Abstract
Foreign body aspirations that are not recognized at the time of aspiration can lead to insidious symptoms that can present a diagnostic challenge. We report the case of a 70-year-old man presenting with postobstructive pneumonia 2 months after aspirating his own tooth during a meal. He had been mistakenly diagnosed with asthma and treated with bronchodilators before a computed tomography scan of the thorax revealed the impacted tooth in his left bronchus. We review the clinical features and microbiology of postobstructive pneumonia and discuss the rationale of its treatment.
Keywords: aspiration, postobstructive pneumonia, tooth
Foreign body aspirations can lead to numerous complications, the most common of which is postobstructive pneumonia. Postobstructive pneumonia can present very insidiously, making it a diagnostic challenge when clinical suspicion is low. We report the case of a 70-year-old man with poor dentition who aspirated his own tooth 2 months before presenting with recurrent cough, fevers, and dyspnea from postobstructive pneumonia. Then, we review the clinical features of foreign body aspiration and postobstructive pneumonia, as well as the latter′s microbiology and treatment.
CASE REPORT
A 70-year-old male with a history of type II diabetes mellitus, hypertension, and a more than 50 pack-year smoking history presented to an outside hospital with a chief complaint of 1 month of a nonproductive cough. Around that time, he first developed a cough that gradually worsened over the next month. He eventually began to have worsening shortness of breath and chills, so he presented to an outside hospital for evaluation.
At that hospital, the patient was found to have a leukocytosis of 12.5 K/µL, heart rate in the 100 s, and decreased breath sounds over the left lower lobe. Chest x-ray showed left lower lobe consolidation with adjacent radiopaque body (Figure 1). Computed tomography (CT) angiogram of the chest showed a calcified body in the left lower lobe bronchus with extensive postobstructive consolidation and no evidence of pulmonary embolism. He was started on parenteral ampicillin-sulbactam for postobstructive pneumonia. Both rigid and flexible bronchoscopy were performed with reported visualization of a calcified lesion that could not be retrieved due to its technically challenging location. He was transferred to our facility for evaluation by another interventional pulmonologist.
Figure 1.
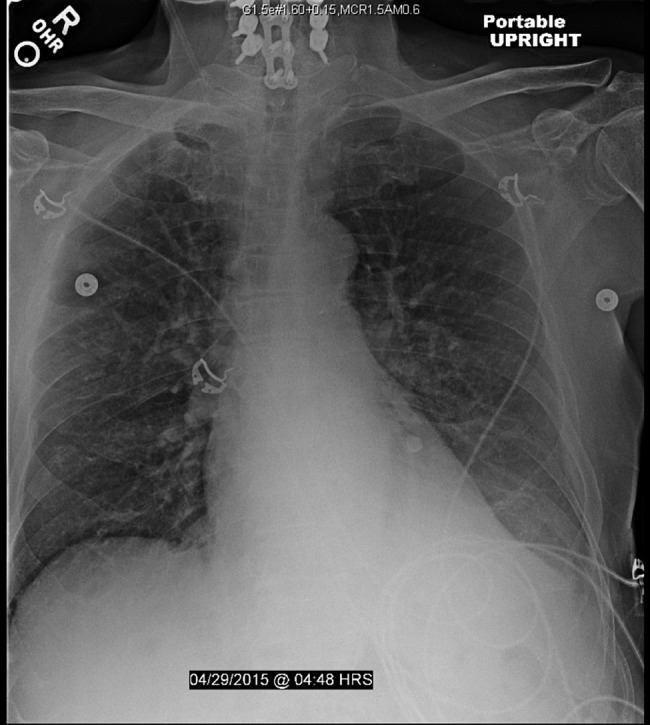
Patient's chest x-ray demonstrating radiopaque object in left lower lobe.
He subsequently underwent repeat flexible bronchoscopy. The offending tooth was found lodged in the takeoff of the basilar segment of the left lower lobe (Figure 2). A basket was advanced past the object and deployed with successful removal of the tooth in 2 pieces (Figure 3). Ampicillin-sulbactam was changed to moxifloxacin as an oral option for discharge for a further 7 day course. After the procedure, his cough resolved. Bedside swallow evaluation was normal. He was discharged to complete his course of antibiotics at home. After the retrieval, the patient recalled that approximately 2 months ago, he had a meal that was difficult to chew and recalls one of his molars fracturing.
Figure 2.
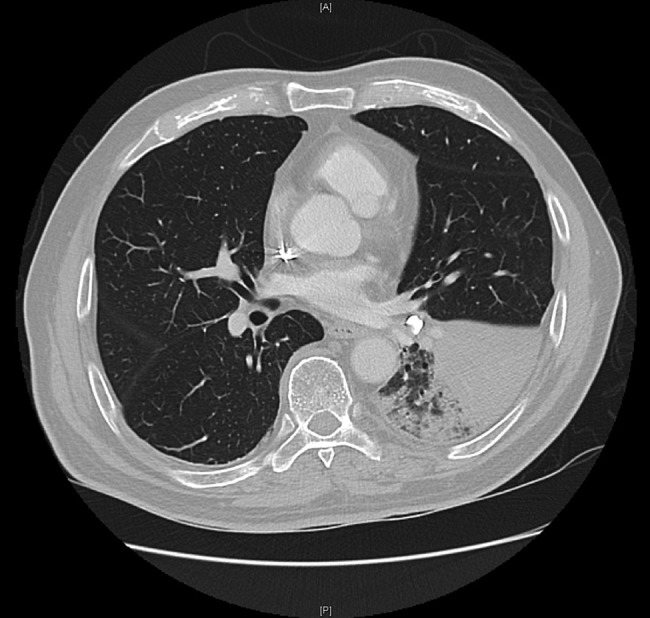
Patient's computed tomography scan from the outside hospital, showing impacted tooth with distal lung consolidation.
Figure 3.
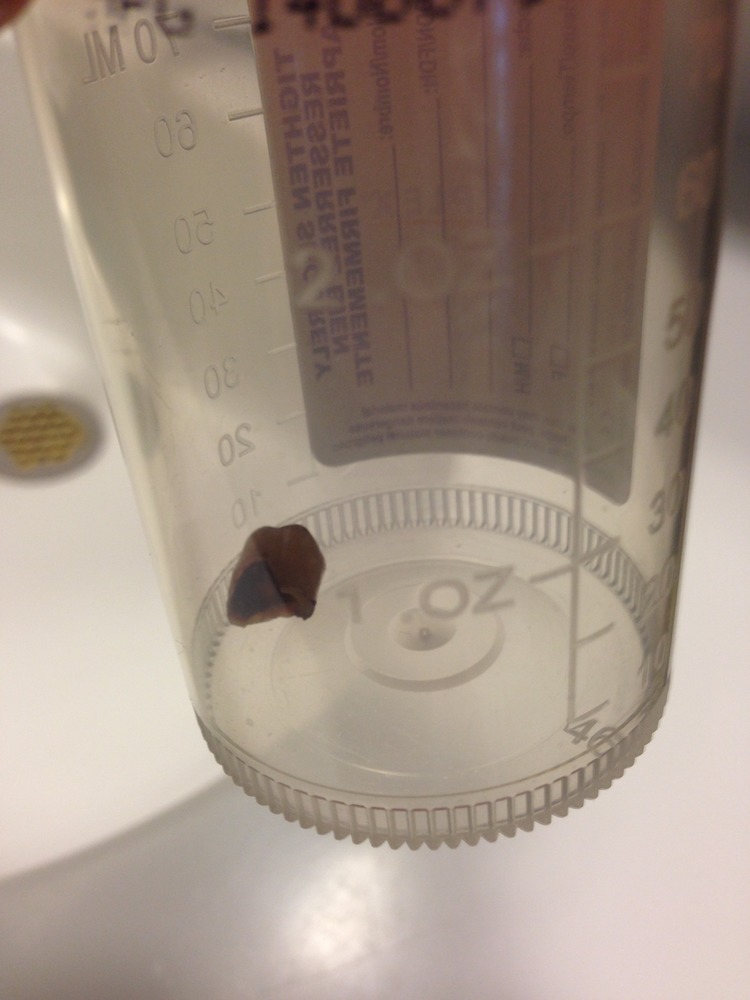
Patient's tooth after extraction via bronchoscopy.
DISCUSSION
Foreign body aspirations (FBAs) are often seen in the pediatric and trauma populations but are less common in adults. They are more likely to occur in the adult patient if they have a decreased level of consciousness, compromised airway defense mechanisms, dysphagia, gastroesophageal reflux disease, or recurrent vomiting. Even without these predisposing factors, some studies have shown that one half of healthy subjects aspirate pharyngeal secretions during sleep [1].
In adults, aspirations peak during the 6th decade of life [2]. Symptoms of an FBA include nonresolving cough, exertional dyspnea, chest pain, hemoptysis, and recurrent pneumonias. In geriatric cases of FBA, cough and sputum production are seen in approximately 88% of patients, dyspnea in 35%, and hemoptysis in 24% [3]. Unfortunately, up to 33% of patients present with fever without radiographic signs of pneumonia, making the x-ray an unreliable sign of superinfection [2].
Fortunately, tooth aspiration can be easier to diagnose because the foreign body is radiopaque. They are most frequently seen after trauma, although they can also occur during intubation, adenotonsillectomy, or dental extractions. However, like most aspirated foreign bodies, they are more challenging to catch if the patient has an altered sensorium, and they can subsequently lead to delayed complications [4]. In general, CT has proven more accurate than chest radiographs because thoracic radiopaque structures are much easier to separate from the radiopaque tooth in cross-section [5, 6].
Postobstructive pneumonia is typically polymicrobial. The opacification that occurs on chest x-ray or CT results from a combination of atelectasis, bronchiectasis, mucus plugging, and parenchymal inflammation with or without infection. Studies using ultrasound-guided needle aspirations show that there is often little concordance between the organisms within the pneumonia and the organisms from sputum cultures [7]. The most common isolated organisms are usually identical to those from typical aspiration pneumonia and include normal oral flora such as Streptococcus, Prevotella, Bacteroides, and Porphyromonas [8]. Pseudomonas aeruginosa and Staphylococcus aureus must also be considered in the healthcare-associated population, ie, those residing in nursing homes or with recent hospital stays [7, 9].
CONCLUSIONS
Treatment of postobstructive pneumonia is typically 2-fold, requiring both removal of the obstruction and antibiotic therapy for the infection. The obstruction is most often removed with either fiberoptic or rigid bronchoscopy, as in this case [2]. Bronchoscopy offers the advantage of both confirmation of the diagnosis and the opportunity for intervention [5]. Flexible bronchoscopy is preferable given the lower morbidity associated with the procedure; approximately 81% of patients have successful removal of the foreign body within 2 attempts [3]. Antibiotic therapy must target similar organisms to aspiration pneumonia [9]. The optimal duration of treatment if the foreign body cannot be removed is unknown, but if empyema develops prolonged therapy may be needed [9]. However, once recognized, postobstructive pneumonia can often be definitively treated with substantial clinical improvement for the patient.
Acknowledgments
Potential conflicts of interest. All authors: No reported conflicts. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest.
References
- 1.Hu X, Lee JS, Pianosi PT, Ryu JH. Aspiration-related pulmonary syndromes. Chest 2015; 147:815–23. [DOI] [PubMed] [Google Scholar]
- 2.Baharloo F, Veyckemans F, Francis C et al. Tracheobronchial foreign bodies: presentation and management in children and adults. Chest 1999; 115:1357–62. [DOI] [PubMed] [Google Scholar]
- 3.Lin L, Lv L, Wang Y et al. The clinical features of foreign body aspiration into the lower airway in geriatric patients. Clin Interv Aging 2014; 9:1613–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Madan K, Aggarwal AN, Bhagat H, Singh N. Acute respiratory failure following traumatic tooth aspiration. BMJ Case Rep 2013; pii: bcr2012008393 doi:10.1136/bcr-2012-008393, p 1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhang M, Zhou GJ, Zhao S et al. Delayed diagnosis of tooth aspiration in three multiple trauma patients with mechanical ventilation. Crit Care 2011; 15:424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yurdakul AS, Kanbay A, Kurul C et al. An occult foreign body aspiration with bronchial anomaly mimicking asthma and pneumonia. Dent Traumatol 2007; 23:368–70. [DOI] [PubMed] [Google Scholar]
- 7.Hsu-Kim C, Hoag J, Cheng G, Lund M. The microbiology of postobstructive pneumonia in lung cancer patients. J Bronchology Interv Pulmonol 2013; 20:266–70. [DOI] [PubMed] [Google Scholar]
- 8.Bennett JE, Dolin R, Martin JB. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases, Philadelphia, PA: Churchill-Livingstone Elsevier, 69; pp 823–846.e5. [Google Scholar]
- 9.Finegold S. Aspiration pneumonia. Rev Infect Dis 1991; 13:S737–42. [DOI] [PubMed] [Google Scholar]


