Summary
Background
Spillage of gallstones in the abdominal cavity may rarely occur during the course of laparoscopic cholecystectomy. Dropped gallstones in the peritoneal and extra-peritoneal cavity are usually asymptomatic. However, they may lead to abscess formation with an estimated incidence of about 0.3%. Common locations of the abscess are in the abdominal wall followed by the intra-abdominal cavity, usually in the sub-hepatic or retro-peritoneum inferior to the sub-hepatic space.
Case Report
We hereby describe an unusual case of infected spilled gallstones in the right sub-phrenic space, prospectively detected on abdominal MRI performed two years after laparoscopic cholecystectomy, in a patient with only a mild right-sided abdominal complaint.
Conclusions
This case highlights the role of MRI in suggesting the right diagnosis in cases with vague or even absent symptomatology. In our case the patient’s history together with high quality abdomen MRI allowed the correct diagnosis. Radiologists should be aware of this rare and late onset complication, even after many years from surgery as an incidental finding in almost asymptomatic patients.
MeSH Keywords: Cholecystectomy, Laparoscopic; Gallbladder; Liver; Magnetic Resonance Imaging
Background
Spillage of gallstones is a relatively common complication after laparoscopic cholecystectomy that may occur in 25–30% of cases [1]. Although dropped gallstones in the peritoneal and extra-peritoneal cavity are usually asymptomatic, they may lead to abscess formation with an estimated incidence of about 0.3% [2]. Common locations of the abscess are in the abdominal wall followed by the intra-abdominal cavity, usually in the sub-hepatic or retro-peritoneum inferior to the sub-hepatic space [3].
Case Report
We hereby describe a case of infected spilled gallstones in the right sub-phrenic space, which is a rare location, prospectively detected on liver MRI performed two years after laparoscopic cholecystectomy in a patient with vague and intermittent right-sided abdominal pain. To our knowledge, there is only one other case described in the English literature in which the diagnosis of sub-phrenic dropped gallstones was primarily established by magnetic resonance cholangio-pancreatography (MRCP) [4]. A 63-year-old male patient presented to his primary care physician for intermittent vague abdominal discomfort in the right upper quadrant. He was afebrile and his vital signs were unremarkable. His abdomen was soft, non-tender and not distended with normal bowel sounds. He had no significant co-morbidities. Laboratory work-up revealed only mild leucocytosis (white blood cells 10.1×103/mL) and increased levels of C-reactive protein (7.3 mg/dL; n.v. <1.0 mg/dL). Other parameters such as liver function, amylase and lipase were within the normal limits. Previous surgical history included a laparoscopic cholecystectomy performed two years earlier in another hospital for chronic cholecystitis. During the immediate postoperative period the patient developed a right pleural effusion that was treated with antibiotic therapy. Late postoperative period was uneventful. Patient underwent an abdominal ultrasound examination but no significant findings were depicted. Subsequently, an abdominal MR examination was obtained for further diagnostic evaluation. Hence, the patient was referred to the MRI division of our institution. At presentation the patient was totally asymptomatic and he only complained of a persistent herpes labialis infection.
Abdominal MR study was performed with a 1.5 Tesla scanner (Siemens, Avanto) by using the following sequences: HASTE (Half-Fourier Acquired Single-Shot Turbo Spin-Echo) T2 in axial and coronal planes, BLADE T2 in axial plane, two breath-hold T1-weighted spoiled gradient-recalled echo (GRE) in-phase and out-of-phase sequences, HASTE T2 fat sat thick-slab MRCP images obtained at three oblique coronal angles (−20°, 0°, and 20°) in order to allow optimal visualization of the bile ducts, diffusion weighted imaging (DWI) sequences (b50, b400, b1000), contrast-enhanced sequences using three-dimensional (3D) volumetric interpolated breath-hold examination (VIBE) dynamic technique with fat saturation and antecubital intravenous administration of hepatocyte-specific contrast agent (gadobenate dimeglumine). Maximum intensity projection (MIP) images for MRCP were then generated interactively from the source images.
The MRI examination showed a right sub-phrenic sovra-fluid collection of intermediate T1 and elevated T2 signal, intermediate diffusivity, with thick enhancing walls and containing multiple T2-and T1-hypointense round bodies consistent with dropped gallstones. The collection indented the liver parenchyma at the level of the right sub-phrenic space (Figures 1–3). Therefore, a diagnosis of abscess resulting from suspected infected spilled gallstones was made. The patient underwent exploratory laparotomy that revealed a 3×3 cm mass containing purulent material and gallstones. Pathology examination showed multifaceted gallstones, fibro-adipose tissue with chronic granulomatous inflammation, giant cell reaction and focal abscess without malignant cells. Prior to the procedure the patient underwent complete bowel clean-up. He was empirically started on ampicillin/sulbactam, a broad-spectrum antibiotic. After the pathological confirmation, metronidazole was added to cover anaerobic bacteria. The post-operative period was uneventful and the patient was completely pain-free at 6 months of clinical follow-up.
Figure 1.
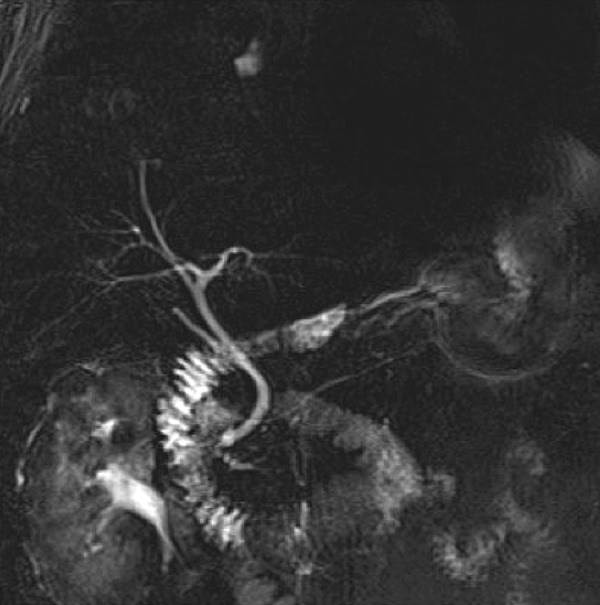
MRCP image showing a centimetric area of hyperintensity in the right sub-phrenic space and post-cholecystectomy findings.
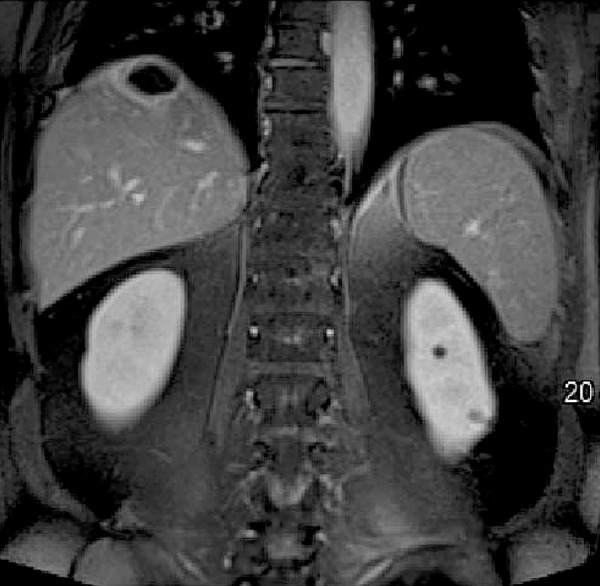
Figure 2.

Coronal HASTE T2 MR image showing multiple hypointense round bodies, surrounded by hyperintense fluid at the level of the right sub-phrenic space.
Figure 3.
Coronal three-dimensional (3D) volumetric interpolated breath-hold examination dynamic images, with fat saturation, showing at the level of the right sub-phrenic space a hypointense area surrounded by mild hyper-enhancement, as expression of an abscess indenting the liver parenchyma.
Discussion
Gallbladder perforations followed by bile leak and gallstone spillage are potential intraoperative events after laparoscopic cholecistectomy. Since its introduction in 1985 by Eric Muhe in Germany, laparoscopic cholecystectomy has become the technique of choice for treatment of a symptomatic gallstone disease, with reported morbidity and mortality rates ranging from 1.9 and 1% compared to 7.7 and 5% for open cholecystectomy, respectively. Risk factors for the development of laparoscopic complications are acute cholecystitis, fibrotic gallbladder, cirrhosis and obesity [5–7]. As previously reported, spillage of gallstones is a relatively common complication as it may occur in 25–30% of cases [7,8]. Although dropped gallstones in the peritoneal and extra-peritoneal cavity are usually asymptomatic, they may lead to abscess formation with an estimated incidence of about 0.3% [5–7]. Due to pneumo-peritoneum created during laparoscopic cholecystectomy, dropped gallstones may reach different locations, even distant from the gallbladder fossa. Hanna et al. in a previous paper reported a case of unsuspected ectopic gallstones in the peritoneal cavity following laparoscopic cholecystectomy, identified on ultrasound and MRI [8,9]. In the majority of cases gallstones are retrieved in the abdominal wall near the site of trocar placements or in the dependent areas of the peritoneal cavity, such as Morrison’s pouch and the pouch of Douglas [10]. Even if surgeons are aware of the possibility of dropping gallstones by acting some measures to prevent this complication (such as retrieval bags, aspiration of bile before dissecting the gallbladder), in cases of severe cholecystitis the gallbladder may perforate during the resection and spillage of gallstones may occur. In these cases peritoneal saline irrigation is recommended to clean and dilute infected bile, while the conversion to open surgery for removal of spilled stones still represents a matter of discussion [8]. Since the spilled gallstones in the majority of cases remains asymptomatic, careful surveillance of these “at risk” patients by physicians is needed to refer the patients for a correct diagnostic work-up if complications appear. Lost gallstones become in fact a site of chronic inflammations and a potential nidus of infection with abscess formation. Other more rare complications associated with spilled gallstones are adhesions, fistulas and ileus [10]. The diagnosis of gallstone abscess is usually late and not easy to make upon patient presentation. Imaging plays a crucial role in the depiction of the abscess and of the gallstones associated. US and CT can demonstrate the presence of the abscess and identify the calculi, but dropped no-opaque or millimetric gallstones may be undetected, and the diagnosis is made only after laparotomy.
We hereby describe a case of a right sub-phrenic chronic abscess due to spilled gallstones, prospectively detected by liver MRI in a relatively rare location. Even if there already is another similar case described in the English literature in this location [4], our case presents a patient that was completely asymptomatic at the moment of MRI examination and did not show acute symptoms but only a vague right-sided abdominal complaint. Therefore, the radiologist could suggest the correct diagnosis on the basis of MRI findings and patient surgical history.
Furthermore, MRI showed the characteristic tri-radiate pattern (Mercedes Benz sign) of the dropped gallstones, a feature described in a previously reported case in the pouch of Douglas of a woman with sudden amenorrhea after six years from laparoscopic cholecystectomy [10].
This is the first case to our knowledge in which all the MRI features are shown, as the other cases lack DWI and dynamic post-contrast and hepato-specific sequences. MRI allowed the characterization of the abscess and its nature, showing a sovra-fluid mass adjacent to the liver containing multiple round gallstones, with thick enhancing walls. No calculi were depicted within the bile ducts at MRCP sequences. In addition, on DWI, diffusivity was not significantly restricted as the abscess was chronic. Finally, the use of a hepato-specific contrast agent could accurately exclude any communication of the abscess with the biliary tree, a finding expected in our case as the collection was chronic, providing a useful information for surgical planning. Gallstone abscess resulting from spilled gallstones is a rare complication following laparoscopic cholecystectomy. Although uncommon, these stones may lead to early or late complications, which can be a diagnostic challenge and cause significant morbidity to the patient. Therefore, proper surgical care should be taken during laparoscopic cholecystectomy to avoid stone spillage.
Conclusions
In our case the patient’s history together with high-quality abdomen MRI allowed the correct diagnosis. Radiologists should be aware of this rare and late-onset complication, even after many years from surgery as an incidental finding in almost asymptomatic patients.
References
- 1.Lillemoe KD, Yeo CJ, Talamini MA, et al. Selective cholangiography. Current role in laparoscopic cholecystectomy. Ann Surg. 1992;215:669–74. doi: 10.1097/00000658-199206000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Horton M, Florence MG. Unusual abscess patterns following dropped gallstones during laparoscopic cholecystectomy. Am J Surg. 1998;175:375–79. doi: 10.1016/S0002-9610(98)00048-8. [DOI] [PubMed] [Google Scholar]
- 3.Rice DC, Memon MA, Jamison RL, et al. Long-term consequences of intraoperative spillage of bile and gallstones during laparoscopic cholecystectomy. J Gastrointest Surg. 1997;1:85–91. doi: 10.1007/s11605-006-0014-x. [DOI] [PubMed] [Google Scholar]
- 4.O’Brien A, Woolfall PA. diagnosis of dropped gallstones and abscess formation established on MRCP. Clinical Radiology Extra. 2005;60:38–39. [Google Scholar]
- 5.Sathesh-Kumar T, Saklani AP, Vinayagam R, Blackett RL. Spilled gallstones during laparoscopic cholecystectomy: A review of the literature. Postgrad Med J. 2004;80:77–79. doi: 10.1136/pmj.2003.006023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zehetner J, Shamiyeh A, Wayand W. Lost gallstones in laparoscopic cholecystectomy: All possible complications. Am J Surg. 2007;193:73–78. doi: 10.1016/j.amjsurg.2006.05.015. [DOI] [PubMed] [Google Scholar]
- 7.Morrin MM, Kruskal JB, Hochman MG, et al. Radiologic features of complications arising from dropped gallstones in laparoscopic cholecystectomy patients. Am J Roentgenol. 2000;174:1441–45. doi: 10.2214/ajr.174.5.1741441. [DOI] [PubMed] [Google Scholar]
- 8.Helme S, Samdani T, Sinha P. Complications of spilled gallstones following laparoscopic cholecystectomy: A case report and literature overview. J Med Case Rep. 2009;3:8626. doi: 10.4076/1752-1947-3-8626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dobradin A, Jugmohan S, Dabul L. Gallstone-related abdominal abscess 8 years after laparoscopic cholecystectomy. JSLS. 2013;17:139–42. doi: 10.4293/108680812X13517013317518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hanna S, Scourt L, Israel G. Ultrasound and MR identification of ectopic gallstones as a complication of laparoscopic cholecystectomy. European Journal of Radiology Extra. 2011;77:e95–e97. [Google Scholar]


