Abstract
Herein, we report a case of nontraumatic bilateral rhegmatogenous retinal detachment (RRD) during external beam radiotherapy for nonocular tumor, presented as an observational case study in conjunction with a review of the relevant literature. A 65-year-old male was referred to our hospital due to bilateral RRD. He underwent a biopsy for a tumor of the left frontal lobe 4 months prior to presentation, and the tumor had been diagnosed as primary central nerve system B-cell type lymphoma. He received chemotherapy and external beam radiotherapy for 1 month. There were no traumatic episodes. Bilateral retinal detachment occurred during a series of radiotherapies. Simultaneous nontraumatic bilateral retinal detachment is rare. The effects of radiotherapy on ocular functionality, particularly in cases involving retinal adhesion and vitreous contraction, may include RRD. Thus, it is necessary to closely monitor the eyes of patients undergoing radiotherapy, particularly those undergoing surgery for retinal detachment and those with a history of photocoagulation for retinal tears, a relevant family history, or risk factors known to be associated with RRD.
Keywords: Bilateral rhegmatogenous retinal detachment, Radiotherapy, Nonocular tumor, Side effects
Introduction
While there are various reports of rhegmatogenous retinal detachment (RRD) after radiotherapy for intraocular tumor [1,2,3], to our knowledge, only 1 case of bilateral RRD after external beam radiotherapy has previously been reported. Herein, we report a rare case of nontraumatic bilateral RRD associated with radiotherapy for malignant lymphoma in the left frontal lobe.
Case Presentation
A 65-year-old male was referred to our hospital for bilateral RRD on February 23, 2015. He noticed a lower visual field defect in his right eye 3 days prior to presentation, and an upper visual field defect in his left eye on the day of presentation. He had undergone intracranial surgery for a left frontal lobe tumor in October 2014. That tumor was diagnosed as a primary central nerve system B-cell type lymphoma (fig. 1a). He had received five courses of MPV (methotrexate, procarbazine, and vincristine) therapy and additional beam radiotherapy from January 28, 2015 onwards. On February 20, 2015, his total photon (X-ray) dose was 34 Gy, and he had received 34 Gy of irradiation to the bilateral posterior segment of his eyes (fig. 1b).
Fig. 1.
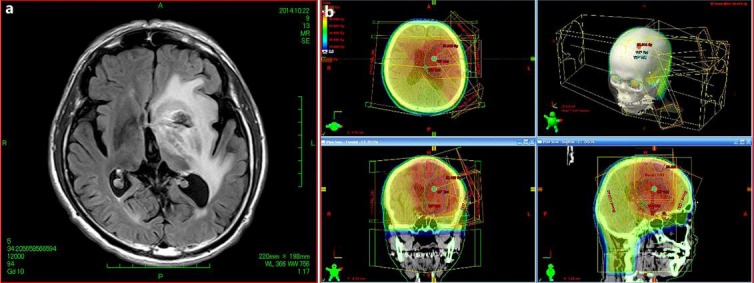
a MRI (fluid-attenuated inversion recovery) revealed intracranial tumor of the left cerebral caudate nucleus, insular gyri, white matter, and frontal lobe. b Isodose curves on a CT scan revealed the irradiation field for each eye.
The patient had a history of photocoagulation for bilateral retinal tears at another clinic. He had no family history of RRD or previous ocular trauma. His eyes were hyperopic, and his bilateral lenses were mildly cataractous. His visual acuity values were 50 cm hand motion OD and 1.2 (1.5 × S + 1.0 D Cyl-1.0 D Ax 90°) OS. His intraocular pressure measurements were 10 mm Hg (OD) and 11 mm Hg (OS). Funduscopic examination revealed a bullous, macula-sparing RRD involving the superior half of the retina, with retinal brakes consisting of 5 tears and a retinal hole in his right eye. Posterior vitreous detachment (PVD) was also apparent. In the left eye, RRD just spared the macula involving the inferior half of the retina, with breaks consisting of 2 horseshoe tears and 1 retinal hole in lattice degeneration. PVD was also evident (fig. 2a, fig. 2b). In both eyes, a vitreous body was attached to the retinal tears. Clusters of pigment cells (tobacco dust) were apparent in the vitreous body of both eyes. There was no evidence of choroidal tumor in either eye.
Fig. 2.
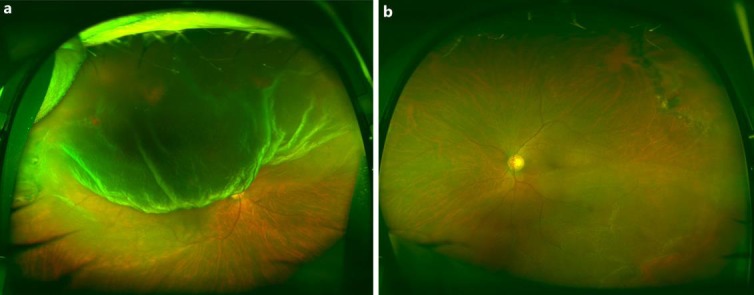
a Wide-field fundus photography of the right eye before surgery revealed the presence of bullous, macula-sparing RRD involving the superior half of the retina, with 5 tears, 1 circular hole, and PVD. b Wide-field fundus photography of the left eye before surgery revealed that RRD spared the macula but involved the inferior half of the retina, with 2 horseshoe tears, 1 circular hole, lattice degeneration, and PVD.
Radiotherapy was interrupted. Combined vitreous and cataract surgery was performed in the patient's right eye on February 25, 2015, and on March 2, 2015, the same procedure was performed in his left eye. RRD did not recur after these surgeries, and radiotherapy was resumed from March 18, 2015. The patient's vision subsequently recovered successfully, such that his visual acuity was 1.0 × S-0.75 D, Cyl-1 0 D Ax 105° (OD) and 1.0 × Cyl-1 0 D Ax 95° (OS) 1 year after the surgeries. Fundus examination and fluorescein fundus angiography (FA) showed no signs of radiation retinopathy, such as retinal hemorrhages, soft drusen, or retinal avascular areas (fig. 3a, b).
Fig. 3.
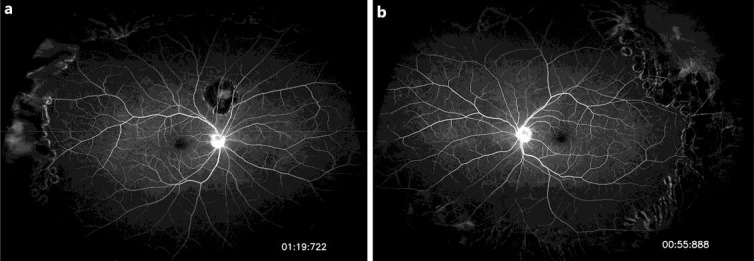
a Wide-field FA of the right eye after surgery showed no signs of radiation retinopathy. b Wide-field FA of the left eye after surgery showed no signs of radiation retinopathy.
Discussion
RRD is reportedly one of the side effects associated with the therapy of intraocular malignancies or choroidal metastasis of extraocular tumors[3,4,5]. To our knowledge, only 1 case of bilateral RRD after external beam radiotherapy has been reported by Kodjikian et al. [6]. In that report, a case of bilateral RRD after external beam radiotherapy for a carcinoma of the left maxillary sinus was described. Our case and that described by Kodjikian et al. [6] share common features. First, in both cases the patients’ ages are similar. Second, both cases had multiple retinal breaks exhibiting vitreous traction. Third, ultrasonography revealed no chorioretinal tumors in either case. Fourth, PVDs existed in both cases. The only notable difference is the timing of the occurrence of RRD. RRD occurred during a series of radiotherapies in our case, but in the case described by Kodjikian et al. [6], RRD occurred 3 weeks after a series of radiotherapies.
Several studies have investigated the effects of radiation on the retina. Alberti and El-Hifnawi [7] reported that adhesion of retinal pigmented epithelial cells to photoreceptors might be impaired by morphological changes resulting from radiation. In that study, a homogeneously distributed layer of collagen fibrils appeared on the vitreous aspect of the inner limiting membrane, and it was suggested that this may have enhanced the adhesion of the interface to the retina.
In both eyes in the case reported herein, there were complete PVDs showing vitreous traction on the retina. As far as we know, to date there have been no reports of radiation directly contributing to vitreous contraction, and little has been reported on the effects of radiotherapy on the vitreous and the vitreoretinal interface. Notably, however, Hikichi et al. [8] reported that inflammation caused vitreous gel contraction. In that study, an experimental model of ocular inflammation was induced in rabbits via the intravitreal injection of endotoxin, and subsequent vitreous changes were investigated. The study suggested that inflammation caused gel contraction and loss of elasticity, accompanied by the release of a water-like liquid from the gel, and increases in the amount of insoluble material and high-molecular-weight components of vitreous collagen; presumably due to extensive cross-links between collagen molecules. The authors surmised that cross-links between vitreous collagen may promote vitreous gel contraction and the release of a water-like liquid from the gel. We suggest that the radiation therapy may also have caused ocular inflammation, and such changes may have caused vitreous contraction. Vitreous contraction was followed by PVDs in the case reported herein, and was also reported by Kodjikian et al. [6].
Bilateral nontraumatic RRD is very rare, with an estimated occurrence rate of 2 per 1,000,000 phakic patients per year [9]. Another study reported that the incidence of bilateral RRD is 13% and that of bilateral RRD is only 1.4% [10]. RRD reportedly occurs in approximately 12 per 100,000 people per year, and is only half as prevalent in nontraumatic phakic patients [9].
The risk factors associated with RRD include high myopia, cataract surgery, advanced age, a familial history of RRD, and eye trauma. Notably, however, the patient reported herein did not fall into any of these categories. These factors suggest the possibility that our case may not have occurred coincidently and instead may have been an ocular side effect of extraocular radiotherapy. When the posterior segment of the eye is involved in the irradiation field of radiation therapy, we recommend periodic ophthalmological examinations during irradiation.
Statement of Ethics
The authors followed the code of ethics of Miyazaki University.
Disclosure Statement
The authors declare that there are no conflicts of interest with regard to the publication of this paper.
References
- 1.Lim TH, Robertson DM. Presumed rhegmatogenous retinal detachment in patients with retinoblastoma. Retina. 2000;20:22–27. doi: 10.1097/00006982-200001000-00004. [DOI] [PubMed] [Google Scholar]
- 2.Mullaney PB, Abboud EB, Al-Mesfer SA. Retinal detachment associated with type III retinoblastoma regression after cryotherapy and external-beam radiotherapy. Am J Ophthalmol. 1997;123:140–142. doi: 10.1016/s0002-9394(14)71013-x. [DOI] [PubMed] [Google Scholar]
- 3.Haimovici R, Mukai S, Schachat AP, Haynie GD, Thomas MA, Meredith TA, Gragoudas ES. Rhegmatogenous retinal detachment in eyes with uveal melanoma. Retina. 1996;16:488–496. doi: 10.1097/00006982-199616060-00004. [DOI] [PubMed] [Google Scholar]
- 4.Bovey EH, Fernandez-Ragaz A, Heon E, Balmer A, Munier FL. Rhegmatogenous retinal detachment after treatment of retinoblastoma. Ophthalmic Genet. 1999;20:141–151. doi: 10.1076/opge.20.3.141.2283. [DOI] [PubMed] [Google Scholar]
- 5.Inoue K, Numaga J, Kaji Y, Toda J, Kato S, Sakurai M, Ikeda M, Motoi N, Murakami T, Fujino Y. Bilateral uterocervical carcinoma of the squamous cell type. Am J Ophthalmol. 2000;130:682–684. doi: 10.1016/s0002-9394(00)00590-0. [DOI] [PubMed] [Google Scholar]
- 6.Kodjikian L, Garweg JG, Fleury J, Rocher F, Burillon C, Grange JD. Bilateral rhegmatogenous retinal detachment after external-beam radiotherapy: just a coincidence? Graefes Arch Clin Exp Ophthalmol. 2004;242:523–526. doi: 10.1007/s00417-004-0860-8. [DOI] [PubMed] [Google Scholar]
- 7.Alberti WE, El-Hifnawi ES. Morphologic changes after fractionated external-beam radiotherapy of minipig eyes. In: Alberti W, Sagerman R, editors. Radiotherapy of Intraocular Tumors. Berlin: Springer; 1993. pp. 400–414. [Google Scholar]
- 8.Hikichi T, Ueno N, Chakrabarti B, Trempe CL, Yoshida A. Evidence of cross-link formation of vitreous collagen during experimental ocular inflammation. Graefes Arch Clin Exp Ophthalmol. 1996;234:47–54. doi: 10.1007/BF00186518. [DOI] [PubMed] [Google Scholar]
- 9.Haimann MH, Burton TC, Brown CK. Epidemiology of retinal detachment. Arch Ophthalmol. 1982;100:289–292. doi: 10.1001/archopht.1982.01030030291012. [DOI] [PubMed] [Google Scholar]
- 10.Delaney WV, Jr, Oates RP. Retinal detachment in the second eye. Arch Ophthalmol. 1978;96:629–634. doi: 10.1001/archopht.1978.03910050325006. [DOI] [PubMed] [Google Scholar]


