Abstract
Background
A considerable amount of studies have examined the relationship between off‐hours (weekends and nights) admission and mortality risk for various diseases, but the results remain equivocal.
Methods and Results
Through a search of EMBASE, PUBMED, Web of Science, and Cochrane Database of Systematic Reviews, we identified cohort studies that evaluated the association between off‐hour admission and mortality risk for disease. In a random effects meta‐analysis of 140 identified articles (251 cohorts), off‐hour admission was strongly associated with increased mortality for aortic aneurysm (odds ratio, 1.52; 95% CI, 1.30–1.77), breast cancer (1.50, 1.21–1.86), leukemia (1.45, 1.17–1.79), respiratory neoplasm (1.32, 1.20–1.26), pancreatic cancer (1.32, 1.12–1.56), malignant neoplasm of genitourinary organs (1.27, 1.08–1.49), colorectal cancer (1.26, 1.07–1.49), pulmonary embolism (1.20, 1.13–1.28), arrhythmia and cardiac arrest (1.19, 1.09–1.29), and lymphoma (1.19, 1.06–1.34). Weaker (odds ratio <1.19) but statistically significant association was noted for renal failure, traumatic brain injury, heart failure, intracerebral hemorrhage, subarachnoid hemorrhage, stroke, gastrointestinal bleeding, myocardial infarction, chronic obstructive pulmonary disease, and bloodstream infections. No association was found for hip fracture, pneumonia, intestinal obstruction, aspiration pneumonia, peptic ulcer, trauma, diverticulitis, and neonatal mortality. Overall, off‐hour admission was associated with increased mortality for 28 diseases combined (odds ratio, 1.11; 95% CI, 1.10–1.13).
Conclusions
Off‐hour admission is associated with increased mortality risk, and the associations varied substantially for different diseases. Specialists, nurses, as well as hospital administrators and health policymakers can take these findings into consideration to improve the quality and continuity of medical services.
Keywords: disease, meta‐analysis, mortality, off‐hour
Subject Categories: Epidemiology, Risk Factors, Health Services, Meta Analysis, Mortality/Survival
Introduction
Due to certain uncontrollable reasons, such as the sudden onset of diseases, patients may be admitted to the hospital on off‐hours (weekends and nights). Because of a shortage of staff,1, 2, 3 lack of experienced clinician expertise,4 as well as inadequate subspecialty care5 and therapeutic6 or diagnostic procedures,4 off‐hour admission may be associated with increased mortality and other adverse outcomes, which has been called “off‐hour effect.”7
In previous studies, mortality has been regarded as a proxy measure to assess hospital performance and quality of care.8, 9 For example, the 30‐day mortality rate after acute myocardial infarction, chronic obstructive pulmonary disease, stroke, heart failure, and pneumonia has been used by the Centers for Medicare & Medicaid Services to compare outcomes across different hospitals.8 The investigation of differences in hospital mortality according to time of admission and possible mechanisms is the research emphasis of off‐hour effect.
Studies conducted as early as the 1970s found that infants born on weekends had slightly higher neonatal mortality compared with those born on weekdays.10, 11 Since the early 21st century, the effects of weekend hospital admissions mortality have been examined among diverse patient groups. In 2001, for example, Bell and Redelmeier conducted a study that investigated the risk of mortality among patients admitted on weekends compared with patients admitted on weekdays for 100 disease conditions.4 In 2004, Cram et al conducted a study to examine the effects of weekend hospital admission among patients with 50 common diagnoses and found statistically significant off‐hour effects on 3 specific diagnoses.12 Recently, Sorita et al performed 2 meta‐analyses and reported that there were significant off‐hour effects for patients diagnosed with myocardial infarction13 and acute ischemic stroke.14 However, several recently published studies were not included in the previous meta‐analyses. In addition, there are a large number of published studies on off‐hour effects for other diagnoses that have not been systematically synthesized in previous systematic reviews.
A comprehensive understanding of the relationship between off‐hour admission and mortality risk for different diseases will provide valuable information to hospital managers and health policymakers. Therefore, we conducted a systematic review and meta‐analysis of published cohort studies to estimate the association between off‐hour admission and mortality risk for a wide range of diseases or conditions.
Methods
Data Sources and Searches
This systematic review was conducted according to the Meta‐analysis Of Observational Studies in Epidemiology (MOOSE) statement.15 Relevant publications were electronically searched in 4 databases: EMBASE (1966 to January 2015), PubMed (1966 to January 2015), Web of Science (1965 to January 2015), and Cochrane Database of Systematic Reviews (1996 to January 2015). We used the following keywords to collect relevant citations: (off‐hour OR weekend OR night) AND (mortality OR fatality OR death OR survival OR hospital staffing). We restricted the search to human studies. There were no restrictions on language. When multiple publications on the same study population were identified, the most complete and recent study was included. Additionally, we scrutinized the references from relevant reviews and retrieved original articles to identify further potentially eligible studies.
Study Selection
We included cohort studies that compared short‐term mortality (in‐hospital, 7‐day, or 30‐day mortality) between patients with off‐hours admission versus regular‐hours admission. The comparison of off‐hours versus regular hours included the following categories: weekend and night versus weekday regular hours, weekends versus weekdays, and night versus day. We regarded national holidays as being equivalent to weekends. To be included, a cohort study should report the outcome measure as an odds ratio (OR), relative risk (RR), or hazard ratio (HR), and 95% CI or provide sufficient data to calculate them.
Data Extraction and Quality Assessment
Two investigators independently extracted data and a third reviewer checked data. Extracted data included information on country, years of enrollment of the cohort, the definition of off‐hours, data source, per‐group sample size, variables adjusted for, outcomes, and effect estimate (OR, RR, HR) with 95% CIs. The Newcastle–Ottawa Scale (NOS) was used to assess the quality of studies.16 The Newcastle–Ottawa Scale for cohort studies include 3 domains (quality of selection, comparability, and quality of outcome and adequacy of follow‐up), with a maximum score of 9 points. Studies with Newcastle–Ottawa Scale scores of 0 to 3, 4 to 6, and 7 to 9 were considered low, moderate, and high quality, respectively.17
Data Synthesis and Analysis
We used short‐term mortality as the main outcome. Thirty‐day mortality was preferable when it was available. We used adjusted estimates if both adjusted and unadjusted were provided. OR was used to measure the association between off‐hours admission and short‐term mortality. If only RR or HR estimates were available, we considered the reported RR or HR approximately as OR. We used the χ2 test and Cochran Q score (reported as I2) to estimate heterogeneity among studies. According to the estimated I2 values, inconsistency across studies was considered to be high (75% or greater), moderate (25–75%), and low (25% or less).18 We used the DerSimonian and Laird random‐effect model to pool results across studies, accounting for between‐study variance.19
For each individual disease, we conducted sensitivity analyses by sequential omission of each included study to investigate the potential influence of a single cohort on the pooled risk estimate. We also conducted sensitivity analyses by excluding studies that reported only RR or HR. In addition, sensitivity analyses were conducted by excluding studies with low‐to‐moderate quality.
For diseases that included more than 10 cohorts, we conducted subgroup analyses and assessed publication bias. Subgroup analyses were conducted to explore whether the association between time of admission and mortality risk differed according to outcome adjustment, data source, region, mortality type, and type of off‐hours. Publication bias was examined in funnel plots and with a rank correlation test.20
We conducted a random‐effects meta‐regression using the midyear of enrollment of the cohort as the independent variable and the natural log of OR for mortality as the dependent variable. All statistical analyses were performed using STATA version 12.0 (STATA Corporation, College Station, TX). All P values were 2‐sided and were considered significant if P<0.05.
Results
Identification and Description of Studies
After reviewing all potentially relevant citations, we identified 251 cohorts from 140 studies that met the inclusion criteria, including 25 450 474 participants. References of studies included in meta‐analyses are listed in Data S1. Figure 1 shows the study selection process. More than half the cohorts (166/251) were published since 2006. Studies published before 2006 were predominantly conducted in North America (Figure 2). Studies from Europe and Australia began to increase after 2006, and only a few studies were conducted in low‐ and middle‐income countries, such as China, Iraq, Saudi Arabia, and Kenya. In total, 146 cohorts were conducted in North America, 78 cohorts in the Europe and Australia, and 27 cohorts in other countries. Of the included studies, 4 studies reported results stratified by years of patient cohort and 11 studies reported off‐hour effect by diseases, resulting in 251 independent cohorts for the main analysis. Of the 251 independent cohorts, 210 cohorts reported adjusted mortality and 41 cohorts reported unadjusted mortality. In terms of data sources, 68 cohorts used data from clinical registry, and 183 cohorts from administrative data. Based on the Newcastle–Ottawa Scale quality assessment results, 238 cohorts had a high quality and 13 cohorts had a moderate quality (Figure 3). The main characteristics of the included cohorts are shown in Table 1, and the detail characteristics of the included studies are available in Table S1.
Figure 1.
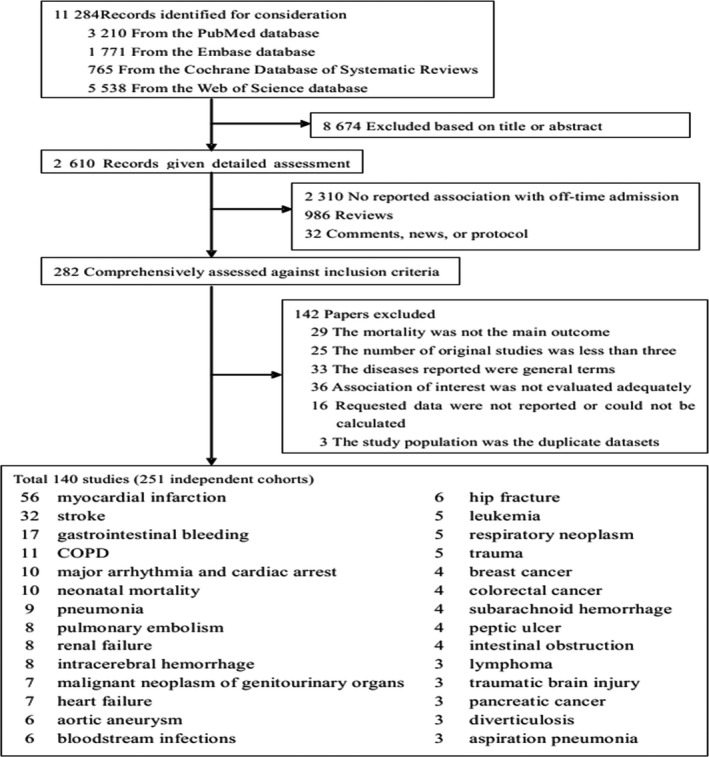
Flow chart for selection of eligible studies. COPD indicates chronic obstructive pulmonary disease.
Figure 2.
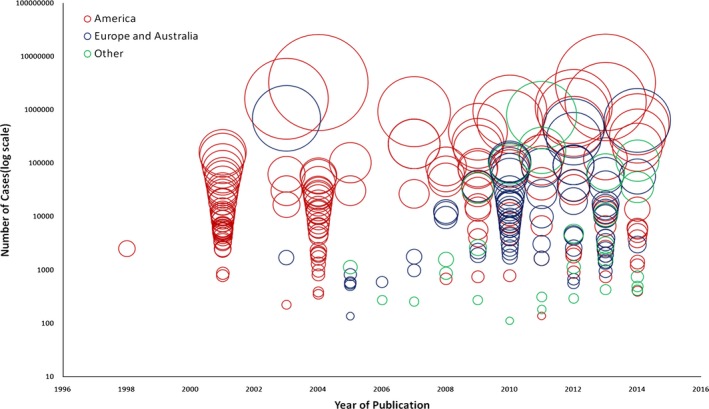
Data sets by year and population group. Size of circle is proportional to sample size.
Figure 3.
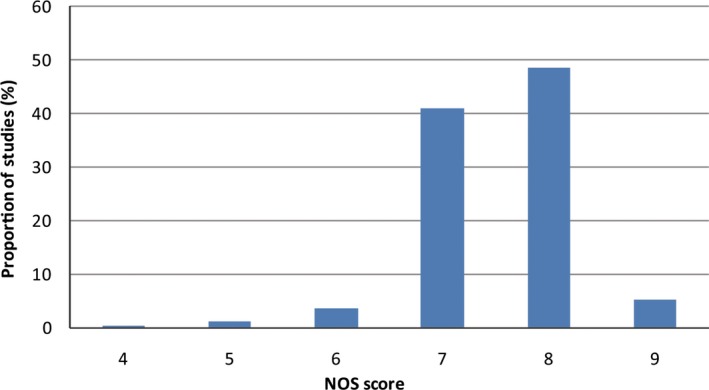
Study quality rating for 140 studies. NOS indicates Newcastle–Ottawa Scale.
Table 1.
Baseline Characteristics for Studies Included in Meta‐Analysis
| Disease | Number of Data Sets | Region | Data source | Median Duration of Study Period (Years) | Total Sample Size | Quality Assessment | Mean Number of Potential Confounders in Analysis | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| North America | Europe and Australia | Others | Clinical Registry | Administrative Data | 7 to 9a | 4 to 6a | |||||
| Myocardial infarction | 56 | 22 | 24 | 10 | 37 | 19 | 5 (0.75–10) | 5 085 950 | 55 | 1 | 6 (0–11) |
| Stroke | 32 | 14 | 10 | 8 | 14 | 18 | 4 (1–18) | 1 865 127 | 30 | 2 | 6 (0–11) |
| Gastrointestinal bleeding | 17 | 9 | 5 | 3 | 5 | 12 | 2 (1–12) | 1 102 795 | 17 | 0 | 3 (0–5) |
| COPD | 11 | 6 | 5 | 0 | 0 | 11 | 1 (1–17) | 862 610 | 11 | 0 | 4 (2–6) |
| Neonatal mortality | 10 | 8 | 2 | 0 | 2 | 8 | 3.5 (1–13) | 7 493 579 | 6 | 4 | 3 (0–5) |
| Arrhythmia and cardiac arrest | 10 | 6 | 3 | 1 | 4 | 6 | 5 (1–10) | 467 660 | 9 | 1 | 3 (0–5) |
| Pneumonia | 9 | 5 | 2 | 2 | 1 | 8 | 4 (1–11) | 1 084 796 | 8 | 1 | 3 (2–4) |
| Pulmonary embolism | 8 | 5 | 3 | 0 | 8 | 0 | 4.5 (1–10) | 1 258 258 | 6 | 2 | 4 (0–8) |
| Renal failure | 8 | 6 | 2 | 0 | 0 | 8 | 5.5 (1–9) | 4 288 095 | 8 | 0 | 4 (3–5) |
| Intracerebral hemorrhage | 8 | 6 | 1 | 1 | 1 | 7 | 1.5 (1–9) | 64 551 | 7 | 1 | 3 (0–6) |
| Heart failure | 7 | 4 | 2 | 1 | 1 | 6 | 3 (1–9) | 399 010 | 7 | 0 | 4 (1–7) |
| Malignant neoplasm of genitourinary organs | 7 | 0 | 7 | 0 | 0 | 7 | 9 (1–11) | 558 898 | 7 | 0 | 3 (2–4) |
| Aortic aneurysm | 6 | 0 | 4 | 2 | 0 | 6 | 1.5 (1–10) | 36 214 | 6 | 0 | 4 (3–5) |
| Hip fracture | 6 | 2 | 4 | 0 | 3 | 3 | 3 (1–9) | 127 461 | 6 | 0 | 3 (0–6) |
| Bloodstream infections | 6 | 5 | 1 | 0 | 2 | 4 | 4 (1–9) | 191 701 | 6 | 0 | 3 (2–5) |
| Trauma | 5 | 5 | 0 | 0 | 0 | 5 | 4 (1–8) | 131 469 | 4 | 1 | 3 (0–5) |
| Leukemia | 5 | 3 | 2 | 0 | 0 | 5 | 2 (1–9) | 17 717 | 5 | 0 | 4 (3–4) |
| Respiratory neoplasm | 5 | 3 | 2 | 0 | 0 | 5 | 7 (1–9) | 65 909 | 5 | 0 | 4 (3–4) |
| Subarachnoid hemorrhage | 4 | 3 | 0 | 1 | 0 | 4 | 2 (1–9) | 14 015 | 4 | 0 | 5 (3–6) |
| Peptic ulcer | 4 | 4 | 0 | 0 | 0 | 4 | 5 (1–9) | 46 087 | 4 | 0 | 4 (3–4) |
| Breast cancer | 4 | 2 | 2 | 0 | 0 | 4 | 4 (1–9) | 13 306 | 4 | 0 | 4 (3–4) |
| Colorectal cancer | 4 | 3 | 1 | 0 | 0 | 4 | 5 (1–9) | 28 307 | 4 | 0 | 4 (3–4) |
| Intestinal obstruction | 4 | 3 | 1 | 0 | 0 | 4 | 4 (1–9) | 79 252 | 4 | 0 | 2 (0–4) |
| Traumatic brain injury | 3 | 3 | 0 | 0 | 0 | 3 | 2 (1–9) | 45 853 | 3 | 0 | 4 (3–5) |
| Diverticulosis | 3 | 3 | 0 | 0 | 0 | 3 | 6 (1–9) | 67 960 | 3 | 0 | 6 (3–9) |
| Pancreatic cancer | 3 | 2 | 1 | 0 | 0 | 3 | 1 (1–9) | 11 755 | 3 | 0 | 4 (3–4) |
| Lymphoma | 3 | 2 | 1 | 0 | 0 | 3 | 1 (1–9) | 15 175 | 3 | 0 | 4 (3–4) |
| Aspiration pneumonia | 3 | 2 | 1 | 0 | 0 | 3 | 1 (1–9) | 26 964 | 3 | 0 | 4 (3–4) |
COPD indicates chronic obstructive pulmonary disease.
Study quality was assessed using the Newcastle–Ottawa Scale.
Mortality for All Diagnoses and by Diagnoses
For all diagnoses combined, off‐hour admission was associated with significantly higher short‐term mortality (OR, 1.11; 95% CI, 1.10–1.13, with a high heterogeneity I2=81.8%, P<0.001).
Figure 4 shows the results of meta‐analyses by individual diagnoses. Among the 28 individual diagnoses, the association between off‐hour admission and short‐term mortality was statistically significant for aortic aneurysm (OR, 1.52; 95% CI, 1.30–1.77), breast cancer (1.50, 1.21–1.86), leukemia (1.45, 1.17–1.79), respiratory neoplasm (1.32, 1.20–1.26), pancreatic cancer (1.32, 1.12–1.56), malignant neoplasm of genitourinary organs (1.27, 1.08–1.49), colorectal cancer (1.26, 1.07–1.49), pulmonary embolism (1.20, 1.13–1.28), arrhythmia and cardiac arrest (1.19, 1.09–1.29), and lymphoma (1.19, 1.06–1.34).
Figure 4.
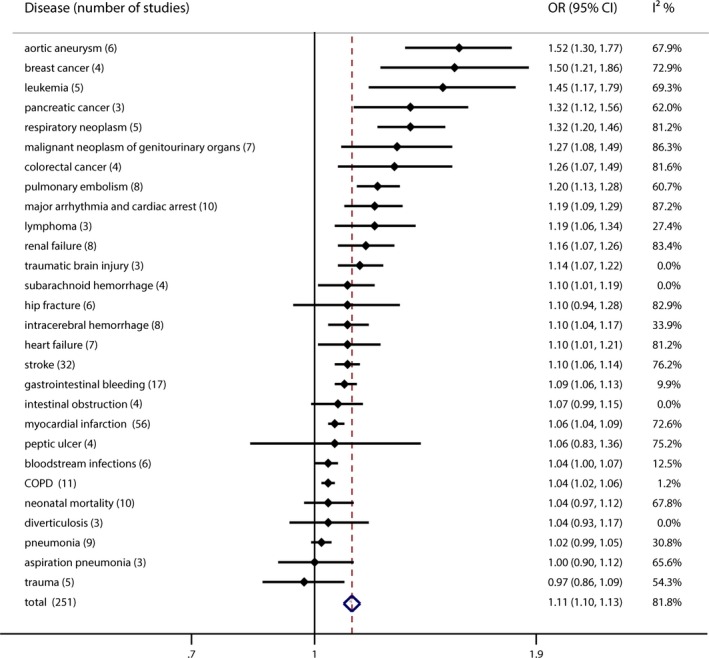
Summary risk estimates of off‐hour admission and mortality risk for 28 specific diseases. Box sizes are in proportion to study weights. “Total” means summary risk estimates for 28 diseases combined. COPD indicates chronic obstructive pulmonary disease; OR, odds ratio.
Weaker (OR <1.19) but statistically significant association was found for renal failure (OR, 1.16; 95% CI, 1.07–1.26), traumatic brain injury (1.14, 1.07–1.22), heart failure (1.10, 1.01–1.21), intracerebral hemorrhage (1.10, 1.04–1.17), subarachnoid hemorrhage (1.10, 1.01–1.19), stroke (1.10, 1.06–1.14), gastrointestinal bleeding (1.09, 1.06–1.13), myocardial infarction (1.06, 1.04–1.09), chronic obstructive pulmonary disease (1.04, 1.02–1.06), and bloodstream infections (1.04, 1.00–1.07).
No significant association was found for hip fracture (OR, 1.10; 95% CI, 0.94–1.28), intestinal obstruction (1.07, 0.99–1.15), peptic ulcer (1.06, 0.83–1.36), trauma (0.97, 0.86–1.09), pneumonia (1.02, 0.99–1.05), aspiration pneumonia (1.00, 0.90–1.12), diverticulitis (1.04, 0.93–1.17), and neonatal mortality (1.04, 0.97–1.12).
No statistically significant heterogeneity across studies was observed for off‐hour admission in relation to mortality risk for lymphoma, gastrointestinal bleeding, traumatic brain injury, intestinal obstruction, bloodstream infections, chronic obstructive pulmonary disease, diverticulitis, pneumonia, subarachnoid hemorrhage, and intracerebral hemorrhage. We observed some heterogeneity for studies of off‐hour admission and the other 18 diseases (Figure 4). Publication bias was not indicated according to funnel plots and results of related statistical tests (the smallest P=0.185, the Begg–Mazumdar test for gastrointestinal bleeding).
Subgroup Analyses, Meta‐Regression, and Sensitivity Analyses
Table 2 shows the results of subgroup analyses. For gastrointestinal hemorrhage, arrhythmia and cardiac arrest, stroke, and myocardial infarction, significant associations between off‐hour admission and mortality risk were observed in studies that adjusted for potential confounding factors, whereas null associations were reported in studies that did not adjust for confounding factors. However, for neonatal mortality, we recorded a positive association for studies that did not adjust for confounding factors (OR, 1.23; 95% CI, 1.05–1.44), but null association was noted for studies that adjusted for potential factors (0.98, 0.94–1.01).
Table 2.
Subgroup Analyses of 6 Diseases
| Subgroup | Gastrointestinal Hemorrhage | Arrhythmia and Cardiac Arrest | Neonatal Mortality | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. of Studies | OR (95% CI) | I2 (%) | P Value | No. of Studies | OR (95% CI) | I2 (%) | P Value | No. of Studies | OR (95% CI) | I2 (%) | P Value | |
| Outcome adjustment | ||||||||||||
| Adjusted | 14 | 1.09 (1.06–1.13) | 18.0 | 0.26 | 6 | 1.24 (1.12–1.37) | 68.9 | 0.01 | 5 | 0.98 (0.94–1.01) | 2.1 | 0.39 |
| Unadjusted | 3 | 1.11 (0.80–1.54) | 0.0 | 0.39 | 4 | 1.11 (0.97–1.26) | 91.8 | <0.001 | 5 | 1.23 (1.05–1.44) | 51.3 | 0.08 |
| Data source | ||||||||||||
| Administrative data | 12 | 1.09 (1.06–1.13) | 9.3 | 0.35 | 6 | 1.22 (1.13–1.30) | 40.7 | 0.13 | 8 | 1.04 (0.96–1.13) | 72.3 | <0.001 |
| Clinical registry | 5 | 1.23 (0.87–1.72) | 20.3 | 0.29 | 4 | 1.13 (0.97–1.30) | 93.3 | <0.001 | 2 | 1.06 (0.92–1.22) | 52.3 | 0.15 |
| Region | ||||||||||||
| North America | 9 | 1.09 (1.04–1.14) | 24.9 | 0.22 | 6 | 1.22 (1.10–1.35) | 71.5 | <0.001 | 8 | 1.03 (0.95–1.12) | 72.1 | <0.001 |
| Europe and Australia | 5 | 1.13 (1.02–1.26) | 32.3 | 0.21 | 3 | 1.21 (1.10–1.34) | 42.4 | 0.18 | 2 | 1.08 (0.97–1.12) | 18.1 | 0.27 |
| Others | 3 | 0.98 (0.67–1.44) | 0.0 | 0.75 | 1 | 1.00 (0.97–1.04) | NA | NA | 0 | NA | NA | NA |
| Mortality | ||||||||||||
| In‐hospital mortality | 14 | 1.09 (1.06–1.12) | 0.0 | 0.47 | 9 | 1.21 (1.13–1.29) | 68.1 | 0.01 | NA | NA | NA | NA |
| 30‐day mortality | 3 | 1.19 (0.78–1.82) | 55.1 | 0.11 | 1 | 1.00 (0.97–1.04) | NA | NA | NA | NA | NA | NA |
| 7‐day mortality | 0 | NA | NA | NA | 0 | NA | NA | NA | NA | NA | NA | NA |
| Type of off‐hour | ||||||||||||
| Weekend and night | 0 | NA | NA | NA | 1 | 5.73 (2.32–14.15) | NA | NA | NA | NA | NA | NA |
| Weekend | 17 | 1.09 (1.06–1.13) | 9.9 | 0.34 | 9 | 1.17 (1.08–1.26) | 86.2 | 0.00 | 10 | 1.04 (0.97–1.12) | 67.8 | 0.00 |
| Night | 0 | NA | NA | NA | 0 | NA | NA | NA | NA | NA | NA | NA |
| Subgroup | Myocardial Infarction | Stroke | COPD | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. of Studies | OR (95% CI) | I2 (%) | P Value | No. of Studies | OR (95% CI) | I2 (%) | P Value | No. of Studies | OR (95% CI) | I2 (%) | P Value | |
| Outcome adjustment | ||||||||||||
| Adjusted | 42 | 1.06 (1.04–1.09) | 74.0 | <0.001 | 23 | 1.10 (1.05–1.14) | 80.6 | <0.001 | 11 | 1.04 (1.02–1.06) | 1.2 | 0.43 |
| Unadjusted | 14 | 1.11 (0.98–1.25) | 42.0 | 0.04 | 9 | 1.10 (1.00–1.21) | 34.9 | 0.14 | 0 | NA | NA | NA |
| Data source | ||||||||||||
| Administrative data | 19 | 1.07 (1.04–1.10) | 85.0 | <0.001 | 18 | 1.08 (1.04–1.13) | 82.8 | <0.001 | 11 | 1.04 (1.02–1.06) | 1.2 | 0.43 |
| Clinical registry | 37 | 1.07 (1.01–1.13) | 54.5 | <0.001 | 14 | 1.13 (1.05–1.22) | 44.1 | 0.04 | 0 | NA | NA | NA |
| Region | ||||||||||||
| North America | 22 | 1.04 (1.02–1.06) | 67.2 | <0.001 | 14 | 1.04 (1.01–1.08) | 39.1 | 0.07 | 5 | 1.05 (1.03–1.07) | 0.0 | 0.91 |
| Europe and Australia | 24 | 1.08 (1.07–1.15) | 53.0 | <0.001 | 10 | 1.14 (1.07–1.21) | 68.6 | <0.001 | 6 | 1.01 (0.96–1.07) | 47.7 | 0.11 |
| Others | 10 | 1.18 (0.97–1.43) | 37.9 | 0.11 | 8 | 1.20 (1.09–1.32) | 60.9 | 0.01 | 0 | NA | NA | NA |
| Mortality | ||||||||||||
| In‐hospital mortality | 42 | 1.06 (1.04–1.08) | 62.5 | <0.001 | 19 | 1.07 (1.03–1.10) | 65.5 | <0.001 | 9 | 1.05 (1.03–1.07) | 0.0 | 0.79 |
| 30‐day mortality | 14 | 1.07 (0.97–1.19) | 84.7 | <0.001 | 9 | 1.14 (1.04–1.24) | 40.2 | 0.10 | 1 | 0.92 (0.81–1.04) | NA | NA |
| 7‐day mortality | 0 | NA | NA | NA | 4 | 1.18 (1.09–1.27) | 70.7 | 0.02 | 1 | 1.75 (0.75–4.11) | NA | NA |
| Type of off‐hour | ||||||||||||
| Weekend and night | 26 | 1.06 (1.01–1.12) | 58.0 | <0.001 | 7 | 1.09 (1.01–1.18) | 48.1 | 0.07 | NA | NA | NA | NA |
| Weekend | 24 | 1.07 (1.04–1.09) | 82.0 | <0.001 | 25 | 1.10 (1.05–1.15) | 79.1 | <0.001 | NA | NA | NA | NA |
| Night | 6 | 1.38 (0.92–2.08) | 57.0 | 0.04 | 0 | NA | NA | NA | NA | NA | NA | NA |
COPD indicates chronic obstructive pulmonary disease; NA, not applicable; OR, odds ratio.
We also observed a positive association between off‐hour effect and gastrointestinal hemorrhage in studies conducted in North American (OR, 1.09; 95% CI, 1.04–1.14) or in European countries (1.13, 1.02–1.26), but the association was not found in studies conducted in other countries (0.98, 0.67–1.44). Similar results were observed in studies of arrhythmia and cardiac arrest, neonatal mortality, and myocardial infarction.
We also conducted subgroup analyses according to whether the off‐hours were defined as weekends, nights, or weekends and nights. For stroke, the results were consistent between studies that defined off‐hours as weekend and night (OR, 1.09; 95% CI, 1.01–1.18) and studies that defined off‐hour as weekend only (1.10, 1.05–1.15). For myocardial infarction, we recorded positive associations in studies that defined off‐hours as weekend and night (1.06, 1.01–1.12) or as weekend only (1.07, 1.04–1.09), but nonsignificant association was noted in studies in which off‐hours were defined as night only (1.38, 0.92–2.08), which may be due to relatively small sample size.
Meta‐regression did not reveal a significant time trend on the mortality difference between off‐hours and regular hours (P=0.23) (Figure 5). Sensitivity analyses by excluding each single cohort showed that no single studies substantially affected the pooled results. The results were also not materially altered when studies that reported only RR or HR and that had a moderate quality were excluded.
Figure 5.
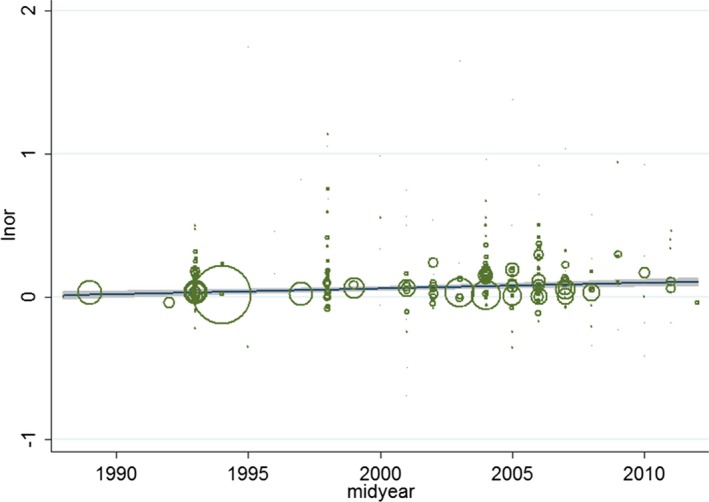
Meta‐regression for short‐term mortality. Inor indicates In(odds ratio).
Discussion
Findings from this systematic review showed that, on average, patients admitted to hospitals during off‐hours experienced higher mortality risk (both 30‐day and in‐hospital mortality) than patients admitted during regular hours. The current meta‐analysis greatly extended the scope of existing systematic reviews13, 14 and showed significant associations between off‐hour admission and mortality risk for 20 diseases (including 7 common malignancies).
Comparison With Other Studies
Many studies have discussed the potential mechanisms of off‐hour effect. Researchers highlighted problems regarding the accessibility and quality of medical services on off‐hours, such as lower levels of medical staff,21 inadequate access to specialized services,1, 22 discontinuity of care,23 and reduced availability of certain procedures.2, 24 Based on findings from the current systematic review of multiple diseases, we found that the off‐hour effect may be exacerbated particularly when optimal patient care requires an increase in medical resources.
Firstly, there were significant off‐hour effects in conditions, such as patients with malignancies and acute illnesses, where the amount of medical resources required were great and advanced medical technology for diagnosis and treatments were required. For example, in patients with acute leukemia, immediate initiation of intensive induction chemotherapy is generally considered requisite for maximizing survival. However, during off‐hours, there is often a reduction in availability of certain procedures and medical staff.25 Considerable medical resources are often required for the care of patients with acute illnesses, such as pulmonary embolism, gastrointestinal bleeding, and cardiac arrest. For example, the diagnosis of pulmonary embolism is complex and requires timely access to radiographic procedures, while the availability and quality of diagnostic and therapeutic procedures may differ between off‐hours and regular hours.26 Early endoscopy may improve gastrointestinal bleeding outcomes, while a delay in the execution of gastrointestinal endoscopy may occur more often on off‐hours.27, 28 Resuscitation system processes can improve patient survival following cardiac arrest, but the procedure may be delayed because of inadequate availability of healthcare professionals on off‐hour periods.29, 30
Secondly, we did not find significant off‐hour effects in conditions, such as patients with hip fracture and peptic ulcer disease, where relatively fewer health resources were needed. Previous studies have proposed that hip fracture is an easily diagnosed condition that requires limited preoperative resources, and a standardized treatment may compensate for the reduced health resources during off‐hours.31, 32 In addition, treatment for peptic ulcer usually means taking medicines and making lifestyle changes, so that the reduced staffing level during weekends and holidays is unlikely to increase mortality risk.33
Thirdly, we did not find an off‐hour effect on diseases that were usually managed in clinical departments with balanced distribution of medical resources during off‐hours and regular hours. This was exemplified in the case of trauma. Compared with other clinical departments, trauma centers were required to be fully resourced and staffed independent of time of day or day of week.34, 35 Trauma centers had a reduced mortality compared with nontrauma centers,36 and the trauma center's systems‐based approach has been recommended by the Institute of Medicine as a model of coordinated, regionalized, and accountable emergency care, which could be a referable model of care, especially for many time‐critical conditions including cardiac arrest and ischemic stroke.34
The off‐hour effect may be partly explained by the reduced accessibility and quality of medical resources.37 In addition, differences in conditions may be attributed to the selection bias on the apparent size of the off‐hour effect. For example, babies are born all times of the day and so one would expect there to be less variation between off‐hour and regular hours in the rate of neonatal admissions, and hence in selection bias. By contrast, it is quite plausible that cancer admissions in off‐hours are biased towards patients with greater illness severity or acuity. Some studies had found that patients admitted during off‐hours may have relatively more severe conditions27 or be intrinsically at higher risk of death by virtue of different case mix as compared with patients admitted on regular hours.38, 39 A higher proportion of severe cases may be admitted to the hospital during off‐hours, while those with milder symptoms would wait to speak to their doctors in the following regular hours.1 In addition, other confounding factors may also affect the off‐hour effect.40, 41 For example, off‐hour admission is not associated with increased neonatal mortality. A small number of studies had observed slightly higher crude risks of early neonatal death on weekends. However, the risks disappeared after adjustment for gestational age42, 43 or birth weight.38, 44
Strengths and Limitations
The strength of our study is that we estimated the off‐hour effect with unprecedented precision and power. We summarized data from 251 cohorts for 28 specific diseases, including 25 450 474 participants, and most of the included studies were adjusted for substantial numbers of potential confounding variables. We also conducted detailed sensitivity analyses and assessed the quality of each included study. Sensitivity analyses confirmed the robustness and reliability of the main results, and study quality assessment showed that most of the included studies had a high quality.
Our study also has some limitations. Firstly, the case mix was an inevitable problem and also was regarded as a limitation in original studies. Secondly, the data source and mortality type were diverse among included studies. However, in subgroup analyses, we found that the data source (clinical registry versus administrative data) and mortality (in‐hospital and 30‐day mortality) did not significantly modify the estimated off‐hour effects. Thirdly, high heterogeneity was observed between studies. Heterogeneity across cohorts may result from differences in healthcare system, care delivery models, staffing or resource availability, and types of facility in different countries.24 Discrepancies in patient demographics and different definitions of weekends or nights may also be causes of unexplained heterogeneity.27, 45 Finally, most of the studies were conducted in North America and Europe where the medical resources are relatively more adequate compared with low‐ and middle‐income countries, such as China and Kenya. Thus, it is unclear whether the results are generalizable to low and middle countries, and future studies are needed in resource‐limited settings.
Implications for Clinicians and Policymakers
Our study evaluated not only the average off‐hour effect for all diseases, but also addressed disease‐specific off‐hour effects. Results of disease‐specific off‐hour effects may inform decision making in different clinical settings. The extent of off‐hour effects clearly varied across different diseases, which may offer valuable information to specialists and nurses to improve the quality of their patient care. In addition, important information could be provided to hospital administrators and health policymakers. They can make evidence‐based decisions about the hospital scheduling systems and equipment arrangement for different diseases and clinical settings, which may play a substantial role in reducing hospital mortality.
Conclusions
Our meta‐analysis suggests that off‐hour admission is on average associated with increased mortality risk, although the off‐hour effects varied substantially for different diseases. Specialists, nurses, as well as hospital administrators and health policymakers can take these findings into consideration to improve the quality and continuity of medical services. Quality improvement strategies should be developed and implemented in healthcare systems to achieve a time‐invariant effect and standardize health care across admission day.
Disclosures
None.
Supporting information
Table S1. Study Characteristics for Cohorts of Off‐hour Admission and Mortality Risk
Data S1. List of references included in meta‐analysis.
Author Contributions
The contributions of the authors were as follows: Zhou, Li, Cao, and Lu conceived and designed the review. Zhou and Li identified and acquired reports of trials, abstracted data, and assessed risk of bias. Zhou, Li, Herath, and Cao drafted the manuscript. Xia, Hu, Song, and Lu provided supervision. Song and Zhou conducted the statistical analyses. All of the authors contributed to the interpretation of data and all of the authors critically revised the manuscript submitted for publication.
(J Am Heart Assoc. 2016;5:e003102 doi: 10.1161/JAHA.115.003102)
Accompanying Data S1 and Table S1 are available at http://jaha.ahajournals.org/content/5/3/e003102/suppl/DC1
References
- 1. Worni M, Schudel IM, Østbye T, Shah A, Khare A, Pietrobon R, Thacker JK, Guller U. Worse outcomes in patients undergoing urgent surgery for left‐sided diverticulitis admitted on weekends vs weekdays: a population‐based study of 31 832 patients. Arch Surg. 2012;147:649–655. [DOI] [PubMed] [Google Scholar]
- 2. Kostis WJ, Demissie K, Marcella SW, Shao YH, Wilson AC, Moreyra AE. Weekend versus weekday admission and mortality from myocardial infarction. N Engl J Med. 2007;356:1099–1109. [DOI] [PubMed] [Google Scholar]
- 3. Ricciardi R, Roberts PL, Read TE, Baxter NN, Marcello PW, Schoetz DJ. Mortality rate after nonelective hospital admission. Arch Surg. 2011;146:545–551. [DOI] [PubMed] [Google Scholar]
- 4. Bell CM, Redelmeier DA. Mortality among patients admitted to hospitals on weekends as compared with weekdays. N Engl J Med. 2001;345:663–668. [DOI] [PubMed] [Google Scholar]
- 5. Needleman J, Buerhaus P, Mattke S, Stewart M, Zelevinsky K. Nurse‐staffing levels and the quality of care in hospitals. N Engl J Med. 2002;346:1715–1722. [DOI] [PubMed] [Google Scholar]
- 6. Magid DJ, Wang Y, Herrin J, McNamara RL, Bradley EH, Curtis JP, Pollack CV Jr, French WJ, Blaney ME, Krumholz HM. Relationship between time of day, day of week, timeliness of reperfusion, and in‐hospital mortality for patients with acute ST‐segment elevation myocardial infarction. JAMA. 2005;294:803–812. [DOI] [PubMed] [Google Scholar]
- 7. McDowell MM, Kellner CP, Sussman ES, Bruce SS, Bruce RA, Heuts SG, Sander Connolly E. The role of admission timing in the outcome of intracerebral hemorrhage patients at a specialized stroke center. Neurol Res. 2014;36:95–101. [DOI] [PubMed] [Google Scholar]
- 8. Chang GM, Tung YC. Factors associated with pneumonia outcomes: a nationwide population‐based study over the 1997–2008 period. J Gen Intern Med. 2012;27:527–533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Agency for Health care Research and Quality . Guide to inpatient quality indicators: quality of care in hospital‐volume, mortality, and utilization. Available at: http://qualityindicators.ahrq.gov/downloads/modules/iqi/v31/iqi_guide_v31.pdf. Accessed March 12, 2007.
- 10. MacFarlane A. Variations in number of births and perinatal mortality by day of week in England and Wales. Br Med J. 1978;2:1670–1673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hendry RA. The weekend—a dangerous time to be born? Br J Obstet Gynaecol. 1981;88:1200–1203. [DOI] [PubMed] [Google Scholar]
- 12. Cram P, Hillis SL, Barnett M, Rosenthal GE. Effects of weekend admission and hospital teaching status on in‐hospital mortality. Am J Med. 2004;117:151–157. [DOI] [PubMed] [Google Scholar]
- 13. Sorita A, Ahmed A, Starr SR, Thompson KM, Reed DA, Prokop L, Shah ND, Murad MH, Ting HH. Off‐hour presentation and outcomes in patients with acute myocardial infarction: systematic review and meta‐analysis. BMJ. 2014;348:f7393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Sorita A, Ahmed A, Starr SR, Thompson KM, Reed DA, Dabrh AM, Prokop L, Kent DM, Shah ND, Murad MH, Ting HH. Off‐hour presentation and outcomes in patients with acute ischemic stroke: a systematic review and meta‐analysis. Eur J Intern Med. 2014;25:394–400. [DOI] [PubMed] [Google Scholar]
- 15. Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB. Meta‐analysis of observational studies in epidemiology: a proposal for reporting. Meta‐analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283:2008–2012. [DOI] [PubMed] [Google Scholar]
- 16. Stang A. Critical evaluation of the Newcastle‐Ottawa scale for the assessment of the quality of nonrandomized studies in meta‐analyses. Eur J Epidemiol. 2010;25:603–605. [DOI] [PubMed] [Google Scholar]
- 17. Wolf HT, Owe KM, Juhl M, Hegaard HK. Leisure time physical activity and the risk of pre‐eclampsia: a systematic review. Matern Child Health J. 2014;18:899–910. [DOI] [PubMed] [Google Scholar]
- 18. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ. 2003;327:557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. DerSimonian R, Laird N. Meta‐analysis in clinical trials. Control Clin Trials. 1986;7:177–188. [DOI] [PubMed] [Google Scholar]
- 20. Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50:1088–1101. [PubMed] [Google Scholar]
- 21. Tarnow‐Mordi WO, Hau C, Warden A, Shearer AJ. Hospital mortality in relation to staff workload: a 4‐year study in an adult intensive‐care unit. Lancet. 2000;356:185–189. [DOI] [PubMed] [Google Scholar]
- 22. Meltzer D, Manning WG, Morrison J, Shah MN, Jin L, Guth T, Levinson W. Effects of physician experience on costs and outcomes on an academic general medicine service: results of a trial of hospitalists. Ann Intern Med. 2002;137:866–874. [DOI] [PubMed] [Google Scholar]
- 23. Gallerani M, Volpato S, Boari B, Pala M, De Giorgi A, Fabbian F, Gasbarro V, Bossone E, Eagle KA, Carle F, Manfredini R. Outcomes of weekend versus weekday admission for acute aortic dissection or rupture: a retrospective study on the Italian National Hospital Database. Int J Cardiol. 2013;168:3117–3119. [DOI] [PubMed] [Google Scholar]
- 24. Jneid H, Fonarow GC, Cannon CP, Palacios IF, Kilic T, Moukarbel GV, Maree AO, LaBresh KA, Liang L, Newby LK, Fletcher G, Wexler L, Peterson E. Impact of time of presentation on the care and outcomes of acute myocardial infarction. Circulation. 2008;117:2502–2509. [DOI] [PubMed] [Google Scholar]
- 25. Bejanyan N, Fu AZ, Lazaryan A, Fu R, Kalaycio M, Advani A, Sobecks R, Copelan E, Maciejewski JP, Sekeres MA. Impact of weekend admissions on quality of care and outcomes in patients with acute myeloid leukemia. Cancer. 2010;116:3614–3620. [DOI] [PubMed] [Google Scholar]
- 26. Aujesky D, Jiménez D, Mor MK, Geng M, Fine MJ, Ibrahim SA. Weekend versus weekday admission and mortality after acute pulmonary embolism. Circulation. 2009;119:962–968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Dorn SD, Shah ND, Berg BP, Naessens JM. Effect of weekend hospital admission on gastrointestinal hemorrhage outcomes. Dig Dis Sci. 2010;55:1658–1666. [DOI] [PubMed] [Google Scholar]
- 28. Abougergi MS, Travis AC, Saltzman JR. Impact of day of admission on mortality and other outcomes in upper GI hemorrhage: a nationwide analysis. Gastrointest Endosc. 2014;80:228–235. [DOI] [PubMed] [Google Scholar]
- 29. Peberdy MA, Ornato JP, Larkin GL, Braithwaite RS, Kashner TM, Carey SM, Meaney PA, Cen L, Nadkarni VM, Praestqaard AH, Berg RA. Survival from in‐hospital cardiac arrest during nights and weekends. JAMA. 2008;299:785–792. [DOI] [PubMed] [Google Scholar]
- 30. Koike S, Tanabe S, Ogawa T, Akahane M, Yasunaga H, Horiguchi H, Matsumoto S, Imamura T. Effect of time and day of admission on 1‐month survival and neurologically favourable 1‐month survival in out‐of‐hospital cardiopulmonary arrest patients. Resuscitation. 2011;82:863–868. [DOI] [PubMed] [Google Scholar]
- 31. Daugaard CL, Jorgensen HL, Riis T, Lauritzen JB, Duus BR, van der Mark S. Is mortality after hip fracture associated with surgical delay or admission during weekends and public holidays? A retrospective study of 38,020 patients. Acta Orthop. 2012;83:609–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Foss NB, Kehlet H. Short‐term mortality in hip fracture patients admitted during weekends and holidays. Br J Anaesth. 2006;96:450–454. [DOI] [PubMed] [Google Scholar]
- 33. Ahsberg K, Ye W, Lu Y, Zheng Z, Staël von Holstein C. Hospitalisation of and mortality from bleeding peptic ulcer in Sweden: a nationwide time‐trend analysis. Aliment Pharmacol Ther. 2011;33:578–584. [DOI] [PubMed] [Google Scholar]
- 34. Carr BG, Jenkins P, Branas CC, Wiebe DJ, Kim P, Schwab CW, Reilly PM. Does the trauma system protect against the weekend effect? J Trauma. 2010;69:1042–1047. [DOI] [PubMed] [Google Scholar]
- 35. Carr BG, Reilly PM, Schwab CW, Branas CC, Geiger J, Wiebe DJ. Weekend and night outcomes in a statewide trauma system. Arch Surg. 2011;146:810–817. [DOI] [PubMed] [Google Scholar]
- 36. MacKenzie EJ, Rivara FP, Jurkovich GJ, Nathens AB, Frey KP, Egleston BL, Salkever DS, Scharfstein DO. A national evaluation of the effect of trauma‐center care on mortality. N Engl J Med. 2006;354:366–378. [DOI] [PubMed] [Google Scholar]
- 37. Concha OP, Gallego B, Hillman K, Delaney GP, Coiera E. Do variations in hospital mortality patterns after weekend admission reflect reduced quality of care or different patient cohorts? A population‐based study BMJ Qual Saf. 2014;23:215–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Gould JB, Qin C, Marks AR, Chavez G. Neonatal mortality in weekend vs weekday births. JAMA. 2003;289:2958–2962. [DOI] [PubMed] [Google Scholar]
- 39. Laupland KB, Ball CG, Kirkpatrick AW. Hospital mortality among major trauma victims admitted on weekends and evenings: a cohort study. J Trauma Manag Outcomes. 2009;3:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Clarke MS, Wills RA, Bowman RV, Zimmerman PV, Fong KM, Coory MD, Yang IA. Exploratory study of the ‘weekend effect’ for acute medical admissions to public hospitals in Queensland, Australia. Intern Med J. 2010;40:777–783. [DOI] [PubMed] [Google Scholar]
- 41. Ibrahimou B, Salihu HM, English G, Anozie C, Lartey G, Dagne G. Twins born over weekends: are they at risk for elevated infant mortality? Arch Gynecol Obstet. 2012;286:1349–1355. [DOI] [PubMed] [Google Scholar]
- 42. Chen XK, Wen SW, Fleming N, Demissie K, Rhoads GG, Walker M. Teenage pregnancy and adverse birth outcomes: a large population based retrospective cohort study. Int J Epidemiol. 2007;36:368–373. [DOI] [PubMed] [Google Scholar]
- 43. Luo ZC, Liu S, Wilkins R, Kramer MS. Risks of stillbirth and early neonatal death by day of week. CMAJ. 2004;170:337–341. [PMC free article] [PubMed] [Google Scholar]
- 44. Bell EF, Hansen NI, Morriss FH Jr, Stoll BJ, Ambalavanan N, Gould JB, Laptook AR, Walsh MC, Carlo WA, Shankaran S, Das A, Hiqqins RD. Impact of timing of birth and resident duty‐hour restrictions on outcomes for small preterm infants. Pediatrics. 2010;126:222–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Hamilton P, Restrepo E. Weekend birth and higher neonatal mortality: a problem of patient acuity or quality of care? J Obstet Gynecol Neonatal Nurs. 2003;32:724–733. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Study Characteristics for Cohorts of Off‐hour Admission and Mortality Risk
Data S1. List of references included in meta‐analysis.


