1097/MEJ.0b013e3282f4d12a. [DOI] [PubMed] [Google Scholar]
- 4.Hazlett SB, McCarthy ML, Londner MS, Onyike CU. Epidemiology of adult psychiatric visits to US emergency departments. Acad Emerg Med. 2004;11:193–5. [PubMed] [Google Scholar]
- 5.Fleischmann A, Bertolote JM, De Leo D, Botega N, Phillips M, Sisask M, et al. Characteristics of attempted suicides seen in emergency-care settings of general hospitals in eight low- and middle-income countries. Psychol Med. 2005;35:1467–74. doi: 10.1017/S0033291705005416. [DOI] [PubMed] [Google Scholar]
- 6.Nagendra Gouda M, Rao SM. Factors related to attempted suicide in davanagere. Indian J Community Med. 2008;33:15–8. doi: 10.4103/0970-0218.39237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Abraham VJ, Abraham S, Jacob KS. Suicide in the elderly in Kaniyambadi block, Tamil Nadu, South India. Int J Geriatr Psychiatry. 2005;20:953–5. doi: 10.1002/gps.1385. [DOI] [PubMed] [Google Scholar]
- 8.Saddichha S, Prasad MN, Saxena MK. Attempted suicides in India: A comprehensive look. Arch Suicide Res. 2010;14:56–65. doi: 10.1080/13811110903479060. [DOI] [PubMed] [Google Scholar]
- 9.Bose A, Konradsen F, John J, Suganthy P, Muliyil J, Abraham S. Mortality rate and years of life lost from unintentional injury and suicide in South India. Trop Med Int Health. 2006;11:1553–6. doi: 10.1111/j.1365-3156.2006.01707.x. [DOI] [PubMed] [Google Scholar]
- 10.Jørs E, Christoffersen M, Veirum NH, Aquilar GC, Morant RC, Konradsen F. Suicide attempts and suicides in Bolivia from 2007 to 2012: Pesticides are the preferred method - females try but males commit suicide! Int J Adolesc Med Health. 2014;26:361–7. doi: 10.1515/ijamh-2013-0309. [DOI] [PubMed] [Google Scholar]
- 11.Kulkarni RR, Rao KN, Begum S. Comorbidity of psychiatric and personality disorders in first suicide attempters: A case-control study. Asian J Psychiatr. 2013;6:410–6. doi: 10.1016/j.ajp.2013.05.004. [DOI] [PubMed] [Google Scholar]
- 12.Haw C, Hawton K, Casey D, Bale E, Shepherd A. Alcohol dependence, excessive drinking and deliberate self-harm: Trends and patterns in Oxford, 1989-2002. Soc Psychiatry Psychiatr Epidemiol. 2005;40:964–71. doi: 10.1007/s00127-005-0981-3. [DOI] [PubMed] [Google Scholar]
- 13.Hawton K, Harriss L, Hodder K, Simkin S, Gunnell D. The influence of the economic and social environment on deliberate self-harm and suicide: An ecological and person-based study. Psychol Med. 2001;31:827–36. doi: 10.1017/s0033291701003993. [DOI] [PubMed] [Google Scholar]
- 14.Hutchinson G. Variation of homicidal and suicidal behaviour within Trinidad and Tobago and the associated ecological risk factors. West Indian Med J. 2005;54:319–24. doi: 10.1590/s0043-31442005000500009. [DOI] [PubMed] [Google Scholar]
- 15.Töro K, Dunay G, Bartholy J, Pongrácz R, Kis Z, Keller E. Relationship between suicidal cases and meteorological conditions. J Forensic Leg Med. 2009;16:277–9. doi: 10.1016/j.jflm.2008.12.015. [DOI] [PubMed] [Google Scholar]


