Abstract
Background
Hyponatremia predicts poor prognosis in patients with acute heart failure (AHF). However, the association of the severity of hyponatremia and changes of serum sodium levels with long‐term outcome has not been delineated.
Methods and Results
The study population was drawn from the HARVEST registry (Heart Failure Registry of Taipei Veterans General Hospital), so that patients hospitalized for acute heart failure (AHF) composed this study. The National Death Registry was linked to identify the clinical outcomes of all‐cause mortality and cardiovascular death, with a follow‐up duration of up to 4 years. Among a total of 2556 patients (76.4 years of age, 67% men), 360 had on‐admission hyponatremia, defined as a serum sodium level of <135 mEq/L on the first day of hospitalization. On‐admission hyponatremia was a predictor for all‐cause mortality (hazard ratio and 95% CI: 1.43, 1.11–1.83) and cardiovascular mortality (1.50, 1.04–2.17), independent of age, sex, hematocrit, estimated glomerular filtration rate, left ventricular ejection fraction, and prescribed medications. Subjects with severe hyponatremia (<125 mEq/L) would even have worse clinical outcomes. During hospitalization, a drop of sodium levels of >3 mEq/L was associated with a marked increase of mortality than those with minimal or no drop of sodium levels. In addition, subjects with on‐admission hyponatremia and drops of serum sodium levels during hospitalization had an incremental risk of death (2.26, 1.36–3.74), relative to those with normonatremia at admission and no treatment‐related drop of serum sodium level in the fully adjusted model.
Conclusions
On‐admission hyponatremia is an independent predictor for long‐term outcomes in patients hospitalized for AHF. Combined the on‐admission hyponatremia with drops of serum sodium levels during hospitalization may make a better risk assessment in AHF patients.
Keywords: acute heart failure, hyponatremia, mortality
Subject Categories: Biomarkers, Heart Failure
Introduction
Hyponatremia, defined as a serum sodium level of less than 135 mEq/L, is one of the major electrolyte disorders in acute hospitalized patients,1 and its prevalence in patients with acute heart failure (AHF) could be as high as 25%.2, 3, 4 It is believed that hyponatremia in AHF is usually a problem of impaired water excretion rather than sodium depletion, attributed mainly to the increase of nonosmotic release of arginine vasopressin (AVP).5 Previous studies have demonstrated the prognostic impacts of on‐admission serum sodium levels in patients hospitalized for AHF.6, 7, 8, 9 A lower serum sodium level in AHF may indicate poor water excretion attributed to cardiorenal insufficiency, which was therefore related to a worse clinical outcome. In contrast, the prognostic value of the changes of sodium levels in AHF patients during hospitalization has been less clear. For example, treatment of hyponatremia in AHF patients with the vasopressin antagonist in the EVEREST study showed an improvement in serum sodium levels and heart failure signs and symptoms, but not clinical outcomes.10 In addition, in observational studies, the changes of serum sodium levels during hospitalization for AHF were not a predictor of long‐term survival, whereas on‐admission hyponatremia indeed was related to their prognoses.11, 12 These results may suggest that hyponatremia is a marker of more‐severe disease, but not a treatment target in AHF.
In contrast, other studies showed that hospital‐acquired hyponatremia was a risk factor for increasing mortality in AHF. A correction of hyponatremia during hospitalization was associated with less subsequent mortality and heart failure readmission.13 In the subgroup of patients with a serum sodium level of <130 mEq/L, rather than 130 to 135 mEq/L, in the EVEREST study, tolvaptan indeed improved cardiovascular mortality and morbidity.14 Therefore, the study aims are to evaluate the survival impacts of on‐admission hyponatremia and treatment‐related changes of serum sodium levels within the hospitalizations for AHF.
Methods
Study Population and Data Collection
The study population was drawn from the HARVEST registry (Heart Failure Registry of Taipei Veterans General Hospital) where patients presented with new or exacerbated symptoms and signs of heart failure, fulfilled with the Framingham criteria, were eligible.15 From October 2003 to December 2012, a total of 2663 patients were admitted primarily for AHF. Patients with acute coronary syndrome, severe hepatic disease, or severe infection have been excluded. Subjects with complete data of on‐admission serum sodium, creatinine and hemoglobin levels, at‐discharge sodium levels, and echocardiographic examinations were eligible for the present analysis. Among them, 107 patients were excluded because of either missing data of sodium levels on admission or loss of follow‐up. Medical history, findings of physical examinations, biochemical tests, and prescriptions were prospectively logged in a Web‐based electronic medical recording system. Subjects who were enrolled in this registry gave informed consent. The investigation conformed to the principles outlined in the Declaration of Helsinki, and the institutional review board of Taipei Veterans General Hospital (Taipei, Taiwan) approved the study.
Left ventricular ejection fraction (LVEF) was measured by M‐mode quantification method in accord with the recommendations of the American Society of Echocardiography,16 as well as the ratio of transmitral flow velocity to mitral annulus motion velocity in early diastole (E/e’). Subjects with LVEF of <50% were referred to have reduced LVEF. N‐terminal pro‐brain natriuretic peptide (NT‐proBNP) was available in patients hospitalized in 2009 and after. Estimated glomerular filtration rate (eGFR) was calculated by a modified modification of diet in renal disease equation based on the Chinese population.17
Definition of Hyponatremia
Hyponatremia was defined as a serum sodium level of <135 mEq/L, whereas severe hyponatremia was referred to a sodium level of <125 mEq/L.18, 19 Changes of sodium levels were available in 2528 subjects and calculated as the difference between the sodium levels at discharge and on admission, which was further stratified into 3 categories: no drop of sodium levels; drop of sodium levels ≤3 mEq/L; and drop of sodium levels >3 mEq/L during hospitalization.
Follow‐up
Mortality statistics for the study populations were obtained by linking our database to the National Death Registry (NDR) with a follow‐up duration of up to 4 years. The NDR database registers valid information according to the International Classification of Disease, Ninth Revision (ICD‐9). The ICD‐9 codes for cardiovascular death were 390 to 459.20
Statistical Analysis
Means, SDs, and percentages were used to describe the characteristics of the study population, compared by using Student t test and chi‐square test. The prognostic difference between patients with normonatremia, hyponatremia, and severe hyponatremia were analyzed by Kaplan–Meier survival analysis and pair‐wise comparisons. Cox proportional hazards models were used to identify the predictors of all‐cause or cardiovascular mortality with adjustments for age, sex, renal function, hematocrit, LVEF, and the prescribed medications. The joint effect of on‐admission serum sodium levels and treatment‐related changes of sodium levels was evaluated by stratifying the study population into 4 subgroups according to the presence or absence of hyponatremia on admission and drop of sodium levels during hospitalization. A P value of <0.05 was considered statistically significant. Analyses were performed using the statistical package SPSS (version 18.0; SPSS, Inc., Chicago, IL)
Results
A total of 2556 patients (76.4±12.9 years; 1725 [67%] men; 1020 [40%] systolic heart failure) were enrolled in this study, and 360 subjects (14%) among them had hyponatremia on admission. Baseline characteristics of the patients with or without hyponatremia were described in Table 1. Patients with hyponatremia were older and more likely to have hypertension, diabetes, and stroke. Sex distribution and presence of coronary artery disease were not significantly different between groups. LVEF was similar in both groups, but patients with hyponatremia had higher E/e’. In addition, hemoglobin levels and hematocrit were lower, and NT‐proBNP levels were higher in patients with hyponatremia. Renal function and glucose levels were not different. Patients with hyponatremia had lower serum sodium levels, both on admission and at discharge, than patients with normonatremia. There was an increase in sodium levels during hospitalization in hyponatremic patients, but a decrease in those without hyponatremia on admission. Hyponatremic patients were less often prescribed with β‐blockers, renin‐angiotensin system (RAS) blockades, and spironolactone than normonatremic patients.
Table 1.
Baseline Characteristics of the Study Population With or Without On‐Admission Hyponatremia
| Normonatremia (n=2196) | Hyponatremia (n=360) | P Valuea | |
|---|---|---|---|
| Age, y | 76.13±12.95 | 78.04±12.24 | 0.009 |
| Male sex, n (%) | 1496 (68.1) | 229 (63.6) | 0.102 |
| Comorbidity | |||
| Hypertension, n (%) | 1355 (61.7) | 200 (55.6) | 0.032 |
| Diabetes mellitus, n (%) | 806 (36.7) | 159 (44.2) | 0.008 |
| Coronary artery disease, n (%) | 669 (30.5) | 91 (25.3) | 0.054 |
| Stroke, n (%) | 163 (7.4) | 44 (12.2) | 0.003 |
| Echocardiography | |||
| LVEF, % | 54.08±20.17 | 54.83±22.05 | 0.516 |
| E/e’ | 17.70±7.80 | 19.15±8.98 | 0.035 |
| Blood examination | |||
| Hemoglobin, mg/dL | 11.85±2.26 | 11.34±2.16 | <0.001 |
| Hematocrit, % | 35.69±6.83 | 33.63±7.02 | 0.001 |
| Glucose, mg/dL | 167.53±89.49 | 177.08±100.77 | 0.306 |
| eGFR, mL/min | 52.71±29.17 | 53.04±34.61 | 0.867 |
| NT‐proBNPb, pg/mL (n=961) | 5218.68±3.90 | 6768.26±4.01 | 0.031 |
| Serum sodium levels | |||
| On admission, mEq/L | 140.11±3.21 | 130.67±4.23 | <0.001 |
| At discharge, mEq/L | 138.57±4.10 | 133.85±5.12 | <0.001 |
| Changes, mEq/L | −1.72±4.25 | 3.56±6.23 | <0.001 |
| Medications at discharge | |||
| Beta‐blocker, n (%) | 1434 (65.3) | 201 (55.8) | 0.001 |
| RAS blockade, n (%) | 1871 (87.2) | 275 (76.4) | <0.001 |
| Spironolactone, n (%) | 1298 (59.1) | 183 (50.8) | 0.004 |
| Diuretics, n (%) | 1804 (82.6) | 262 (73.2) | <0.001 |
E/e’ indicates ration of early diastolic mitral flow velocity to the early diastolic mitral septal annulus motion velocity; eGFR, estimated glomerular filtration rate; LVEF, left ventricle ejection fraction; NT‐proBNP, N‐terminal pro‐brain natriuretic peptide; RAS blockade, angiotensin‐converting enzyme inhibitor and angiotensin II receptor blocker.
Continuous and categorical variables were compared by using Student t test and chi‐square test, respectively.
Geometric means and SDs.
Hyponatremia and Clinical Outcomes
Comparing to patients with normal serum sodium levels, patients with on‐admission hyponatremia had higher in‐hospital, 90‐day, and 4‐year mortality rate (Figure 1). Subjects with severe hyponatremia had the worst clinical outcomes, in contrast to those with mild hyponatremia or normonatremia (Figure 2). Hyponatremia was a significant predictor of cardiovascular mortality (hazard ratio [HR] and 95% CI: 1.76; 1.39–2.23) as well as total mortality (1.64; 1.40–1.93; Table 2, model 1). Hyponatremia was an independent predictor of cardiovascular (1.71; 1.350–2.16) and total mortality (1.57; 1.34–1.85) after accounting for age and sex (Table 2, model 2). With further adjustments for hematocrit, eGFR, LVEF, use of β‐blockers, RAS blockade, spironolactone, and even NT‐proBNP level, hyponatremia remained independently associated with clinical outcomes (Table 2, model 3 and 4). In addition, severity of hyponatremia correlated with increased risks of mortality in uni‐ and multivariate Cox proportional hazard model (Table 3).
Figure 1.
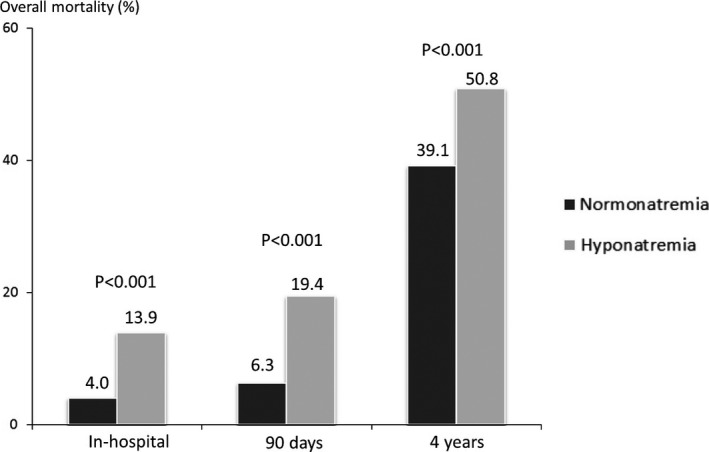
In‐hospital, 90‐day, and 4‐year mortality cumulative in patients with and without on‐admission hyponatremia.
Figure 2.
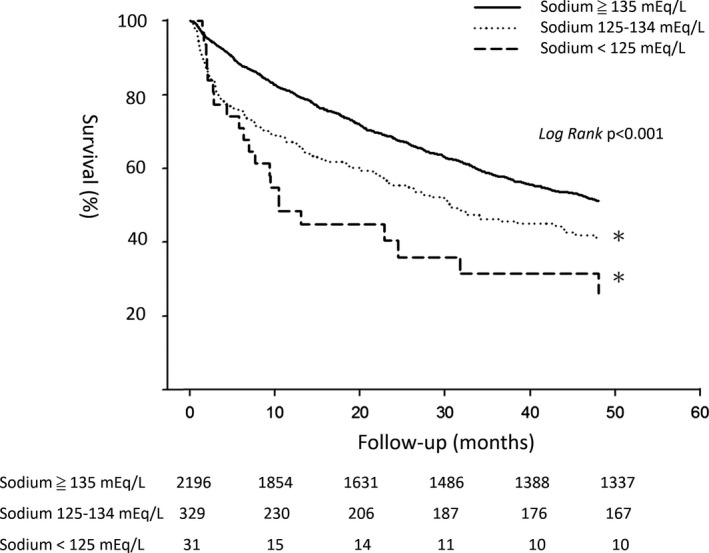
Kaplan–Meier survival curve analysis in patients with an on‐admission serum sodium level of ≥135, <135 and ≥125, and <125 mEq/L. *Significant difference (P<0.001), comparing to subjects with serum sodium levels of ≥135 mEq/L. The χ2 values of the pair‐wise comparisons were 18.67 and 28.15 for a sodium level of 125 to 134 and <125 mEq/L, respectively.
Table 2.
Relative Risks for Cardiovascular Death and Total Mortality During the 4 Year Follow‐up by On‐Admission Serum Sodium Levels
| Cardiovascular Mortality | Total Mortality | |||
|---|---|---|---|---|
| HR (95% CI) | P Value | HR (95% CI) | P Value | |
| Per 5‐mEq/L decrease in Na | ||||
| Model 1 | 1.14 (1.04–1.25) | 0.007 | 1.12 (1.05–1.20) | 0.001 |
| Model 2 | 1.13 (1.03–1.24) | 0.012 | 1.10 (1.04–1.18) | 0.002 |
| Model 3 | 1.14 (0.99–1.31) | 0.072 | 1.09 (0.99–1.20) | 0.071 |
| Model 4 | 2.01 (1.34–3.01) | 0.001 | 1.41 (1.08–1.86) | 0.013 |
| Hyponatremia | ||||
| Model 1 | 1.76 (1.39–2.23) | <0.001 | 1.64 (1.40–1.93) | <0.001 |
| Model 2 | 1.71 (1.35–2.16) | <0.001 | 1.57 (1.34–1.85) | <0.001 |
| Model 3 | 1.50 (1.04–2.17) | 0.032 | 1.43 (1.11–1.83) | 0.005 |
| Model 4 | 4.46 (1.67–11.88) | 0.003 | 2.83 (1.46–5.47) | 0.002 |
Model 1: crude ratio; model 2: adjust for age and sex; model 3: adjust for age, sex, hematocrit, estimated glomerular filtration rate, LVEF, use of beta‐blocker, renin angiotensin system blockade, and spironolactone; Model 4: Model 3+N‐terminal pro‐brain natriuretic peptide (n=961). CI indicates confidence interval; HR, hazard ratio.
Table 3.
Relative Risk for Mortality During the 4‐Year Follow‐Up, Stratified by the Severity of On‐Admission Hyponatremia
| On‐Admission Sodium Levels | Cases/Deaths | Model 1 | Model 2 | Model 3 | Model 4 |
|---|---|---|---|---|---|
| HR (95% CI) | HR (95% CI) | HR (95% CI) | HR (95% CI) | ||
| ≥135 mEq/L | 2196/859 | 1 | 1 | 1 | 1 |
| 125 to 134 mEq/L | 329/162 | 1.58 (1.33–1.87) | 1.52 (1.28–1.80) | 1.28 (0.98–1.67) | 2.64 (1.33–5.27) |
| <125 mEq/L | 31/21 | 2.48 (1.61–3.82) | 2.11 (1.37–3.27) | 3.68 (2.04–6.64) | 5.13 (1.15–22.83) |
Model 1: crude ratio; Model 2: adjust for age and sex; Model 3: adjust for age, sex, hematocrit, estimated glomerular filtration rate, left ventricle ejection fraction, use of beta‐blocker, renin angiotensin system blockade, and spironolactone; model 4: model 3+NT‐proBNP (n=947).
In the subgroup analyses, hyponatremia was consistently associated with higher risks for all‐cause mortality in various subpopulations after accounting for age, regardless of age > or ≤75 years, men or women, reduced or preserved LVEF, and with or without chronic renal disease (Figure 3). There was only a significant interaction between age and on‐admission hyponatremia (P=0.030). Furthermore, a drop of sodium levels during hospitalization was also an independent risk factor across all subgroups (Figure 3).
Figure 3.
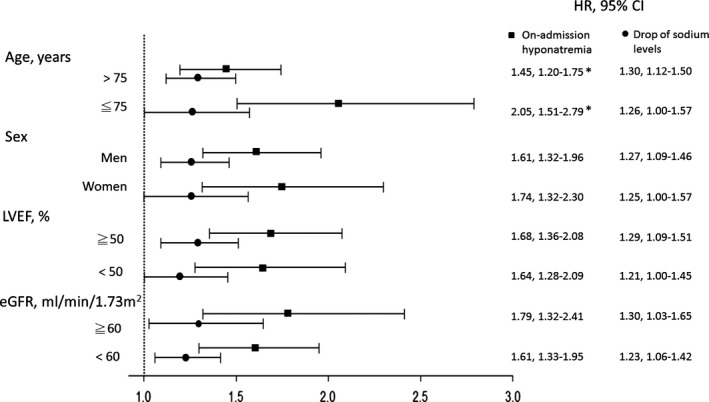
Hazard ratios (HRs) and 95% CI for mortality of on‐admission hyponatremia and any drop of serum sodium levels during hospitalization in subgroup analyses, after accounting for age. *Significant interaction with P<0.05. eGFR indicates estimated glomerular filtration rate; LVEF, left ventricular ejection fraction.
Treatment‐Related Changes of Serum Sodium Levels and Clinical Outcomes
On‐admission hyponatremia in combination with a drop of serum sodium levels during hospitalization was associated with a higher mortality rate in this study population, demonstrated by Kaplan–Meier survival curve analysis (Figure 4). Such incremental effects were also presented in patients with either preserved or reduced LVEF (Figure 4). Combined on‐admission hyponatremia and drops of sodium levels was also significantly associated with higher mortality rate than either alone in Cox proportional hazards models (Table 4, Model 1). The joint effect of on‐admission hyponatremia and drops of sodium levels remained significant when age, sex, hematocrit, eGFR, LVEF, prescribed medications, and even NT‐proBNP were accounted for (Table 4, models 2–4). In patients with on‐admission hyponatremia, a drop of sodium levels of >3 mEq/L was associated with a marked increase in mortality than those with a drop of ≤3 mEq/L or no drop of sodium levels (Figure 5). In patients without hyponatremia on admission, mortality was also increased with severity of drops of sodium levels during hospitalization (Figure 5).
Figure 4.

Kaplan–Meier survival curve analysis in total study population (A) and in subjects with preserved ejection fraction (HFpEF; B) or reduced ejection fraction (HFrEF; C), stratified by on‐admission serum sodium level and change of serum sodium level during hospitalization. Group 1=normonatremia on admission without any drop of serum sodium level during hospitalization; group 2=normonatremia on admission with a drop of serum sodium level during hospitalization; group 3=hyponatremia on admission without any drop of serum sodium level during hospitalization; group 4=hyponatremia on admission with a drop of serum sodium level during hospitalization.
Table 4.
Relative Risk for Mortality During the 4‐Year Follow‐up Stratified by On‐Admission Serum Sodium Level and Change of Serum Sodium Level During Hospitalization
| Group | Cases/Deaths | Model 1 | Model 2 | Model 3 | Model 4 |
|---|---|---|---|---|---|
| HR (95% CI) | HR (95% CI) | HR (95% CI) | HR (95% CI) | ||
| 1 | 608/233 | 1 | 1 | 1 | 1 |
| 2 | 987/443 | 1.21 (1.03–1.42) | 1.24 (1.06–1.45) | 1.32 (1.07–1.62) | 0.94 (0.48–1.84) |
| 3 | 221/110 | 1.55 (1.24–1.95) | 1.51 (1.20–1.89) | 1.55 (1.15–2.10) | 2.31 (1.02–5.22) |
| 4 | 64/38 | 2.45 (1.72–3.48) | 2.49 (1.97–3.54) | 2.26 (1.36–3.74) | 7.79 (2.29–26.56) |
Model 1: crude ratio; model 2: adjust for age and sex; model 3: adjust for age, sex, hematocrit, estimated glomerular filtration rate, left ventricle ejection fraction, use of beta‐blocker, renin angiotensin system blockade, and spironolactone; model 4: model 3+NT‐proBNP (n=947); group 1=normonatremia on admission without any drop of serum sodium level during hospitalization; group 2=normonatremia on admission with a drop of serum sodium level during hospitalization; group 3=hyponatremia on admission without any drop of serum sodium level during hospitalization; group 4=hyponatremia on admission with a drop of serum sodium level during hospitalization.
Figure 5.
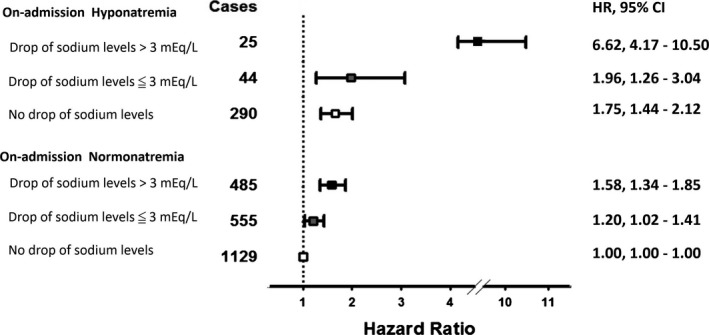
Hazard ratios (HRs) and 95% CIs for the changes of serum sodium levels of no drop, a drop of ≦3 mEq/L, and a drop of >3 mEq/L during hospitalization, stratified by on‐admission sodium levels.
Discussion
In the present investigation, we reconfirmed that on‐admission hyponatremia in AHF patients was associated with an increase in short‐ and long‐term mortality.21, 22 A dose‐response relationship between severity of hyponatremia and clinical outcomes was also observed. In addition, changes of serum sodium levels during hospitalization for AHF would exert an incremental prognostic impact on top of on‐admission sodium levels.
Hyponatremia and Clinical Outcomes in AHF
Hyponatremia is a common disorder in patients with either acute or chronic heart failure, caused mainly by impaired water excretion instead of sodium depletion. The underlying pathophysiology may involve an increase of nonosmotic release of AVP attributed to baroreceptor activation and decreased distal renal tubular flow attributed to compromised glomerular filtration.23 The question in need of an answer is whether hyponatremia is an active contributor to poor outcomes in heart failure or whether it is simply associated with poor outcomes, because it tends to occur in patients with more‐advanced disease. Although the EVEREST study presented a disappointing result that improving serum sodium levels did not correspond to better clinical outcomes,10 the post‐hoc analysis indeed suggested that a correction of severe hyponatremia was beneficial. In this study, we demonstrated that the more severe the hyponatremia, the more poor the outcome. This may support that patients with severe hyponatremia would be more likely to get benefits by correcting serum sodium levels.
Prognostic Impact of Serum Sodium‐Level Change During Hospitalization
In contrast to the EVEREST study, the ACTIV trial has shown favorable short‐term survival at 60 days in hyponatremic patients who experienced improvements of serum sodium levels during hospitalization.2 However, only 21.6% of the study population was selected for this post‐hoc analysis, giving the selection bias as a major confounder. In the Korea AHF registry of 2888 subjects, treatment‐related changes of serum sodium levels during hospitalization did not correlate with clinical outcomes. Among the 19.9% of the study population that presented with hyponatremia at admission, the comparisons between those with persistent hyponatremia and improved hyponatremia showed no significant difference, as well.11 In another observational study of 322 AHF patients with hyponatremia at admission, Madan et al. showed that changes of sodium levels within 60 to 270 days were a strong predictor of long‐term survival.12 However, the treatment‐related change of sodium levels during hospitalization was not a predictor of mortality during a median follow‐up duration of 20 months.12 In contrast, Konishi et al. suggested that new‐onset hyponatremia during hospitalization for AHF in patients who were normonatremic at admission was related to an increase in 1‐year death and cardiac events.24 In the present study, with a longer follow‐up duration, we clearly demonstrated that treatment‐related changes of sodium levels were an independent risk for long‐term mortality in AHF patients presenting with hyponatremia or normonatremia. Fluctuations of sodium levels during hospitalization had a prognostic impact on top of the on‐admission sodium levels in both patients with preserved or reduced LVEF.
Subgroup Analyses
Whereas renal function is a major determinant of serum sodium levels in AHF,25 Lee et al. clarified a significant interaction between blood urea nitrogen (BUN) and improved hyponatremia.11 However, improved hyponatremia was related to better outcomes only in subjects with elevated BUN. Because elevated BUN is a complex indicator related to impaired left ventricular function, poor renal function, inadequate kidney perfusion, hypovolemia, hyperprotein diet, and even gastrointestinal bleeding, the interaction between renal function and hyponatremia remains a controversy. In this study, we illustrated that both on‐admission hyponatremia and drop of sodium levels during hospitalization consistently correlated with worse long‐term outcomes both in the elderly and the young, in men and women, in patients with reduced or preserved LVEF, and in patients with preserved or impaired renal function. In addition, there was a trend that hyponatremia carried a higher risk in the elderly than in the young.
Study Limitations
There were several limitations in the present study. First, this was a single‐center registry and the mean age of the study population was 76.4 years, which might be the oldest population among the publish data.11, 24, 26 Because the in‐hospital mortality of the study population was 3.9%, which was the same as other studies,11, 27 the disease severity and quality of care were supposed to be equal to other study populations. Given a more prominently prognostic impact of sodium‐level changes compared to other studies, the study might support hyponatremia in AHF as a more relevant issue in the elderly. Second, we were not able to demonstrate the fluctuations of individual fluid status, which might confound the prognostic impacts of sodium levels. However, we have adjusted all the observed confounders to show the independently prognostic values of sodium levels. Third, NT‐proBNP was only available in 37.6% of the study population. In this subset of 961 patients with available NT‐proBNP data, there were 266 mortalities. We therefore still had sufficient power to demonstrate the prognostic value of sodium levels independent of NT‐proBNP. Fourth, 103 patients were excluded because of missing data of on‐admission sodium levels; however, their 4‐year mortality rate (39%) was not different from this study population. Given the selection bias a major confounder of an observational study, the study results should be carefully interpreted. Last, the study only analyzed the mortality endpoint. Further work is needed to address the risks of hyponatremia for morbidities, such as heart failure rehospitalization, in patients with AHF.
Conclusions
On‐admission hyponatremia was an independent predictor for short‐ and long‐term mortality in patients hospitalized for AHF. In addition, the treatment‐related changes of sodium levels were also correlated with the clinical outcomes in patients with either reduced or preserved LVEF and in patients with or without chronic kidney disease. Combining on‐admission hyponatremia with changes of sodium levels during hospitalization may further improve the risk classification for AHF patients.
Sources of Funding
The study was supported by Taipei Veterans General Hospital (V100C‐145, V101C‐092, V102C‐119, and V103B‐017), and Ministry of Health and Welfare, Taiwan grant (MOHW‐104‐TDU‐B‐211‐113003, MOHW‐104‐TDU‐B‐211‐113017), and the death registry.
Disclosures
None.
(J Am Heart Assoc. 2016;5:e002668 doi: 10.1161/JAHA.115.002668)
References
- 1. Mohan S, Gu S, Parikh A, Radhakrishnan J. Prevalence of hyponatremia and association with mortality: results from NHANES. Am J Med. 2013;126:1127–1137.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Rossi J, Bayram M, Udelson JE, Lloyd‐Jones D, Adams KF, Oconnor CM, Stough WG, Ouyang J, Shin DD, Orlandi C, Gheorghiade M. Improvement in hyponatremia during hospitalization for worsening heart failure is associated with improved outcomes: insights from the Acute and Chronic Therapeutic Impact of a Vasopressin Antagonist in Chronic Heart Failure (ACTIV in CHF) trial. Acute Card Care. 2007;9:82–86. [DOI] [PubMed] [Google Scholar]
- 3. Gheorghiade M, Abraham WT, Albert NM, Gattis Stough W, Greenberg BH, O'Connor CM, She L, Yancy CW, Young J, Fonarow GC; OPTIMIZE‐HF Investigators and Coordinators . Relationship between admission serum sodium concentration and clinical outcomes in patients hospitalized for heart failure: an analysis from the OPTIMIZE‐HF registry. Eur Heart J. 2007;28:980–988. [DOI] [PubMed] [Google Scholar]
- 4. Gheorghiade M, Rossi JS, Cotts W, Shin DD, Hellkamp AS, Pina IL, Fonarow GC, DeMarco T, Pauly DF, Rogers J, DiSalvo TG, Butler J, Hare JM, Francis GS, Stough WG, O'Connor CM. Characterization and prognostic value of persistent hyponatremia in patients with severe heart failure in the ESCAPE Trial. Arch Intern Med. 2007;167:1998–2005. [DOI] [PubMed] [Google Scholar]
- 5. Oren RM. Hyponatremia in congestive heart failure. Am J Cardiol. 2005;95:2B–7B. [DOI] [PubMed] [Google Scholar]
- 6. Felker GM, Leimberger JD, Califf RM, Cuffe MS, Massie BM, Adams KF Jr, Gheorghiade M, O'Connor CM. Risk stratification after hospitalization for decompensated heart failure. J Card Fail. 2004;10:460–466. [DOI] [PubMed] [Google Scholar]
- 7. Lee DS, Austin PC, Rouleau JL, Liu PP, Naimark D, Tu JV. Predicting mortality among patients hospitalized for heart failure: derivation and validation of a clinical model. JAMA. 2003;290:2581–2587. [DOI] [PubMed] [Google Scholar]
- 8. Rusinaru D, Tribouilloy C, Berry C, Richards AM, Whalley GA, Earle N, Poppe KK, Guazzi M, Macin SM, Komajda M, Doughty RN; MAGGIC Investigators . Relationship of serum sodium concentration to mortality in a wide spectrum of heart failure patients with preserved and with reduced ejection fraction: an individual patient data meta‐analysis(dagger): Meta‐Analysis Global Group in Chronic heart failure (MAGGIC). Eur J Heart Fail. 2012;14:1139–1146. [DOI] [PubMed] [Google Scholar]
- 9. Klein L, O'Connor CM, Leimberger JD, Gattis‐Stough W, Pina IL, Felker GM, Adams KF Jr, Califf RM, Gheorghiade M; OPTIME‐CHF Investigators . Lower serum sodium is associated with increased short‐term mortality in hospitalized patients with worsening heart failure: results from the Outcomes of a Prospective Trial of Intravenous Milrinone for Exacerbations of Chronic Heart Failure (OPTIME‐CHF) study. Circulation. 2005;111:2454–2460. [DOI] [PubMed] [Google Scholar]
- 10. Gheorghiade M, Konstam MA, Burnett JC Jr, Grinfeld L, Maggioni AP, Swedberg K, Udelson JE, Zannad F, Cook T, Ouyang J, Zimmer C, Orlandi C; Efficacy of Vasopressin Antagonism in Heart Failure Outcome Study With Tolvaptan (EVEREST) Investigators . Short‐term clinical effects of tolvaptan, an oral vasopressin antagonist, in patients hospitalized for heart failure: the EVEREST Clinical Status Trials. JAMA. 2007;297:1332–1343. [DOI] [PubMed] [Google Scholar]
- 11. Lee SE, Choi DJ, Yoon CH, Oh IY, Jeon ES, Kim JJ, Cho MC, Chae SC, Ryu KH, Oh BH; KorHF Registry . Improvement of hyponatraemia during hospitalisation for acute heart failure is not associated with improvement of prognosis: an analysis from the Korean Heart Failure (KorHF) registry. Heart. 2012;98:1798–1804. [DOI] [PubMed] [Google Scholar]
- 12. Madan VD, Novak E, Rich MW. Impact of change in serum sodium concentration on mortality in patients hospitalized with heart failure and hyponatremia. Circ Heart Fail. 2011;4:637–643. [DOI] [PubMed] [Google Scholar]
- 13. Goldsmith SR. Hyponatremia in heart failure: time for a trial. J Card Fail. 2013;19:398–400. [DOI] [PubMed] [Google Scholar]
- 14. Hauptman PJ, Burnett J, Gheorghiade M, Grinfeld L, Konstam MA, Kostic D, Krasa HB, Maggioni A, Ouyang J, Swedberg K, Zannad F, Zimmer C, Udelson JE; Everest Investigators . Clinical course of patients with hyponatremia and decompensated systolic heart failure and the effect of vasopressin receptor antagonism with tolvaptan. J Card Fail. 2013;19:390–397. [DOI] [PubMed] [Google Scholar]
- 15. Ho KK, Anderson KM, Kannel WB, Grossman W, Levy D. Survival after the onset of congestive heart failure in Framingham Heart Study subjects. Circulation. 1993;88:107–115. [DOI] [PubMed] [Google Scholar]
- 16. Sahn DJ, DeMaria A, Kisslo J, Weyman A. Recommendations regarding quantitation in M‐mode echocardiography: results of a survey of echocardiographic measurements. Circulation. 1978;58:1072–1083. [DOI] [PubMed] [Google Scholar]
- 17. Ma YC, Zuo L, Chen JH, Luo Q, Yu XQ, Li Y, Xu JS, Huang SM, Wang LN, Huang W, Wang M, Xu GB, Wang HY. Modified glomerular filtration rate estimating equation for Chinese patients with chronic kidney disease. J Am Soc Nephrol. 2006;17:2937–2944. [DOI] [PubMed] [Google Scholar]
- 18. Gill G, Huda B, Boyd A, Skagen K, Wile D, Watson I, van Heyningen C. Characteristics and mortality of severe hyponatraemia—a hospital‐based study. Clin Endocrinol (Oxf). 2006;65:246–249. [DOI] [PubMed] [Google Scholar]
- 19. Shapiro DS, Sonnenblick M, Galperin I, Melkonyan L, Munter G. Severe hyponatraemia in elderly hospitalized patients: prevalence, aetiology and outcome. Intern Med J. 2010;40:574–580. [DOI] [PubMed] [Google Scholar]
- 20. Sung SH, Cheng HM, Wang KL, Yu WC, Chuang SY, Ting CT, Lakatta EG, Yin FC, Chou P, Chen CH. White coat hypertension is more risky than prehypertension: important role of arterial wave reflections. Hypertension. 2013;61:1346–1353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Cleland JG, McDonagh T, Rigby AS, Yassin A, Whittaker T, Dargie HJ; National Heart Failure Audit Team for England and Wales . The national heart failure audit for England and Wales 2008–2009. Heart. 2011;97:876–986. [DOI] [PubMed] [Google Scholar]
- 22. Cowie MR, Fox KF, Wood DA, Metcalfe C, Thompson SG, Coats AJ, Poole‐Wilson PA, Sutton GC. Hospitalization of patients with heart failure: a population‐based study. Eur Heart J. 2002;23:877–885. [DOI] [PubMed] [Google Scholar]
- 23. Sica DA. Sodium and water retention in heart failure and diuretic therapy: basic mechanisms. Cleve Clin J Med. 2006;73(suppl 2):S2–S7. discussion S30‐S33. [DOI] [PubMed] [Google Scholar]
- 24. Konishi M, Haraguchi G, Ohigashi H, Sasaoka T, Yoshikawa S, Inagaki H, Ashikaga T, Isobe M. Progression of hyponatremia is associated with increased cardiac mortality in patients hospitalized for acute decompensated heart failure. J Card Fail. 2012;18:620–625. [DOI] [PubMed] [Google Scholar]
- 25. Sarraf M, Masoumi A, Schrier RW. Cardiorenal syndrome in acute decompensated heart failure. Clin J Am Soc Nephrol. 2009;4:2013–2026. [DOI] [PubMed] [Google Scholar]
- 26. Hamaguchi S, Kinugawa S, Tsuchihashi‐Makaya M, Matsushima S, Sakakibara M, Ishimori N, Goto D, Tsutsui H. Hyponatremia is an independent predictor of adverse clinical outcomes in hospitalized patients due to worsening heart failure. J Cardiol. 2014;63:182–188. [DOI] [PubMed] [Google Scholar]
- 27. Sato N, Gheorghiade M, Kajimoto K, Munakata R, Minami Y, Mizuno M, Aokage T, Asai K, Sakata Y, Yumino D, Mizuno K, Takano T; ATTEND Investigators . Hyponatremia and in‐hospital mortality in patients admitted for heart failure (from the ATTEND registry). Am J Cardiol. 2013;111:1019–1925. [DOI] [PubMed] [Google Scholar]


