Abstract
Background
Traditional Chinese exercise (TCE) has widespread use for the prevention and treatment of cardiovascular disease; however, there appears to be no consensus about the benefits of TCE for patients with cardiovascular disease. The objective of this systematic review was to determine the effects of TCE for patients with cardiovascular disease.
Methods and Results
Relevant studies were searched by PubMed, Embase, Web of Science, the Cochrane Library, the Cumulative Index to Nursing and Allied Health Literature, and the China National Knowledge Infrastructure. We covered only published articles with randomized controlled trials. The outcome measures included physiological outcomes, biochemical outcomes, physical function, quality of life, and depression. A total of 35 articles with 2249 cardiovascular disease patients satisfied the inclusion criteria. The pooling revealed that TCE could decrease systolic blood pressure by 9.12 mm Hg (95% CI −16.38 to −1.86, P=0.01) and diastolic blood pressure by 5.12 mm Hg (95% CI −7.71 to −2.52, P<0.001). Patients performing TCE also found benefits compared with those in the control group in terms of triglyceride (standardized mean difference −0.33, 95% CI −0.56 to −0.09, P=0.006), 6‐minute walk test (mean difference 59.58 m, 95% CI −153.13 to 269.93, P=0.03), Minnesota Living With Heart Failure Questionnaire results (mean difference −17.08, 95% CI −23.74 to −10.41, P<0.001), 36‐Item Short Form physical function scale (mean difference 0.82, 95% CI 0.32–1.33, P=0.001), and Profile of Mood States depression scale (mean difference −3.02, 95% CI −3.50 to −2.53, P<0.001).
Conclusions
This study demonstrated that TCE can effectively improve physiological outcomes, biochemical outcomes, physical function, quality of life, and depression among patients with cardiovascular disease. More high‐quality randomized controlled trials on this topic are warranted.
Keywords: cardiovascular disease, exercise, meta‐analysis, rehabilitation
Subject Categories: Cardiorenal Syndrome, Exercise, Rehabilitation
Introduction
Cardiovascular diseases (CVDs) are the leading causes of disability and death in the world and in 2010 were considered the main risk factor for the overall global burden of disease.1, 2According to the World Health Organization,3 ≈17.3 million people worldwide died from CVD in 2008, and 80% of CVD‐related deaths were recorded in low‐ and middle‐income countries. Among CVDs, heart disorder has reportedly claimed 7.3 million lives, whereas stroke has caused 6.2 million deaths. Low‐cost, easily accessible, and symptom‐free programs are needed to treat and prevent CVD.
Physical inactivity is estimated to be the fourth main risk factor for global mortality.4, 5 Regular exercise is shown to have significant benefits for the maintenance of blood pressure and blood cholesterol.6, 7, 8 The practice and increasing global popularity of traditional Chinese exercises (TCEs), such as tai chi, qigong, and baduanjin, for >2000 years has substantially benefited human health.9, 10, 11, 12, 13 TCE is a low‐risk, promising intervention that can help improve physiological outcomes, biochemical outcomes, physical function, quality of life, and depression among patients with CVD.14, 15, 16
Although TCEs have been widely performed for the prevention and treatment of CVD,17, 18 no consensus has been reached about the benefits of these exercises for the maintenance of physiological outcomes, biochemical outcomes, physical function, and quality of life or for the prevention of depression among CVD patients. We are also unaware of any systematic reviews that have assessed the effect of TCEs on physiological outcomes, blood cholesterol, quality of life, and depression among patients with CVD.
The effect of TCEs in CVD patients must be determined based on scientific evidence to conserve time and resources. The objective of this systematic review was to determine the effects of TCEs on physiological outcomes, biochemical outcomes, physical function, quality of life, and depression among CVD patients.
Methods
The protocol for our study is registered in the international prospective register of systematic reviews (PROSPERO registration number CRD42013006474).
Search Strategy
Relevant studies published between January 1957 and January 2015 were obtained from the following electronic data sources: PubMed, Embase, Web of Science, the Cochrane Library, Cumulative Index to Nursing and Allied Health Literature (CINAHL), and the China National Knowledge Infrastructure. No language restrictions were imposed, and the search was limited to randomized controlled trials (RCTs). The full electronic search strategies for all databases are provided in Data S1.
Inclusion Criteria
First, the only studies covered were published RCTs. Second, we included articles that discussed patients with CVD including ischemic heart disease or coronary artery disease (eg, heart attack), cerebrovascular disease (eg, stroke), diseases of the aorta and arteries (eg, hypertension), and peripheral vascular disease. Third, we considered only articles that compared an intervention group, that is, a group performing TCEs (eg, tai chi, qigong, baduanjin) with a control group that performed other exercises (eg, strength exercises), that received usual care, or that did not undergo any intervention. Fourth, outcome measures included physiological outcomes (eg, blood pressure, heart rate, peak oxygen uptake), biochemical outcomes (eg, cholesterol and triglyceride [TG]), physical function (eg, 6‐minute walk test, timed up and go test), quality of life (eg, Minnesota Living With Heart Failure Questionnaire [MLHFQ], General Health Questionnaire [GHQ], and 36‐Item Short Form [SF‐36]), and depression (eg, Hamilton Depression Rating Scale [HAMD], Profile of Mood States [POMS] depression scale).
Selection of Studies
Two authors independently used the same selection criteria to screen the titles, abstracts, and full contents of the relevant articles. A study was removed from the selection if the inclusion criteria were not fulfilled. Any disagreements were resolved by discussion. A third author was consulted if a disagreement persisted.
Data Extraction and Management
The following data were extracted: study characteristics (eg, author and year), participant characteristics (eg, age and number of participants), description of interventions, duration of trial period, types of assessed outcomes, and time points. The 2 authors who selected the studies also extracted the data from the included articles. Any disagreement was resolved by discussion, and a third author was consulted if a disagreement persisted.
Quality Assessment
As recommended,19 we used the Cochrane Collaboration tool for assessing the risk of bias of the included trials. The following information was evaluated: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessments, incomplete outcome data, selective reporting, and other sources of bias.
The trials were graded as unclear, high, or low risk of bias. The methodological quality of each study was independently assessed by 2 review authors. A third author was consulted if any disagreement occurred.
Statistical Analysis
The Review Manager software (RevMan 5.2; Cochrane Collaboration) was used to conduct the meta‐analysis. We used the chi‐square test and the I2 statistic to evaluate heterogeneity among the studies. The outcome measures from the individual studies were combined by meta‐analysis using a random‐effects model. Given that all variables in the included studies were continuous data, we used the standardized mean difference (SMD) or mean difference (MD) and 95% CI to analyze the studies. The MD was used as a summary statistic in meta‐analysis when all studies reported the same outcome using the same scale. The SMD was used as a summary statistic in meta‐analysis when all studies assessed the same outcome using different scales (ie, the outcome was measured using different units). We considered P<0.05 to be statistically significant. Funnel plot asymmetry was used to assess possible publication bias by the Egger's regression test. Sensitivity analysis was conducted by removing each study individually to evaluate the quality and consistency of the results.
If the continuous data were reported as median and interquartile range, the median would be assumed to be equivalent to the mean, and the relationship of interquartile range and the standard deviation would be roughly computed as SD=IQR/1.35.20 The standard deviation could be obtained from the standard error of a mean by multiplying by the square root of the sample size: SD=SE×.20 In specific cases, we also estimated the means and standard deviations for the data and reported them graphically rather than in a table. The authors of the selected studies were contacted if the standard deviations were not shown in the paper or could not be derived from their data. If the authors contacted did not reply, their articles were excluded.
Results
Search Results
We identified 68 potentially eligible records from the 2824 records obtained from PubMed, the Cochrane Library, Embase, CINAHL, the China National Knowledge Infrastructure, and Web of Science. After reviewing the full content of the papers, 35 articles21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52, 53, 54, 55 satisfied the inclusion criteria. The remaining 33 articles were excluded for several reasons (eg, participants did not have CVD, studies were not randomized). The process of identifying the eligible studies is outlined in Figure 1. Table 1 summarizes the characteristics of each included study. The 35 articles covered 2249 patients with CVD (15 articles covered patients with heart disease, 13 articles covered those with hypertension, and 7 articles covered those with cerebrovascular disease). The countries or regions of publication were mainly the People's Republic of China (n=17, 48.57%), the United States (n=5, 14.28%), the United Kingdom (n=3, 8.57%), the Republic of Korea (n=3, 8.57%), Japan (n=2, 5.71%), Hong Kong (n=1, 2.85%), Italy (n=1, 2.85%), Taiwan (n=1, 2.85%), New Zealand (n=1, 2.85%), and Israel (n=1, 2.85%).
Figure 1.
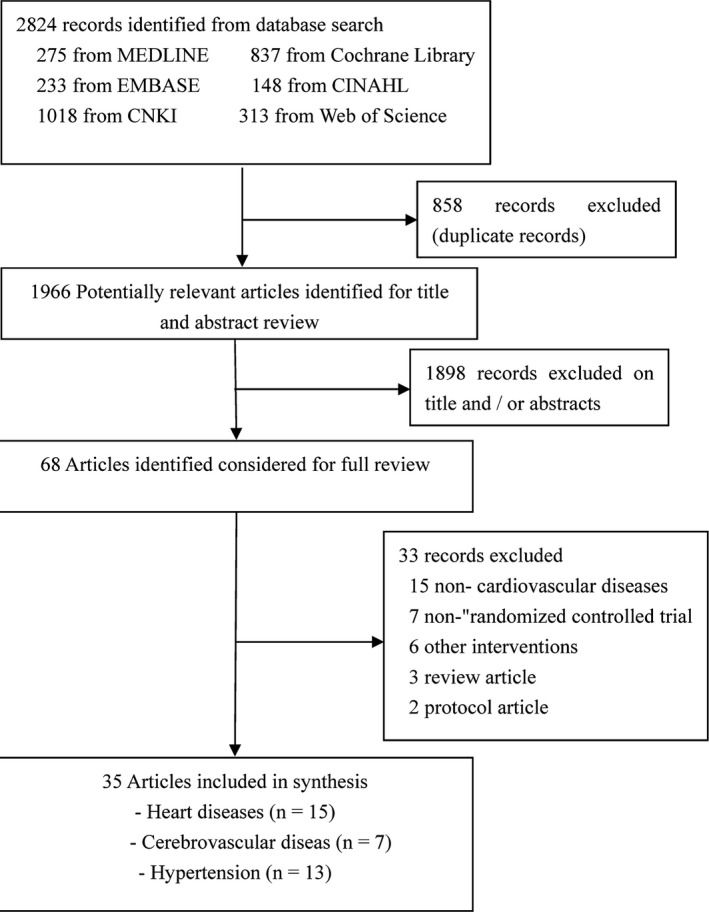
Flow chart of the study selection procedure. CKNI indicates China National Knowledge Infrastructure.
Table 1.
Characteristics of Included Studies
| Article, Year | Country/Region | Participant Characteristics, Sample Size | Disease | Intervention | Duration of Trial Period | Outcomes | Time Point |
|---|---|---|---|---|---|---|---|
| Barrow (2007)21 | UK | 65 participants (G1=32, G2=33). Mean age: G1=68.4 years, G2=67.9 years | Heart failure |
G1: Tai chi exercise G2: Standard medical care |
Twice a week for 16 weeks | Physiological outcomes (blood pressure), quality of life (MLHFQ), depression (SCL‐R depression index) | 16 weeks |
| Blake (2009)22 | UK | 20 participants (G1=10, G2=10). Mean age (SD): G1=46.2 years (11.27), G2=44.5 years (10.52). Mean duration of disease (SD): G1=16.40 years (9.04), G2=14.98 years (13.62) | Brain injury |
G1: Tai Chi and qigong exercise G2: No exercise |
Once a week for 8 weeks | QOL (GHQ) | 8 weeks |
| Cai (2010)23 | China | 60 participants (G1=30, G2=30). Mean age (SD): G1=60.3 years (10.5), G2=61.3 years (7.4) | Stroke |
G1: Baduanjin and health education G2: Health education |
4 to 5 times a week for 3 months | QOL (WHOQOL‐BREF) | 3 months |
| Caminiti (2011)24 | Italy | 60 participants (G1=30, G2=30). Mean age (SD): G1=73.4 years (2), G2=73.8 years (6). Duration of disease: >3 months | Chronic heart failure |
G1: Tai chi exercise plus endurance training G2: Endurance training |
4 sessions a week for 8 weeks | Physiological outcomes (blood pressure, heart rate), physical function (6MWT) | 12 weeks |
| Channer (1996)25 | UK | 79 participants (G1=38, G2=41). Age range: 39–80 years | Acute myocardial infarction |
G1: Tai chi exercise G2: Aerobic exercise |
Twice weekly for 3 weeks then weekly for a further 5 weeks | Physiological outcomes (blood pressure, heart rate) | 8 weeks |
| Chen (2006)26 | China | 40 participants (G1=20, G2=20). Mean age: G1=64.3 years, G2=60.7. Mean duration of disease (SD): G1=8.4 years (4.9), G2=7.8 years (5.4) | Hypertension |
G1: Tai chi plus drug G2: Drug |
7 times a week for 9 weeks | Physiological outcomes (blood pressure), biochemical outcomes (endothelin) | 10 weeks |
| Chen (2013)27 | China | 68 participants (G1=50, G2=18). Age range: 30–82 years | Hypertension |
G1: Conventional treatment and tai chi G2: Conventional treatment |
6 times a week for 12 weeks | Physiological outcomes (blood pressure) | 12 weeks |
| Chen (2013)28 | China | 60 participants (G1=32, G2=28). Mean age (SD): G1=69.3 years (10.6), G2=68.7 years (11.1) | Coronary disease |
G1: Conventional treatment and tai chi G2: Conventional treatment |
4 times a week for 12 weeks | Biochemical outcomes (TC, TG, LDL‐C, HDL‐C) | 12 weeks |
| Cheung (2005)29 | Hong Kong, China | 88 participants (G1=47, G2=41). Mean age (SD): G1=57.2 years (9.5), G2=51.2 years (7.4). Mean duration of disease (SD): G1=4.0 years (5.6), G2=3.9 years (5.1) | Hypertension |
G1: Qigong exercise G2: conventional exercise |
4 hours a week for 16 weeks | Physiological outcomes (blood pressure, heart rate), biochemical outcomes (TC, TG, LDL‐C, HDL‐C), QOL (SF‐36), depression (Beck Depression Inventory) |
4 weeks 8 weeks 12 weeks 16 weeks |
| Ding (2013)30 | China | 90 participants (G1=30, G2=30, G3=30). Mean age (SD): G1=66.2 years (11.6), G2=64.9 years (11.0), G3=66.7 years (13.1) | Percutaneous transluminal coronary intervention |
G1: Tai chi exercise G2: Walking G3: No intervention |
5 times a week for 6 months | QOL (SF‐36) |
6 weeks 6 months |
| Gemmell (2006)31 | New Zealand | 18 participants (G1=9, G2=9) | Braumatic brain injury |
G1: TCE (tai chi) G2: No intervention |
Once a week for 6 weeks | QOL (SF‐36) | 6 weeks |
| Hart (2004)32 | Israel | 152 participants (G1=56, G2=55, G3=41). Mean age (SD): G1=70.8 years (6.3), G2=70 years (6.3), G3=69.6 years (6.1) | Stroke |
G1: TCE (tai chi) G2: Hydrotherapy G3: No intervention |
Twice a week for 12 weeks | QOL (Duke Health Profile) |
6 weeks 12 weeks |
| Lee (2003)33 | Korea | 58 participants (G1=29, G2=29). Mean age (SD): G1=55.8 years (6.3), G2=57.1 years (7.6) | Hypertension |
G1: Qigong exercise G2: No intervention |
7 times a week for 10 weeks | Physiological outcomes (blood pressure, heart rate) | 10 weeks |
| Lee (2003)34 | Korea | 58 participants (G1=29, G2=29). Mean age (SD): G1=56.0 years (5.9), G2=56.5 years (7.2) | Hypertension |
G1: Qigong exercise G2: No intervention |
3 times a week for 10 weeks | Physiological outcomes (blood pressure, heart rate) | 10 weeks |
| Lee (2004)35 | Korea | 36 participants (G1=17, G2=19). Mean age (SD): G1=52.6 years (5.1), G2=54.3 years (5.5) | Hypertension |
G1: Qigong exercise G2: No intervention |
7 times a week for 8 weeks | Physiological outcomes (blood pressure), biochemical outcomes (TC, TG, HDL‐C) | 8 weeks |
| Li (2012)36 | China | 68 participants (G1=36, G2=32). Age range: 38–76 years | Stroke |
G1: Tai chi exercise G2: Strength exercise |
Twice weekly for 5 weeks | Depression (HAMD) | 5 weeks |
| Lin (2012)37 | China | 60 participants (G1=30, G2=30). Mean age (SD): G1=66.47 years (8.26) G2=64.90 years (8.87) | Coronary artery bypass grafting |
G1: Baduanjin G2: Conventional exercise |
4–5 times a week for 23 weeks | QOL |
8 weeks 20 weeks |
| Luo (2006)38 | China | 84 participants (G1=44, G2=40). Mean age (SD): G1=44.74 years (12.1), G2=44.86 years (13.05) | Hypertension |
G1: Tai chi plus drug G2: Drug |
7 times a week for 6 months | Physiological outcomes (blood pressure) | 6 months |
| Mao (2006)39 | China | 62 participants (G1=51, G2=11). Mean age: G1=62.2 years, G2=63.3 | Hypertension |
G1: Tai chi exercise G2: Drug |
6 times a week for 8 weeks | Physiological outcomes (blood pressure), biochemical outcomes (endothelin, no) | 8 weeks |
| Ning (2010)40 | China | 50 participants (G1=26, G2=24). Mean age (SD): G1=53.9 years (6.4), G2=53.5 years (6.7) | Coronary disease |
G1: Tai chi exercise G2: Drug |
2 or 3 times a week for 6 months | Biochemical outcomes (TC, TG) | 8 weeks |
| Pan (2009) 41 | China | 48 participants (G1=24, G2=24). Mean age (SD): G1=62.1 years (5.8), G2=61.4 years (7.1) | Hypertension |
G1: Baduanjin exercise plus drug G2: Drug |
5 times a week for 24 weeks | Physiological outcomes (blood pressure), biochemical outcomes (TC, TG, HDL‐C) | 24 weeks |
| Sato (2010)42 | Japan | 20 participants (G1=10, G2=10). Mean age (SD): G1=68 years (5), G2=68 years (4). Mean duration of disease (SD): G1=19 months (15), G2=21 months (13) | Coronary disease |
G1: Tai chi exercise plus conventional rehabilitation G2: Conventional rehabilitation |
4 times a week for 1 year | Physiological outcomes (peak oxygen uptake, blood pressure, heart rate) | 1 year |
| Taylor‐Piliae (2012)43 | USA | 28 participants (G1=16, G2=12). Mean age (SD): G1=72.8 years (10.1), G2=64.5 years (10.9). Mean duration of disease (SD): G1=58.3 months (46.7), G2=47.9 months (42.5) | Chronic stroke |
G1: Tai chi G2: Usual care |
Once a week for 8 weeks | Physical function (Short Physical Performance Battery), QOL (SF‐36) | 8 weeks |
| Tsai (2003)44 | Taiwan, China | 76 participants (G1=37, G2=39). Mean age (SD): G1=50.5 years (7), G2=62.7 years (4) | Hypertension |
G1: TCE (tai chi chuan) G2: Sedentary life controls |
3 times a week for 12 weeks | Physiological outcomes (blood pressure, heart rate), biochemical outcomes (TC, TG, LDL‐C, HDL‐C) | 12 weeks |
| Wang (1989)45 | China | 100 participants (G1=50, G2=50). Age range: 45–65 | Hypertension |
G1: Qigong exercise plus drug G2: Drug |
7 times a week for 1 year | Biochemical outcomes (TC, TG, LDL‐C, HDL‐C) | 1 year |
| Wang (2010)46 | Japan | 34 participants (G1=17, G2=17). Age: >50 years | Cerebral vascular disorder |
G1: TCE (tai chi) G2: Rehabilitation exercise |
Once a week for 12 weeks | QOL (GHQ), depressing (GHQ) | 12 weeks |
| Wang (2012)47 | China | 69 participants (G1=36, G2=33). Mean age (SD): G1=55.8 years (3.54), G2=51.2 years (7.8) | Stroke |
G1: Tai chi exercise G2: Conventional exercise |
2 times a week for 3 months | QOL (SF‐36) and depression (HAMD) | 6 months |
| Wang (2013)48 | China | 60 participants (G1=30, G2=30). Mean age (SD): G1=55.25 years (11.13), G2=54.86 years (12.05) | Percutaneous transluminal coronary intervention |
G1: Conventional treatment and tai chi G2: Conventional treatment |
5 times a week for 6 months | QOL (SF‐36) | 3 months 6 months |
| Yao (2010)49 | China | 150 participants (G1=80, G2=70). Mean age (SD): G1=52.4 years (6.32), G2=51.7 years (7.26) | Chronic heart failure |
G1: Conventional treatment and tai chi G2: Conventional treatment |
>5 times a week for 6 months | Physical function (6MWT), quality of life (SF‐36) | 6 months |
| Yeh (2004)50 | USA | 30 participants (G1=15, G2=15). Mean age (SD): G1=66 years (12), G2=61 years (14) | Chronic heart failure |
G1: Usual care and tai chi exercise G2: Usual care |
Twice weekly for 12 weeks | Physiological outcomes (peak oxygen uptake), biochemical outcomes (BNP), physical function (6MWT), QOL (MLHFQ) | 12 weeks |
| Yeh (2008)51 | USA | 18 participants (G1=8, G2=10). Mean age (SD): G1=54.7 years (11.8), G2=64.2 years (16.2) | Chronic heart failure |
G1: Tai chi exercise and usual care G2: Usual care |
Twice weekly for 12 weeks | Biochemical outcomes (BNP), physical function (6MWT), quality of life (MLHFQ) | 12 weeks |
| Yeh (2011)52 | USA | 100 participants (G1=50, G2=50). Mean age (SD): G1=68.1 years (11.9), G2=66.6 years (12.1) | Chronic heart failure |
G1: Usual care and tai chi exercise G2: Usual care and education sessions |
Twice weekly for 12 weeks | Physiological outcomes (peak oxygen uptake), biochemical outcomes (BNP), physical function (timed up and go, 6MWT), QOL (MLHFQ), depression (POMS) | 12 weeks |
| Yeh (2013)53 | USA | 16 participants (G1=8, G2=8). Mean age (SD): G1=68 years (11), G2=63 years (11) | Heart failure |
G1: Tai chi exercise G2: Aerobic exercise |
Twice weekly for 12 weeks | Physiological outcomes (blood pressure, Peak oxygen uptake, heart rate), biochemical outcomes (BNP), physical function (time up and go, 6MWT), quality of life (MLHF), depression (POMS) | 12 weeks |
| Yu (2013)54 | China | 104 participants (G1=52, G2=52). Age range: 40–70 years | Hypertension |
G1: Baduanjin exercise plus education G2: Education |
3 or 4 times a week for 1 year | Blood pressure | 1 year |
| Zhang (2013)55 | China | 120 participants (G1=60, G2=60). Mean age: G1=73.9 years, G2=76.5 years | Hypertension |
G1: Baduanjin exercise plus drug G2: Drug |
7 times a week for 2 months | QOL | 2 months |
6MWT indicates 6‐minute walk test; BNP, B‐type natriuretic peptide; G, group; GHQ, General Health Questionnaire; HAMD, Hamilton Depression Rating Scale; HDL‐C, high‐density lipoprotein cholesterol; LDL‐C, low‐density lipoprotein cholesterol; MLHFQ, Minnesota Living With Heart Failure Questionnaire; POMS, Profile of Mood States; QOL, quality of life; SCL‐R, Symptom Checklist 90–Revised; SF‐36, 36‐Item Short Form; TC, total cholesterol; TCE, traditional Chinese exercise; TG, triglyceride; WHOQOL‐BREF, World Health Organization Quality of Life project 26‐item instrument.
Risk of Bias Among the Selected Articles
We assessed the risk of bias in all selected articles (Table 2). All articles used the generation of the allocation sequence (n=35, 100%). Allocation concealment was inadequate in most articles (n=26, 74%). None of the studies blinded their participants or personnel. Eight articles (23%) masked their outcome assessors to the treatment allocation. A low risk of incomplete outcome bias was reported in 31 articles (88.5%), whereas a low risk of selective reporting bias was reported in most articles (n=28, 73.6%).
Table 2.
Risk of Bias Assessment of Included Studies
| Article, Year | Random Sequence Generation | Allocation Concealment | Blinding of Participants and Personnel | Blinding of Outcome Assessment | Incomplete Outcome Data | Selective Reporting | Other Bias |
|---|---|---|---|---|---|---|---|
| Barrow (2007)21 | Low | High | High | High | Low | Low | Unclear |
| Blake (2009)22 | Low | Low | High | High | Low | Low | Unclear |
| Cai (2010)23 | Low | High | High | High | Low | Low | Unclear |
| Caminiti (2011)24 | Low | High | High | High | Low | Low | Unclear |
| Channer (1996)25 | Low | High | High | High | Low | Low | Unclear |
| Chen (2006)26 | Low | High | High | High | Low | Low | Unclear |
| Chen (2013)27 | Low | High | High | High | Low | Low | Unclear |
| Chen (2013)28 | Low | High | High | High | Low | Low | Unclear |
| Cheung (2005)29 | Low | Low | High | Low | Low | Low | Unclear |
| Ding (2013)30 | Low | High | High | High | Low | Low | Unclear |
| Gemmell (2006)31 | Low | High | High | Low | Low | Low | Unclear |
| Hart (2004)32 | Low | High | High | High | Low | Low | Unclear |
| Lee (2003)33 | Low | High | High | High | Unclear | Unclear | Unclear |
| Lee (2003)34 | Low | Low | High | High | Unclear | Unclear | Unclear |
| Lee (2004)35 | Low | High | High | High | Low | Unclear | Unclear |
| Li (2012)36 | Low | High | High | High | Low | Low | Unclear |
| Lin (2012)37 | Low | High | High | High | Low | Low | Unclear |
| Luo (2006)38 | Low | High | High | High | Low | Low | Unclear |
| Mao (2006)39 | Low | High | High | High | Low | Low | Unclear |
| Ning (2010)40 | Low | High | High | High | Low | Low | Unclear |
| Pan (2009)41 | Low | Low | High | High | Low | Low | Unclear |
| Sato (2010)42 | Low | High | High | High | Low | Low | Unclear |
| Taylor‐Piliae (2012)43 | Low | Low | High | Low | Low | Low | Unclear |
| Tsai (2003)44 | Low | Low | High | Low | Low | Low | Unclear |
| Wang (1989)45 | Low | High | High | High | Low | Low | Unclear |
| Wang (2010)46 | Low | High | High | Low | Low | Low | Unclear |
| Wang (2012)47 | Low | High | High | High | Unclear | Low | Unclear |
| Wang (2013)48 | Low | High | High | High | Low | Low | Unclear |
| Yao (2010)49 | Low | High | High | High | Low | Low | Unclear |
| Yeh (2004)50 | Low | Low | High | Low | Low | Unclear | Unclear |
| Yeh (2008)51 | Low | High | High | High | Unclear | Unclear | Unclear |
| Yeh (2011)52 | Low | Low | High | Low | Low | Unclear | Unclear |
| Yeh (2013)53 | Low | Low | High | Low | Low | Unclear | Unclear |
| Yu (2013)54 | Low | High | High | High | Low | Low | Unclear |
| Zhang (2013)55 | Low | High | High | High | Low | Low | Unclear |
Effects of TCE on Physiological Outcomes
Blood pressure
Sixteen articles* involving 939 patients compared the systolic blood pressures (SBPs) and diastolic blood pressures (DBPs) between patients performing TCEs and those in the control group. Based on a random‐effects model, TCE was found to decrease SBP by 9.12 mm Hg (95% CI −16.38 to −1.86, P=0.01; I2=99%, P<0.00001) and DBP by 5.12 mm Hg (95% CI −7.71 to −2.52, P<0.001; I2=97%, P<0.00001) among patients performing TCEs compared with those in the control group (Figure 2 and Table 3).
Figure 2.
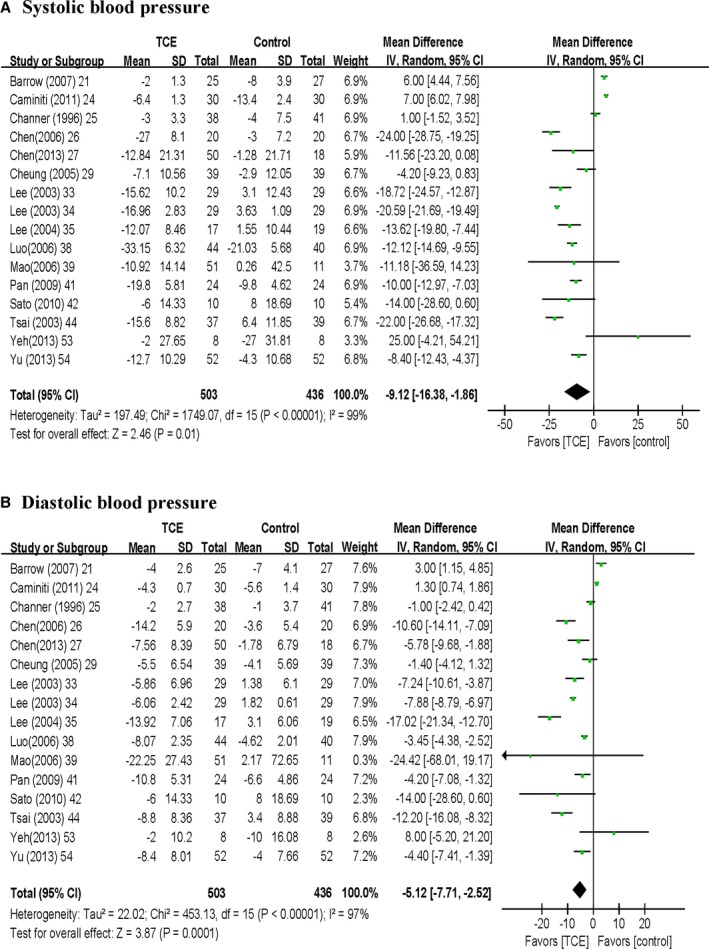
Meta‐analysis of effects of traditional Chinese exercise on blood pressure: (A) systolic blood pressure, (B) diastolic blood pressure. IV, inverse variance; Std., standardized; TCE, traditional Chinese exercise.
Table 3.
Summary of Results
| Outcome | Trials | Participants | Statistical Method | Effect Estimate | Heterogeneity | P Value |
|---|---|---|---|---|---|---|
| Physiological outcomes | ||||||
| SBP, mm Hg | 1621, 24, 25, 26, 27, 29, 33, 34, 35, 38, 39, 41, 42, 44, 53, 54 | 939 | MD (IV, random, 95% CI) | −9.12 [−16.38 to −1.86] | <0.001 | 0.01 |
| DBP, mm Hg | 1621, 24, 25, 26, 27, 29, 33, 34, 35, 38, 39, 41, 42, 44, 53, 54 | 939 | MD (IV, random, 95% CI) | −5.12 [−7.71 to −2.52] | <0.001 | <0.001 |
| Heart rate, beats per minute | 924, 25, 29, 33, 34, 42, 44, 51, 53 | 463 | MD (IV, random, 95% CI) | −2.39 [−5.61 to 0.82] | <0.001 | 0.14 |
| Peak oxygen uptake, L/min | 442, 50, 52, 53 | 166 | SMD (IV, random, 95% CI) | 0.04 [−0.46 to 0.55] | 0.11 | 0.87 |
| Biochemical outcomes | ||||||
| TG | 628, 29, 35, 41, 44, 45 | 408 | SMD (IV, random, 95% CI) | −0.33 [−0.56 to −0.09] | 0.23 | 0.006 |
| TC | 628, 29, 35, 41, 44, 45 | 408 | SMD (IV, random, 95% CI) | −1.12 [−1.97 to −0.27] | <0.001 | 0.01 |
| LDL‐C | 428, 29, 44, 45 | 324 | SMD (IV, random, 95% CI) | −0.81 [−1.24 to −0.38] | 0.02 | <0.001 |
| HDL‐C | 628, 29, 35, 41, 44, 45 | 408 | SMD (IV, random, 95% CI) | 0.74 [0.29–1.18] | <0.001 | 0.001 |
| BNP, ng ⁄ mL | 350, 52, 53 | 146 | MD (IV, random, 95% CI) | −23.04 [−27.10 to −18.98] | 0.73 | <0.001 |
| Physical function | ||||||
| Timed up and go test, s | 252, 53 | 116 | MD (IV, random, 95% CI) | −0.20 [−0.64 to 0.24] | 0.77 | 0.38 |
| 6‐minute walk test, m | 624, 49, 50, 51, 52, 53 | 374 | MD (IV, random, 95% CI) | 59.58 [4.95–114.20] | <0.001 | 0.03 |
| Quality of life | ||||||
| MLHFQ | 521, 50, 51, 52, 53 | 216 | MD (IV, random, 95% CI) | −17.08 [−23.74 to −10.41] | 0.02 | <0.001 |
| GHQ | 222, 46 | 49 | MD (IV, random, 95% CI) | −1.02 [−2.91 to 0.87] | 0.19 | 0.29 |
| SF‐36, total | 230, 49 | 148 | MD (IV, random, 95% CI) | −5.95 [−16.16 to 4.27] | 0.02 | 0.25 |
| SF‐36, general health | 329, 31, 49 | 126 | MD (IV, random, 95% CI) | −1.56 [−2.52 to −0.61] | 0.4 | 0.001 |
| SF‐36, physical function | 329, 31, 43 | 131 | MD (IV, random, 95% CI) | 0.82 [0.32–1.33] | 0.45 | 0.001 |
| SF‐36, mental health | 329, 31, 43 | 131 | MD (IV, random, 95% CI) | −2.67 [−10.08 to 4.75] | 0.09 | 0.48 |
| Depression | ||||||
| HAMD | 236, 47 | 129 | MD (IV, random, 95% CI) | −3.97 [−5.05 to −2.89] | 0.91 | <0.001 |
| POMS depression scale | 252, 53 | 116 | MD (IV, random, 95% CI) | −3.02 [−3.50 to −2.53] | 0.76 | <0.001 |
BNP indicates B‐type natriuretic peptide; DBP, diastolic blood pressure; GHQ, General Health Questionnaire; HAMD, Hamilton Depression Rating Scale; HDL‐C, high‐density lipoprotein cholesterol; IV, inverse variance; LDL‐C, low‐density lipoprotein cholesterol; MD, mean difference; MLHFQ, Minnesota Living With Heart Failure Questionnaire; POMS, Profile of Mood States; SBP, systolic blood pressure; SF‐36, 36‐Item Short Form; SMD, standardized mean difference; TC, total cholesterol; TG, triglyceride.
Heart rate
Nine articles** involving 463 patients compared the heart rate between patients performing TCEs and those in the control group. No significant differences were observed between the 2 groups based on a random‐effects model (MD −2.39 beats per minute, 95% CI −5.61 to −0.82, P=0.14) (Table 3).
Peak oxygen uptake
Four articles42, 50, 52, 53 involving 166 patients compared the peak oxygen uptake of patients performing TCEs and those in the control group. The peak oxygen uptake of patients performing TCEs did not increase significantly compared with that of the patients in the control group, based on a random‐effects model (SMD 0.04, 95% CI −0.46 to 0.55, P=0.87) (Table 3).
Sensitivity analysis revealed that the pooled results of SBP, DBP, and peak oxygen uptake did not change statistical significance of the overall analysis when studies were removed 1 by 1. When 1 study24 was removed, however, the result of heart rate was significant in the sensitivity analysis; it offered inferior evidence for the effect of TCE on heart rate. The sensitivity analysis did not affect heterogeneity of blood pressure, heart rate, or peak oxygen uptake outcomes.
Effects of TCE on Biochemical Outcomes
Triglyceride
Six articles28, 29, 35, 41, 44, 45 involving 408 patients compared the TG levels of patients performing TCEs and those in the control group. Based on a random‐effects model, the TG levels of patients performing TCEs significantly decreased (SMD −0.33, 95% CI −0.56 to −0.09, P=0.006; I2=28%, P=0.23) compared with those of the patients in the control group (Figure 3A and Table 3).
Figure 3.
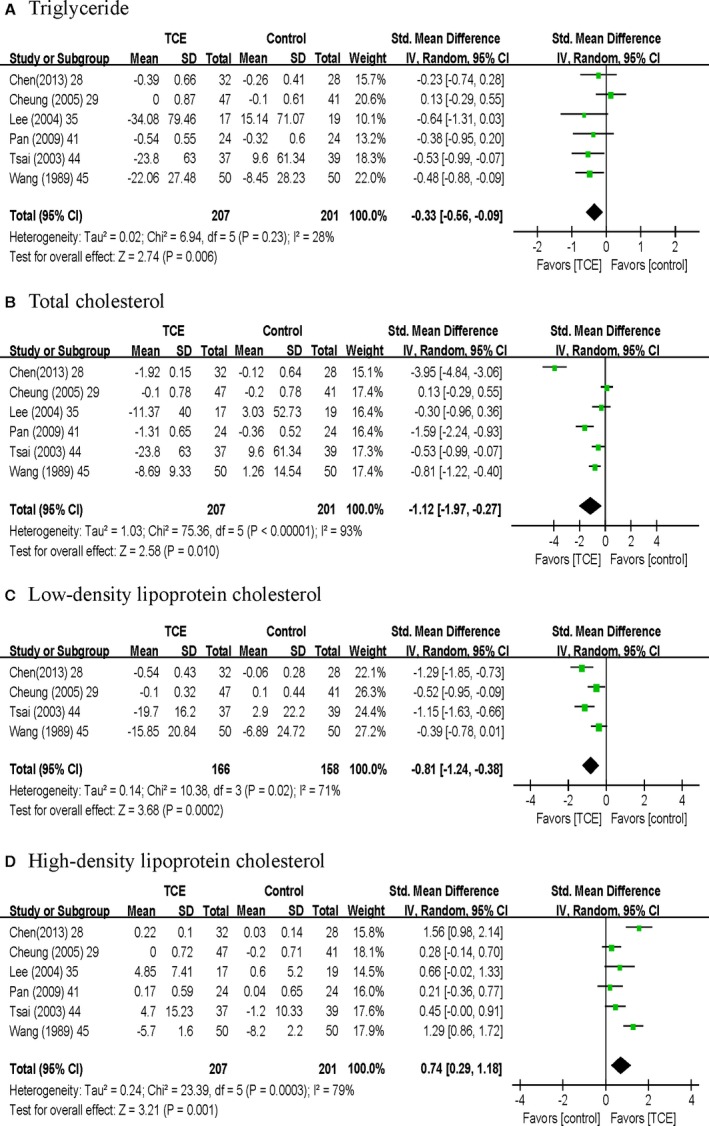
Meta‐analysis of effects of traditional Chinese exercise on biochemical outcomes: (A) triglyceride, (B) total cholesterol, (C) low‐density lipoprotein cholesterol, (D) high‐density lipoprotein cholesterol. IV, inverse variance; TCE, traditional Chinese exercise.
Total cholesterol
Six articles28, 29, 35, 41, 44, 45 involving 408 patients were included to estimate the effect of TCEs on the amount of total cholesterol (TC). TC of the patients performing TCEs significantly improved (SMD −1.12, 95% CI −1.97 to −0.27, P=0.01; I2=93%, P<0.00001) compared with that of the patients in the control group based on a random‐effects model (Figure 3B and Table 3).
Low‐density lipoprotein cholesterol
Four articles28, 29, 44, 45 involving 324 patients compared the low‐density lipoprotein cholesterol (LDL‐C) levels between patients performing TCEs and those in the control group. In a random‐effects model, the LDL‐C of patients performing TCEs significantly decreased (SMD −0.81, 95% CI −1.24 to −0.38, P<0.001; I2=71%, P=0.02) compared with that of the patients in the control group (Figure 3C and Table 3).
High‐density lipoprotein cholesterol
Six articles28, 29, 35, 41, 44, 45 involving 408 patients were included in the meta‐analysis to assess the effect of TCE on HDL‐C. The HDL‐C of patients performing TCEs significantly improved (SMD 0.74, 95% CI 0.29–1.18, P=0.001; I2=79%, P=0.0003) compared with that of the patients in the control group based on a random‐effects model (Figure 3D and Table 3).
B‐type natriuretic peptide
Three articles50, 52, 53 involving 146 patients compared the B‐type natriuretic peptide (BNP) of patients performing TCEs and those in the control group. Based on a random‐effects model, the BNP of the patients performing TCEs significantly improved (MD −23.04 ng/mL, 95% CI −27.10 to −18.98, P<0.001) compared with that of the patients in the control group (Table 3).
Sensitivity analysis revealed that TG, TC, LDL‐C, and HDL‐C outcomes were stable when studies were removed 1 by 1. The significance of the BNP outcome was changed in the sensitivity analysis when 1 study52 was removed; this result offered inferior evidence for the effect of TCE on BNP. The sensitivity analysis did not affect heterogeneity of TG, TC, LDL‐C, HDL‐C and BNP outcomes.
Effects of TCE on Physical Function
Timed up and go test
Two articles52, 53 involving 116 patients compared the timed up and go tests of patients performing TCEs and those in the control group. No significant difference was found between the 2 groups (MD −0.2 second, 95% CI −0.64 to 0.24, P=0.38) (Table 3).
Six‐minute walk test
Six articles24, 49, 50, 51, 52, 53 involving 374 patients were used to estimate the effect of TCE on 6‐minute walk test. The 6‐minute walk tests of patients performing TCEs improved by 59.58 m (95% CI 4.95–114.20, P=0.03; I2=93%, P<0.00001) compared with that of the control group, based on a random‐effects model (Figure 4A and Table 3). Sensitivity analysis revealed that the 6‐minute walk test outcome was not stable when studies were removed 1 by 1. The sensitivity analysis did not affect heterogeneity of the timed up and go or 6‐minute walk test outcomes.
Figure 4.
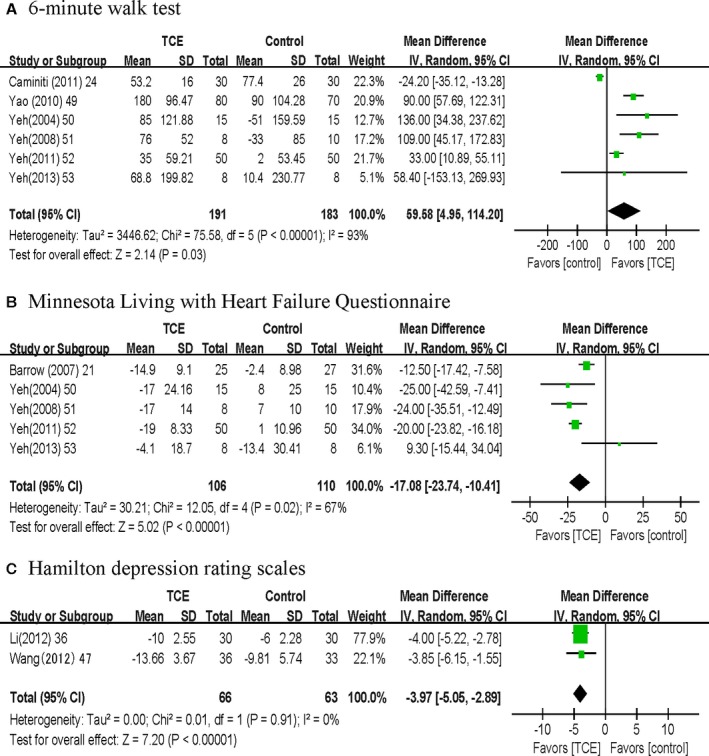
Meta‐analysis of effects of traditional Chinese exercise on (A) 6‐minute walk test, (B) Minnesota Living with Heart Failure Questionnaire, and (C) Hamilton depression rating scales. IV, inverse variance; TCE, traditional Chinese exercise.
Effects of TCE on Quality of Life
Minnesota Living With Heart Failure Questionnaire
Five articles21, 50, 51, 52, 53 involving 216 patients were included to assess the effect of TCE on MLHFQ. The MLHFQ scores of patients performing TCEs significantly improved (MD −17.08, 95% CI −23.74 to −10.41, P<0.001; I2=67%, P=0.02) compared with that of the patients in the control group, based on a random effects model (Figure 4B and Table 3).
General Health Questionnaire
Two articles22, 46 involving 49 patients compared the GHQ scores of patients performing TCEs and those in the control group. No significant differences were found between these groups based on a random‐effects model (MD −1.02, 95% CI −2.91 to 0.87, P=0.29; I2=43%, P=0.29) (Table 3).
36‐Item Short Form
Five articles29, 30, 31, 43, 46, 49 involving 374 patients were used to estimate the effect of TCE on SF‐36. Compared with the patients in the control group, those performing TCEs showed improved SF‐36 general health results (MD −1.56, 95% CI −2.52 to −0.61, P=0.001; I2=0%, P=0.4) and SF‐36 physical function (MD 0.82, 95% CI 0.32–1.33, P=0.001; I2=0%, P=0.45). No significant differences were found between the 2 groups in terms of SF‐36 total score (MD −5.95, 95% CI −16.16 to 4.27, P=0.25; I2=82%, P=0.02) and SF‐36 mental health results (MD −2.67, 95% CI −10.08 to 4.75, P=0.29; I2=43%, P=0.09) (Table 3).
Sensitivity analysis revealed that MLHFQ outcome was stable when studies were removed 1 by 1. The significance of SF‐36 outcome was changed in the sensitivity analysis when 1 study was removed;31 this result offered inferior evidence for the effect of TCE on SF‐36. The sensitivity analysis did not affect heterogeneity of SF‐36 outcome, but sensitivity analysis affected heterogeneity of MLHFQ outcome.
Effects of TCE on Depression
Hamilton Depression Rating Scale
Two articles36, 47 involving129 patients compared HAMD scores for patients performing TCEs and those in the control group. The HAMD scores of patients performing TCEs improved (MD −3.97, 95% CI −5.05 to −2.89, P<0.001; I2=0, P=0.91) compared with those of patients in the control group, based on a random‐effects model (Figure 4C and Table 3).
POMS Depression Scale
Two articles52, 53 involving 116 patients were included to assess the effect of TCE on the POMS depression scale. The POMS depression scale scores of the patients performing TCEs significantly improved (MD −3.02, 95% CI −3.50 to −2.53, P<0.001; I2=0%, P=0.76) compared with those of patients in the control group, based on a random‐effects model (Table 3).
Publication Bias
The Egger's regression test results did not show any publication bias for SBP (asymmetry test P=0.46), DBP (asymmetry test P=0.192), heart rate (asymmetry test P=0.406), TG (asymmetry test P=0.503), TC (asymmetry test P=0.08), HDL‐C (asymmetry test P=0.814), 6‐minute walk test (asymmetry test P=0.871), and MLHFQ (asymmetry test P=0.304).
Discussion
TCEs are mind–body exercises that focus on posture, coordination of breathing patterns, and meditation. Several TCEs are used to treat patients with CVDs. Previous systematic reviews focused on specific TCEs, such as tai chi and qigong.18, 56, 57, 58 This systematic review compiled evidence from a large number of trials assessing the effectiveness of TCEs to evaluate the overall effect of TCEs on patients with CVD compared with other exercises or of the absence of any intervention.
This systematic review and meta‐analysis included 35 RCTs involving 2249 patients with CVD to provide further evidence of the effect of TCEs on physiological outcomes, biochemical outcomes, quality of life, and depression in CVD patients. The SBP, DBP, TG, TC, LDL‐C, HDL‐C, BNP, 6‐minute walk test, MLHFQ, SF‐36 (general health and physical function), HAMD, and POMS depression scale of patients performing TCEs significantly improved compared with those of the patients in the control group. The benefits of TCEs for SBP, DBP, TG, TC, LDL‐C, HDL‐C, MLHFQ, and depression of CVD patients reached certain levels that could signify clinical importance. In particular, the effects TCE on blood pressure and blood lipids are clinically significant because blood pressure and LDL‐C are the primary targets for cardiovascular risk reduction.
A meta‐analysis59 showed that by reducing the SBP and DBP by 10 and 5 mm Hg, respectively, TCE could reduce the occurrences of stroke and coronary heart disease by 41% and 22%, respectively. Another systematic review revealed that the morbidity and mortality of CVDs could be reduced by up to 50% if blood cholesterol was reduced by ≈20%, SBP by 10 to 15 mm Hg, and DBP by 5 to 8 mm Hg.60 Based on current evidence from systematic reviews, TCE could improve the quality of life and reduce the depression of CVD patients; however, no significant differences were found between patients performing TCEs and those in the control group in terms of heart rate, peak oxygen uptake, timed up and go test, and 12‐item GHQ.
Although the intensity of TCE ranged from low to moderate, we found that TCE could improve physiological outcomes (eg, blood pressure), biochemical outcomes (eg, cholesterol and TG), quality of life (eg, MLHFQ), and depression of patients with CVDs. TCE has a complex mechanism for treating CVD. TCE is based on the theoretical principles of traditional Chinese medicine. The integrated exercise of mind and body, which includes stillness of mind, flow of breath, movement of body, and self‐correction of posture, activates the natural self‐regulatory (self‐healing) ability and evokes a balanced release of endogenous neurohormones and a wide array of natural health recoverymechanisms.61 Nevertheless, the contribution of TCEs in improving the health of patients with CVD requires further investigation.
The pooled estimate of effect for the outcome (Figure 2) has significant heterogeneity. There may be important clinical and methodological differences among studies that influence the differences between intervention and controls. Some differences existed in inclusion criteria and among the participants, who came from different countries and may have different understandings of TCE. Different types of TCE include not only include tai chi but also baduanjin, yijinjing, and other forms. Even tai chi has a lot of branches.
Strengths and Limitations
This paper is the first systematic review and meta‐analysis to assess and compare the effects of TCE with other exercises or with no intervention regarding physiological outcomes (eg, blood pressure), biochemical outcomes (eg, cholesterol and TG), quality of life, and depression among patients with CVD. Unlike prior systematic reviews, more than a quarter of the included studies were published within the past 2 years.
This systematic review searched a wide variety of electronic databases for relevant articles. We searched primarily for articles in the Chinese electronic database because TCEs originated in China. Two reviewers independently selected the studies, extracted the data, and evaluated the quality of the studies to decrease bias and transcription errors. Consequently, the results of our systematic review are considered robust.
Our meta‐analysis had several limitations. First, although all included studies were RCTs, only a few (9 of 35) clearly indicated allocation concealment in their experimental procedures; therefore, selection bias or confounding may be present. Moreover, only 8 of the included studies blinded their assessors. Second, only 2 or 3 of the included studies assessed the effect of TCE on BNP, timed up and go test, GHQ‐12, SF‐36, HAMD, and POMS. More quality RCTs are needed to have confidence in the results in the future. Third, although 6 electronic databases were searched systematically for relevant articles by using a prespecified search strategy and because publication bias was assessed by Egger's regression test, we did not search for any unpublished trials. Consequently, the probability of publication bias may also exist in our study. Fourth, the follow‐up durations of most studies were no longer than 1 year; therefore, we did not perform the meta‐analysis to assess the long‐term effect of TCE for CVD patients. Although each included study was an RCT, most of these studies did not adhere to the generally accepted standards in reporting clinical trials (eg, the Consolidated Standards of Reporting Trials statement).62 The methodological standards of future studies must be improved in terms of allocation concealment, blinding of outcome assessment, adequate follow‐up, and intention‐to‐treat analysis. Fifth, TCE includes different types of exercise, and it is necessary to have detailed subgroups for different types of TCE and different types of controls in the future.
Conclusions
This study showed that TCE could provide more benefits than other exercises or no intervention for decreasing SBP and DBP and improving biochemical outcomes, physical function, quality of life, and depression in patients with CVD. The results may improve some CVD risk factors; therefore, the clinical implications of our systematic review results showed that TCE should be useful for patients with CVD, medical staff, and health care decision makers. Nevertheless, extreme heterogeneity in the analyses remained unexplained, and the number of high‐quality studies was not large in the systematic review. More multicenter RCTs with large sample sizes must be conducted to assess the effects of TCEs in CVD patients. The long‐term effectiveness of TCEs for patients with CVD must also be evaluated. Theories about how TCE could treat patients with CVDs and prevent such diseases should be further clarified.
Author Contributions
All authors read and approved the final manuscript. Conceived and designed the experiments: P.‐J. Chen, X.Q. Wang and Y.L. Pi. Extracted the information from the eligible studies: Y. Liu, R. Wang, X. Li. Analyzed the data: B.L. Chen, Y. Zhu, X.Q. Wang. Contributed reagents/materials/analysis tools: Y.J. Yang, Z.B. Niu. Wrote the paper: X.Q. Wang, P.J. Chen.
Sources of Funding
This study was supported by the Shanghai Key Lab of Human Performance (Shanghai University of Sport) (No. 11DZ2261100); National Natural Science Foundation of China (81501956); Innovation Program of Shanghai Municipal Education Commission (15ZZ084); Shanghai Committee of Science and Technology (14490503800); Shanghai Youth Science and Technology Sail Project (15YF1411400), the Key Disciplines Group Construction Project of Pudong Health Bureau of Shanghai (grant no. PWZxkq2011‐02).
Disclosures
None.
Supporting information
Data S1. Search strategies for all databases.
(J Am Heart Assoc. 2016;5:e002562 doi: 10.1161/JAHA.115.002562)
An accompanying Data S1 is available at http://jaha.ahajournals.org/content/5/3/e002562/suppl/DC1
Notes
References
- 1. Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair‐Rohani H, Amann M, Anderson HR, Andrews KG, Aryee M, Atkinson C, Bacchus LJ, Bahalim AN, Balakrishnan K, Balmes J, Barker‐Collo S, Baxter A, Bell ML, Blore JD, Blyth F, Bonner C, Borges G, Bourne R, Boussinesq M, Brauer M, Brooks P, Bruce NG, Brunekreef B, Bryan‐Hancock C, Bucello C, Buchbinder R, Bull F, Burnett RT, Byers TE, Calabria B, Carapetis J, Carnahan E, Chafe Z, Charlson F, Chen H, Chen JS, Cheng AT, Child JC, Cohen A, Colson KE, Cowie BC, Darby S, Darling S, Davis A, Degenhardt L, Dentener F, Des Jarlais DC, Devries K, Dherani M, Ding EL, Dorsey ER, Driscoll T, Edmond K, Ali SE, Engell RE, Erwin PJ, Fahimi S, Falder G, Farzadfar F, Ferrari A, Finucane MM, Flaxman S, Fowkes FG, Freedman G, Freeman MK, Gakidou E, Ghosh S, Giovannucci E, Gmel G, Graham K, Grainger R, Grant B, Gunnell D, Gutierrez HR, Hall W, Hoek HW, Hogan A, Hosgood HD III, Hoy D, Hu H, Hubbell BJ, Hutchings SJ, Ibeanusi SE, Jacklyn GL, Jasrasaria R, Jonas JB, Kan H, Kanis JA, Kassebaum N, Kawakami N, Khang YH, Khatibzadeh S, Khoo JP, Kok C, Laden F, Lalloo R, Lan Q, Lathlean T, Leasher JL, Leigh J, Li Y, Lin JK, Lipshultz SE, London S, Lozano R, Lu Y, Mak J, Malekzadeh R, Mallinger L, Marcenes W, March L, Marks R, Martin R, McGale P, McGrath J, Mehta S, Mensah GA, Merriman TR, Micha R, Michaud C, Mishra V, Mohd Hanafiah K, Mokdad AA, Morawska L, Mozaffarian D, Murphy T, Naghavi M, Neal B, Nelson PK, Nolla JM, Norman R, Olives C, Omer SB, Orchard J, Osborne R, Ostro B, Page A, Pandey KD, Parry CD, Passmore E, Patra J, Pearce N, Pelizzari PM, Petzold M, Phillips MR, Pope D, Pope CA III, Powles J, Rao M, Razavi H, Rehfuess EA, Rehm JT, Ritz B, Rivara FP, Roberts T, Robinson C, Rodriguez‐Portales JA, Romieu I, Room R, Rosenfeld LC, Roy A, Rushton L, Salomon JA, Sampson U, Sanchez‐Riera L, Sanman E, Sapkota A, Seedat S, Shi P, Shield K, Shivakoti R, Singh GM, Sleet DA, Smith E, Smith KR, Stapelberg NJ, Steenland K, Stöckl H, Stovner LJ, Straif K, Straney L, Thurston GD, Tran JH, Van Dingenen R, van Donkelaar A, Veerman JL. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2224–2260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Taylor‐Piliae RE. Tai Ji Quan as an exercise modality to prevent and manage cardiovascular disease: a review. J Sport Health Sci. 2014;3:43–51. [Google Scholar]
- 3. World Health Organization . Global Atlas on Cardiovascular Disease Prevention and Control. Geneva: World Health Organization; 2011. [Google Scholar]
- 4. Kohl HW III, Craig CL, Lambert EV, Inoue S, Alkandari JR, Leetongin G, Kahlmeier S; Lancet Physical Activity Series Working Group . The pandemic of physical inactivity: global action for public health. Lancet. 2012;380:294–305. [DOI] [PubMed] [Google Scholar]
- 5. Li L. The financial burden of physical inactivity. J Sport Health Sci. 2014;3:58–59. [Google Scholar]
- 6. Vasconcellos F, Seabra A, Katzmarzyk PT, Kraemer‐Aguiar LG, Bouskela E, Farinatti P. Physical activity in overweight and obese adolescents: systematic review of the effects on physical fitness components and cardiovascular risk factors. Sports Med. 2014;44:1139–1152. [DOI] [PubMed] [Google Scholar]
- 7. Dimeo F, Pagonas N, Seibert F, Arndt R, Zidek W, Westhoff TH. Aerobic exercise reduces blood pressure in resistant hypertension. Hypertension. 2012;60:653–658. [DOI] [PubMed] [Google Scholar]
- 8. Kendall KL, Fairman CM. Women and exercise in aging. J Sport Health Sci. 2014;3:170–178. [Google Scholar]
- 9. Guo YC, Qiu PX, Liu TG. Tai Ji Quan: an overview of its history, health benefits, and cultural value. J Sport Health Sci. 2014;3:3–8. [Google Scholar]
- 10. Chan JS, Ho RT, Chung KF, Wang CW, Yao TJ, Ng SM, Chan CL. Qigong exercise alleviates fatigue, anxiety, and depressive symptoms, improves sleep quality, and shortens sleep latency in persons with chronic fatigue syndrome‐like illness. Evid Based Complement Alternat Med. 2014;2014:106048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Cheng FK. Effects of Baduanjin on mental health: a comprehensive review. J Bodyw Mov Ther. 2015;19:138–149. [DOI] [PubMed] [Google Scholar]
- 12. Li FZ, Harmer PA. Tai Ji Quan: from traditional applications to contemporary practice. J Sport Health Sci. 2014;3:1–2. [Google Scholar]
- 13. Stevens JA, Voukelatos A, Ehrenreich H. Preventing falls with Tai Ji Quan: a public health perspective. J Sport Health Sci. 2014;3:21–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hartley L, Flowers N, Lee MS, Ernst E, Rees K. Tai Chi for primary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2014;4:CD010366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Jiang Y, Zou J. Analysis of the TCM theory of traditional Chinese health exercise. J Sport Health Sci. 2013;2:204–208. [Google Scholar]
- 16. Winters‐Stone K. Tai Ji Quan for the aging cancer survivor: mitigating the accelerated development of disability, falls, and cardiovascular disease from cancer treatment. J Sport Health Sci. 2014;3:52–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lan C, Su TC, Chen SY, Lai JS. Effect of T'ai Chi Chuan training on cardiovascular risk factors in dyslipidemic patients. J Altern Complement Med. 2008;14:813–819. [DOI] [PubMed] [Google Scholar]
- 18. Chan CL, Wang CW, Ho RT, Ho AH, Ziea ET, Taam Wong VC, Ng SM. A systematic review of the effectiveness of Qigong exercise in cardiac rehabilitation. Am J Chin Med. 2012;40:255–267. [DOI] [PubMed] [Google Scholar]
- 19. Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA; Cochrane Bias Methods Group; Cochrane Statistical Methods Group . The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions. Hoboken, NJ: Wiley; 2011. [Google Scholar]
- 21. Barrow DE, Bedford A, Ives G, O'Toole L, Channer KS. An evaluation of the effects of Tai Chi Chuan and Chi Kung training in patients with symptomatic heart failure: a randomised controlled pilot study. Postgrad Med J. 2007;83:717–721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Blake H, Batson M. Exercise intervention in brain injury: a pilot randomized study of Tai Chi Qigong. Clin Rehabil. 2009;23:589–598. [DOI] [PubMed] [Google Scholar]
- 23. Cai W. Influence of sitting Baduanjin on quality of life of cerebral apoplexypatients with sequela in community. Chin Nurs Res. 2010;24:2667–2668. [Google Scholar]
- 24. Caminiti G, Volterrani M, Marazzi G, Cerrito A, Massaro R, Arisi A, Franchini A, Sposato B, Rosano G. Tai Chi enhances the effects of endurance training in the rehabilitation of elderly patients with chronic heart failure. Rehabil Res Pract. 2011;2011:761958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Channer KS, Barrow D, Barrow R, Osborne M, Ives G. Changes in haemodynamic parameters following Tai Chi Chuan and aerobic exercise in patients recovering from acute myocardial infarction. Postgrad Med J. 1996;72:349–351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Chen XX, Lv HQ. Effects of Taijiquan exercise on hypertension patients. NO consistency in plasma, the activity of RBC Na+‐ K+ ATPase and Ca2+‐ Mg2+ ATPase. J Beijing Sport Univ. 2006;29:1359–1361. [Google Scholar]
- 27. Chen FZ, Lv QB. Effect of Tai Chi exercise on blood pressure in patients with hypertension. Today Nurse. 2013;4:18–19. [Google Scholar]
- 28. Chen JF. Effect of Tai Chi exercise on blood lipid for elderly patients with coronary heart disease. Guide China Med. 2013;11:583–584. [Google Scholar]
- 29. Cheung BM, Lo JL, Fong DY, Chan MY, Wong SH, Wong VC, Lam KS, Lau CP, Karlberg JP. Randomised controlled trial of Qigong in the treatment of mild essential hypertension. J Hum Hypertens. 2005;19:697–704. [DOI] [PubMed] [Google Scholar]
- 30. Ding FM, Wang JH, Wang XK, Guan MD. Effect of Tai Chi exercise and running for patients with post‐ percutaneous coronary intervention in short term. Chin J Clin Res. 2013;26:126–127. [Google Scholar]
- 31. Gemmell C, Leathem JM. A study investigating the effects of Tai Chi Chuan: individuals with traumatic brain injury compared to controls. Brain Inj. 2006;20:151–156. [DOI] [PubMed] [Google Scholar]
- 32. Hart J, Kanner H, Gilboa‐Mayo R, Haroeh‐Peer O, Rozenthul‐Sorokin N, Eldar R. Tai Chi Chuan practice in community‐dwelling persons after stroke. Int J Rehabil Res. 2004;27:303–304. [DOI] [PubMed] [Google Scholar]
- 33. Lee MS, Choi ES, Chung HT. Effects of Qigong on blood pressure, blood pressure determinants and ventilatory function in middle‐aged patients with essential hypertension. Am J Chin Med. 2003;31:489–497. [DOI] [PubMed] [Google Scholar]
- 34. Lee MS, Kim HJ, Moon SR. Qigong reduced blood pressure and catecholamine levels of patients with essential hypertension. Int J Neurosci. 2003;113:1691–1701. [DOI] [PubMed] [Google Scholar]
- 35. Lee MS, Lee MS, Kim HJ, Choi ES. Effects of Qigong on blood pressure, high‐density lipoprotein cholesterol and other lipid levels in essential hypertension patients. Int J Neurosci. 2004;114:777–786. [DOI] [PubMed] [Google Scholar]
- 36. Li YL, Hu XJ, Cui LN. Clinical observation on sitting Tai Chi exercise used for 30 cases of patients with depression after stroke. Chin Nurs Res. 2012;26:2254–2256. [Google Scholar]
- 37. Lin XL, Chen JW, Zhang GQ, Zhao JY, Tang C. Effects of Baduanjin on quality of life for patients after coronary artery bypass grafting. J Nurs (China). 2012;19:63–67. [Google Scholar]
- 38. Luo H. Effects of Tai Chi exercise and drug for hypertension: a randomized controlled trial. Chin Med Herald. 2006;3:43–44. [Google Scholar]
- 39. Mao HN, Sha P. Effect of Tai Chi exercise on blood pressure, plasma nitrogenmonoxidum and endothelin in hypertensive patients. Chin J Clin Rehabil. 2006;10:65–67. [Google Scholar]
- 40. Ning J, Shen GY, Su JY, Ju SQ, Zhu ZJ. Effect of Tai Chi exercise on ischemia modified albumin for patients with coronary heart disease. Chongqing Med. 2010;39:320–322. [Google Scholar]
- 41. Pan HS, Feng YZ. Clinical observation of Baduanjin exercise for patients with hypertension. J Nanjing Inst Phys Educ (Nat Sci). 2010;9:4–6. [Google Scholar]
- 42. Sato S, Makita S, Uchida R, Ishihara S, Masuda M. Effect of Tai Chi training on baroreflex sensitivity and heart rate variability in patients with coronary heart disease. Int Heart J. 2010;51:238–241. [DOI] [PubMed] [Google Scholar]
- 43. Taylor‐Piliae RE, Coull BM. Community‐based Yang‐style Tai Chi is safe and feasible in chronic stroke: a pilot study. Clin Rehabil. 2012;26:121–131. [DOI] [PubMed] [Google Scholar]
- 44. Tsai JC, Wang WH, Chan P, Lin LJ, Wang CH, Tomlinson B, Hsieh MH, Yang HY, Liu JC. The beneficial effects of Tai Chi Chuan on blood pressure and lipid profile and anxiety status in a randomized controlled trial. J Altern Complement Med. 2003;9:747–754. [DOI] [PubMed] [Google Scholar]
- 45. Wang CX, Xu DH, Qian YS, Zhao GS, Kuang AF. Effects of Qigong on high‐density lipoprotein cholesterol for patients with hypertensiona randomized controlled trial. Chin J Integr Med. 1989;9:514–516. [Google Scholar]
- 46. Wang W, Sawada M, Noriyama Y, Arita K, Ota T, Sadamatsu M, Kiyotou R, Hirai M, Kishimoto T. Tai Chi exercise versus rehabilitation for the elderly with cerebral vascular disorder: a single‐blinded randomized controlled trial. Psychogeriatrics. 2010;10:160–166. [DOI] [PubMed] [Google Scholar]
- 47. Wang L, Zhou QA, Xu JG, Yang LJ, Yang B, Du HX. Effects of Tai Chi exercise on depression in patients with stroke. China Community Physicians. 2012;14:222. [Google Scholar]
- 48. Wang XK, Zhang XL, Ding FM, Jiang WQ. Effects of Tai Chi exercise on quality of life and NT‐proBNP in patients with STEMI. Guide China Med. 2013;11:659–661. [Google Scholar]
- 49. Yao CD, Li F, Ma YB. Effects of shadow boxing on rehabilitation in patients with chronic heart failure. Chin J Cardiovasc Rehabil Med. 2010;19:364–367. [Google Scholar]
- 50. Yeh GY, Wood MJ, Lorell BH, Stevenson LW, Eisenberg DM, Wayne PM, Goldberger AL, Davis RB, Phillips RS. Effects of Tai Chi mind‐body movement therapy on functional status and exercise capacity in patients with chronic heart failure: a randomized controlled trial. Am J Med. 2004;117:541–548. [DOI] [PubMed] [Google Scholar]
- 51. Yeh GY, Mietus JE, Peng CK, Phillips RS, Davis RB, Wayne PM, Goldberger AL, Thomas RJ. Enhancement of sleep stability with Tai Chi exercise in chronic heart failure: preliminary findings using an ECG‐based spectrogram method. Sleep Med. 2008;9:527–536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Yeh GY, McCarthy EP, Wayne PM, Stevenson LW, Wood MJ, Forman D, Davis RB, Phillips RS. Tai Chi exercise in patients with chronic heart failure: a randomized clinical trial. Arch Intern Med. 2011;171:750–757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Yeh GY, Wood MJ, Wayne PM, Quilty MT, Stevenson LW, Davis RB, Phillips RS, Forman DE. Tai Chi in patients with heart failure with preserved ejection fraction. Congest Heart Fail. 2013;19:77–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Yu HL. Clinical observation of Baduanjin exercise used for 104 cases of hypertension patients with obesity. Chin J Clin. 2013;41:47–48. [Google Scholar]
- 55. Zhang JF, Ai J. Effects of Baduanjin and drug therapy on quality of life in elderly patients with hypertension. Chin J Trauma Disabil Med. 2013;21:179–180. [Google Scholar]
- 56. Yeh GY, Wang C, Wayne PM, Phillips R. Tai Chi exercise for patients with cardiovascular conditions and risk factors: a systematic review. J Cardiopulm Rehabil Prev. 2009;29:152–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Dalusung‐Angosta A. The impact of Tai Chi exercise on coronary heart disease: a systematic review. J Am Acad Nurse Pract. 2011;23:376–381. [DOI] [PubMed] [Google Scholar]
- 58. Ding M. Tai Chi for stroke rehabilitation: a focused review. Am J Phys Med Rehabil. 2012;91:1091–1096. [DOI] [PubMed] [Google Scholar]
- 59. Law MR, Morris JK, Wald NJ. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: meta‐analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ. 2009;338:b1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Wald NJ, Law MR. A strategy to reduce cardiovascular disease by more than 80%. BMJ. 2003;326:1419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Jahnke R, Larkey L, Rogers C, Etnier J, Lin F. A comprehensive review of health benefits of Qigong and Tai Chi. Am J Health Promot. 2010;24:e1–e25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. CONSORT GROUP (Consolidated Standards of Reporting Trials) . The CONSORT statement: revised recommendations for improving the quality of reports of parallel‐group randomized trials. Ann Intern Med. 2001;134:657–662. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1. Search strategies for all databases.


