Abstract
Background:
Iodine deficiency is the world's single greatest cause of preventable mental retardation. In developing countries, only 69% of households are consuming iodized salt.
Objective:
To assess knowledge and practices with respect to the current use of iodized salt, and to estimate its uptake at the household level.
Materials and Methods:
This cross-sectional survey was conducted in six villages under Rural Health Training Center. A total number of households surveyed were 253. The data collectors obtained verbal consent from the Family, and Pretested Standardized Questionnaire was administered in every selected household. The respondents were asked questions regarding salt purchasing and consumption habits, salt storage, awareness of iodized salt, and iodine deficiency diseases. Rapid iodized salt test kit (MBI kit) was used in the survey to assess iodine content in salt used in households.
Results:
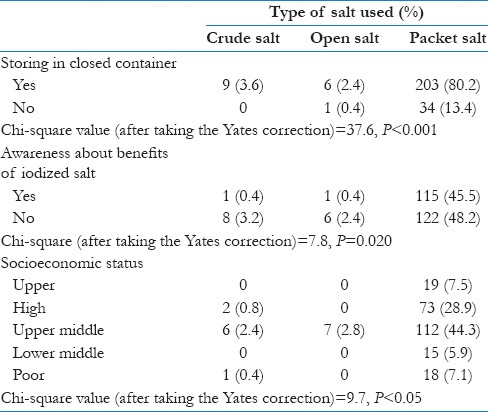
In this study, 93.7% households were using packet salt. The most common source of information was a television (31.1%). More than half (53.8%) of the households were unaware of the benefits of iodine. About 62.5% of households were consuming adequately iodized salt. Significant association was found between the practice of storing salt in closed containers and use of packaged iodized salt (Chi-square value −37.6, P < 0.001), awareness about the benefits of iodine and type of salt used (P = 0.02) while no association was observed between the socioeconomic status and type of salt used in the household.
Conclusions:
Though the use of packet salt was more than 90%, adequately iodized salt was consumed only in 62.5%, and more than half of the subjects lacked the knowledge about iodine deficiency diseases.
Keywords: Field, household, implication, iodized salt, policy makers, rural
Introduction
Iodine deficiency is the world's single greatest cause of preventable mental retardation. It is especially damaging during the early stages of pregnancy and in early childhood.[1] Iodine is an essential component of thyroid hormones, which are needed for optimal mental and physical development and regulation of body metabolism (generation and utilization of body energy). Iodine deficiency disorder (IDD) has been recognized as a public health problem in India. An estimated 167 million people in India are at risk of IDDs. Of these, 54 million suffer from goiter, 2 million suffer from cretinism, and 6.6 million children have neurological deficits.[2] Surveys conducted in various states showed that no state in the country is free from IDD.[3]
Globally, IDDs are associated with many thyroid related diseases including hypothyroidism, hyperthyroidism, goiter and cretinism, and also inherit real risk of coronary artery diseases, autoimmune disorders, psychiatric disorders, cognitive impairment, and cancer.[4,5,6] Salt iodization programs have been implemented in many countries of the world, and two-thirds of the global population (71%) is estimated to be covered by iodized salt.[7] About 31% (1900.9 million) of the world population is estimated to have insufficient iodine intakes, with the most affected the WHO regions being South-East Asia and Europe.
In India, the entire population is prone to IDD due to deficiency of iodine in the soil of the subcontinent and consequently the food derived from it. Of these, an estimated 350 million people are at risk of IDD as they consume salt with inadequate iodine.[8] Though universal salt iodization (USI) was made mandatory in the country from 2005, only 71% of households were consuming adequately iodized salt as per the Coverage Evaluation Survey, 2009.[9] This gap in the utilization of adequately iodized salt could be due to various reasons such as nonavailability in the rural areas, poverty, poor knowledge of iodine deficiency diseases, and faulty storage practices.
Since no such evaluation was recently done in our catered area, this study was conducted to evaluate the various factors related with iodized salt consumption in a rural area of Gautambudh Nagar District of Uttar Pradesh. The main hypothesis of this study was that to assess about the usage of iodized salt in the selected population. The aim of the present survey was to assess the knowledge related to health benefits of iodine and practices with respect to storage and use of iodized salt, as well as to estimate the uptake of iodized salt at the household level.
Objectives
To assess knowledge regarding benefits of iodized salt use, iodine deficiency diseases and practices with respect to the current use of iodized salt
To find the percentage of adequately iodized salt users in the rural population of District Gautam Budh Nagar.
Materials and Methods
This was a cross-sectional survey conducted in the villages of Gautam Budh Nagar, catered by Rural Health Training Center under the Department of Community Medicine, SMSR. One-fifth of the total numbers of households in the area was interviewed for the purpose of the study. Ethical clearance was obtained from the Ethical Committee of School of Medical Sciences and Research, Sharda University.
The stratified random sampling method was used to select the households applying population proportionate to size technique. Every fifth household was interviewed until the required sample from that particular village was achieved. The total numbers of households in the area were 1255 and using the above methodology the number of households covered was 253. A structured Knowledge and Practices Questionnaire was administered to the head of the household and household salt was tested for estimating the level of iodine in salt. If the head of that household was not available, the next senior-most member available was interviewed.
Total 253 households were included in the study. Before doing the data collection, the survey team consisting of health workers and interns was given training regarding the testing for estimation of iodine in salt with the help of MBI kits and administration of the questionnaire. The data collectors obtained verbal consent from the Family and Pretested Standardized Questionnaire was administered in every selected household, and the respondents were asked questions regarding salt purchasing and consumption habits, benefits of Iodine, and iodized salt awareness, etc.
Rapid iodized salt test kit (MBI kit) was used to assess iodine content in salt consumed in the household. The kit contained stabilized starch-based solution, which causes chemical reaction manifested by color change. The salt sample was taken in a teaspoon, and after shaking the reagent (test solution) bottle well, a drop of the test solution was poured on the salt. The salt turned light blue to dark violet depending on the iodine content of the salt. To assess the iodine content, the color of the salt was compared with accompanying chart (0, 7, 15, and 30 parts/million [ppm]). The cut-off proportion of 15 ppm and above was considered as adequately iodized salt using the WHO/United Nations International Children's Emergency Fund reference indicators for monitoring of iodized salt. The data were entered on spread sheet and analyzed with help of Microsoft excel. Descriptive analysis and Chi-square test were used to present the data. If the P value in Chi-square test was found <0.05 then the association was considered as significant.
Results and Observation
Most of the households belonged to high (30%) and upper middle class (49%) according to modified BG Prasad classification as shown in Figure 1.[11]
Figure 1.
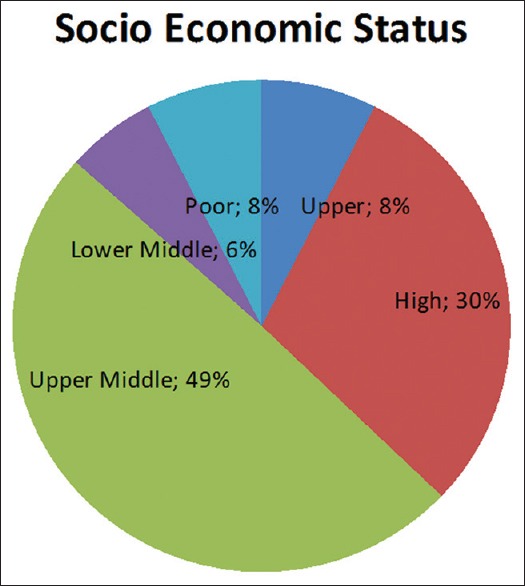
Distribution of population according to socioeconomic status of household units of District Gautam Budh Nagar
Among the 253 households surveyed for the study, 93.7% households were using packet salt. Rest of the households was using either open salt (2.8%) or crude salt (3.6%). The reasons of not using the packet salt were mainly disliking the taste (50%), the nonavailability of the packet iodized salt (33.3%), and compulsion to buy atleast 1 kg packet at a time (16.7%). Of the 253 respondents, only 71.1% had heard about iodized salt. The most common source of information regarding the iodized salt was television (31.1%), followed by radio (30%). Around 14% household came to know about iodized salt from the health workers as shown in Figure 2.
Figure 2.
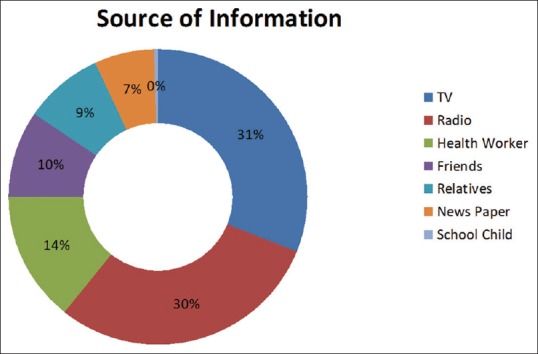
Sources of information regarding iodized salt among rural people of District Gautam Budh Nagar
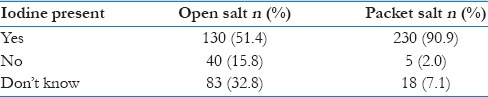
Majority of the respondents (90.9%) knew that packet salt contains iodine. However, almost half of the respondents (51.4%) were wrongly aware of the presence of iodine in open salt [as shown in Table 1].
Table 1.
Knowledge about iodine content in salt among rural people of District Gautam Budh Nagar
More than half of the households (53.8%) were unaware about the benefits of iodine. Out of the rest 46.2% of the households, who were aware about the benefits of iodine, 54.1% knew about its role in the cure of goiter, for growth and development (15.4%), and 15% believed that it was important for remaining healthy. More than 90% of the respondents knew that the iodine content of the salt reduces if the salt is kept in an open container and 87% stored the salt in closed containers.
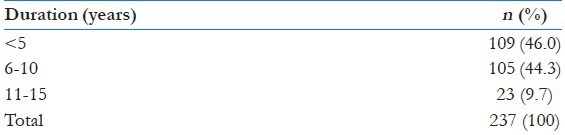
137 households (54%) were using iodized salt for 5 or more years and the rest were using it for <5 years [Table 2].
Table 2.
Duration of use of iodized salt among rural people of District Gautam Budh Nagar
One hundred fifty-eight households (62.4%) were using adequately iodized salt (iodine content >15 ppm) while 26.1% and 11.5% were using inadequately iodized because of improper storage and non-iodized salt, respectively [Figure 4].
Figure 4.
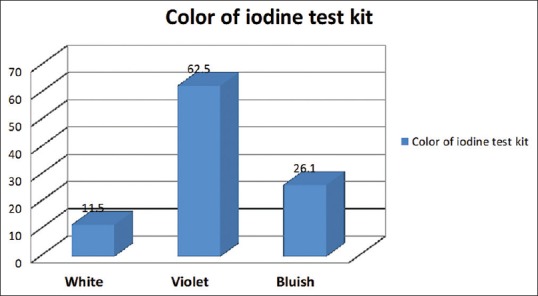
Iodine test kit results for the salt samples tested among rural people of District Gautam Budh Nagar
Figure 3.
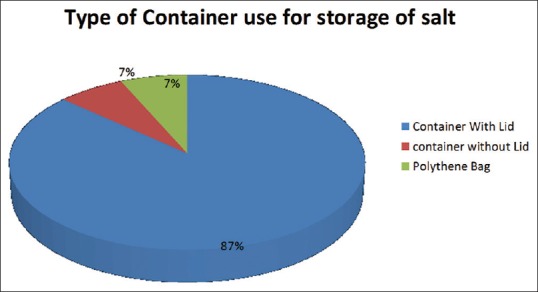
Type of container used for storage of salt among rural people of District Gautam Budh Nagar
The type of salt used was significantly affected by the knowledge about the benefits of iodine (Chi-square = 7.8, P = 0.02). The association between practice of utilization of iodized salt and the socioeconomic status of the family/household was statistically significant (Chi-square = 9.7, P = 0.05). Correct storage practices for the household salt were significantly related with the type of salt being used (Chi-square = 37.6, P < 0.001) [as shown in Table 3].
Table 3.
Effect of different variables on the type of salt used among rural people of District Gautam Budh Nagar
Discussion
The Government of India established the National Goitre Control Programme (NGCP) in 1962 at the end of the second 5-year plan. The objectives of NGCP were to identify the goiter endemic regions of the country and supplement the intake of iodine to the entire population in these regions. The NGCP primarily focused on the so called “goiter belt” in the country which comprised the Himalayan and Tarai region in the North and North-Eastern parts of India.[12] The nomenclature of the NGCP was changed to National IDD Control Programme (NIDDCP) in 1992 to emphasize the wider implications of iodine deficiency. The identified objectives of the NIDDCP were to conduct surveys to assess the magnitude of the IDD, supply of iodated salt in place of common salt, resurvey after every 5 years to assess the extent of IDD and the impact of iodated salt, laboratory monitoring of iodized salt and urinary iodine excretion and health education and advocacy.[13] The NIDDCP identifies USI as the primary strategy to eliminate IDD as a public health problem in the country.
This study was therefore undertaken to assess the utilization of iodized salt in the rural communities to monitor the progress of NIDDCP. The limitation of this study is sample size as only 20% household was covered under this study. Another limitation, in some household though practice of storing was not proper but because of open of new packet during data collection, test give higher level of iodine.
This study revealed that 93.7% households were using packet salt. Rest of the households was using either open salt (2.8%) or crude salt (3.6%). The reasons for not using the packet salt were non availability (33.3%), or dislike for the taste (50%), or compulsion to buy 1 kg packet at a time (16.7%). Almost similar findings were obtained by the Coverage Evaluation Survey, 2009.[9] According to it, 91% population was using iodized salt. Another study done by Agarwal et al.[14] also revealed 91% population coverage of iodized salt among slum households of North-East Delhi. Reasons for non-utilization as reported by Agarwal et al.[14] included “low cost,” “since it tasted better” and “feeling it is pure and uncontaminated unlike refined salt.” However, in a study done by Manish Chaturvedi et al.[15] in the District of Agra in 2005, only 40.8% rural households were using packed salt.
The common sources of information for iodized salt were television (31.1%), followed by radio (30%). However, in a study by Sen et al.,[2] television (66.7%) was the principal source of information. Our study revealed that 54.1% of the study population knew about the role of iodine in cure of goiter, while in the studies done by Strange et al.[16] and Sen's study[2] 62% and 60% of the people surveyed, respectively knew that iodine deficiency results in goiter.
In this study, 62.5% household were using adequately iodized salt that is almost similar to that revealed by the Coverage Evaluation Survey, 2009 (66.1%),[9] but less than the findings of Agarwal et al.[14] (75.7%), Yadav et al.[17] (71.1%), and Sen et al.[2] (72.9%). However, Chaturvedi et al.[15] in their study found that only 9.8% of rural households of Agra were consuming adequately iodized salt.
Our study did not find any significant association between socioeconomic status of the study population and type of salt used but Sen et al.[2] found the same significant.
Conclusions and Recommendations
Less than two-third of the rural households were consuming adequately iodized salt. Even among those households consuming refined salt, nearly one-fourth households were not consuming adequately iodized salt. The level of awareness regarding the benefits of consuming iodized salt among the studied population was <50%. Fourteen percent of the rural households gained knowledge about the benefits of iodine through the health workers.
Role of health workers in disseminating the knowledge regarding the benefits of using iodized salt cannot be undermined as evident from the study. Despite NIDDCP being in place for more than 20 years, the consumption of adequately iodized salt in rural areas is still less than the goal of the program and there is a big gap between the awareness of the benefits of iodized salt and its consumption per se. This can only be improved by active participation of our grass root level workers in generating awareness about the health benefits of consuming adequately iodized salt.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The authors gratefully acknowledge MBI International, for providing the authors MBI kit for the study and the field workers of the Rural Health Training Center (RHTC), Panchayatan, working in the study areas, for their contribution in conducting the survey.
References
- 1.United Nations Children's Fund. Sustainable Elimination of Iodine Deficiency, Progress since the 1990 World Summit for Children; May. 2008. [Last accessed on 2015 Sep 27]. Available from: http://www.unicef.org/iran/Sustainable_Elimination_of_iodine_Deficiency_053008%281%29.pdf .
- 2.Sen TK, Das DK, Biswas AB, Chakrabarty I, Mukhopadhyay S, Roy R. Limited access to iodized salt among the poor and disadvantaged in North 24 Parganas district of West Bengal, India. J Health Popul Nutr. 2010;28:369–74. doi: 10.3329/jhpn.v28i4.6043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kamath R, Bhat V, Rao R, Das A, Ks G, Kamath A. Prevalence of goiter in rural area of Belgaum district, Karnataka. Indian J Community Med. 2009;34:48–51. doi: 10.4103/0970-0218.45373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Patrick L. Iodine: Deficiency and therapeutic considerations. Altern Med Rev. 2008;13:116–27. [PubMed] [Google Scholar]
- 5.Verheesen RH, Schweitzer CM. Iodine deficiency, more than cretinism and goiter. Med Hypotheses. 2008;71:645–8. doi: 10.1016/j.mehy.2008.06.020. [DOI] [PubMed] [Google Scholar]
- 6.Simone Caramel. Coronary Artery Disease and CAD Inherited Real Risk. 2010. [Last accessed on 2015 Aug 11]. Available from: http://www.sisbq.org/uploads/5/6/8/7/5687930/cad_caramel.pdf .
- 7.UNICEF. The State of the World's Children. Adolescence: An Age of Opportunity. New York: United Nations Children's Fund; 2011. [Google Scholar]
- 8.Pandav CS, Yadav K, Srivastava R, Pandav R, Karmarkar MG. Iodine deficiency disorders (IDD) control in India. Indian J Med Res. 2013;138:418–33. [PMC free article] [PubMed] [Google Scholar]
- 9.UNICEF. Coverage Evaluation Survey 2009, All India Report. Ministry of Health and Family Welfare, Government of India, New Delhi. 2010. [Last accessed on 2015 Sep 27]. Available from: http://www.unicef.org/india/health.html .
- 10.National Urban Health Mission. District Action Plan-Gautam Budha Nagar, Uttar Pradesh. 2013-14:8. [Google Scholar]
- 11.Reddy SD, Reddy KA, Prabhu GR. Prasad's socio-economic status classification - An update for 2014. Int J Res Health Sci. 2014;2:875–8. [Google Scholar]
- 12.Pandav CS, Kochupillai N, Karmarkar MG, Nath LM. Iodine deficiency disorders in India: Review of control measures. Indian Pediatr. 1986;23:325–9. [PubMed] [Google Scholar]
- 13.Directorate General of Health Services (DGHS). Policy Guidelines on National Iodine Deficiency Disorders Control Programme. New Delhi: DGHS, Ministry of Health and Family Welfare, Government of India; 2003. pp. 1–10. [Google Scholar]
- 14.Agarwal S, Sethi V, Sharma D, Vaid M, Agnihotri A, Sindhwani A, et al. Consumption of iodized salt among slum households of north-East Delhi, India. Indian J Community Med. 2009;34:368–9. doi: 10.4103/0970-0218.58406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chaturvedi M, Gupta SC, Nandan D. Status of consumption of iodized salt in Agra District. Indian J Community Health. 2006;18:30–3. [Google Scholar]
- 16.Strange B, Joseph M, Kaushik S, Dey S, Dutt S, Jha RK. Reaching the Rural Poor in India with Iodized Salt: The Micronutrient Initiative's Iodized Salt Coverage Study 2010. International Council for Control of Iodine Deficiency Disorders Newsletter. 2011 May;39 [Google Scholar]
- 17.Yadav K, Pandav CS, Karmarkar MG. Vol. 39. International Council for Control of Iodine Deficiency Disorders Newsletter: 2011. May, Adequately Iodized Salt Covered Seventy-One Percent of India in 2009. [Google Scholar]


