Abstract
A 22-year-old male patient underwent a segmental resection of the ileum due to clinical symptoms of bowel obstruction and radiological evidence of ileal wall thickening and enlarged mesenteric nodes. Histopathological examination of the resected specimen revealed an extranodal marginal zone B-cell lymphoma(MALToma) of the intestine and tuberculous lesions along with a solitary Peutz-Jeghers polyp. The case is presented for its rarity and to stress upon the clinical and radiological challenges that arise when lymphomas and tuberculous lesions co-exist at the same site.
KEY WORDS: Intestinal lymphoma, MALToma, marginal zone lymphoma, Peutz-Jeghers polyp, tuberculosis
Introduction
MALToma (lymphoma of mucosa-associated lymphoid tissue) of the gastrointestinal tract most commonly occurs in the stomach. Malignant tumors of the lymphoreticular system depress the body's T-cell immunity that may predispose the patient to several infections especially chronic ones such as tuberculosis. We present in this paper, a case of intestinal MALToma which was an extranodal marginal zone B-cell lymphoma of the small intestine along with tuberculosis in a young male patient that presented a confusing picture on clinical as well as on radiological grounds. Though such a condition is documented in literature, the additional presence of a solitary Peutz-Jeghers polyp makes it a rare entity.
Case Report
A 22-year-old male patient was admitted in the surgery ward with symptoms of bowel obstruction. He had a history of vomiting and abdominal distention since 10 days. The patient had experienced similar complaints on and off for the past year. On examination, the patient's abdomen was distended and a vague swelling was noted in the umbilical region. The baseline investigations were normal with only a rise noted in the patient's erythrocyte sedimentation rate which was 70 mm at 30 minutes and 118 mm at the end of 1hour. His Mantoux tested negative. An X-ray abdomen showed multiple fluid levels and a contrast-enhanced CT scan revealed ileal wall thickening and mesenteric nodes. The surgeon proceeded with a laparotomy and resected a segment of ileum with omental adhesions and sent for histopathological examination.
The cut open small intestinal segment measured 34 × 6 cm. A polyp of 1.5 cm diameter was noted 18 cm from the proximal end. Two ulcers were identified, the first measuring 2 × 2.5 cm was 14 cm from the proximal end and the second, measuring 2 × 1.5 cm was 20cm from the proximal end. Both ulcers were shallow, situated along the horizontal plane, with undermined edges and a fibrotic base. A stricture was present 9cm from the distal end with dilatation of the proximal segment. The serosa showed large lymph nodes measuring 4 × 5 cm, whose cut section was whitish and creamy in consistency. The areas adjacent to the ulcers showed diffuse thickening of the wall and on cut section revealed a whitish mass extending from the submucosa upto the serosa. Representative sections from each of the grossly abnormal areas and the resected margins were submitted for processing.
Sections from the polyp showed a polypoidal mass with a core containing smooth muscle fibers and was identified as a Peutz-Jeghers polyp. Sections from the ulcerated areas showed edematous lamina propria with a dense infiltration of eosinophils and lymphocytes with congested blood vessels in the submucosa and a dense lymphocytic infiltration in the muscularis propria [Figure 1] and serosa. Sections from the lymph node showed partial loss of architecture, areas of necrosis and fibrosis with epithelioid cell aggregates but no definite granuloma was made out. Multiple sections from the thickened areas showed diffuse sheets of lymphocytes ulcerating the mucosa and infiltrating transmurally upto the serosa and periserosal fat. Rest of the mucosa showed focal erosions, increased eosinophilic and lymphocytic infiltrates in the lamina propria and increased intra-epithelial lymphocytes with focal shortening of villi. In view of the high suspicion of tuberculosis and lymphoma, further diagnostic modalities were sought after such as acid fast staining, polymerase chain reaction (PCR) and immunohistochemistry.
Figure 1.
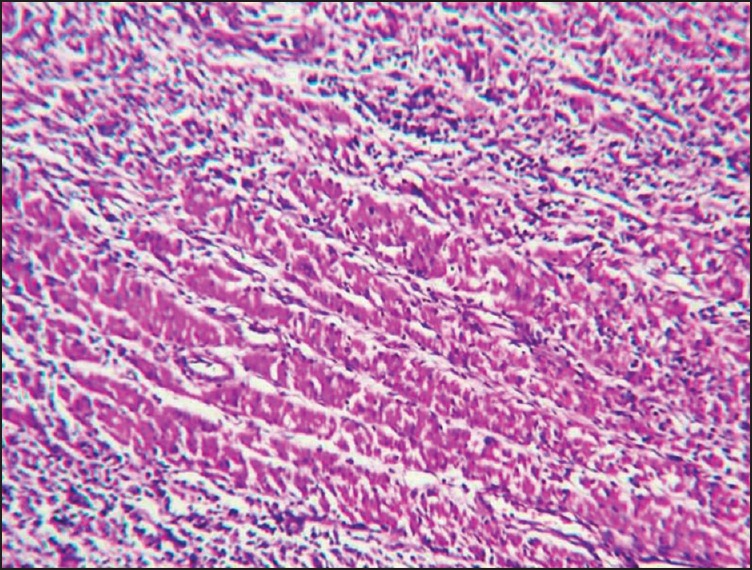
Lymphocytes infiltrating the muscularispropria H&E 100×
Ziehl–Neilson acid fast staining revealed numerous acid fast bacilli. The PCR was positive for tubercle bacilli. A lymphoma panel of immunohistochemical markers showed CD 45 and CD 20 positivity [Figure 2] with weak positivity for Bcl2. The rest of the IHC markers such as cytokeratin, chromogranin, CD 3 and CD 10 were negative.
Figure 2.

CD 20 positive lymphocytic proliferation 100×
Thus, a final diagnosis of primary small intestinal B-cell lymphoma, tuberculosis and Peutz-Jeghers polyp was made.
Discussion
Extranodal marginal zone B-cell lymphoma of mucosa-associated lymphoid tissue or MALToma as in common parlance is commonly encountered in the gastrointestinal tract in the setting of chronic inflammatory disorders such as Helicobacter pylori-induced chronic gastritis and autoimmune disorders. An accumulation of lymphocytes in the extranodal tissue due to these disease processes is implicated in the pathogenesis of MALToma.[1,2] This is usually a disease of elderly adults with a female preponderance.
A primary gastrointestinal lymphoma has to satisfy five criteria laid down by Dawson[3] which include:
Absence of peripheral lymphadenopathy at the time of presentation,
Lack of enlarged mediastinal lymph nodes,
Normal total and differential white blood cell count,
Predominance of bowel lesion at the time of laparotomy with only lymph nodes obviously affected in the immediate vicinity and,
No lymphomatous involvement of liver and spleen. And all these criteria were satisfied in our case too.
Tuberculosis is very common in India and abdominal tuberculosis may result in transverse intestinal ulcers or an ileocaecal mass that may mimic other malignant mass lesions. Thus, confusion arises while evaluating a patient based on clinical history, examination findings and imaging findings. The problems in diagnosis of tuberculosis or cancer was extensively researched upon by Falagas et al.[4] who in one study presented 17 case reports where malignancy mimicked mycobacterial infections. The main findings of the clinical and radiological examination had indicated a tubercular infection but the histopathological results revealed a malignant tumor. They also made an interesting observation that the tuberculin skin test or Mantoux test was often false negative in patients suffering from diseases affecting the lymphoid organs such as Hodgkin's disease, lymphoma and chronic leukemia. The authors concluded that:
Tuberculosis infection may be associated with the subsequent development of cancer,
Tuberculosis and malignancy may co-exist in some cases and,
Similarities in clinical and radiological presentations between tuberculosis and malignancy might mislead diagnosis.
Several authors[5] have reported co-existent lymphoma and tuberculosis in the same patient with diagnostic confusion arising from clinical and radiological findings put to rest only by a detailed histopathological examination of the biopsy material.
Melero et al.[6] studied 506 cases of lymphomas and observed that in biopsy material in which Mycobacterium tuberculosis was isolated, neither epithelioid cell granulomas with caseation necrosis nor acid-fast bacilli were histopathologically documented.
Sporadic Peutz-Jeghers polyps carry the same increased risk of GI malignancy as Peutz-Jeghers syndrome and have been reported as a rare occurrence in the medical literature.[7] Pieter et al[8] have reported a case of solitary Peutz-Jeghers polyp of the jejunum in a 19-year-old male patient. Recently, co-existent MALToma and Peutz-Jeghers syndrome was reported in a young patient which highlights the importance of life-long screening of patients with hamartomatous polyps for identification of additional malignancies.[9]
A multimodality workup is thus indicated in cases with features suspicious of co-existent tuberculosis and lymphoma as definite diagnosis can be provided only after histopathological examination.
Acknowledgments
The authors wish to thank Dr. Sasikumar, Dr. Ravishankar and Dr. Yogeshwaran, Department of Surgery, SreeBalaji Medical College and Hospital for the case details and surgical specimen, Dr. Bheema Rao G and Dr. Priavadhana for their guidance and valuable inputs, Dr. D.P. Dinisha and Dr. E.Harish Kumar for the photographs, Mrs.Subhasini and Mr.Srinivasan, for processing and staining of the tissue sections and Dr. Godfred and his team for help with PCR.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Isaacson PG, Berger F, Müller-Hermelink HK, Nathwani BN, Piris MA, Swerdlow SH, et al. In: Pathology and Genetics of Tumours of Hematopoietic and Lymphoid Tissues. Jaffe ES, Harris NL, Stein H, Vardiman JW, editors. Lyon: IARC Press; 2001. pp. 157–60. [Google Scholar]
- 2.Ghimire P, Wu GY, Zhu L. Primary gastrointestinal lymphoma. World J Gastroenterol. 2011;17:697–707. doi: 10.3748/wjg.v17.i6.697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dawson IM, Cornes JS, Morson BC. Primary malignant lymphoid tumours of the intestinal tract.Report of 37 cases with a study of factors influencing prognosis. Br J Surg. 1961;49:80–9. doi: 10.1002/bjs.18004921319. [DOI] [PubMed] [Google Scholar]
- 4.Falagas ME, Kouranos VD, Athanassa Z, Kopterides P. Tuberculosis and malignancy. QJM. 2010;103:461–87. doi: 10.1093/qjmed/hcq068. [DOI] [PubMed] [Google Scholar]
- 5.Fanourgiakis P, Mylona E, Androulakis II, Eftychiou C, Vryonis E, Georgala A. Non-Hodgkin's lymphoma and tuberculosis coexistence in the same organs: A report of two cases. Postgrad Med J. 2008;84:276–7. doi: 10.1136/pgmj.2007.066183. [DOI] [PubMed] [Google Scholar]
- 6.Melero M, Gennaro O, Domínguez C, Sánchez Avalos JC. Tuberculosis in patients with lymphomas. Medicina (B Aires) 1992;52:291–5. [PubMed] [Google Scholar]
- 7.Oncel M, Remzi FH, Church JM, Goldblum JR, Zutshi M, Fazio VW. Course and follow-up of solitary Peutz-Jeghers polyps: A case series. Int J Colorectal Dis. 2003;18:33–5. doi: 10.1007/s00384-002-0411-x. [DOI] [PubMed] [Google Scholar]
- 8.Ter Borg PP, Westenend PP, Hesp FW, van der Straaten FF, van de Vrie WW, Honkoop PP. A solitary Peutz-Jeghers type polyp in the jejunum of a 19 year- old male. Cases J. 2008;1:68. doi: 10.1186/1757-1626-1-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mukherjee A, Chattopadhyay S, Azam M, Saha A. Peutz-Jegher's syndrome with gut maltoma: A rare presentation. Clin Cancer Investig J. 2014;3:350–2. [Google Scholar]


