To assess the effect of treatment summaries and follow-up care plans on self-efficacy and health care utilization, cancer survivors (≥65 years old) were surveyed. Receiving a verbal explanation of follow-up care instructions was significantly associated with higher self-efficacy scores, which in turn were significantly associated with lower prevalence ratios of emergency room visits and hospitalizations.
Keywords: Cancer, Survivorship, Self-efficacy, Disease management
Abstract
Background.
Treatment summaries and follow-up care plan information should be provided to cancer survivors. This study examines the association of receiving summaries and care plans with cancer survivor self-efficacy for chronic illness management, and whether self-efficacy was associated with health care utilization.
Methods.
Four hundred forty-one cancer survivors (≥2 years from diagnosis and had completed treatment) ≥65 years old from 12 cancer centers across 5 states completed telephone surveys. Survivors responded to three questions about receiving a written treatment summary, written follow-up plan, and an explanation of follow-up care plans. Respondents completed the Stanford Chronic Illness Management Self-Efficacy Scale and reported emergency room visits and hospitalizations in the past year. Three multiple linear regression models estimated the association of written treatment summary, written follow-up care plan, and verbal explanation of follow-up plan with total self-efficacy score. Log-binomial models estimated the association of self-efficacy scores with emergency room visits and hospitalizations (yes/no).
Results.
Among survivors, 40% and 35% received a written treatment summary and follow-up care plan, respectively. Seventy-nine percent received an explanation of follow-up care plans. Receiving a verbal explanation of follow-up care instructions was significantly associated with higher self-efficacy scores (β = 0.72, p = .009). Higher self-efficacy scores were significantly associated with lower prevalence ratios of emergency room visits (prevalence ratio, 0.92; 95% confidence interval, 0.88–0.97) and hospitalizations (prevalence ratio, 0.94; 95% confidence interval, 0.89–0.99).
Conclusion.
Explanation of the follow-up care plan, beyond the written component, enhances survivor self-efficacy for managing cancer as a chronic condition—an important mediator for improving health care utilization outcomes.
Implications for Practice:
Older cancer survivors (>65 years) are especially vulnerable to poor outcomes in survivorship because of the complexity of follow-up care and other chronic conditions. Delivering written treatment summaries, written follow-up care plans, and verbal explanations of follow-up care plans all independently increased the self-efficacy for chronic illness management among older survivors. In particular, delivering this information in the verbal format was significantly associated with higher self-efficacy and, subsequently, a lower likelihood of emergency room visits. Understanding the mechanism through which summaries and follow-up care plans may positively influence survivor health is critical to increasing the delivery of the information.
Introduction
Older cancer survivors are particularly vulnerable to adverse sequelae in the postcancer period, given the combined effects of aging and the consequences of cancer and its treatment [1]. This combination results in an increased risk of morbidity and downstream late effects (e.g., functional decline, management of multiple conditions) [2–4]. The physical, mental, emotional, and financial toll associated with the immediate or delayed consequences of cancer and treatment can be substantial for survivors, their families, and the health care system [5].
Given these consequences, it is not surprising that survivors have reported anxiety about leaving the cancer care system upon completion of treatment [6]. Receiving treatment summaries and survivorship care plans (SCPs) may be one strategy to reduce the anxiety by increasing survivors’ ability to self-manage while also providing information to primary care physicians (PCPs) responsible for follow-up care [7, 8]. Although there is a lack of agreement on the exact contents of SCPs, the overall goals are to provide summaries of patients’ diagnoses and treatments, inform patients of potential late effects and recommendations for ongoing care (both self-maintenance and care delivered by the health care provider), and identify resources for survivors that may be helpful for the multiple issues arising in survivorship [7, 9]. In studies of other chronic diseases, such as diabetes or arthritis, the receipt of treatment information and care planning increases patients’ self-efficacy to manage their condition and side effects, resulting in decreased health care utilization (e.g., hospitalizations and emergency room [ER] visits) [10]. Patients with higher self-efficacy for chronic illness management have confidence in their ability to manage symptoms, treatment, and physical consequences of their condition, as well as their ability to make behavioral, cognitive, or emotional changes needed to maintain quality of life and overall health [11].
Given the positive effects treatment information and follow-up plans have for other conditions, SCPs, treatment summaries, and other follow-up care information may positively influence cancer survivor self-efficacy to better manage their cancer as a chronic condition. However, summaries and follow-up care plan uptake has been limited in the United States. Logistical issues and resource constraints are contributing factors, as is the lack of empirical evidence demonstrating a change in patient outcomes [12, 13]. The present study aims to contribute evidence on the association of postcancer treatment summaries and follow-up information with survivors’ self-efficacy for chronic illness management. Specifically, we examined how receiving treatment summaries and follow-up care information, both written and verbal, may be associated with self-efficacy and the relationship with health care utilization. Additionally, we conducted exploratory mediation and moderation analyses to generate future hypotheses on the mechanism through which these different components are related to self-efficacy and health care use.
Methods
Study Population
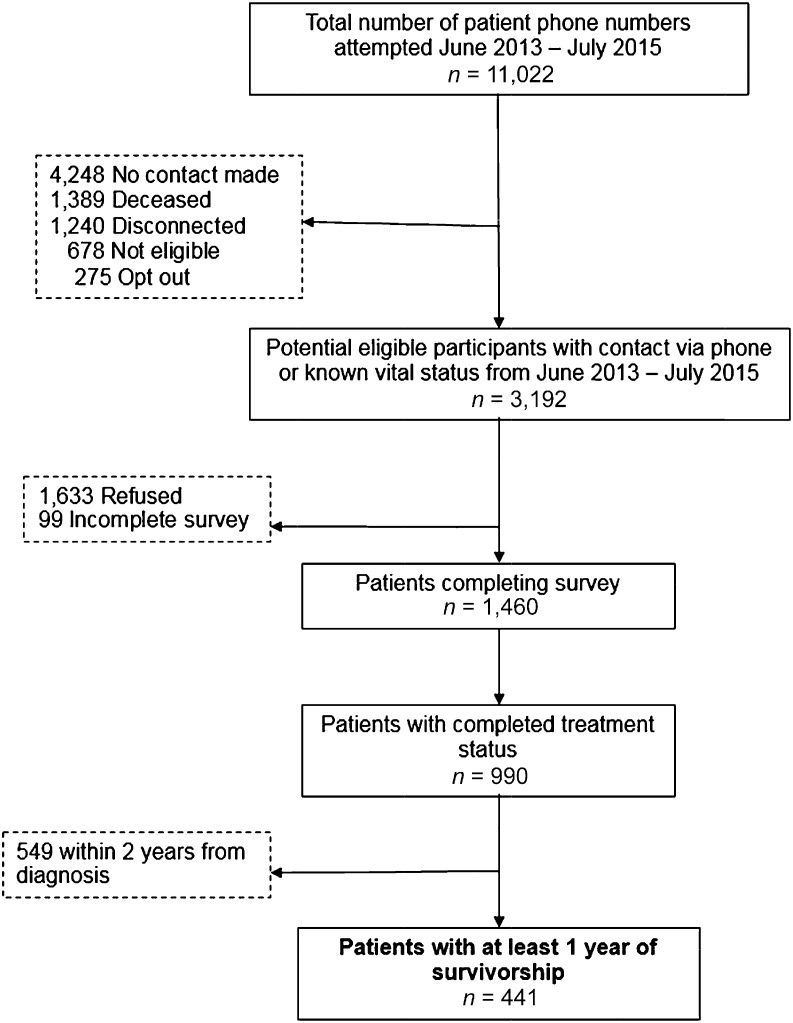
From June 2013 to July 2015, individuals aged 65 years and older with a cancer diagnosis after January 1, 2008, were identified from within the University of Alabama at Birmingham Health System Cancer Community Network (CCN). The CCN includes 12 different hospitals across Alabama, Georgia, Tennessee, Mississippi, and Florida. Registry data were used to ascertain contact information on potentially eligible participants to complete a telephone survey. The survey included questions on the receipt of treatment summaries and follow-up care plans, chronic illness management self-efficacy, and health care utilization, as well as questions on demographics, social support, quality of life, symptoms, and financial issues. Figure 1 outlines the sample selection process. Overall, of the eligible patients contacted (n = 3,192), 1,460 completed the survey (46% completion rate). For this analysis, we included those who completed treatment (n = 990) and were ≥2 years from diagnosis (n = 441). The institutional review boards at the University of Alabama at Birmingham and each CCN site approved the study.
Figure 1.
Survey response and sample selection.
Treatment Summary and Follow-Up Care Plan
The study’s three primary explanatory variables included the following items: “Did any doctor, nurse, or other health professional (1) ever give you a written summary of all the cancer treatments that you received? (2) ever give you a written summary of the plan for follow-up care? and (3) explain the plan for follow-up care?” (yes/no response option).
Self-Efficacy
The Stanford Chronic Illness Self-Efficacy scale is a six-item scale measuring a person’s confidence in their ability to manage health conditions [14]. Question stems referred specifically to conditions or symptoms caused by cancer or treatment. The first question stem asked, “How confident are you that you can keep [blank] caused by your cancer/treatment from interfering with things you want to do?” Respondents answered this question stem for “fatigue,” “physical discomfort/pain,” “emotional distress,” and “symptoms/health problems.” The second question stem asked, “How confident are you that you can do the [blank] needed to manage your health condition so as to reduce your need to see a doctor?” Respondents answered this question stem for “different tasks/activities” and “things other than just taking medication.” Response options were on a scale from 1 to 10, where 1 = “not confident” and 10 = “totally confident.” Responses were summed to create an overall self-efficacy score.
Health Care Use
Survivors were asked if they had (a) been seen in an ER in the past year and (b) whether they had been hospitalized (spent at least one night in the hospital) in the past year.
Covariates
Demographic information obtained included age at time of survey, race, sex, education, annual household income, and marital status. Clinical information derived from hospital data included cancer type, time from diagnosis, and cancer stage. Because of high rates of missing data, the stage variable was categorized as 0/1, II–IV, and missing/unknown for analyses. Comorbidity was extracted from Medicare claims, and scoring was based on Surveillance, Epidemiology, and End Results, Medicare’s calculation of comorbidity weights [15]. A categorical variable was create to indicate 0, 1, or 2+ on the index scale. Of the 441 survivors, 122 had at least one contact with a cancer navigation program.
Primary Analysis
Frequencies, means, and SDs were calculated for categorical and continuous variables, respectively. In addition to examining the frequency of each of the three information items (written treatment summary, written follow-up care plan, explanation of follow-up care plan), we evaluated whether survivors received none or all three pieces of information.
Three multiple linear regression models estimated the association between each of the primary independent variables (three information items) and the dependent variable, total self-efficacy score. Covariates for each model included age, sex, race (minority versus non-Hispanic white), education, income, marital status, stage at diagnosis, time since diagnosis, and comorbidity (0 versus ≥1).
We estimated prevalence ratios (PRs) and 95% confidence intervals (CIs) for ER visits and hospitalizations in the past year using log-binomial models (ER visits) and Poisson regression models with robust variance if log-binomial models did not converge (hospitalizations) [16, 17]. We estimated three models each for ER visits and hospitalization as dependent variables. The total self-efficacy score was included in all models, and the variables indicating receiving a treatment summary, written follow-up care plan, and explanations of follow-up care plan were included separately. All models controlled for age, sex, race (minority versus nonminority), education, income, marital status, stage at diagnosis, time since diagnosis, and comorbidity (0 versus ≥1).
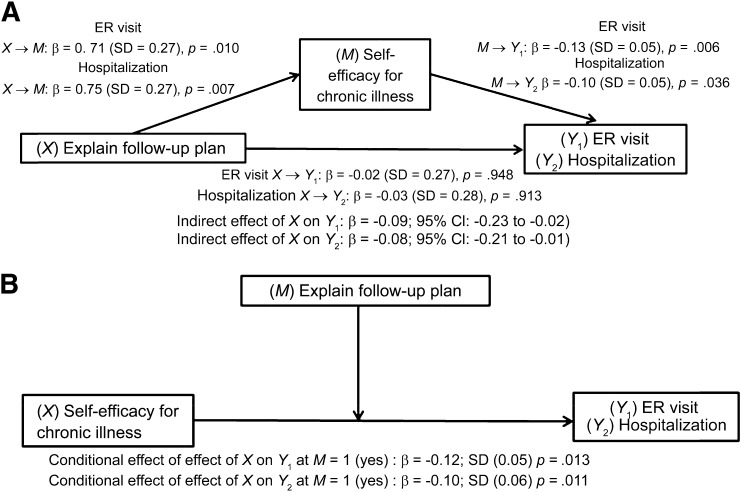
Exploratory Analyses
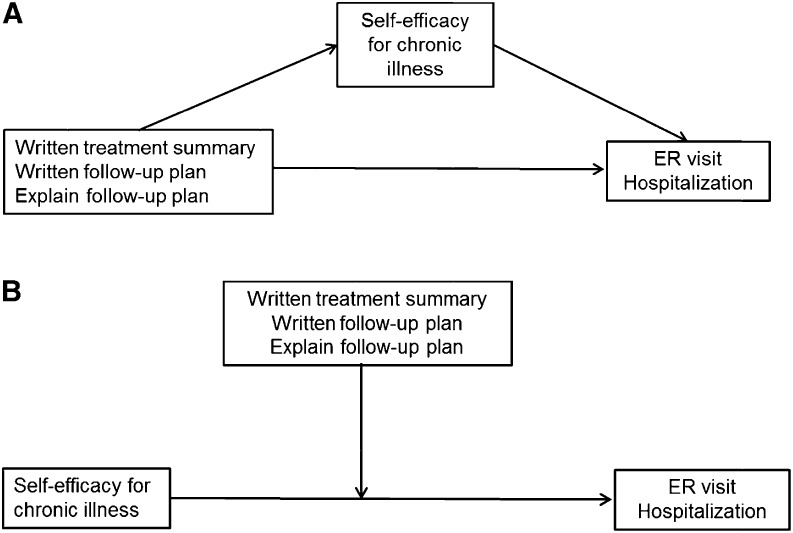
Mediation analysis was used to examine how receiving treatment summaries or follow-up care plan information may influence health care utilization (ER or hospitalization). Mediation analyses allows us to estimate the direct associations, or relationship, between two variables (X→Y), as well as the indirect effect through another variable (X→M→Y). In our model, the indirect effect is the association of one of the explanatory variables (X) with health care utilization (Y) through self-efficacy (M). For example, we hypothesize that receiving a verbal explanation of follow-up care plans may be directly associated with decreased ER visits. It may also be indirectly associated with decreased ER visits through its association with higher self-efficacy scores (Fig. 2A). Following approaches outlined by Hayes [18], MacKinnon et al. [19], and Preacher and Hayes [20], we used the PROCESS macro for mediation and moderation analyses. Self-efficacy (M) is estimated from the variable for receiving follow-up care plans (X) to health care utilization while controlling for covariates (Fig. 2A). Indirect effects are estimated as the product of the coefficients linking X to M and X to Y [19, 20].
Figure 2.
Study models. (A): Mediation model. (B): Moderator model.
Abbreviation: ER, emergency room.
Second, we modeled the receipt of treatment summaries/follow-up care information as a moderator of the relationship between self-efficacy and health care utilization (Fig. 2B). This model hypothesizes that a level of self-efficacy is present, and that receiving a treatment summary/follow-up care information may plausibly increase, or moderate, the level of self-efficacy, resulting in a decreased risk of ER visits or hospitalizations.
Post Hoc Analysis
We conducted a post hoc analysis of the regression models in which we stratified by comorbidity score (0 versus ≥1). This allowed an examination of the impact of the receipt of treatment summaries, written follow-up care plans, and explanation of follow-up care plans on both self-efficacy and health care utilization among those with and without additional comorbidities to manage.
Results
Population
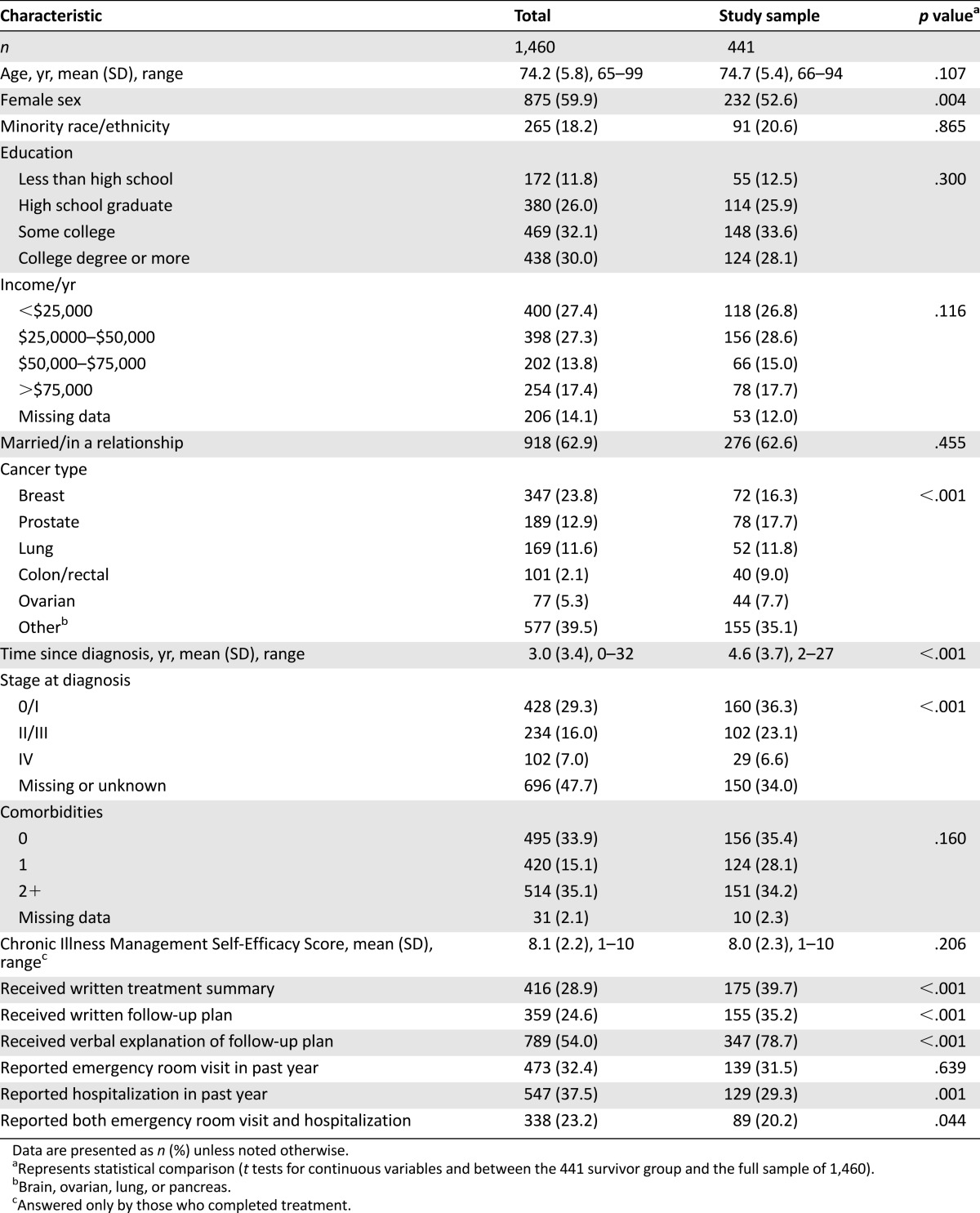
The mean age at survey of our sample was 74.7 years, and 60% of respondents were female (Table 1). More than half of the sample reported ≤$50,000 annual income, and 49% had a high school degree or less. The most frequent cancer type was prostate, followed by breast. The average time from diagnosis was 4.6 years, and ∼36% were diagnosed at stage 0 or I. This was significantly more than the proportion of the overall sample diagnosed at stage 0/1 (36% vs. 29%, p < .001). The analytic sample had more prostate, colorectal, and ovarian cancer survivors (p < .001) and fewer females (p = .004) than the overall sample.
Table 1.
Sample characteristics
The mean self-efficacy score was 8.1 (SD 2.2). Approximately 40% of survivors reported receiving a written treatment summary, and 35% received a written summary of the follow-up care plan (33% received both). However, 79% of the sample reported receiving a verbal explanation of the follow-up care plan. One quarter of survivors received all three. One-third reported an ER visit, 29% reported a hospitalization, and 20% reported both.
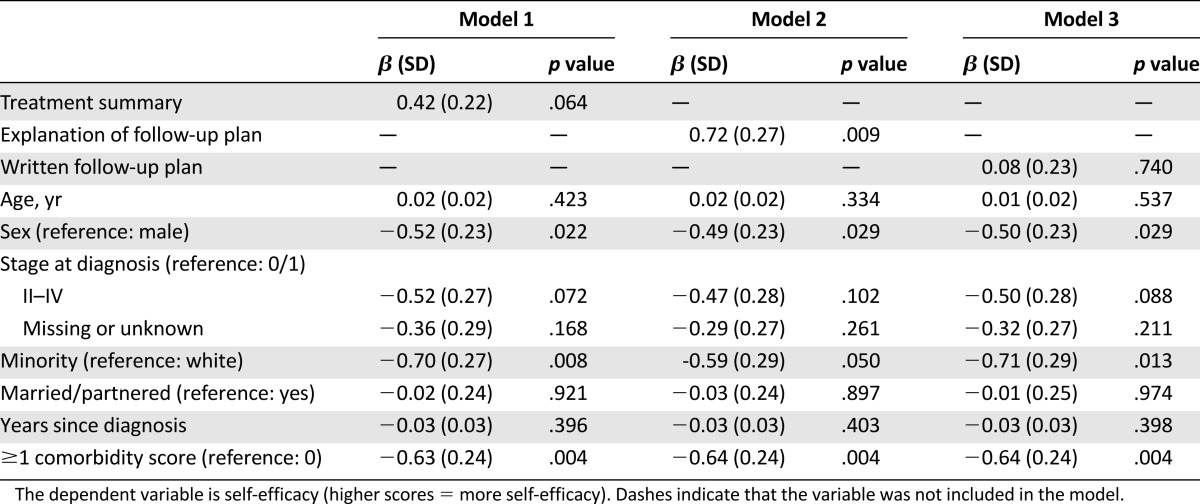
Self-Efficacy
Table 2 shows the results of the three linear regression models. Model 2 with verbal explanation of follow-up care plans was the only one of the three primary variables that was significantly associated with higher self-efficacy scores in the adjusted model (β = 0.72, SD = 0.27, p = .009). Female sex, minority race/ethnicity, and comorbidity score of at least 1 were associated with significantly lower self-efficacy scores in all three models.
Table 2.
Linear regression models: receiving treatment summaries and follow-up care plan instructions and self-efficacy
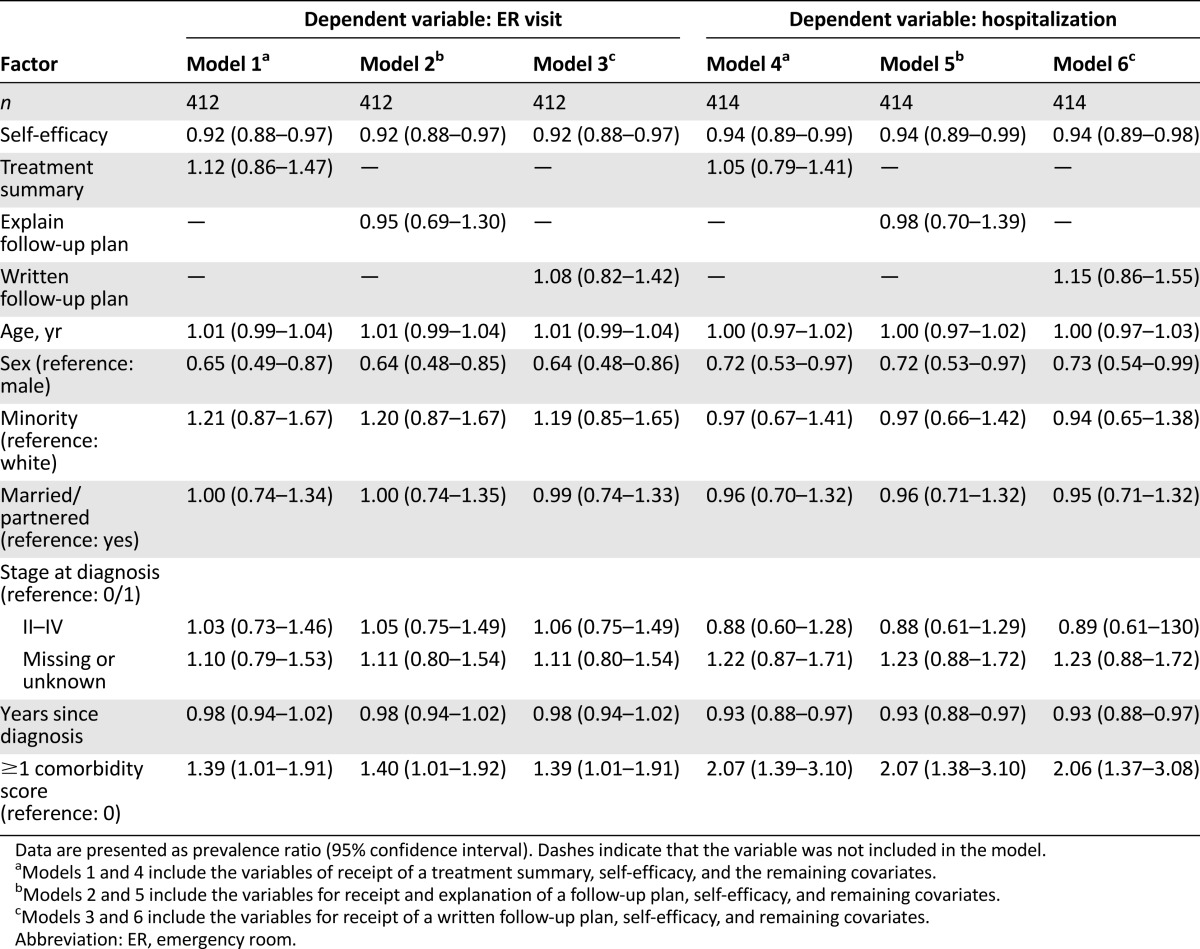
ER and Hospitalization
Higher self-efficacy scores were associated with significantly lower risk of ER and hospitalizations in the past year across all three models for each of the two dependent variables (Table 3). PRs were similar for ER visits, at 0.82 (95% CI 0.88–0.97), and for hospitalizations, at 0.94 (95% CI 0.89–0.99). Treatment summaries and verbal or written instructions of follow-up care plans were not significantly associated with ER visits or hospitalizations in the fully adjusted model. Females had a lower likelihood of reporting ER visits or hospitalizations consistently across all models. Those with a comorbidity score of ≥1 were more likely to report ER visits (PR 1.39 [95% CI 1.01–1.91]) and hospitalizations (PR 2.07 [95% CI 1.38–3.10]) across all three models.
Table 3.
Prevalence ratios for likelihood of reporting and ER visit or hospitalization
Exploratory Analyses
Figure 3 displays results of the exploratory analyses. In the two mediation analyses including verbal explanation as the primary independent variable (X), the indirect effects on ER visits and hospitalizations were significant through self-efficacy (β = −0.09 [95% CI −0.23 to −0.02] and β = −0.08 [95% CI −0.21 to −0.01], respectively). In the mediation analyses using treatment summary and written follow-up care plan as mediators (results not presented), both were significantly directly associated with self-efficacy, but the direct and indirect effects from treatment summary or written follow-up care plan to ER visits and hospitalization were not significant.
Figure 3.
Exploratory analysis results for the models with explanation of follow-up care plan. (A): Mediation. (B): Moderation.
Abbreviation: ER, emergency room.
In the moderation analyses, verbal explanation of the follow-up care plan significantly moderated the relationship between self-efficacy and ER visits (conditional effect of X on Y at M = 1, β = −0.12, p = .024), but not hospitalization (β = −0.10, p = .080) (Fig. 3B). Survivors with low self-efficacy (≤1 SD below the mean self-efficacy score) and who received the verbal explanation had a 0.37 probability of reporting an ER visit compared with a 0.40 probability of those with low self-efficacy who did not receive the explanation. Treatment summaries and written follow-up plans did not significantly moderate the relationship between self-efficacy and ER visits or hospitalizations (results not presented).
Post Hoc Results
In the stratified analyses, among those with a comorbidity score ≥1, written treatment summary, written follow-up care plan, and explanation of care plan were more strongly associated with higher self-efficacy in the linear regression models. Among the group with no comorbidity, the relationships between treatment summary, written follow-up care plan, and verbal explanation were nonsignificant.
Discussion
Less than 40% of older cancer survivors in our sample reported receiving a written treatment summary or a written follow-up care plan. Whereas a national survey reports that 38% and 58% of survivors reported written treatment and follow-up information, respectively, comparisons may not be equivalent given the regional nature of our data (i.e., southeast) [21]. In contrast, ∼79% of survivors in our study received a verbal explanation of the follow-up care plan. Receiving the verbal explanation of the follow-up care plan was associated with higher self-efficacy scores and with a decreased likelihood of ER visits and hospitalizations. Furthermore, the exploratory mediation analyses supported the possibility of a positive relationship between receiving the verbal explanation of the follow-up care plan and decreased health care utilization through the relationship with higher self-efficacy. These trends, however, were not observed for written treatment summaries or written follow-up care plans.
Despite the relatively low frequency of the written components, both of those components, along with the verbal explanation, were associated with increased self-efficacy, adding evidence to the limited body of literature on treatment summaries and care plans. Of the few studies conducted, results from a randomized trial of SCP versus usual care delivery in the Netherlands found that although cancer survivors in the SCP arm reported receiving more information about treatment and doing things to help themselves recover compared with the usual care arm, they also reported more concern about their illness and more cancer-related visits with their PCP [22]. Because the study did not assess survivor self-efficacy or confidence in the ability to manage cancer, it is unclear whether the increased concern and PCP contact was proactive management of symptoms and problems or whether these were concerns and doctor visits resulting from the lack of self-management or lack of confidence to self-manage. Another study using the Web-based LIVESTRONG Care Plan [23] assessed whether the care plan prompted survivors to change the way they participate in their health care (61% said yes) and whether it helped them communicate with health care providers (80% said yes) [24]. The study also reported on survivor-reported changes in behaviors, most notably improvements in diet and exercise. Although these are not direct assessments of self-efficacy, the LIVESTRONG study findings suggest that the information provided to the survivors assisted them in their health care. In contrast with our study, however, the information associated with these changes was in a written format (Web-based delivery). The population under study was substantially younger than our study sample, with a mean age of 52 versus 75 years, possibly indicating that older survivors may require face-to-face or verbal delivery of this information to have an impact. Furthermore, the population was more highly educated and contained fewer minorities compared with our sample.
In addition to managing cancer as a chronic condition, most of our older survivors had a comorbidity score of at least 1 (65%), and many had a score of 2 or more (34%). This additional morbidity was, unsurprisingly, highly negatively associated with self-efficacy and positively associated with health care utilization. The post hoc results suggest that this high-risk group may stand to benefit most from treatment summaries and follow-up care plan information (both verbal and written). This is consistent with findings from studies on self-management of other chronic conditions.
Limitations of this study include the reliance on self-report of receiving treatment summaries, follow-up care information, and health care utilization. However, patient perception is an important indicator of information received. Patient recollection of verbal information may be a surrogate for an unmeasured variable, such as quality of relationship with the oncology provider, which may influence self-efficacy. We also do not know the specific contents of the summaries or care plans received, and plans that were received were not standardized across sites. Importantly, the data are cross-sectional; therefore, our mediation and moderation analyses are strictly hypothesis generating, and no causal conclusions can be made. Furthermore, we do not have information on the reasons for the ER visits or hospitalizations, the lack of which limits inferences we can make on the relationship between self-efficacy and decreased ER visits. Along these same lines, ER visits may also be related to PCP experience (essentially, if the physician instructs the survivor to go to the ER to address a complicated health issue). This study was designed to identify a preliminary association between treatment summaries, follow-up care plans, self-efficacy, and health care use. Given those associations, additional study, preferably through randomized trial, is needed to strategically assess the delivery of treatment summaries and care plans and the downstream effects on health care use.
Our findings have several important contributions. First, treatment summary and follow-up care plan evaluation has been largely skewed toward qualitative studies involving interviews and focus groups of patients and physicians. This previous research provides rich information on patient and physician preferences and personal experiences, but lacks the external validity to broad groups of patients and the impact of care transition efforts. The few recent quantitative studies examining these issues have been either homogeneous populations [22] or much younger than the population presented in our study (mean age of 52 versus 75 years [24]). Thus, our study provides much-needed data on the population of older survivors who are traditionally understudied, yet comprise the majority of cancer patients. Second, examining the impact of treatment summaries and follow-up care plans on survivor self-efficacy gives a new perspective on how the components and delivery of treatment summaries and follow-up care plans may influence survivor behavior and health outcomes. We also provide a new pathway for future studies or practice implementation (i.e., delivering verbal explanation of follow-up care plans) by generating new hypotheses on how survivor self-efficacy may be a measurable target to decrease ER visits or hospitalizations long-term. Finally, we identify a high-risk group comprising survivors with at least one comorbid condition that stand to benefit most in self-efficacy for chronic illness management.
Although less than 40% of survivors received written components of treatment summaries or care plans, these two pieces are limited in their association with self-efficacy for chronic illness management in our study and, subsequently, on the relationship between self-efficacy and health care utilization. Future research directions include examining the components of the follow-up care plan that may help survivors, identifying strategies to integrate verbal explanations into care (e.g., which health care provider can deliver the explanation), and improving the written components to increase effectiveness for survivors’ self-efficacy.
Acknowledgments
This project was supported by grant 1C1CMS331023 from the Department of Health and Human Services, Centers for Medicare and Medicaid Services. The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the U.S. Department of Health and Human Services or any of its agencies. The research presented here was conducted by the awardee. Findings might or might not be consistent with or confirmed by the findings of the independent evaluation contractor. K.M. Kenzik was supported by grants T32HS013852 and K12HS023009 from the Agency for Healthcare Research and Quality. This article's content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality. Additional support for project development was provided by the UAB Comprehensive Cancer Center grant P30CA013148. We thank the entire evaluation team for their support on the CMS Innovation Grant, including Richard Taylor, Aras Acemgil, Yufeng Li, Xuelin Li, Chen Dai, Cynthia Y. Johnson, Cynthia Flanigan, Carol Chambless, and Mona Fouad.
Author Contributions
Conception/Design: Kelly M. Kenzik, Elizabeth A. Kvale, Gabrielle B. Rocque, Wendy Demark-Wahnefried, Michelle Y. Martin, Bradford E. Jackson, Karen Meneses, Edward E. Partridge, Maria Pisu
Provision of study material or patients: Elizabeth A. Kvale, Gabrielle B. Rocque, Wendy Demark-Wahnefried, Edward E. Partridge, Maria Pisu
Collection and/or assembly of data: Kelly M. Kenzik, Elizabeth A. Kvale, Gabrielle B. Rocque, Wendy Demark-Wahnefried, Bradford E. Jackson, Karen Meneses, Edward E. Partridge, Maria Pisu
Data analysis and interpretation: Kelly M. Kenzik, Elizabeth A. Kvale, Gabrielle B. Rocque, Wendy Demark-Wahnefried, Michelle Y. Martin, Bradford E. Jackson, Karen Meneses, Edward E. Partridge, Maria Pisu
Manuscript writing: Kelly M. Kenzik, Elizabeth A. Kvale, Gabrielle B. Rocque, Wendy Demark-Wahnefried, Michelle Y. Martin, Bradford E. Jackson, Karen Meneses, Edward E. Partridge, Maria Pisu
Final approval of manuscript: Kelly M. Kenzik, Elizabeth A. Kvale, Gabrielle B. Rocque, Wendy Demark-Wahnefried, Michelle Y. Martin, Bradford E. Jackson, Karen Meneses, Edward E. Partridge, Maria Pisu
Disclosures
Elizabeth A. Kvale: Aspire Healthcare (OI); Gabrielle B. Rocque: Medscape, PackHealth, Carevive (RF), Medscape (H). The other authors indicated no financial relationships.
(C/A) Consulting/advisory relationship; (RF) Research funding; (E) Employment; (ET) Expert testimony; (H) Honoraria received; (OI) Ownership interests; (IP) Intellectual property rights/inventor/patent holder; (SAB) Scientific advisory board
References
- 1.Rowland JH, Bellizzi KM. Cancer survivorship issues: Life after treatment and implications for an aging population. J Clin Oncol. 2014;32:2662–2668. doi: 10.1200/JCO.2014.55.8361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bender CM, Engberg SJ, Donovan HS, et al. Symptom clusters in adults with chronic health problems and cancer as a comorbidity. Oncol Nurs Forum. 2008;35:E1–E11. doi: 10.1188/08.ONF.E1-E11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cohen HJ, Lan L, Archer L, et al. Impact of age, comorbidity and symptoms on physical function in long-term breast cancer survivors (CALGB 70803) J Geriatr Oncol. 2012;3:82–89. doi: 10.1016/j.jgo.2012.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hays RD, Reeve BB, Smith AW, et al. Associations of cancer and other chronic medical conditions with SF-6D preference-based scores in Medicare beneficiaries. Qual Life Res. 2014;23:385–391. doi: 10.1007/s11136-013-0503-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mohile SG, Xian Y, Dale W, et al. Association of a cancer diagnosis with vulnerability and frailty in older Medicare beneficiaries. J Natl Cancer Inst. 2009;101:1206–1215. doi: 10.1093/jnci/djp239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jefford M, Karahalios E, Pollard A, et al. Survivorship issues following treatment completion—Results from focus groups with Australian cancer survivors and health professionals. J Cancer Surviv. 2008;2:20–32. doi: 10.1007/s11764-008-0043-4. [DOI] [PubMed] [Google Scholar]
- 7.Hewitt M, Greenfield W, Stovall E, editors. From Cancer Patient to Cancer Survivor: Lost in Transition. Washington, D.C.: National Academies Press; 2006. [Google Scholar]
- 8.Mayer DK, Nekhlyudov L, Snyder CF, et al. American Society of Clinical Oncology clinical expert statement on cancer survivorship care planning. J Oncol Pract. 2014;10:345–351. doi: 10.1200/JOP.2014.001321. [DOI] [PubMed] [Google Scholar]
- 9.Salz T, Oeffinger KC, McCabe MS, et al. Survivorship care plans in research and practice. CA Cancer J Clin. 2012;62:101–117. doi: 10.3322/caac.20142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lorig KR, Sobel DS, Ritter PL, et al. Effect of a self-management program on patients with chronic disease. Eff Clin Pract. 2001;4:256–262. [PubMed] [Google Scholar]
- 11.Barlow J, Wright C, Sheasby J, et al. Self-management approaches for people with chronic conditions: A review. Patient Educ Couns. 2002;48:177–187. doi: 10.1016/s0738-3991(02)00032-0. [DOI] [PubMed] [Google Scholar]
- 12.Grunfeld E, Julian JA, Pond G, et al. Evaluating survivorship care plans: Results of a randomized, clinical trial of patients with breast cancer. J Clin Oncol. 2011;29:4755–4762. doi: 10.1200/JCO.2011.36.8373. [DOI] [PubMed] [Google Scholar]
- 13.Stricker CT, Jacobs LA, Palmer SC. Survivorship care plans: An argument for evidence over common sense. J Clin Oncol. 2012;30:1392–1393; author reply 1393–1395. doi: 10.1200/JCO.2011.40.7940. [DOI] [PubMed] [Google Scholar]
- Lorig K, Stewart A, Ritter P et al. Stanford chronic disease self-management study. In: Outcome Measures for Health Education and Other Health Care Interventions. Thousand Oaks, CA: Sage Publications; 1996:24–25, 41–45.
- 15.Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 16.Coutinho LM, Scazufca M, Menezes PR. Methods for estimating prevalence ratios in cross-sectional studies. Rev Saude Publica. 2008;42:992–998. [PubMed] [Google Scholar]
- 17.Petersen MR, Deddens JA. A comparison of two methods for estimating prevalence ratios. BMC Med Res Methodol. 2008;8:9. doi: 10.1186/1471-2288-8-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hayes AF. PROCESS: A versatile computational tool for observed variable mediation, moderation, and conditional process modeling. White paper. 2012. Available at http://www.afhayes.com/public/process2012.pdf. Accessed November 28, 2015.
- 19.MacKinnon DP, Fairchild AJ, Fritz MS. Mediation analysis. Annu Rev Psychol. 2007;58:593–614. doi: 10.1146/annurev.psych.58.110405.085542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behav Res Methods Instrum Comput. 2004;36:717–731. doi: 10.3758/bf03206553. [DOI] [PubMed] [Google Scholar]
- 21.Sabatino SA, Thompson TD, Smith JL, et al. Receipt of cancer treatment summaries and follow-up instructions among adult cancer survivors: Results from a national survey. J Cancer Surviv. 2013;7:32–43. doi: 10.1007/s11764-012-0242-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nicolaije KAH, Ezendam NPM, Vos MC, et al. Impact of an automatically generated cancer survivorship care plan on patient-reported outcomes in routine clinical practice: Longitudinal outcomes of a pragmatic, cluster randomized trial. J Clin Oncol. 2015;33:3550–3559. doi: 10.1200/JCO.2014.60.3399. [DOI] [PubMed] [Google Scholar]
- 23.Hill-Kayser CE, Vachani C, Hampshire MK, et al. An internet tool for creation of cancer survivorship care plans for survivors and health care providers: Design, implementation, use and user satisfaction. J Med Internet Res. 2009;11:e39. doi: 10.2196/jmir.1223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hill-Kayser CE, Vachani CC, Hampshire MK, et al. Impact of internet-based cancer survivorship care plans on health care and lifestyle behaviors. Cancer. 2013;119:3854–3860. doi: 10.1002/cncr.28286. [DOI] [PubMed] [Google Scholar]