Abstract
Background
Understanding how to mitigate language barriers is becoming increasingly important for health care providers around the world. Language barriers adversely affect patients in their access to health services; comprehension and adherence; quality of care; and patient and provider satisfaction. In 2003, the United States (US) government made a major change in national policy guidance that significantly affected limited English proficient patients’ ability to access language services.
Objective
The objectives of this paper are to describe the state of the language barriers literature inside and outside the US since 2003 and to compare the research that was conducted before and after a national policy change occurred in the US. We hypothesize that language barrier research would increase inside and outside the US but that the increase in research would be larger inside the US in response to this national policy change.
Methods
We reviewed the research literature on language barriers in health care and conducted a cross sectional analysis by tabulating frequencies for geographic location, language group, methodology, research focus and specialty and compared the literature before and after 2003.
Results
Our sample included 136 studies prior to 2003 and 426 studies from 2003–2010. In the 2003–2010 time period there was a new interest in studying the providers’ perspective instead of or in addition to the patients’ perspective. The methods remained similar between periods with greater than 60% of studies being descriptive and 12% being interventions.
Conclusions
There was an increase in research on language barriers inside and outside the US and we believe this was larger due to the change in the national policy. We suggest that researchers worldwide should move away from simply documenting the existence of language barriers and should begin to focus their research on documenting how language concordant care influences patient outcomes, providing evidence for interventions that mitigate language barriers, and evaluating the cost effectiveness of providing language concordant care to patients with language barriers. We think this is possible if funding agencies around the world begin to request proposals for these types of research studies. Together, we can begin document meaningful ways to provide high quality health care to patients with language barriers.
Keywords: Cross sectional review, Language barriers, Limited English proficiency, Policy change
1. Introduction
There is a law in the United States, Title VI of the Civil Rights Act of 1964, that requires all federally funded programs to provide meaningful access to care for limited English proficient (LEP) individuals.(1974) Despite the federal right to meaningful access to language services for LEP patients in federally funded programs, the reality is that many health care providers are not providing adequate services to their LEP populations.(Chen et al., 2007) This is because it is not widely enforced and health care providers have little understanding of how to comply with it. To increase awareness of the law and to provide explicit guidance as to how health care organizations could comply with the law, President Clinton issued Executive Order (EO) 13166 in August, 2000, Improving Access to Services for Persons with Limited English Proficiency.(August 16, 2000) Some health care providers and professional organizations took issue with this guidance, calling it an “unfunded mandate” (Neighborhood Health Plan of Rhode Island), and in response, the Bush Administration revised and reissued the Policy Guidance soon after taking office.(August 8, 2003) This reversal in provision of explicit guidance by the Bush Administration brought publicity to the issue of language barriers in health care and the impact they potentially have on care(Meyers et al., 2009, National Council on Interpreting in Health Care, 2011). We hypothesized that this policy debate and the surrounding publicity galvanized the research community in the US to increase their investigation of language barriers in health care, how to overcome them, how they impact care, and interventions to reduce them, and that this increase would not occur to the same degree outside the US. We undertook this study to describe the state of language barriers research inside and outside the US from 2003–2010 and to descriptively compare the research that occurred before and after this national policy change.
1.1 Language Barriers in Health Care are a Global Problem
Countries around the globe welcome and/or absorb immigrants. In Europe, Canada, and Australia, for example, there have been growing numbers of immigrants and patients who do not speak the language(s) used in their health care systems.(2013, Australian Government, Diez Guardia N. and Pichelman, September 2006, Somerville, 2009, Taylor, 2012) Over the last decade in the UK, there have been growing numbers of immigrants, and they are coming from more diverse backgrounds than ever before. (Somerville, 2009) In Canada, although the number of immigrants has remained relatively constant; the countries they come from have shifted. (Government of Canada, 2011) Currently, the largest percentage of immigrants come from Asia (including the Middle East) as compared to European immigrants which made up the majority of Canadian immigrants up until the 1970s.(Government of Canada, 2011) In Australia, migration continues to be the major component of population growth with almost half of Australia’s population either born overseas or with a migrant parent.(Australian Government)
1.2 Language Barriers Impact Health Around the Globe
Language barriers significantly affect quality of care in the health care system around the world. (Fassaert et al., 2010, Murray et al., 2010, Ou et al., 2010, Ponce et al., 2006, Poureslami et al., 2010, Puthussery et al., 2010, Sokal, 2010, Timmins, 2002) Research suggests that language barriers adversely affect patients in their access to health services (Jacobs et al., 2006, Pippins et al., 2007, Robert Wood Johnson Foundation, 2001); comprehension and adherence(Cheng et al., 2007, Jacobs et al., 2006); quality of care (Cohen et al., 2005, Diamond et al., 2009, Jacobs et al., 2003, Jacobs et al., 2006); and patient and provider satisfaction. (Arthur et al., 2014, Baker et al., 1996, Jacobs et al., 2006)
1.2 Relevance of Studying How National Policy Impacts Research on Language Barriers in the US
Language barriers are also a big issue in the US as they affect a growing portion of the population there as well. The number of limited English proficient (LEP) individuals in the US increased by 80 percent between 1990 and 2010 (Pandya et al., 2011) and, according to the 2010 US census, 25.2 million people or nine percent of the US population over the age of five is LEP.(Pandya et al., 2011) Given this large and growing population in the United States, US Federal Policy around language barriers in health care, and the significant publicity and debate around a change in policy guidance in 2003, we had the opportunity to study whether or not this impacted the quantity and type of language barriers research.
While the analysis focused on a policy change in the US, this work is relevant to a global audience because it provides a broad summary of the state of language barriers research around the world and is a case study of how a policy change in the US did or did not impact the trajectory of language barriers research. Policy makers in other countries likely will be interested to see if national policies influence the research community and if so, in what ways.
1.4. Purpose of this Study
The aims of this work are (1) to describe the state of the language barriers literature inside and outside the US from 2003–2010 and (2) to compare the research that was conducted before and after the national policy change. A comprehensive annotated bibliography describing the state of the language barriers literature was published in 2003,(Jacobs et al., 2003) but to our knowledge no comprehensive description of the state of the language barriers research across all specialties has been conducted since that time. We hypothesized that research on language barriers would dramatically increase after 2003, and the focus of the research would shift from documentation of language barriers as a risk for disparities in health care to evidence that interventions improved care. We included studies conducted outside the US to show how the language barriers literature evolved independent of the national policy change that occurred in the US. We hypothesized that we would see more of a pronounced increase in studies and change in methodology within the US compared with outside the US as a result of the national policy change in the US.
2. Design and methods
2.1 Review
We reviewed the literature focusing on language barriers and health from 1975 to 2010 in two steps and then conducted a cross sectional analysis of the type and distribution of manuscripts in the literature that were published before and after the policy change in 2003.
First, we completed a review of the literature in 2003 for an annotated bibliography entitled Language Barriers in Health Care Settings: An Annotated Bibliography of the Research Literature, commissioned by The California Endowment.(Jacobs et al., 2003) All articles in this review were published in January 2003 or earlier. To be included in the bibliography, articles had to be published in English, in the peer-reviewed literature, have a primary focus or finding specific to language barriers and contain original research. To identify articles, we searched MEDLINE, CINAHL, PsycINFO, Sociological Abstracts, Periodical Abstracts, ArticleFirst, Social Sciences Abstracts and Digital Dissertations searches using the Medical Subject Heading terms, language, communication-barrier, multilingual and translation as well as text words such as interpreter, non-English-speaking and limited English proficient. Additional articles were identified from the reference lists of key articles. Second, we undertook another review of the literature in 2011 using this same set of inclusion criteria, and it included articles from February 2003 to December 2010. The focus of the follow-up literature review was to characterize the language barriers literature in the same way it had been characterized in 2003 and to characterize how the language barrier literature had changed. Due to the increased number of peer-reviewed articles on language barriers in the 2003–2010 sample, only articles in the MEDLINE/PubMed and CINAHL databases were used. The search term was language barriers. Any articles for which there were questions about excluding or including a manuscript were reviewed by the senior author (EAJ) as a check for appropriateness.
2.2 Classification
We then systematically classified all manuscripts that met our inclusion criterion by geographic location, language group, methodology, research focus, and specialty. We chose these classifications to characterize the topic of the investigations, the means of the investigation, and if they were conducted in areas where language barriers were more commonly encountered (geographic location) Study location was defined as the geographic location where the study took place. We categorized all studies by country. All US-based studies were then categorized as a multi-regional study (conducted in more than one US region), occurring in one of the four US census bureau regions (Midwest, Northeast, South and West), and by state. We used the US Census Bureau definitions of language groups to categorize studies. They include Chinese languages, other Asian and Pacific Island languages, Spanish, other Indo-European languages (examples: French, German, Russian, Urdu) and other languages. (Shin and Kominski, 2010, United States Census Bureau). If more than one language group was studied, language was classified as more than one category. If the language group was unknown or if the study talked about language barriers generally, then the language group was classified as general/unknown. The general/unknown and more than one language categories were collapsed due to small numbers in both categories (n=26, total). Every study received two methodology classifications. First, studies were classified as quantitative, qualitative, or mixed methods. Studies were classified as quantitative or qualitative if they used exclusively quantitative or qualitative methods, respectively. Studies were classified as mixed method if they used a combination of quantitative and qualitative methods. Second, studies were classified as descriptive, preference, impact or intervention. Descriptive studies characterized the existence of language barriers in health care but did not examine at the relationship between language barriers and health outcomes. Studies investigating preferred strategies for reducing language barriers when receiving or providing care were classified as preference studies. Two types of studies were classified as impact studies: (1) retrospective studies evaluating how a change in policy or a new program influenced language barriers in the health care setting and (2) cross-sectional studies examining the association between language barriers and health outcomes. Studies prospectively evaluating how a new program or tool affected language barriers in health care were categorized as intervention studies. All methodology codes were reviewed by the senior author (EAJ) to ensure accuracy (examples of articles in the different methodology categories can be found in Appendix 1). There were a total of 35 research foci used to classify the studies (Not shown; see Appendix 2). Research foci are descriptive key words that the research team assigned to each research study. 29 research foci were identified in the first annotated bibliography. From the original list, the research team removed the descriptive keywords that pertained to methodology (qualitative study and research methodology) and added descriptive key words that applied to the new literature: data use, discrimination, ethics, health information seeking, instrument, language barriers in research, outcomes (provider-reported), policy, trust and provider type. Provider type included: care workers, interpreters, nurse educators, nurse practitioners, nursing assistants, occupational therapists, pharmacists, physical therapists, physician assistants, physicians, registered nurses, social workers, students and other. Each study could have more than one provider subgroup classification. Once the 35 research foci were identified, all studies were checked to make sure they were classified appropriately. Studies could have more than one categorization. Finally, specialty was defined as the major clinical setting or topic of the article (e.g. cardiology, emergency department, pediatrics, primary care, etc.). Each study could be classified by as many specialties as documented by the authors. If a study setting was not clear then the study setting was classified as general.
2.3 Descriptive Analysis
We tallied the number of articles published by geographical location, language group, methodology, research focus, and specialty before and after 2003. We also calculated the change in proportional contribution of studies to the research literature by geographic location and language group before and after 2003; we subtracted the percent contribution of articles in the pre-2003 period from the percent contribution of articles in the 2003–2010 period.
We compared the research conducted inside the US to research conducted outside the US in both time periods by geographic location, language group, methodology, research focus, and specialty. Research conducted outside of the US served as a control group to the research conducted inside the US. We believe research conducted outside the US serves as an appropriate control group because we are not aware of any substantive language barrier policy changes that occurred in Australia, Canada and the European Union (>75% of the research studies in the sample were conducted in these countries) in the 2003–2010 study period.(Healthcare Interpretation Network, 2007, Norstrom, 2010, Pandya et al., 2011)
3. Results
One hundred thirty six published studies met our inclusion criterion in the pre-2003 period and 426 studies in the 2003–2010 period (Appendix 3). The percent of published peer-reviewed studies in the 2003–2010 period increased by 326% in the US and by 292% outside the US. Researchers in the US continued to publish the majority of the research on language barriers in the 2003–2010 period (Table 1). Outside of the US, Australia, Canada and the United Kingdom also continued to conduct the most language barriers research (Table 1).
Table 1.
Geographic Study Location Pre and Post 2003 (%, n)
| Country | Pre -2003 (n=136) |
2003–2010 (n=426) |
Change in proportional contribution (%) |
|---|---|---|---|
| Australia | 12%, 16 | 6%, 26 | −6% |
| Canada | 3%, 4 | 8%, 33 | 5% |
| Other* | 8%, 11 | 14%, 61 | 6% |
| United States | 62%, 84 | 64%, 274 | 2% |
| United Kingdom | 15%, 21 | 8%, 32 | −7% |
Austria, Belgium, Chile, Egypt, Germany, Greece, India, Ireland, Israel, Italy, Japan, Kuwait, Mexico, New Zealand, Nigeria, Norway, Papa New Guinea, Saudi Arabia, Singapore, South Africa, Spain, Sweden, Switzerland, Thailand and The Netherlands
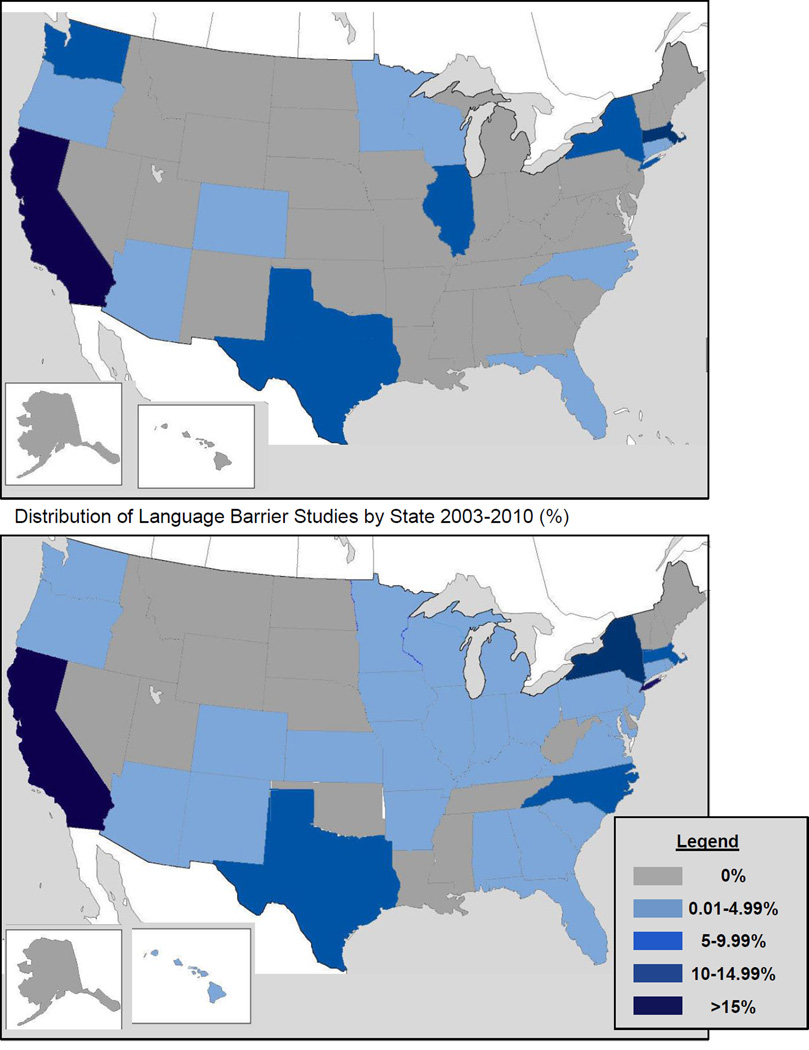
Within the US, there was a 12% increase in the number of multi-region studies done in 2003–2010 compared with pre-2003 (data not shown). Although there was an increase in the research done in the Midwest and South in the 2003–2010 period, the majority of research continues to be done in the West (28%) and Northeast (21%). In the pre-2003 period, six states (California, Illinois, Massachusetts, New York, Texas and Washington) conducted 72% of research in the US (Figure 1). In the 2003–2010 period, these same six states conducted 47% of the research. Additionally, 17 states had at least one study published in the 2003–2010 period that had none previously.
Figure 1.
Distribution of Language Barrier Studies by State Pre-2003 (%)
*California made up 40% and 23% of the research before and after 2003 respectively
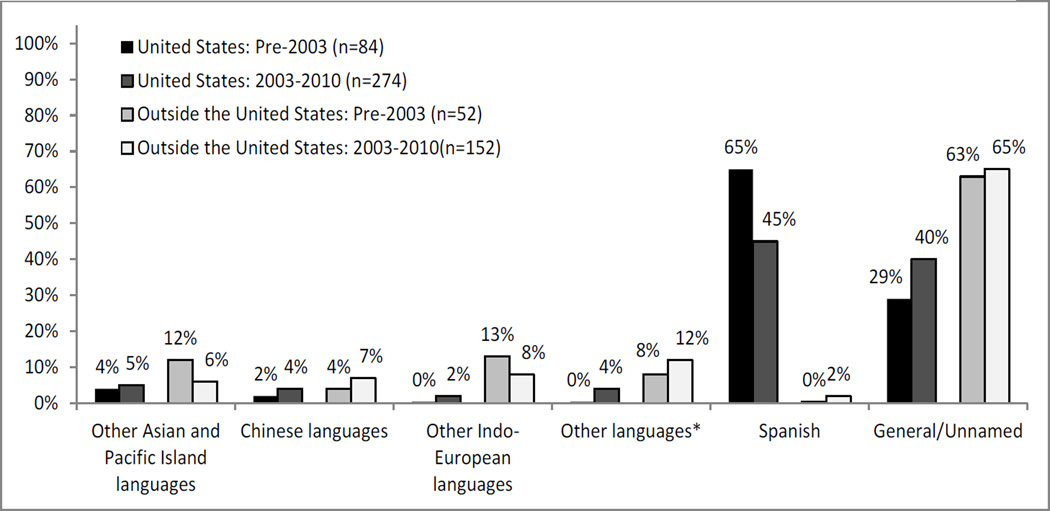
Figure 2 highlights the distribution of language groups studied. In the US, Spanish was the most studied language with 65% of the studies studying Spanish pre-2003 and 45% in 2003–2010.. Outside the US, there was much more variety in the types of language studied than inside the US; however most of the studies outside of the US, in both periods, studied language barriers generally, or never named the languages that were studied.
Figure 2.
Language Studied in the US and Outside the US Before and After 2003
*Other languages includes Aboriginal Australian, non-specific African languages, Arabic, Ahmaric, Hausa, Hebrew, Inuit, Mayan, Saulteau, Somali, Xhosa
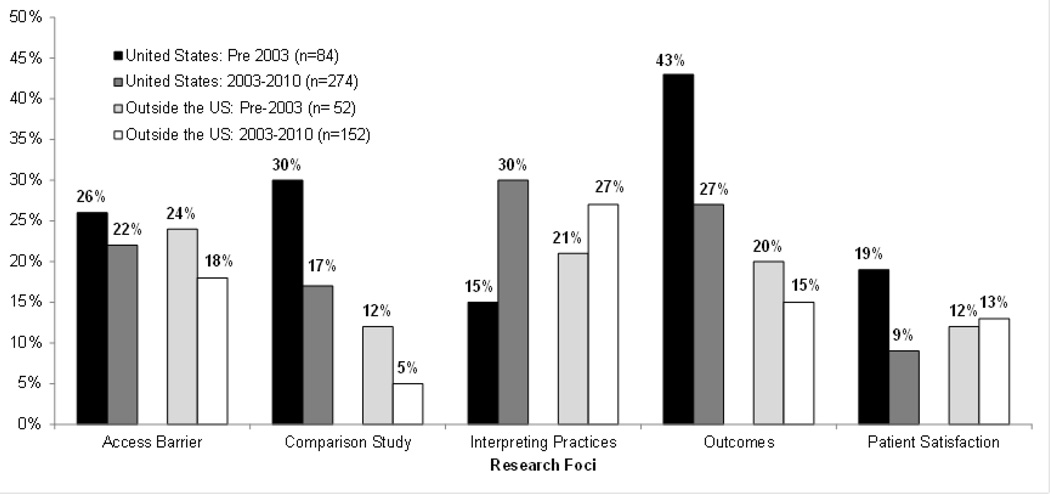
The most frequently studied research foci were similar in the US and outside the US before and after 2003 (Figure 3). Access barriers, studies in which language was investigated as a barrier to obtaining health care services, was a major research focus in the US and outside the US both pre-2003 and 2003–2010. The percentage of comparison studies, studies with an explicit comparison of people proficient in the primary language of a country compared to people with limited proficiency in the primary language, decreased both in the US and outside the US in the 2003–2010 sample and were more commonly conducted in the US than outside the US in both time periods. Outcomes research, studies that examine the relationship between language and outcomes, including utilization and health status decreased in the US from 43% pre-2003 to 27% in 2003–2010, but it remained a dominant area of research inside the US and outside the US in both time periods. Additionally, in studies conducted outside the US there was an increased focus on studying ethics and medical decision making; health information seeking, instrument development and provider satisfaction; and there was less of a focus on comparison studies, prevention and provider competency and training. Access barriers, interpreting practices, health beliefs, need, outcomes, patient satisfaction, and utilization were among the top ten research foci in the US and outside the US in both periods.
Figure 3.
Research Foci of Studies in the US and Outside the US before and after 2003
There was considerable overlap in the specialties where research was conducted in the US and outside the US in the pre-2003 and in the 2003–2010. However, there was a new interest in the 2003–2010 period to try and understand the providers’ perspectives pertaining to language barriers in the health care setting. Eight percent of the studies in the 2003 to 2010 period identified the health care workers as the group that was being studied instead of or in addition to the patients. Table 2 describes in greater detail the types of providers that were studied in the 2003–2010 time period. The top three provider types studied in the US included physicians (39%), students (36%) and registered nurses (24%). Outside the US the three most commonly studied provider types were registered nurses (46%), pharmacists (23%) and other health professionals (23%). There was also an increased interest in the 2003–2010 period in studying health in the community and studying chronic diseases and there was a decreased emphasis on obstetrics and gynecology. In the US researchers studied language barriers in pharmacy and emergency medicine settings more often than their peers outside the US. Researchers outside the US studied language barriers in the hospital setting more than researchers in the US.
Table 2.
Type of Providers Studied Inside and Outside the US in the 2003–2010 time period*
| United States (n=33) |
Outside United States (n=39) |
|
|---|---|---|
| Care Workers | 0%, 0 | 8%, 3 |
| Interpreters | 9%, 3 | 3%, 1 |
| Nurse Educators | 0%, 0 | 8%, 3 |
| Nurse Practitioner | 12%, 4 | 5%, 2 |
| Nursing Assistants | 3%, 1 | 0%, 0 |
| Occupational Therapists |
0%, 0 | 3%, 2 |
| Pharmacists | 3%, 1 | 23%, 9 |
| Physical Therapists | 3%, 1 | 3%, 1 |
| Physician Assistant | 9%, 3 | 0%, 0 |
| Physicians | 39%, 13 | 18%, 7 |
| Registered Nurses | 24%, 8 | 46%, 18 |
| Social Workers | 0%, 0 | 3%, 1 |
| Students | 36%, 12 | 18%, 7 |
| Other** | 6%, 2 | 23%, 9 |
The listed provider types are those that have been studied in the literature and are not meant to be an exhaustive list
Child welfare workers, clinical practice managers, health professionals generally, health visitors, midwives, radiation therapists, sexual heatlh counselors
The methods used to study language barriers remained similar before and after 2003 (not shown, see Appendix 4). Greater than 60% of studies inside and outside the US and before and after 2003 were descriptive in nature. There was a 4% proportional change in the US and a 6% proportional change outside the US in intervention studies before and after 2003. Inside and outside the US the total percentage of intervention studies in the 2003–2010 period remained low at 12%. In all study types, there was an increase in qualitative studies in the 2003–2010 (36%) period compared with the pre-2003 period (25%).
When comparing the general patterns in the research that was conducted in the US and outside the US from 2003–2010 one main differences was in the number of studies conducted; a greater number of studies on language barriers were conducted in the US than outside the US. Research on language barriers did increase in the US and outside the US; however, the increase was larger in the US. The methodologies used were similar in the US and outside the US.
4. Discussion
A substantial amount of research on language barriers in the health care setting was done inside and outside the US in the 2003–2010 time period and this represented an increase from our initial review from 1974–2003. The majority of this more recent research focused on access barriers, comparison studies, interpreting practices, outcomes and patient satisfaction. It was descriptive in nature and most of the research conducted in the US focused on Spanish-language research.
As hypothesized, we found that the increase in the amount of research focusing on language barriers in the US in the 2003–2010 time period was much greater than the increase in this research literature outside the US. We think that the national policy change is one plausible explanation for the greater increase in language barriers research in the US as compared to the rest of the world. It is also possible that the successful implementation of language access programs in the US (Meyers et al., 2009) contributed to the increased interest in understanding how these programs impact care for LEP patients in the US. We believe that increasing immigration in the US(Pandya et al., 2011), Canada,(Government of Canada, 2011) the UK,(Somerville, 2009) Europe and Australia(Diez Guardia N and Pichelmann, September 2006) contributed to the overall increase in language barriers research inside and outside the US.
Although the focus of research remained relatively consistent inside and outside the US, it is interesting to observe that there was a new focus on understanding the provider perspective that emerged in the 2003–2010 worldwide. It is especially interesting to note the wide variety of health care professionals where language barriers have been studied. Inside the US the major focus was on studying physicians’ perspectives working with patients that have language barriers; outside the US the major focus was on studying nurses’ perspectives working with patients that have language barriers; however there was substantial variety of types of providers studied inside and outside the US. This new area of interest in language barriers research is an important area to continue to explore because it acknowledges that the health care providers’ training relating to language barriers and their perceptions of language barriers in general do have an impact on the health outcomes of LEP patients. Previous researchers have called for an increase in standardized training for health care providers in regards to patient communication strategies including communicating with patients that have language barriers.(Patak et al., 2009) We hope that research evaluating the role that all different types of health care providers have in mitigating language barriers will continue to grow inside and outside the US.
We were disappointed to see that while the absolute number of studies increased, there was a drop in the percentage of published articles on outcomes research in the 2003–2010 time period compared to the pre-2003 period. The majority of studies continue to be descriptive in nature, despite the fact that it has already been well-documented that language barriers adversely affect access to health services(Jacobs et al., 2006, Pippins et al., 2007, Robert Wood Johnson Foundation, 2001); comprehension and adherence(Cheng et al., 2007, Jacobs et al., 2006); quality of care(Cohen et al., 2005, Diamond et al., 2009, Jacobs et al., 2003); and patient and provider satisfaction.(Arthur et al., 2014, Baker et al., 1996, Jacobs et al., 2006) Work demonstrating the effectiveness of interventions to overcome language barriers would likely more successfully drive the implementation of language access services. While we are not able to investigate this possibility, it may be that relatively limited funding opportunities for intervention studies, which tend to be more costly and higher risk than other types of research on this topic, may have prompted researchers interested in this topic to conduct descriptive studies which are much less resource intensive and therefore feasible with limited funding.
In the United States, the majority of research on language barriers continues to be done in the West and the Northeast. This is not that surprising given the fact that a large percentage of the LEP population lives in these regions,(Pandya et al., 2011) and that two large interpreter advocacy organizations, National Council on Interpreting in Health Care and The California Healthcare Interpreting Association originate from the Northeast and West respectively. It is interesting to note that the increase in states conducting language barriers research parallels the shifting immigration trends in the US. This finding along with previous research supports hypothesis that this increase in language barriers research is associated with increasing LEP populations in nontraditional immigration states within the US. (Schiaffino et al., 2014, Terrazas, 2011) We were unable to adequately describe the languages that were studied outside the US because greater than 60% of those studies did not define the languages they investigated or talked about language barriers generally. Within the US, Spanish continues to be the language most often studied, which is not surprising given that 65% of the LEP population in the US speak Spanish.( Pandya et al., 2011) The next most common language spoken is Chinese which makes up 6% of the LEP population. (Pandya et al., 2011) Again, similar to geographic location, it is interesting to observe how the distribution of languages studied in the US mirror the distribution of languages spoken by LEP people in the US.
Our study had several limitations. First, because the literature surrounding language barriers increased so dramatically since 2003, in the 2003–2010 sample we limited the literature review to articles published in the MEDLINE/PubMed and CINAHL databases. This could have led to accidental exclusion of some relevant literature. We feel that the risk of this is quite small as there is substantial overlap in articles listed in each index, and we believe we have captured most of the relevant literature in the 2003–2010 period in our analysis. Second, it is possible that because we relied on author reporting of specialty and language group that we may have misclassified some of the specialties into general and some of the languages into the unknown/more than one. Misclassification could be why these categories make up such a large percentage of the whole. We are not too concerned with this misclassification because it is likely that this misclassification occurred in both time periods and thus a comparison between time period would still show an accurate trend. Finally, by only including studies written in English we are limiting our sample to researchers who speak English well; however the vast majority of peer-reviewed literature is published in the English language, making it unlikely that we have omitted a substantial amount of relevant manuscripts.
This study documents that while there has been an increase in research surrounding language barriers, the research methods have not shifted from descriptive towards intervention as we expected. The increase in research surrounding language barriers is a positive step forward. We believe that the national policy change in 2003 that removed explicit guidance on how to comply with the policy in 2003 partially contributed to the increase in language barriers studies in the US. We believe that the work done by advocacy, governmental and health care organizations also have led to high levels of awareness in the health care community regarding the necessity of language barriers research.(Meyers et al., 2009, National Council on Interpreting in Health Care, 2011, Office of Minority Health) However, in spite of the increase in research, the national policy has not changed. This suggests that while increasing language barriers research is an important step forwards it isn’t sufficient to promote policy change at the national level in the US. Future research is needed to elevate policy to the next level. At this point, we should be having discussions about how to provide better linguistic access rather than continuing to document how they negatively impact care. In addition policy makers would benefit from more investigation as to how national policy changes can impact the research trajectory of a field and the provision of care.
To continue to move forward on issues relating to language barriers in the health care system, we need more research documenting how language concordant care influences patient outcomes, providing evidence for interventions that mitigate language barriers, and evaluating the cost effectiveness of providing language concordant care to patients with language barriers. We suggest that researchers around the world shift their attention towards these types of investigations as the populations and health care providers impacted by language barriers will continue to increase around the world over the next century.
The findings from our study show that continuing to document the existence of health disparities among patients with language barriers did not change national policy in the US and likely will bnot influence policy in most countries around the world. The international research community can help facilitate the creation of creative new policies that mitigate the impact of language barriers by studying new interventions that have the potential to lessen these health disparities and sharing these findings with policy makers.
It will, however, be difficult to shift language barriers research, without specific requests for proposals from major funding agencies such as the Agency for Healthcare Research and Quality in the US. Specifically, funding agencies should consider issuing requests for proposals that address the efficacy of linguistic access service interventions and of the cost of language barriers and the efforts to overcome them.(Jacobs et al., 2006) With the combined efforts of researchers and funding agencies, research relating to language barriers can begin to provide evidence-based solutions to improve care for patient populations with language barriers in health care settings.
Acknowledgments
This work would not have been possible without the support of National Council on Interpreting in Health Care (NCIHC), a multidisciplinary organization whose mission is to promote and enhance language access in health care in the United States. Support was provided by the Departments of Medicine and data storage and analytic software was supported by the Clinical and Translational Science Award (CTSA) program, previously through the National Center for Research Resources (NCRR) grant 1UL1RR025011, and now by the National Center for Advancing Translational Sciences (NCATS), grant 9U54TR000021. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. Additional funding for this project was provided by the UW School of Medicine and Public Health from the Wisconsin Partnership Program.
Footnotes
The authors have no conflicts of interest to declare.
References
- 2000 Aug 16; 65 Fed. Reg 50121. [Google Scholar]
- 2003 Aug 8; 68 Fed. Reg 47311. [Google Scholar]
- History of TIS National [Google Scholar]
- 1974 Lau et al. v. Nichols et al., 414 U.S. 563. [Google Scholar]
- National Register of Public Service Interpreters [Google Scholar]
- Young, suburban and mostly Asian: Canada's immigrant population surges. Canadian Press; 2013. [Google Scholar]
- Arthur KC, Mangione-Smith R, Meischke H, Zhou C, Strelitz B, Acosta Garcia M, Brown JC. Impact of English Proficiency on Care Experiences in a Pediatric Emergency Department. Acad Pediatr. 2014 doi: 10.1016/j.acap.2014.06.019. [DOI] [PubMed] [Google Scholar]
- Australian Government. Australia's Migration Trends 2011–12 at a glance [Google Scholar]
- Baker DW, Parker RM, Williams MV, Coates WC, Pitkin K. Use and effectiveness of interpreters in an emergency department. JAMA. 1996;275:783–788. [PubMed] [Google Scholar]
- Chen AH, Youdelman MK, Brooks J. The legal framework for language access in healthcare settings: Title VI and beyond. J Gen Intern Med. 2007;22(Suppl 2):362–367. doi: 10.1007/s11606-007-0366-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng EM, Chen A, Cunningham W. Primary language and receipt of recommended health care among Hispanics in the United States. J Gen Intern Med. 2007;22(Suppl 2):283–288. doi: 10.1007/s11606-007-0346-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen AL, Rivara F, Marcuse EK, McPhillips H, Davis R. Are language barriers associated with serious medical events in hospitalized pediatric patients? Pediatrics. 2005;116(3):575–579. doi: 10.1542/peds.2005-0521. [DOI] [PubMed] [Google Scholar]
- Diamond LC, Schenker Y, Curry L, Bradley EH, Fernandez A. Getting by: underuse of interpreters by resident physicians. J Gen Intern Med. 2009;24(2):256–262. doi: 10.1007/s11606-008-0875-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diez Guardia N, Pichelmann K. Labour Migration Patterns in Europe: Recent Trends, Future Challenges. 2006 Sep [Google Scholar]
- Diez Guardia N, Pichelman K. Labour Migration Patterns in Europe: Recent Trends, Future Challenges. 2006 Sep [Google Scholar]
- Fassaert T, Peen J, van Straten A, de Wit M, Schrier A, Heijnen H, Cuijpers P, Verhoeff A, Beekman A, Dekker J. Ethnic differences and similarities in outpatient treatment for depression in the Netherlands. Psychiatric Services. 2010;61(7):690–697. doi: 10.1176/ps.2010.61.7.690. [DOI] [PubMed] [Google Scholar]
- Government of Canada. Immigration and Ethnocultural Diversity in Canada. 2011 [Google Scholar]
- Healthcare Interpretation Network. National Standard Guide for Community Interpreting Services. Toronto, Canada: 2007. [Google Scholar]
- Jacobs E, Agger-Gupta N, Chen A, Piotrowski A, Hardt E. Language barriers in health care settings: an annotated bibliography of the research literature. Woodland Hills, CA: The California Endowment; 2003. [Google Scholar]
- Jacobs E, Chen AH, Karliner LS, Agger-Gupta N, Mutha S. The need for more research on language barriers in health care: a proposed research agenda. Milbank Q. 2006;84(1):111–133. doi: 10.1111/j.1468-0009.2006.00440.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyers K, Tang G, Fernandez A. Responding to the Language Challenge: Kaiser Permanente's Approach. The Permanente Journal. 2009;13(3):77–83. doi: 10.7812/tpp/08-103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray L, Windsor C, Parker E, Tewfik O. The experiences of African women giving birth in Brisbane, Australia. Health Care for Women International. 2010;31(5):458–472. doi: 10.1080/07399330903548928. [DOI] [PubMed] [Google Scholar]
- National Council on Interpreting in Health Care. National Standards for Healthcare Interpreter Training Programs. 2011 [Google Scholar]
- Neighborhood Health Plan of Rhode Island. Incentive to Care: Paying Healthcare Organizations to Provide Interpreter Services-White Paper [Google Scholar]
- Norstrom E. Cultural diversity, Multilingualism and Ethnic Minorities in Sweden. International Webjournal. 2010 [Google Scholar]
- Office of Minority Health. CLAS & the CLAS Standards [Google Scholar]
- Ou L, Chen J, Hillman K. Health services utilisation disparities between English speaking and non-English speaking background Australian infants. BMC Public Health. 2010;10:182. doi: 10.1186/1471-2458-10-182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pandya C, McHugh M, Batalova J. Limited English Proficient Individuals in the United States: Number, Share, Growth, and Linguistic Diversity. Washington DC: 2011. [Google Scholar]
- Patak L, Wilson-Stronks A, Costello J, Kleinpell RM, Henneman EA, Person C, Happ MB. Improving patient-provider communication: a call to action. J Nurs Adm. 2009;39(9):372–376. doi: 10.1097/NNA.0b013e3181b414ca. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pippins JR, Alegria M, Haas JS. Association between language proficiency and the quality of primary care among a national sample of insured Latinos. Med Care. 2007;45(11):1020–1025. doi: 10.1097/MLR.0b013e31814847be. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ponce NA, Hays RD, Cunningham WE. Linguistic disparities in health care access and health status among older adults. J Gen Intern Med. 2006;21(7):786–791. doi: 10.1111/j.1525-1497.2006.00491.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poureslami I, Rootman I, Doyle-Waters MM, Nimmon L, Fitzgerald JM. Health Literacy, Language, and Ethnicity-Related Factors in Newcomer Asthma Patients to Canada: A Qualitative Study. J Immigr Minor Health. 2010 doi: 10.1007/s10903-010-9405-x. [DOI] [PubMed] [Google Scholar]
- Puthussery S, Twamley K, Macfarlane A, Harding S, Baron M. 'You need that loving tender care': maternity care experiences and expectations of ethnic minority women born in the United Kingdom. Journal of Health Services Research & Policy. 2010;15(3):156–162. doi: 10.1258/jhsrp.2009.009067. [DOI] [PubMed] [Google Scholar]
- Robert Wood Johnson Foundation. Hablamos Juntos. Princeton, NJ: 2001. New survey shows language barriers causing many Spanish-speaking Latinos to skip care. [Google Scholar]
- Schiaffino MK, Al-Amin M, Schumacher JR. Predictors of language service availability in U.S. hospitals. Int J Health Policy Manag. 2014;3(5):259–268. doi: 10.15171/ijhpm.2014.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shin HB, Kominski RA. Language Use in the United States: 2007. 2010 [Google Scholar]
- Sokal R. A critical review of the literature on the uptake of cervical and breast screening in British South Asian women. Quality in Primary Care. 2010;18(4):251–261. [PubMed] [Google Scholar]
- Somerville W. Future Immigration Patterns and Policies in the United Kingdom. 2009 [Google Scholar]
- Taylor L. For immigrants, language barrier is a health barrier. 2012 [Google Scholar]
- Terrazas A. Immigrants in New-Destination States. US in Focus. 2011 [Google Scholar]
- Timmins CL. The impact of language barriers on the health care of Latinos in the United States: a review of the literature and guidelines for practice. J Midwifery Womens Health. 2002;47(2):80–96. doi: 10.1016/s1526-9523(02)00218-0. [DOI] [PubMed] [Google Scholar]
- United States Census Bureau. Language Use. Dec 30; [Google Scholar]