Abstract
To slow the growth of Medicare spending, some policy makers have advocated raising the Medicare eligibility age from the current sixty-five years to sixty-seven years. For the majority of affected adults, this would delay entry into Medicare and increase the time they are covered by private insurance. Despite its policy importance, little is known about how such a change would affect national health care spending, which is the sum of health care spending for all consumers and payers—including governments. We examined how spending differed between Medicare and private insurance using longitudinal data on imaging and procedures for a national cohort of individuals who switched from private insurance to Medicare at age sixty-five. Using a regression discontinuity design, we found that spending fell by $38.56 per beneficiary per quarter—or 32.4 percent—upon entry into Medicare at age sixty-five. In contrast, we found no changes in the volume of services at age sixty-five. For the previously insured, entry into Medicare led to a large drop in spending driven by lower provider prices, which may reflect Medicare's purchasing power as a large insurer. These findings imply that increasing the Medicare eligibility age may raise national health care spending by replacing Medicare coverage with private insurance, which pays higher provider prices than Medicare does.
INTRODUCTION
As the US economy recovers and increasing numbers of Americans gain health insurance, health care spending growth is expected to accelerate.1–4 Amid mounting pressure to control Medicare spending, some lawmakers have proposed raising the Medicare eligibility age.5,6 The Congressional Budget Office estimates that if the Medicare eligibility age changed from sixty-five to sixty-seven, most of those who would need to wait longer to receive Medicare coverage would stay in their private plans until age sixty-seven.7,8 Therefore, to evaluate this proposal it is crucial to understand how health care spending and use differ between Medicare and private insurance.
While most Americans transition to Medicare from private coverage, little is known about how health care use and spending change during this transition. Earlier work examining the transition to Medicare at age sixty-five has focused primarily on previously uninsured adults entering Medicare, a significantly smaller share of Medicare entrants compared to the previously insured, and on a limited set of outcomes including mortality,9 self-reported health,10 and utilization.11–14
In contrast, we examined how health care spending, utilization, and price differ for adults with private insurance before and after they gain Medicare coverage at age sixty-five. We measured spending as the sum of insurer-paid amounts and enrollee cost sharing. We focused on outpatient imaging and procedures, which are categories of services with fully reported data from Truven Health Analytics for adults before and after they turn sixty-five. The detailed claims information and longitudinal nature of the data allowed us to control flexibly for age (we used age in months), time, and individual characteristics, which would otherwise threaten to confound comparisons of traditional Medicare and private insurance.
We used a regression discontinuity design that adjusted for age trends and quarter, year, and individual fixed effects. With this design and a continuously enrolled national cohort of individuals, our study provides the first causal estimates of the difference in health care spending, volume, and price between traditional Medicare and private insurance. Previous studies have shown that Medicare prices are lower than those of private insurers.15,16 However, little is known about how or whether providers respond to Medicare's lower prices. If providers respond by seeing fewer Medicare patients, we would expect to see a drop in health care use at age sixty-five, as Medicare becomes the primary payer. Instead, our results indicate that Medicare beneficiaries do not face reduced access upon entry to the program, at least as measured by health care use—which is unchanged before and after age sixty-five. One possible explanation for this is providers' willingness to contract with Medicare despite its lower rates, which may be a result of Medicare's purchasing power as a large insurer.17
DATA AND METHODS
Population
We acquired data on 1,387,534 individuals who transitioned from commercial insurance to Medicare at age sixty-five in Truven Health Analytics' 2007–13 Medicare and Commercial Claims and Encounters database, a large nationwide convenience sample of employer-sponsored health insurance enrollees at large employers. These data contain fully integrated patient-level claims and enrollment information, including benefit design and cost sharing.18
We excluded individuals who did not have at least one year of continuous enrollment before and after entering Medicare at age sixty-five and individuals with Social Security Disability Insurance (SSDI) or end-stage renal disease, who are eligible for Medicare before age sixty-five.
We restricted the sample to retired individuals, since active workers often retain employer-sponsored insurance as their primary coverage after age sixty-five. We limited our sample to individuals whose commercial plan before age sixty-five was a broad network plan (indemnity, preferred provider organization, or point-of-service plan) and who entered traditional Medicare instead of Medicare Advantage. We excluded Medicare Advantage because of concerns that capitated claims are not always reported to the former employer, and hence we might not observe all of those claims. Finally, we excluded individuals with any capitated claims or claims for which the final paid amount was negative.19
Our final sample consisted of 200,870 continuously enrolled individuals. Importantly, each individual's claims and enrollment information could be tracked from when he or she had private insurance to when he or she was covered by Medicare—a unique advantage of using these longitudinal data that was lacking in the previous literature.
Data And Variables
Our primary outcomes were spending, volume, and price at the person-quarter level. For our spending analyses, the dependent variable was claims payments, which reflect negotiated prices among commercial enrollees, administratively set prices for Medicare beneficiaries, and patient cost sharing. Cost sharing for a given service was the sum of its copayment, coinsurance, and deductible. For utilization analyses, we constructed counts of services. Services with both professional and facility claims on the same day were counted once. For prices, the actual paid amounts reflect negotiated rates between private insurers and providers. We calculated a price index by dividing spending by utilization, using mean prices at the person-quarter level.
We decomposed health care spending by type of service, and we focused on services for which we had complete payment data from both the payer and patient. Since Medicare supplemental coverage applies only to Medicare-covered services that contain cost sharing, we restricted our analyses to the following two categories of services that consistently have cost sharing in traditional Medicare: imaging and procedures. In our main analyses we examined total health care spending, which included the actual amount paid by payers that reflected payer-provider negotiated prices (or administered prices in the case of traditional Medicare) and enrollee cost sharing. We also analyzed the use of and average prices for these services.
In subgroup analyses we analyzed a number of sentinel services with large sample sizes, including x-rays, computed tomography (CT) scans, and magnetic resonance imaging (MRI); and ophthalmologic, dermatologic, respiratory, and other procedural services. The service group codes we examined for both categories are listed in online Appendix 1.20 Most laboratory tests and many office visits, such as preventive visits and “Welcome to Medicare” visits, do not require cost sharing from Medicare beneficiaries. Therefore, they are not consistently reported to employers that offer supplemental coverage and do not consistently appear in the data.21,22 Similarly, deductibles for inpatient care are set on an episode basis and extend to sixty days after the end of the most recent inpatient or skilled nursing facility stay.23 As a result, if a readmission occurs within this benefit period, there is no additional cost sharing, and the readmission may not appear in the Truven claims data. Thus, we focused on services that were reliably reported each time a claim was generated.
Lastly, because of data confidentiality protections, patient age was reported only at the year and month level. Since our claims included exact dates of service, we could not reliably assign claims to a given month for individuals who switched coverage. To address this, we excluded any month immediately before a plan switch from the data, as was done in a previous study on the transition into Medicare.9
Statistical Analysis
We used a regression discontinuity design to identify the causal effect of entry into Medicare on total health care spending, volume, and price for previously insured adults. Regression discontinuity—an increasingly common method in empirical research—makes it possible to identify effects caused by a policy change.24⇓–26 We compared changes in spending, volume, and price from shortly before to shortly after the Medicare eligibility threshold at age sixty-five. As was done in previous studies, we modeled age trends as continuous polynomials and attributed discontinuities in outcomes at age sixty-five to the effect of entry into Medicare.
Base regression models were estimated using ordinary least squares with second-order polynomials (quadratic form) that allowed for different age trends before and after age sixty-five.27 Our independent variable of interest was an indicator for age sixty-five, which captured sharp changes in the outcomes of interest at the Medicare eligibility threshold. Because our treatment-determining variable was discrete (age), the treatment effect of Medicare was not identified without assuming a parametric functional form.28 We adjusted for individual fixed effects, age, and quarter and year fixed effects. Standard errors were clustered by individual and by age in quarters and reported with two-tailed p values. More details about our model specification are provided in Appendix 2.20 In sensitivity analyses we altered various aspects of the model, including functional form, covariates, and bandwidth on either side of the discontinuity at age sixty-five. Our base model used a quadratic functional form because lower-order polynomial functions have been shown to be preferable.29 All analyses used Stata, version 13.
Limitations
Our study had several limitations. First, our regression discontinuity analyses relied on the assumption that the dependent variables of interest would evolve smoothly with age in the absence of the transition to Medicare at age sixty-five.30 Although this assumption could not be fully tested, we partially tested it by examining spending trends for individuals with SSDI. These beneficiaries enroll in Medicare early and thus experience no change in coverage at age sixty-five. If outcomes were discontinuous for these individuals at age sixty-five, that would suggest that other factors in addition to the switch to Medicare might have biased our results. Reassuringly, spending, volume, and price trended smoothly across age sixty-five for adults in the sample with SSDI (Appendix 7).20
Second, data limitations precluded the assessment of all types of services. Since all of the people in our sample of Medicare beneficiaries received some form of supplemental retiree coverage, we did not consistently observe claims for services covered by Medicare with no cost sharing. To address this limitation conservatively, we restricted our analysis to outpatient imaging and surgery services subject to Medicare Part B cost sharing. Nevertheless, Medicare coverage may have different implications for those services that we did not study, including laboratory tests, office visits, and inpatient care. We were also unable to analyze the quality of care. Although we found little change in utilization, we could not observe whether lower Medicare prices drove beneficiaries to receive care from lower-quality providers or to receive lower-quality care.
Third, our study sample was not representative of all adults who enter Medicare at age sixty-five. Because of data limitations, we observed only individuals who had private insurance before entering Medicare. Although this represents the bulk of adults entering Medicare, Medicare beneficiaries may have previously been covered by Medicaid, enrolled in a plan listed on a health insurance exchange (or Marketplace), or uninsured. Our results thus are not generalizable to these populations. Nonetheless, they complement results of earlier work that examined how outcomes change at age sixty-five for the previously uninsured.9–13 In addition, our study did not include Medicare Advantage plans, which now cover about 30 percent of Medicare beneficiaries.31
Instead, we focused on the transition from broad network plans (indemnity plans and preferred provider organizations) to traditional Medicare, in an effort to compare insurance with similar benefit designs before and after age sixty-five. Because Medicare Advantage plans use different benefits, provider networks, and managed care strategies than traditional Medicare does, changes in health care spending and use at age sixty-five for enrollees in Medicare Advantage may differ from our findings.32–34 Relatedly, we did not include new beneficiaries who were previously covered by private plans on exchanges, since data on those individuals are not yet broadly available.
RESULTS
Population
Characteristics of the population are shown in Appendix 3.20 The 200,870 unique enrollees were ages 62–68 during the study period and were predominantly from the North Central and South regions of the United States; 56.7 percent of the enrollees were male. About 80 percent entered Medicare from a fee-for-service plan or a preferred provider organization; the remainder entered from a point-of-service plan. In total, the sample contained 3,911,685 unique enrollee quarters within a twelve-quarter (three-year) bandwidth of the Medicare eligibility age.
Spending
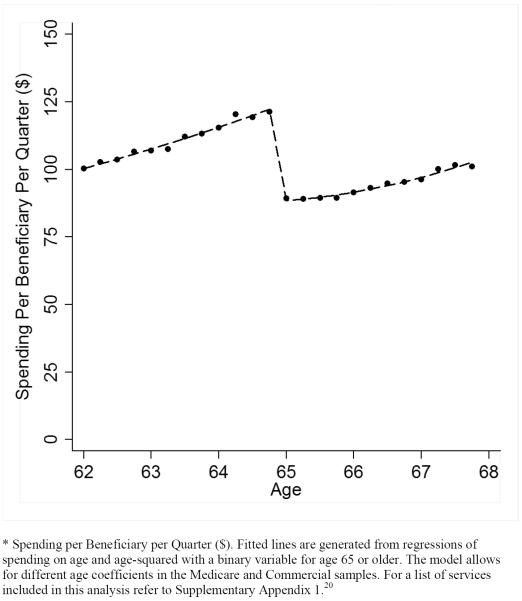
Unadjusted spending per person per quarter for the services we analyzed fell sharply after entry into Medicare, while spending trends were similar before and after age sixty-five (Exhibit 1). After spending an average of $119.12 per quarter in their last year with private insurance, new Medicare beneficiaries spent $89.28 per quarter, on average, in their first year in Medicare. In an adjusted analysis, average spending was $38.56 (or 32.4 percent) lower after transitioning into Medicare, compared to before the transition (p<0.001) (Exhibit 2).
Exhibit 1.
Unadjusted Spending Before and After Entry into Medicare*
Exhibit 2.
Adjusted spending before and after transition from private insurance to Medicare at age sixty-five
| Adjusted difference | ||||||
|---|---|---|---|---|---|---|
| Age 64 | Age 65 | Unadjusted difference | Amount | Percent change | p value | |
| Spending per beneficiary per quarter ($) | ||||||
| Total spending | 119.12 | 89.28 | −29.84 | −38.56 | −32.4 | <0.001 |
| Imaging | 84.06 | 57.15 | −26.92 | −33.75 | −40.2 | <0.001 |
| X-ray | 15.86 | 11.43 | −4.43 | −5.58 | −35.2 | <0.001 |
| CT and MRI | 57.03 | 38.42 | −18.61 | −24.20 | −42.4 | <0.001 |
| Electrocardiogram | 11.18 | 7.30 | −3.88 | −3.98 | −35.6 | <0.001 |
| Procedures | 35.05 | 32.13 | −2.93 | −4.82 | −13.8 | <0.001 |
| Cataract removal | 15.15 | 15.31 | 0.17 | −0.26 | −1.7 | 0.70 |
| Ophthalmologic | 7.75 | 6.15 | −1.60 | −2.28 | −29.4 | <0.001 |
| Dermatologic | 6.29 | 5.88 | −0.41 | −0.87 | −13.8 | <0.001 |
| Respiratory | 2.49 | 1.99 | −0.50 | −0.81 | −32.5 | <0.001 |
| Arthrocentesis | 3.37 | 2.80 | −0.58 | −0.60 | −17.8 | <0.001 |
| Utilization per 1,000 beneficiaries per quarter | ||||||
| Total volume | 608.28 | 631.59 | 23.31 | −3.24 | −0.5 | 0.52 |
| Imaging | 476.62 | 491.03 | 14.41 | −2.94 | −0.6 | 0.54 |
| X-ray | 215.34 | 220.26 | 4.93 | −3.33 | −1.5 | 0.28 |
| CT and MRI | 89.24 | 93.87 | 4.62 | 2.01 | 2.3 | 0.24 |
| Electrocardiogram | 172.04 | 176.90 | 4.86 | −1.62 | −0.9 | 0.48 |
| Procedures | 131.66 | 140.56 | 8.90 | −0.29 | −0.2 | 0.85 |
| Cataract removal | 8.97 | 12.02 | 3.05 | 2.58 | 28.8 | <0.001 |
| Ophthalmologic | 10.25 | 11.48 | 1.24 | 0.43 | 4.2 | 0.30 |
| Dermatologic | 72.95 | 75.02 | 2.08 | −3.77 | −5.2 | 0.007 |
| Respiratory | 8.58 | 9.24 | 0.66 | 0.00 | 0.0 | 0.99 |
| Arthrocentesis | 30.91 | 32.79 | 1.88 | 0.46 | 1.5 | 0.43 |
| Average price ($) | ||||||
| All services | 193.69 | 146.42 | −47.26 | −56.48 | −29.2 | <0.001 |
| Imaging | 167.30 | 115.41 | −51.89 | −63.20 | −37.8 | <0.001 |
| X-ray | 72.68 | 52.50 | −20.18 | −23.55 | −32.4 | <0.001 |
| CT and MRI | 660.44 | 429.64 | −230.81 | −278.01 | −42.1 | <0.001 |
| Electrocardiogram | 55.65 | 35.88 | −19.77 | −17.32 | −31.1 | <0.001 |
| Procedures | 279.34 | 239.56 | −39.79 | −37.07 | −13.3 | <0.001 |
| Cataract removal | 1,676.24 | 1,239.85 | −436.39 | −183.72 | −11.0 | 0.22 |
| Ophthalmologic | 721.51 | 539.64 | −181.86 | −202.25 | −28.0 | <0.001 |
| Dermatologic | 93.31 | 84.51 | −8.81 | −8.14 | −8.7 | <0.001 |
| Respiratory | 251.51 | 194.04 | −57.47 | −72.34 | −28.8 | 0.001 |
| Arthrocentesis | 108.51 | 83.88 | −24.63 | −20.52 | −18.9 | <0.001 |
SOURCE Authors' analysis. NOTES Our sample contained data on 200,870 people when they were ages sixty-four and sixty-five. All spending and prices are in 2013 US dollars. Adjusted differences are based on a regression discontinuity model that controlled for age, quarter, year, and individual fixed effects. A detailed description of the regression specification is available in Appendix 2 (see Note 20 in text). Categories of services were designated according to the Medicare procedure groups, a procedure commonly used by commercial insurers. CT is computed tomography. MRI is magnetic resonance imaging.
Decomposition of spending by service category highlighted this result (Appendix 4).20 Unadjusted spending for imaging decreased from $84.06 per beneficiary per quarter at age sixty-four to $57.15 at age sixty-five, with adjusted savings of $33.75 (40.2 percent) attributable to entry into Medicare. Subgroup analyses demonstrated savings of $5.58 for x-rays, $24.20 for CT scans and MRIs, and $3.98 for electrocardiograms (Exhibit 2). Analogously, spending for procedures decreased from $35.05 to $32.13, with adjusted savings of $4.82 attributable to Medicare. This was reflected in subgroup analyses as well, with most procedural subcategories showing a significant reduction in spending after entry into Medicare.
The results from our sensitivity analyses were consistent with our general findings (Appendices 5 and 6).20 Of note, results were very similar across alterations in the model's bandwidth, functional form, and control variables, including the removal of individual, year, or quarter fixed effects. In addition, Medicare beneficiaries who were SSDI recipients and therefore experienced no change in coverage at age sixty-five exhibited no change in spending at that age (Appendix 7).20 This strengthens our inference that the sharp decrease in spending for the main sample of individuals without SSDI at age sixty-five is attributable to entry into Medicare.
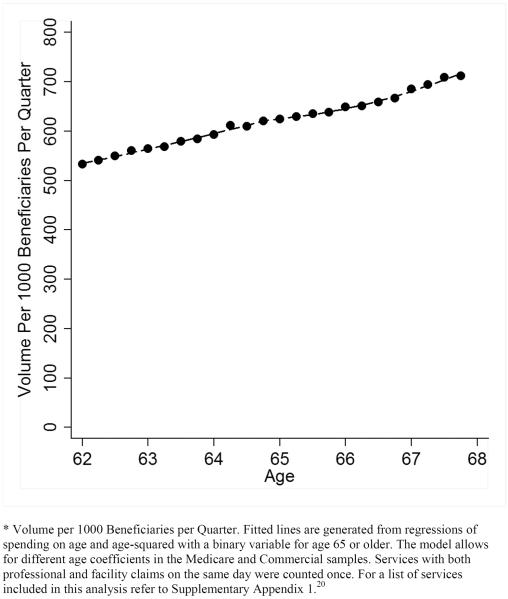
Volume
Unadjusted total volume of services showed no discontinuous changes at age sixty-five (Exhibit 3). A decomposition of this unadjusted analysis by type of service is shown in Appendix 8.20 This was consistent with adjusted analyses, which found a reduction in quarterly volume of 3.24 (p=0.52) services per 1,000 beneficiaries per quarter after the transition into Medicare (Exhibit 2). Similarly, the changes in use of imaging and procedures were not significant, which suggests that changes in spending were driven primarily by lower prices in Medicare. These findings were broadly consistent with the results of our sensitivity analyses (Appendices 5 and 6).20
Exhibit 3.
Unadjusted Volume Before and After Entry into Medicare*
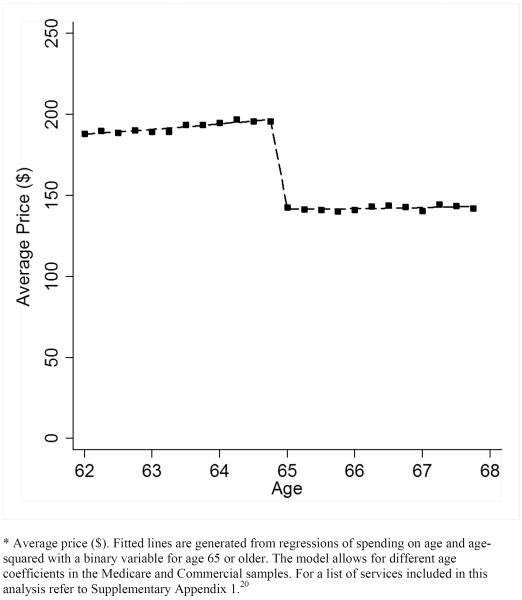
Price
The average price across all services decreased sharply after entry into Medicare, from $193.69 to $146.42 (Exhibits 2 and 4). A similar decomposition by type of service is provided in Appendix 9.20 In adjusted analyses, the average price decrease attributable to Medicare was $56.48, or 29.2 percent (p<0.001; Exhibit 2).
Exhibit 4.
Unadjusted Price Before and After Entry into Medicare*
The price decline was greater for imaging (37.8 percent; p<0.001) than for procedures (13.3 percent; p<0.001). In subgroup analyses, imaging price reductions ranged from 31.1 percent (p<0.001) for electrocardiograms to 42.1 percent (p<0.001) for CT scans and MRIs. Price reductions for procedures ranged from 8.7 percent (p<0.001) for dermatologic procedures to 28.8 percent (p=0.001) for respiratory procedures. Results from sensitivity analyses were consistent with these findings (Appendices 5 and 6).20 Of note, prices for cataract removal behaved differently from prices for other services: While cataract prices were lower after age sixty-five, the decline was not significant.
DISCUSSION
Entry into Medicare decreased health care spending by 32 percent for new beneficiaries previously covered by private insurance. Lower Medicare prices, rather than changes in health care use, drove the decrease in spending. While previous work has shown that providers' prices are lower in Medicare than in private insurance,15,16 we found no evidence that these prices reduced health care utilization. One possible explanation for providers' willingness to see Medicare patients at lower rates is Medicare's purchasing power as a large insurer.
To our knowledge, this study is the first attempt to measure differences in health care spending and use between private insurance and traditional Medicare using claims data from a national sample of continuously enrolled adults. Instead of relying on ecological methods, cross-sectional data, or simulations, we used unique longitudinal data and a regression discontinuity design to provide causal estimates of changes in health care spending, volume, and price at age sixty-five.35,36 Our study leveraged data that followed individuals as they aged into Medicare at sixty-five. This permitted us to control for a key confounder in studies that compare outcomes for individuals with Medicare to those with private insurance: namely, unobserved differences in the characteristics of the groups being compared.
Changes Attributable To Medicare Entry At Age 65
Our findings add to the evidence on changes in health care use and outcomes attributable to entry into Medicare at age sixty-five. First, we analyzed a national cohort of previously insured adults who switched from private insurance to traditional Medicare as their primary source of coverage at age sixty-five—a path followed by the majority of working US adults. Earlier studies have focused on previously uninsured individuals entering Medicare, who differ from continuously insured adults on measures of race, education, income, geography, health status, and health behaviors.10
Second, earlier studies that included previously insured beneficiaries used them as controls instead of focusing on their outcomes, and they analyzed measures of health care utilization constructed from household surveys or hospital discharge data.9–14 In contrast, we used detailed claims data integrated with enrollment information. Finally, our estimates of how spending and volume change for imaging and surgery at age sixty-five complement findings from earlier studies, which report no decreases (and some increases) in the volume of office visits and certain tests upon entry to Medicare.10,11
Increasing The Medicare Eligibility Age
Our results also help forecast how proposals to increase the Medicare eligibility age would affect health care spending. In this discussion we consider national health care spending and government health care spending separately.
National Health Spending
National health care spending is the sum of health care spending for all consumers and payers (including government payers). The Congressional Budget Office projects that the majority of people who would lose Medicare coverage if the eligibility age were increased would continue to be covered by private insurance.7,8 For these individuals, our study suggests that between ages sixty-five and sixty-seven, national health care spending would increase by roughly 30 percent for the services we examined. This increase would be because the use of outpatient imaging and surgery would be unlikely to change for adults who retained private insurance, but health care providers would be reimbursed by private insurers at negotiated prices that are higher than what Medicare would pay.
Our findings are consistent with an analysis by the Henry J. Kaiser Family Foundation arguing that increasing the Medicare eligibility age would raise overall health care spending.37 For example, the Kaiser Family Foundation estimated that $5.7 billion in net savings to the federal government in the first year would be offset by a net increase of $3.7 billion in out-of-pocket spending for people ages sixty-five and sixty-six and an increase of $4.5 billion in employers' medical costs for retirees.37 According to the foundation's estimates, health care spending would be 20 percent higher for individuals who had private employer-sponsored coverage instead of Medicare—a spending difference that is a third lower than what we found.
Government Spending
Of particular interest to policy makers is how an increase in the Medicare eligibility age would affect government spending. To account for the full effect of such a change on government spending, one must consider several additional factors. These include increased federal subsidies to individuals with private insurance from the exchanges, increased spending on beneficiaries eligible for Medicaid alone or with Medicare, and changes in premiums for the remaining Medicare beneficiaries.37
The Congressional Budget Office estimates that if the Medicare eligibility age were raised to sixty-seven, Medicare spending would be $17.1 billion lower than projected in 2023 but that offsetting subsidy spending, Medicaid spending, and revenue losses would sum to $10.4 billion, resulting in a net decrease in the deficit of $6.7 billion.38 By 2038 Medicare spending would be 3 percent lower than projected, decreasing its share of the gross domestic product from 4.9 to 4.7 percent, but two-thirds of the savings would be offset by the above factors.
Finally, our regression discontinuity estimates were based on changes in health care use and spending that happen right around age sixty-five. Some proposals, as we have noted, would raise the Medicare eligibility age to sixty-seven. Such a large increase could trigger broader changes in health care markets that would limit the generalizability of our findings. For example, if more individuals retained private insurance after age sixty-five, this might have the effect of increasing insurers' market power and altering providers' negotiated prices. In addition or alternatively, private insurers and self-insured employers might adjust their benefits to account for their risk pools' getting older. Lastly, the expansion of private insurance might reduce the pressure for health care providers to cross-subsidize—the practice of raising rates charged to private insurers to cover losses from government payers.
Conclusion
Our finding that Medicare's lower prices reduce health care spending but not utilization as people transition from private insurance to Medicare has important policy implications. First, it provides evidence on how spending and access differ between Medicare and private insurance, thereby helping policy makers forecast the impact of proposed changes in the Medicare eligibility age on health care spending and beneficiary access.
Second, and more broadly, it provides new insight into the effect of Medicare's market power on health care prices and access. If this finding is generalizable to other health care services, populations, and payers, it suggests that insurers with market power can pay lower rates than insurers that lack market power without losing access to providers.
Supplementary Material
Acknowledgements
This research was supported by a grant from the National Science Foundation to Jacob Wallace (Grant No. DGE 1144152) and a Ruth L. Kirschstein National Research Service Award for Individual Predoctoral MD/PhD Fellows from the National Institute on Aging to Zirui Song (Award No. F30-AG039175). The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the National Science Foundation or National Institutes of Health.
References / End Notes
- 1.Sisko AM, Keehan SP, Cuckler GA, Madison AJ, Smith SD, Wolfe CJ, et al. National health expenditure projections, 2013–23: faster growth expected with expanded coverage and improving economy. Health Aff (Millwood) 2014;33(10):1841–50. doi: 10.1377/hlthaff.2014.0560. [DOI] [PubMed] [Google Scholar]
- 2.Cuckler GA, Sisko AM, Keehan SP, Smith SD, Madison AJ, Poisal JA, et al. National health expenditure projections, 2012–22: slow growth until coverage expands and economy improves. Health Aff (Millwood) 2013;32(10):1820–31. doi: 10.1377/hlthaff.2013.0721. [DOI] [PubMed] [Google Scholar]
- 3.Keehan SP, Cuckler GA, Sisko AM, Madison AJ, Smith SD, Lizonitz JM, et al. National health expenditure projections: modest annual growth until coverage expands and economic growth accelerates. Health Aff (Millwood) 2012;31(7):1600–12. doi: 10.1377/hlthaff.2012.0404. [DOI] [PubMed] [Google Scholar]
- 4.Roehrig C. National health spending in 2014—acceleration delayed. N Engl J Med. 2014;371(19):1767–9. doi: 10.1056/NEJMp1409360. [DOI] [PubMed] [Google Scholar]
- 5.Capretta J. Raising Medicare eligibility a first step towards deficit reduction. U.S. News & World Report [serial on the Internet] 2012 Dec 5; [cited 2016 Mar 4]. Available from: http://www.usnews.com/debate-club/should-the-medicare-eligibility-age-be-raised/raising-medicare-eligibility-a-first-step-towards-deficit-reduction.
- 6.MacGuineas M, Carroll AE. Should the eligibility age for Medicare be raised? Wall Street Journal. 2012 Sep 18; [Google Scholar]
- 7.Congressional Budget Office . Options for reducing the deficit: 2015 to 2024 [Internet] Washington (DC): CBO; 2014 Nov [cited 2016 Mar 4]. Available from: https://www.cbo.gov/sites/default/files/cbofiles/attachments/49638-BudgetOptions.pdf. [Google Scholar]
- 8.Congressional Budget Office . Options for reducing the deficit: 2014 to 2023 [Internet] Washington (DC): CBO; 2013 Nov [cited 2016 Mar 4]. Available from: https://www.cbo.gov/sites/default/files/cbofiles/attachments/44715-OptionsForReducingDeficit-3.pdf. [Google Scholar]
- 9.Card D, Dobkin C, Maestas N. Does Medicare save lives? Q J Econ. 2009;124(2):597–636. doi: 10.1162/qjec.2009.124.2.597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McWilliams JM, Meara E, Zaslavsky AM, Ayanian JZ. Health of previously uninsured adults after acquiring Medicare coverage. JAMA. 2007;298(24):2886–94. doi: 10.1001/jama.298.24.2886. [DOI] [PubMed] [Google Scholar]
- 11.Card D, Dobkin C, Maestas N. The impact of nearly universal insurance coverage on health care utilization: evidence from Medicare. Am Econ Rev. 2008;98(5):2242–58. doi: 10.1257/aer.98.5.2242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McWilliams JM, Zaslavsky AM, Meara E, Ayanian JZ. Impact of Medicare coverage on basic clinical services for previously uninsured adults. JAMA. 2003;290(6):757–64. doi: 10.1001/jama.290.6.757. [DOI] [PubMed] [Google Scholar]
- 13.McWilliams JM, Meara E, Zaslavsky AM, Ayanian JZ. Use of health services by previously uninsured Medicare beneficiaries. N. Engl J Med. 2007;357(2):143–53. doi: 10.1056/NEJMsa067712. [DOI] [PubMed] [Google Scholar]
- 14.Decker SL. Medicare and the health of women with breast cancer. J Hum Resour. 2005;40(4):948–68. [Google Scholar]
- 15.Berenson R, Zuckerman S, Stockley K, Nath R, Gans D, Hammons T. An analysis using Medical Group Management Association data [Internet] Medicare Payment Advisory Commission; Washington (DC): Mar, 2010. What if all physician services were paid under the Medicare fee schedule? [cited 2016 Mar 7]. Available from: http://www.urban.org/sites/default/files/alfresco/publication-pdfs/412051-What-if-All-Physician-Services-Were-Paid-Under-the-Medicare-Fee-Schedule-.PDF. [Google Scholar]
- 16.Clemens J, Gottlieb JD. In the shadow of a giant: Medicare's influence on private physician payments [Internet] National Bureau of Economic Research; Cambridge (MA): Oct, 2013. [cited 2016 Mar 7]. (NBER Working Paper No. 19503). Available from: http://www.nber.org/papers/w19503.pdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chernew ME, Sabik LM, Chandra A, Gibson TB, Newhouse JP. Geographic correlation between large-firm commercial spending and Medicare spending. Am J Manag Care. 2010;16(2):131–8. [PMC free article] [PubMed] [Google Scholar]
- 18.Adamson DM, Chang S, Hansen LG. Health research data for the real world: the MarketScan® Databases [Internet] Thomson Reuters; New York (NY): Jul, 2008. [cited 2016 Mar 7]. Available from: http:// depts.washington.edu/chaseall/pdfs/white%20paper_Thomson%20Reuters% 20WP%20MarketScan%20Databases%200708.pdf. [Google Scholar]
- 19.These sample restrictions had the following effect on our study population. From the original 1,387,534 individuals we removed 149,335 who had capitated claims or claims with negative paid amounts, 858 with missing plan information, 5,368 with end-stage renal disease, 52,935 with SSDI, 121,421 for whom the only data available were during months in which they switched plans and for whom we did not observe all spending and utilization, 852,765 who were not coded as retired and who may have remained on private insurance past age sixty-five, and 17,739 who were not in broad network plans. In analyses available upon request, we examined how our overall spending result would have changed if we had not restricted our sample to individuals coded as retired and those in broad network plans. For this alternative sample, we found that overall spending fell by 20.2 percent after entry into Medicare at age sixty-five
- 20.Please see the Appendix
- 21. Medicare.gov . Your Medicare coverage: laboratory services (clinical) [Internet] Centers for Medicare and Medicaid Services; Baltimore (MD): [cited 2016 Mar 7]. Available from: http://www.medicare.gov/coverage/clinical-lab-services.html. [Google Scholar]
- 22. Medicare.gov . Your Medicare coverage: preventive visit and yearly wellness exams [Internet] Centers for Medicare and Medicaid Services; Baltimore (MD): [cited 2016 Mar 7]. Available from: http://www.medicare.gov/coverage/preventive-visit-and-yearly-wellness-exams.html. [Google Scholar]
- 23. Medicare.gov . Your Medicare coverage: inpatient hospital care [Internet] Centers for Medicare and Medicaid Services; Baltimore (MD): [cited 2016 Mar 9]. Available from: http://www.medicare.gov/coverage/hospital-care-inpatient.html. [Google Scholar]
- 24.Imbens GW, Lemieux T. Regression discontinuity designs: a guide to practice. J Econom. 2008;142(2):615–35. [Google Scholar]
- 25.Thistlethwaite DL, Campbell DT. Regression-discontinuity analysis: an alternative to the ex post facto experiment. J Educ Psychol. 1960;51(6):309–17. [Google Scholar]
- 26.Linden A, Adams JL. Combining the regression discontinuity design and propensity score-based weighting to improve causal inference in program evaluation. J Eval Clin Pract. 2012;18(2):317–25. doi: 10.1111/j.1365-2753.2011.01768.x. [DOI] [PubMed] [Google Scholar]
- 27.Lee DS, Lemieux T. Regression discontinuity designs in economics. J Econ Lit. 2010;48(2):281–55. [Google Scholar]
- 28.Lee DS, Card D. Regression discontinuity inference with specification error. J Econom. 2008;142(2):655–74. [Google Scholar]
- 29.Gelman A, Imbens G. Why high-order polynomials should not be used in regression discontinuity designs [Internet] National Bureau of Economic Research; Cambridge (MA): Aug, 2014. [cited 2016 Mar 7]. (NBER Working Paper No. 20405). Available from: http://www.nber.org/papers/w20405. [Google Scholar]
- 30.Angrist JD, Pischke J-S. Mostly harmless econometrics: an empiricist's companion. Princeton University Press; Princeton (NJ): 2009. [Google Scholar]
- 31.Jacobson G, Damico A, Neuman T, Gold M. Medicare Advantage 2015 data spotlight: overview of plan changes [Internet] Henry J. Kaiser Family Foundation; Menlo Park (CA): Dec 10, 2014. [cited 2016 Mar 7]. Available from: http://kff.org/medicare/issue-brief/medicare-advantage-2015-data-spotlight-overview-of-plan-changes/ [Google Scholar]
- 32.Landon BE, Zaslavsky AM, Saunders RC, Pawlson LG, Newhouse JP, Ayanian JZ. Analysis of Medicare Advantage HMOs compared with traditional Medicare shows lower use of many services during 2003–09. Health Aff (Millwood) 2012;31(12):2609–17. doi: 10.1377/hlthaff.2012.0179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ayanian JZ, Landon BE, Zaslavsky AM, Saunders RC, Pawlson LG, Newhouse JP. Medicare beneficiaries more likely to receive appropriate ambulatory services in HMOs than in traditional Medicare. Health Aff (Millwood) 2013;32(7):1228–35. doi: 10.1377/hlthaff.2012.0773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Stevenson DG, Ayanian JZ, Zaslavsky AM, Newhouse JP, Landon BE. Service use at the end-of-life in Medicare Advantage versus traditional Medicare. Med Care. 2013;51(10):931–7. doi: 10.1097/MLR.0b013e3182a50278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hadley J, Waidmann T. Health insurance and health at age 65: implications for medical care spending on new Medicare beneficiaries. Health Serv Res. 2006;41(2):429–51. doi: 10.1111/j.1475-6773.2005.00491.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Joyce GF, Keeler EB, Shang B, Goldman DP. The lifetime burden of chronic disease among the elderly. Health Aff (Millwood) 2005;24(Suppl 2):W5R18–29. doi: 10.1377/hlthaff.w5.r18. DOI: 10.1377/hlthaff.w5.r18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Henry J. Raising the age of Medicare eligibility: a fresh look following implementation of health reform [Internet] KFF; Menlo Park (CA): Jul 18, 2011. Kaiser Family Foundation. [cited 2016 Mar 7]. Available from: http://kff.org/medicare/report/raising-the-age-of-medicare-eligibility/ [Google Scholar]
- 38.Congressional Budget Office . Raising the age of eligibility for Medicare to 67: an updated estimate of the budgetary effects [Internet] Washington (DC): Oct, 2013. [cited 2016 Mar 7]. Available from: https://www.cbo.gov/sites/default/files/113th-congress-2013-2014/reports/44661-EligibilityAgeforMedicare.pdf. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.