Abstract
Importance
Racial differences in breast cancer treatment may result in part from differences in the providers from whom patients receive their care. However, little is known about differences in patients’ selection of providers.
Objective
To examine racial/ethnic differences in how women selected their surgeons and hospitals for breast cancer surgery.
Design, Setting, Participants
We surveyed 500 women (222 non-Hispanic white, 142 non-Hispanic black, 89 English-speaking Hispanic, and 47 Spanish-speaking Hispanic) from northern California cancer registries with stage 0–III breast cancer diagnosed during 2010–2011 (participation rate=68.5%). We used multivariate logistic regression to assess the reasons for surgeon and hospital selection by race/ethnicity, adjusting for other patient characteristics. We also assessed the association between reasons for physician selection and patients’ ratings of their surgeon and hospital.
Main Outcome
Reasons for surgeon and hospital selection, ratings of surgeon and hospital.
Results
The most frequently-reported reason for surgeon selection was referral by another doctor (77.6%); the most frequently-reported reason for hospital selection was because it was a part of a patient’s health plan (58.4%). After adjustment, 78.6%–86.5% of black and Spanish-speaking Hispanic women reported selecting their surgeon based on a doctor’s referral versus 75.7% of white women (P=.007). Black and Hispanic patients were less likely than white patients to report selecting their surgeon based on reputation (adjusted rates=17.5–22.1% of blacks and Hispanics vs. 31.9% of whites; P=.02). Black and Hispanic women were also less likely than white women to select their hospital based on reputation (adjusted rates=7.2%–15.0% vs. 23.2%, P=.003). Women who selected their surgeon based on reputation more often rated the care from their surgeon excellent (adjusted odds ratio [OR]=2.21, 95%CI=1.24–3.93); those reporting their surgeon was one of the only surgeons available through the health plan less often reported excellent quality of surgical care (OR=0.56, 95%CI=0.34–0.91).
Conclusions and Relevance
Compared with white breast cancer patients, minority patients were less actively involved in physician and hospital selection, relying more on physician referral and health plans rather than reputation. Interventions to promote involvement in provider selection may have potential for addressing disparities related to care from lower-quality providers.
INTRODUCTION
Racial/ethnic disparities in the utilization, quality, and delivery of medical care have been well described1–3 and may impact clinical outcomes for patients receiving cancer-directed treatments. Research suggests that differences in treatment and outcomes may occur in part because of differences in the providers and institutions where patients receive their care.4–14 Minority patients are more likely than white patients to receive medical care in lower quality hospitals,4,5,7,8,15–17 from providers caring for higher proportions of minority patients,18,19 and from physicians who are less well trained than those treating white patients.19 Among patients with breast cancer, black women are more likely than white women to undergo breast surgery at hospitals with lower rates of radiation following breast conservation.18 Hospital factors may also contribute to racial differences in delays in adjuvant breast cancer care.20
These racial/ethnic differences in where patients obtain oncology care may be due in part to differences in referral patterns among providers or patients’ involvement in selecting providers and preferences about those providers. A patient’s choice of hospital and physician may be influenced by past experiences, other medical conditions, type of surgery to be performed, hospital location, or recommendations by family and friends.21,22 Previous research has shown that breast cancer patients who ‘actively’ participate in selecting their surgeons are more likely to receive care in higher-volume hospitals and in hospitals with cancer programs.23 However, data are limited with regard to how women select their cancer providers and whether there are racial/ethnic differences in such decisions. Promoting thoughtful decision-making when choosing a physician and hospital may be an important element in addressing treatment disparities.
In this study, we interviewed a diverse sample of women with breast cancer in northern California to understand racial/ethnic differences in how patients select their surgeons and hospitals for breast cancer surgery, accounting for relevant factors such as educational attainment, insurance, health literacy, and English-language proficiency.
METHODS
Study Population
As previously described24 we identified 1,118 white, black, or Hispanic women from Regions 1/8 (San Francisco/Santa Clara) and Region 3 (Sacramento) of the California Cancer Registry (CCR) who were diagnosed with stage 0-III breast cancer in 2010–2011 and underwent primary surgery for their breast cancer. We obtained study approvals from the CCR, the California Health and Human Services Agency Committee for the Protection of Human Subjects, and Harvard Medical School’s Committee on Human Studies.
Survey Administration and Patient Enrollment
We mailed letters to eligible patients in English and Spanish inviting them to participate in a survey about their breast cancer care. Potential participants were contacted by phone. Women who agreed to participate provided verbal consent before the interview and received a $20 incentive upon interview completion. Interviews were conducted by bilingual trained study staff using computer assisted telephone interview software.
Survey
Participants were asked which of several statements describe how they selected their breast cancer surgeons22,23 and hospitals where they underwent cancer-directed surgery;21,22 including statements such as “I was referred to the surgeon by another doctor”, and “I chose this surgeon (or hospital) because of his/her (or its) reputation” (eTable 1). We also asked about patients’ priorities in making decisions about hospitals (e.g. “Which was more important when choosing the hospital that you went to—the location…reputation…or both equally important?”)21 as well as patients’ ratings of the overall quality of care provided by their surgeon and hospital. In addition, we collected information on race/ethnicity, educational attainment,25 insurance coverage at diagnosis,25 health literacy,26 and comorbidity25,27; Hispanic women were asked what language(s) they read and speak.28 Prior to participant enrollment, cognitive testing with 10 patients (in English and Spanish) demonstrated survey feasibility and clarity. A copy of the survey instrument is available upon request from the authors.
Response Rates
As described previously,24 among 1,118 patients, 231 refused participation, 317 could not be reached, and 68 were deceased/too ill. Among the 502 women surveyed, two self-identified as Asian and were excluded. The American Association for Public Opinion Research29 response rate was 47.8%; the participation rate among those for whom we had contact information was 68.5%. Fewer white women had no contact information (15%) than black (25%) and Hispanic (23%) women. However, among women with contact information (n=891), respondents (n=502) had similar baseline characteristics as non-respondents [n=389], except respondents were younger (mean age=58 vs. 64; p<.0001). Seventy of 136 Hispanic women were interviewed in Spanish.
Outcome Variables
The outcomes of interest were responses to questions about surgeon and hospital selection (eTable 1). Women identified all response(s) that applied to their selection of surgeon and hospital. Women replying ‘other’ were asked to specify further. We reviewed each ‘other’ response and re-categorized them as appropriate. For example, ‘primary care provider chose surgeon’ was re-categorized as ‘referred to surgeon by another doctor’; responses for ‘Kaiser selected surgeon’ and ‘surgeon assigned through health plan’ were categorized as ‘surgeon was one of the only ones available through my health care plan’. Responses suggesting active investigation into a surgeon’s reputation were re-categorized as ‘chose surgeon based on reputation’ (e.g., ‘researched him’, ‘second opinion’). Lastly, we created a new response category for the 14 women who reported selecting their surgeon because they had received prior treatment with that provider. Two ‘other’ responses were not re-categorized: “Spanish speaker” and “referral sent out to various surgeons--was the first to return call.” For hospital selection, the most common ‘other’ responses reflected the need to go to a hospital within their health plan, and we added a category for this (n=292); we also added a category for the 13 patients who reported prior treatment at that hospital.
Independent Variables
Our independent variable of interest was self-reported race/ethnicity. Because of the potential impact of language spoken on surgeon/hospital selection, we further categorized the 136 Hispanic participants based on responses to the question: “In general, what language(s) do you read and speak?”28 Women who responded ‘only Spanish’ or ‘more Spanish than English’ were categorized as Spanish-speaking Hispanic (n=47) and women who responded ‘both equally’, ‘more English than Spanish’, or ‘only English’ were categorized as English-speaking Hispanic (n=89).
Control Variables
Control variables included age, marital status, insurance status at diagnosis, disease stage (using registry data), number of self-reported comorbidities25,27 (past diagnosis of another cancer, diabetes, heart disease, stroke, chronic lung disease, kidney problem, depression/psychiatric problems), educational attainment, and mean health literacy score.26 We assessed health literacy using a 3-item screening tool:26 (1) “How confident are you filling out medical forms,” (2) “How often do you have problems learning about your medical condition?,” and (3) “How often do you have someone help you read hospital materials?” Responses used a 5-item Likert scale. After reversing responses for the first item, we assigned each answer a score of 1–5 (lower numbers reflect most confidence/fewest problems) and averaged the three scores. One participant did not answer question (2) above; we averaged her two other responses. Variables were categorized as in Table 1. We also examined the time from diagnosis to survey administration (median=2.8 years; Q1–Q3=2.1–2.7 years); this variable was not significantly associated with any responses for surgeon or hospital selection and was not included in multivariable models.
Table 1.
Participant characteristics by race/ethnicity for surveyed women (n=500) a
| Characteristic | Overall N=500 |
Non-Hispanic N=364 |
Hispanic N=136 |
p-value b | ||
|---|---|---|---|---|---|---|
| White N=222 |
Black N=142 |
English-speaking N=89 |
Spanish-speaking N=47 |
|||
| Age at diagnosis, N (%) | <.001 | |||||
| <50 | 129 (26) | 45 (20) | 32 (23) | 27 (30) | 25 (53) | |
| 50–59 | 153 (31) | 67 (30) | 48 (34) | 26 (29) | 12 (25) | |
| >60 | 218 (44) | 110 (50) | 62 (44) | 36 (40) | 10 (21) | |
| Marital status, N (%) | <.001 | |||||
| Married | 280 (56) | 149 (67) | 46 (32) | 51 (57) | 34 (72) | |
| Not married/unknown | 220 (44) | 73 (33) | 96 (68) | 38 (43) | 13 (28) | |
| Number of comorbid conditions, N (%)d | .94 | |||||
| 0 | 201 (40) | 89 (40) | 56 (39) | 39 (44) | 17 (36) | |
| 1 | 182 (36) | 84 (38) | 49 (35) | 30 (34) | 19 (40) | |
| 2+ | 117 (23) | 49 (22) | 37 (26) | 20 (22) | 11 (23) | |
| Educational attainment, N (%) | <.001 | |||||
| Some high school or less | 57 (11) | 6 (3) | 8 (6) | 13 (15) | 30 (64) | |
| High school diploma | 108 (22) | 45 (20) | 27 (19) | 27 (30) | 9 (19) | |
| Some college | 157 (31) | 70 (32) | 56 (39) | 28 (31) | 3 (6) | |
| College graduate | 178 (36) | 101 (46) | 51 (36) | 21 (24) | 5 (11) | |
| Insurance at diagnosis, N (%) | <.0001c | |||||
| None | 28 (6) | 3 (1) | 10 (7) | 3 (3) | 12 (26) | |
| Insured | 472 (94) | 219 (99) | 132 (93) | 86 (97) | 35 (75) | |
|
Mean health literacy score (lower=better literacy) (standard deviation) |
1.78 (1.04) | 1.48 (.77) | 1.65 (.95) | 1.94 (1.02) | 3.22 (1.22) | <.001 |
| Cancer stagee | .04 | |||||
| 0 | 86 (17) | 39 (18) | 14 (10) | 17 (19) | 16 (34) | |
| I | 199 (40) | 84 (38) | 61 (43) | 36 (40) | 18 (38) | |
| II | 166 (33) | 77 (35) | 50 (35) | 27 (30) | 12 (25) | |
| III | 49 (10) | 22 (10) | 17 (12) | 9 (10) | 1 (2) | |
Totals may not always equal 100% because of rounding
Using chi-square tests for categorical variables and the Kruskal-Wallis test for the health literacy score
Using the fisher’s exact test because some cell counts <5
Comorbidity was assessed by adding the number of self-reported medical conditions25,27 including other cancers, diabetes, heart attack, stroke, emphysema/chronic bronchitis/asthma/other chronic lung disease, kidney problems, and depression/other psychiatric illness.
Using cancer registry data; one case reported as stage IV was categorized as stage III
Statistical Analysis
We used χ2 tests to assess racial/ethnic differences in baseline characteristics and reasons for surgeon/hospital selection, the Fisher’s exact test to examine differences in insurance at diagnosis, and Kruskal Wallis tests to assess differences in mean health literacy scores. We used multivariate logistic regression to assess the probability of providing each possible response to the choice of surgeon or hospital (eTable 1) by race/ethnicity after re-categorizing ‘other’ responses as described above, adjusting for age, marital status, insurance, stage, education, mean health literacy score, and comorbidity. We calculated the adjusted proportion of patients’ reporting each reason for selection of surgeon or hospital by race/ethnicity, adjusting for covariates, based on the regression model.30 For the models examining ‘referred by a friend or family member’ to the surgeon and hospital, we omitted the insurance variable because no uninsured participants selected these reasons. Because of small numbers in some education categories for those reporting referral to the hospital by a relative/friend, we created a binary variable for education (college graduate vs. non-college graduate) for this model.
Finally, we described patients’ priorities for hospital location vs. reputation, ratings of surgical/hospital care, and likelihood of recommending their surgeon/hospital to family and friends by race/ethnicity.21 Using a second set of multivariate logistic regression models, we assessed whether (a) reported reasons for selecting physicians were associated with excellent ratings of surgeons and (b) reported reasons for selecting hospitals were associated with excellent ratings of hospital care. We performed separate models for each reason endorsed by at least 10% of women, adjusting for race/ethnicity, age, comorbidity, mean health literacy score, stage, and education. Other than the literacy item described above and one woman who did not rate hospital care quality, there was no item non-response.
RESULTS
Baseline characteristics for the 500 participants (222 white, 142 black, 89 English-speaking Hispanic, 47 Spanish-speaking Hispanic) are shown in Table 1. In general, Hispanic women were younger and had poorer mean health literacy scores compared with others and black women were less likely to be married than other groups. Spanish-speaking Hispanic women had the highest rates of no insurance at breast cancer diagnosis and the lowest educational attainment.
Surgeon Selection
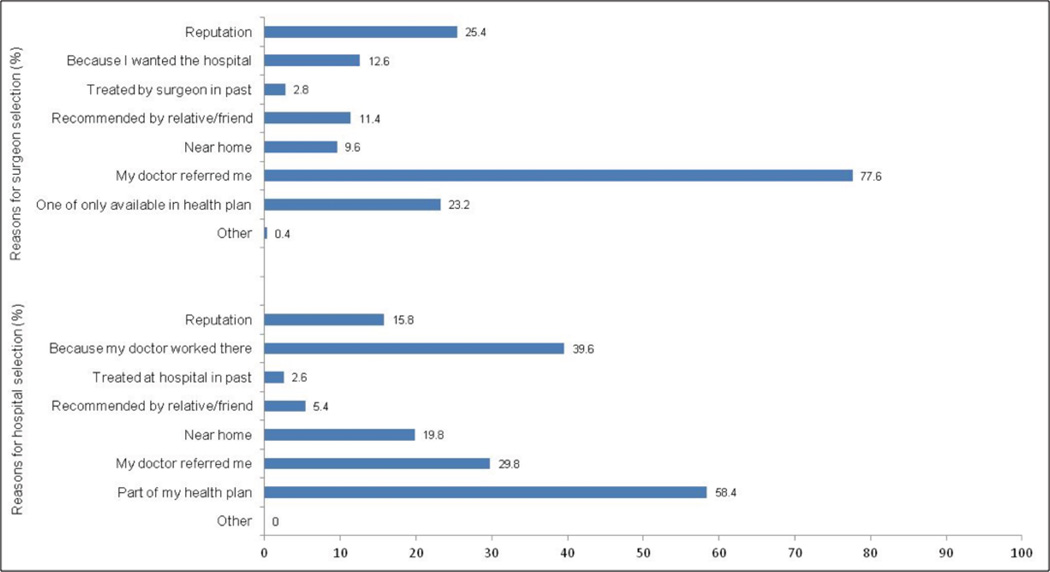
Of seven response options for selection of their surgeon, most women selected one (56%) or two (31%) responses. Approximately 81% of white women, 93% of black women, 88% of English-speaking Hispanic women, and 92% of Spanish-speaking Hispanic women selected one or two responses with the remaining participants selecting more than two reasons for selecting surgeons. Rates for each response are displayed in Figure 1 (upper bars) and stratified by race/ethnicity in Table 2. Most patients (77.6%) reported being referred by another doctor. Approximately 25% of women selected their surgeon based on reputation. Less than one-quarter of women provided other response options for surgeon selection.
Figure 1.
Unadjusted percentages for each response for why the surgeon (upper bars) and hospital (lower bars) were selected a
a Note: Women could select more than one reason for each question.
Table 2.
Unadjusted and adjusted rates (%) for positive responses to each question for physician selection and hospital selection by race/ethnicity
| Non-Hispanic | Hispanic | Non-Hispanic | Hispanic | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Question and responses | N (%) | White (n=222) |
Black (n=142) |
English Speaking (n=89) |
Spanish- speaking (n=47) |
p- valueb |
White (n=222) |
Black (n=142) |
English Speaking (n=89) |
Spanish- speaking (n=47) |
p- valuec,d |
Hosmer- Lemeshow goodness of fit (p value)h,i |
| 500 (100) | Unadjusted percent | Adjusted percent | ||||||||||
| Surgeon selection: Which of the following statements describe how the surgeon who performed your breast surgery was selected?e | ||||||||||||
| Chose surgeon based on his/her reputationc |
127 (25) | 34.2 | 16.9 | 21.3 | 17.0 | <.001 | 31.9 | 17.5 | 22.1 | 22.0 | .02 | .77 |
| Chose surgeon because I wanted to be treated at the medical institution where he/she workedc |
63 (13) | 17.6 | 7.0 | 12.4 | 6.4 | .01 | 17.0 | 7.0 | 12.9 | 7.1 | .06 | .35 |
| Surgeon recommended by relative or friendd |
57 (11) | 15.3 | 6.3 | 13.5 | 4.3 | .02 | 16.8 | 6.1 | 13.7 | 3.1 | .007 | .40 |
| Wanted surgeon who practiced near my homec |
48 (10) | 10.8 | 4.9 | 13.5 | 10.6 | .14 | 10.8 | 4.6 | 13.9 | 12.2 | .12 | .81 |
| Referred to surgeon by another doctorc |
388 (78) | 73.9 | 85.9 | 69.7 | 85.1 | .007 | 75.7 | 86.5 | 66.9 | 78.6 | .007 | .89 |
| Surgeon was one of the only ones available through health care planc |
116 (23) | 22.5 | 20.4 | 31.4 | 19.2 | .21 | 23.2 | 19.4 | 33.7 | 16.5 | .06 | .91 |
| Hospital selection: Which of the following statements describe how the hospital where you had your breast cancer surgery was selected?f | ||||||||||||
| Chose hospital because of its reputationc |
79 (16) | 22.5 | 9.2 | 14.6 | 6.4 | .001 | 23.2 | 8.3 | 15.0 | 7.2 | .003 | .77 |
| Chose hospital because I wanted to be treated at the medical institution where my doctor workedc |
198 (40) | 50.5 | 31.7 | 37.1 | 17.0 | <.001 | 48.9 | 31.7 | 37.8 | 17.2 | .001 | .46 |
| Hospital recommended by relative or friendd |
27 (5) | 5.0 | 5.6 | 7.9 | 2.1 | .57g | 5.1 | 5.4 | 8.3 | 1.9 | .49 | .76 |
| Wanted hospital near my homec |
99 (20) | 24.3 | 14.1 | 21.4 | 12.78 | .06 | 24.3 | 14.4 | 22.6 | 10.7 | .08 | .02 |
| Referred to hospital by my doctorc |
149 (30) | 25.7 | 32.4 | 27.0 | 46.8 | .03 | 28.4 | 30.5 | 27.1 | 38.4 | .67 | .76 |
| Hospital available through health planc |
292 (58) | 53.2 | 60.6 | 64.0 | 66.0 | .17 | 50.6 | 60.5 | 63.9 | 77.8 | .02 | .13 |
For each question, patients were instructed to select all responses that applied to them.
By chi-square testing for differences in responses by race/ethnicity
Using multivariable logistic regression, adjusting for age, comorbidity, marital status, mean health literacy score, insurance status, stage, and education. Bolded results are significant with p<.05.
Using multivariable logistic regression, adjusting for age, comorbidity, marital status, mean health literacy score, stage, and education. Bolded results are significant with p<.05.
Participants may be included in more than one model. Models were not performed for ‘treated by surgeon in past’ and ‘other’ because of the rarity of these responses
Participants may be included in more than one model. Models were not performed for ‘treated by hospital in past’ and ‘other’ because of the rarity of these responses
Using the fisher’s exact test because some cell counts <5
Models for surgeon selection had c-statistics ranging from .62–.72
Models for hospital selection had c-statistics ranging from .63–.71
In adjusted analyses (Table 2), black (86.5%) and Spanish-speaking Hispanic women (78.6%) had higher adjusted rates of selecting their surgeon based on physician referral than white (75.7%) and English-speaking Hispanic women (66.9, P=.007). Black (17.5%), Spanish-speaking (22.0%) and English-speaking Hispanic women (22.1%) were less likely to report selecting their surgeons based on reputation than white women (31.9%, P=.02) and to select surgeons based on recommendations by relatives/friends (3.1% to 13.7% for minority women vs. 16.8% for white women, P=.007).
Hospital Selection
Of seven response options for hospital selection for their breast cancer surgery, most women selected one (53%) or two (32%) reasons. Approximately 82% of whites, 89% blacks, 84% of English-speaking Hispanics, and 94% of Spanish-speaking Hispanics selected one or two responses, with the remaining women selecting more than two responses. Rates for each response are displayed in Figure 1 (lower bars) and stratified by race/ethnicity in Table 2, with the most frequent reason for hospital selection that the hospital was available through the patient’s health plan (58.4%).
In adjusted analyses, white women (23.2%) were more likely than black (8.3%), English-speaking Hispanic (15.0%) and Spanish-speaking Hispanic (7.2%) women to report choosing their hospital because of its reputation (P=.003, Table 2). Whites (48.9%) were also more likely than minority women (17.2% to 37.8%) to report selecting the hospital because they wanted to be treated at the hospital where their doctor worked (P=.001). Spanish-speaking Hispanic (77.8%), English-speaking Hispanic (63.9%) and black (60.5%) women were more likely than white women (50.6%) to report that they chose the hospital because it was a part of their health plan (P=.02). There were no racial/ethnic differences in reporting being referred to hospitals by their doctors. All models suggested good fit except the model assessing the outcome of choosing a hospital because ‘it was near my home’ (Hosmer Lemeshow P=0.02).
Hospital location and reputation
Most participants (64%) stated that they had other hospitals in their area to choose from for surgery (Table 3), and 44% reported that there were hospitals closer to their home than the one they selected. Overall, 51% of women reported that the hospital’s reputation was more important than location and reputation was more important for white women (60%) than black (45%), English-speaking Hispanic (55%), and Spanish-speaking Hispanic (23%) women (P<.0001).
Table 3.
Responses of surveyed patients to questions about decision making for their surgery21
| Question and possible responses | Number of respondents (%) with positive (yes) response | |||||
|---|---|---|---|---|---|---|
| Overall (n=500) |
White (n=222) |
Black (n=142) |
English- speaking Hispanic (n=89) |
Spanish- speaking Hispanic (n-47) |
p-valuea | |
| Location and reputation | ||||||
| Other than the hospital where you had your surgery, were there any other hospitals in your area where you could have had the operation? |
64 | 68 | 59 | 61 | 66 | .21 |
| Were any of the other hospitals closer to where you lived than the hospital where you had your breast surgery? |
44 | 47 | 47 | 34 | 47 | .10 |
| Which was more important when choosing the hospital you went to: | <.0001 | |||||
| Reputation more than location | 51 | 60 | 45 | 55 | 23 | |
| Location more important than reputation or both equally important | 49 | 40 | 55 | 45 | 77 | |
| Ratings of care | ||||||
| How would you rate the quality of care received by your surgeon for your breast cancer surgery? |
.37 | |||||
| Excellent | 77 | 78 | 75 | 81 | 68 | |
| Very good/good/fair/poor | 23 | 22 | 25 | 19 | 32 | |
| How likely would you be to recommend this surgeon to a friend or family member who needed the same operation you had? |
.11 | |||||
| Extremely likely | 68 | 72 | 62 | 73 | 62 | |
| Very likely/a little likely/not at all likely | 32 | 28 | 38 | 27 | 38 | |
| How would you rate the quality of your overall experience at this hospital?b | .87 | |||||
| Excellent | 63 | 63 | 64 | 63 | 57 | |
| Very good/good/fair/poor | 37 | 37 | 36 | 38 | 43 | |
| How likely would you be to recommend this hospital to a friend or family member who needed the same operation you had? |
.95 | |||||
| Extremely likely | 56 | 57 | 58 | 54 | 55 | |
| Very likely/a little likely/not at all likely | 44 | 43 | 42 | 46 | 45 | |
| How do you think the hospital where you had your surgery compares to other hospitals in your area? |
.38 | |||||
| Best | 21 | 20 | 20 | 25 | 26 | |
| Better than most | 28 | 32 | 27 | 24 | 17 | |
| About same/worse than most/I don’t know | 51 | 48 | 53 | 52 | 58 | |
By chi-square testing, unadjusted
One English-speaking Hispanic women did not answer this question
Ratings of care
Overall, most women, regardless of race/ethnicity, reported excellent ratings of the quality of care delivered by their surgeon (77%) and hospital (63%) and most women stated that they would be extremely likely to recommend their surgeon/hospital to family members or friends (68% and 56%, respectively, Table 3). Approximately 21% of women reported that their hospital was the ‘best’ compared to others in the area.
In adjusted analyses examining associations of patients’ reasons for selecting their surgeon with excellent ratings of care for the surgeon (Table 4), choosing a surgeon based on reputation was significantly associated with higher odds of reporting excellent care from their surgeon (adjusted odds ratio [OR]=2.21, 95%CI=1.24–3.93), while choosing a surgeon because of one’s health plan was associated with lower odds of reporting excellent care from the surgeon (OR=0.56, 95%CI=0.34–0.91, Table 4). No other responses for the selection of surgeons or hospitals were significantly associated with excellent ratings and race/ethnicity was not significantly associated with reporting excellent ratings for surgeon or hospital in any of the models.
Table 4.
Adjusted odds ratios for rating surgeon and hospital care as excellent
| Variable/response | Adjusted odds ratio (95% Confidence Interval) |
p-value | Hosmer- Lemeshow goodness of fit (P value) |
|---|---|---|---|
| Responses regarding surgeon selection and association with excellent rating for quality of health care provided by surgeona,b,e | |||
| Chose surgeon based on his/her reputation | 2.21 (1.24–3.93) | <.01 | .86 |
| Chose surgeon because I wanted to be treated at the medical institution where he/she worked | 1.56 (.75–3.27) | .24 | .80 |
| Surgeon recommended by relative or friend | 1.51 (.72–3.20) | .28 | .79 |
| Referred to surgeon by another doctor | 1.19 (.70–2.02) | .52 | .69 |
| Surgeon was one of the only ones available through health care plan | .56 (.34–.91) | .02 | .31 |
| Responses regarding hospital selection and association with excellent rating for quality of experience at the treating hospital a,c,d,e | |||
| Chose hospital because of its reputation | 1.23 (.72–2.09) | .44 | .78 |
| Chose hospital because I wanted to be treated at the medical institution where my doctor worked | 1.40 (.94–2.08) | .10 | .20 |
| Wanted hospital near my home | .95 (.60–1.52) | .84 | .37 |
| Referred to hospital by my doctor | 1.32 (.87–1.99) | .20 | .55 |
| Hospital available through health plan | 1.09 (.75–1.60) | .64 | .19 |
Using multivariable logistic regression, adjusting for race/ethnicity, age, comorbidity, marital status, stage, mean health literacy score, and education. Insurance was not included because of the rarity of uninsured status. Bolded results are significant with p<.05.
Each possible response with at least 10% of women answering ‘yes’ for the reasons for surgeon selection was added to base model (patient variables listed above) and then a final model was performed which included all possible responses for surgeon selection.
Each possible response with at least 10% of women answering ‘yes’ for the reasons for hospital selection was added to base model (patient variables listed above) and then a final model was performed which included all possible responses for hospital selection.
One English-speaking Hispanic women did not answer this question
Model c-statistics ranged from .64–.66 for ratings of surgeon and .59–.60 for ratings of hospital
DISCUSSION
In a large, diverse cohort of women with breast cancer, we observed variability in how women selected their surgeons and hospitals for their breast cancer-directed surgery. Most women relied on referrals from their physicians for selecting surgeons, particularly black women and Spanish-speaking Hispanic women. In addition, minority patients were less likely to report reputation as an important component of their decisions about surgeons and hospitals, and were more likely to select a hospital because it was part of their health plan. These findings suggest less active involvement of minority patients with regard to selecting providers for their care.
Prior studies have documented a more passive approach to medical care and decision-making for black and Hispanic versus white women, particularly for those who do not speak English.31–33 These studies have observed less active participation by minority and non-English speakers with more reliance on physicians to make decisions and to provide information about health conditions.31–33 This decision-making approach may be even more evident when a patient is anxious, vulnerable, and overwhelmed in the setting of a new breast cancer diagnosis or if a patient isn’t proficient in English. In our study, we could not assess whether a less active approach to provider selection led to worse quality of cancer care; however, women who selected the surgeon based on reputation rated the quality of care delivered by their surgeons more highly than others and women who were directed to their surgeon via their health plan rated the quality of care from their surgeon lower. Although more research is needed to fully understand the impact of patient engagement in provider selection on quality of care, outcomes, and patient experiences, interventions that promote more active patient involvement in this process may have potential for addressing disparities related to care from lower-quality providers.
Alternatively, since most patients in our cohort relied on referrals from physicians when selecting breast surgeons and hospitals, interventions could instead be targeted to referring physicians to ensure referrals to provider systems that deliver coordinated and high-quality cancer care. Surgeons are often the first cancer specialist a woman with a new diagnosis of breast cancer will encounter and thus may play a major role in securing high quality medical oncology and radiation oncology referrals. Thus, an initial referral to a high-quality surgeon and hospital may lead to high quality care throughout the cancer care continuum. However, we need more research on the potential associations of surgeons and other cancer care providers and how pre-existing patterns34–36 of referrals could be optimally modified.
Although location was important to some women in selecting their surgeon (10%) and hospital (20%) in our study, most women reported other hospitals in their area where they could have had their surgery, and nearly half of women reported that there were other hospitals closer to their home. Other evidence suggests that, particularly in areas with high levels of racial segregation, black patients are more likely than white patients to undergo major surgical procedures at lower quality hospitals despite living nearer to higher-quality hospitals.37 It is likely that factors such as comfort with receiving care in certain hospitals or physician referral patterns play a role in these decisions.
We recognize several study limitations. First, although population-based, we studied women in northern California where a relatively high proportion of women are insured by Kaiser Permanente.38 This may explain the large number of patients reporting that their health plan influenced selection. Second, we cannot rule out non-response bias, although responders were similar to non-responders. Third, recall bias may have affected findings, however the time to survey administration was not associated with responses for provider/hospital selection. Fourth, we lacked information about the sources (i.e. other providers, family members, etc.) patients used to classify surgeons/hospitals as ‘reputable’ when they provided this response; we also did not ask about women’s employment status. Finally, we did not ask women to provide a single most important reason for their choice of doctors and hospitals, which may have enabled us to better identify the most important factors. However, the vast majority of women only selected one or two responses and women also provided information on the relative importance of hospital reputation vs. location.
CONCLUSIONS
In conclusion, among a diverse group of breast cancer patients, we observed differences by race/ethnicity in the level of involvement in selecting providers and hospitals, with white women more likely than minority women to select providers based on reputation and less likely to be directed to providers by their health plan or other physicians. These findings may explain some of the segregation in care that has been observed in other studies.4,5,7,8,15–17 More research is needed on how these selection strategies (or lack thereof) affect the quality of care patients receive and how we can best intervene to guarantee excellent and equal care for all patients with breast cancer. Assuring thoughtful decision-making for provider and hospital selection may be an important element in addressing treatment disparities in cancer and has the potential to be an important focus for interventions.
Supplementary Material
Acknowledgments
FUNDING: Komen for the Cure Foundation. Dr. Keating is also supported by K24CA181510 from the National Cancer Institute.
DATA: The collection of cancer incidence data used in this study was supported by the California Department of Public Health as part of the statewide cancer reporting program mandated by California Health and Safety Code Section 103885; the National Cancer Institute’s Surveillance, Epidemiology and End Results Program under contract HHSN261201000140C awarded to the Cancer Prevention Institute of California, contract HHSN261201000035C awarded to the University of Southern California, and contract HHSN261201000034C awarded to the Public Health Institute; and the Centers for Disease Control and Prevention’s National Program of Cancer Registries, under agreement U58DP003862-01 awarded to the California Department of Public Health. The ideas and opinions expressed herein are those of the author(s) and endorsement by the State of California, Department of Public Health the National Cancer Institute, and the Centers for Disease Control and Prevention or their Contractors and Subcontractors is not intended nor should be inferred.
We thank all women who participated in interviews, the Cancer Registry of Greater California, Ana Guerrero for assistance with interviews, and Huichuan Lii for her programming expertise.
Footnotes
DISCLOSURES: none
REFERENCES
- 1.Trivedi AN, Zaslavsky AM, Schneider EC, Ayanian JZ. Trends in the quality of care and racial disparities in Medicare managed care. N Engl J Med. 2005 Aug 18;353(7):692–700. doi: 10.1056/NEJMsa051207. [DOI] [PubMed] [Google Scholar]
- 2.Jha AK, Fisher ES, Li Z, Orav EJ, Epstein AM. Racial trends in the use of major procedures among the elderly. N Engl J Med. 2005 Aug 18;353(7):683–691. doi: 10.1056/NEJMsa050672. [DOI] [PubMed] [Google Scholar]
- 3.Smedley BD, Stith AY, Nelson AR, editors. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care Appendix C. Federal-Level and Other Initiatives to Address Racial and Ethnic Disparities in Healthcare. National Academies Press; 2003. Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care, Institute of Medicine; pp. 384–391. [PubMed] [Google Scholar]
- 4.Jha AK, Orav EJ, Li Z, Epstein AM. Concentration and quality of hospitals that care for elderly black patients. Arch Intern Med. 2007 Jun 11;167(11):1177–1182. doi: 10.1001/archinte.167.11.1177. [DOI] [PubMed] [Google Scholar]
- 5.Hasnain-Wynia R, Baker DW, Nerenz D, et al. Disparities in health care are driven by where minority patients seek care: examination of the hospital quality alliance measures. Arch Intern Med. 2007 Jun 25;167(12):1233–1239. doi: 10.1001/archinte.167.12.1233. [DOI] [PubMed] [Google Scholar]
- 6.Regenbogen SE, Gawande AA, Lipsitz SR, Greenberg CC, Jha AK. Do differences in hospital and surgeon quality explain racial disparities in lower-extremity vascular amputations? Ann Surg. 2009 Sep;250(3):424–431. doi: 10.1097/SLA.0b013e3181b41d53. [DOI] [PubMed] [Google Scholar]
- 7.Barnato AE, Lucas FL, Staiger D, Wennberg DE, Chandra A. Hospital-level racial disparities in acute myocardial infarction treatment and outcomes. Med Care. 2005 Apr;43(4):308–319. doi: 10.1097/01.mlr.0000156848.62086.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Skinner J, Chandra A, Staiger D, Lee J, McClellan M. Mortality after acute myocardial infarction in hospitals that disproportionately treat black patients. Circulation. 2005 Oct 25;112(17):2634–2641. doi: 10.1161/CIRCULATIONAHA.105.543231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liu JH, Zingmond DS, McGory ML, et al. Disparities in the utilization of high-volume hospitals for complex surgery. Jama. 2006 Oct 25;296(16):1973–1980. doi: 10.1001/jama.296.16.1973. [DOI] [PubMed] [Google Scholar]
- 10.Lucas FL, Stukel TA, Morris AM, Siewers AE, Birkmeyer JD. Race and surgical mortality in the United States. Ann Surg. 2006 Feb;243(2):281–286. doi: 10.1097/01.sla.0000197560.92456.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lathan CS, Neville BA, Earle CC. Racial composition of hospitals: effects on surgery for early-stage non-small-cell lung cancer. J Clin Oncol. 2008 Sep 10;26(26):4347–4352. doi: 10.1200/JCO.2007.15.5291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Breslin TM, Morris AM, Gu N, et al. Hospital factors and racial disparities in mortality after surgery for breast and colon cancer. J Clin Oncol. 2009 Aug 20;27(24):3945–3950. doi: 10.1200/JCO.2008.20.8546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Morris AM, Wei Y, Birkmeyer NJ, Birkmeyer JD. Racial disparities in late survival after rectal cancer surgery. J Am Coll Surg. 2006 Dec;203(6):787–794. doi: 10.1016/j.jamcollsurg.2006.08.005. [DOI] [PubMed] [Google Scholar]
- 14.Zhang W, Ayanian JZ, Zaslavsky AM. Patient characteristics and hospital quality for colorectal cancer surgery. Int J Qual Health Care. 2007 Feb;19(1):11–20. doi: 10.1093/intqhc/mzl047. [DOI] [PubMed] [Google Scholar]
- 15.Sarrazin MV, Cannon KT, Rosenthal GE, Kaldjian LC. Racial differences in mortality among veterans hospitalized for exacerbation of chronic obstructive pulmonary disease. J Natl Med Assoc. 2009 Jul;101(7):656–662. doi: 10.1016/s0027-9684(15)30974-3. [DOI] [PubMed] [Google Scholar]
- 16.Sarrazin MV, Campbell M, Rosenthal GE. Racial differences in hospital use after acute myocardial infarction: does residential segregation play a role? Health Aff (Millwood) 2009 Mar-Apr;28(2):w368–w378. doi: 10.1377/hlthaff.28.2.w368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Varkey AB, Manwell LB, Williams ES, et al. Separate and unequal: clinics where minority and nonminority patients receive primary care. Arch Intern Med. 2009 Feb 9;169(3):243–250. doi: 10.1001/archinternmed.2008.559. [DOI] [PubMed] [Google Scholar]
- 18.Keating NL, Kouri E, He Y, Weeks JC, Winer EP. Racial differences in definitive breast cancer therapy in older women: are they explained by the hospitals where patients undergo surgery? Med Care. 2009 Jul;47(7):765–773. doi: 10.1097/MLR.0b013e31819e1fe7. [DOI] [PubMed] [Google Scholar]
- 19.Bach PB, Pham HH, Schrag D, Tate RC, Hargraves JL. Primary care physicians who treat blacks and whites. N Engl J Med. 2004 Aug 5;351(6):575–584. doi: 10.1056/NEJMsa040609. [DOI] [PubMed] [Google Scholar]
- 20.Freedman R, He Y, Winer E, Keating N. Racial/Ethnic Differences in Receipt of Timely Adjuvant Therapy for Older Women with Breast Cancer: Are Delays Influenced by the Hospitals where Patients Obtain Surgical Care? Health Services Research. 2013 doi: 10.1111/1475-6773.12063. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schwartz LM, Woloshin S, Birkmeyer JD. How do elderly patients decide where to go for major surgery? Telephone interview survey. BMJ. 2005 Oct 8;331(7520):821. doi: 10.1136/bmj.38614.449016.DE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wilson CT, Woloshin S, Schwartz LM. Choosing where to have major surgery: who makes the decision? Arch Surg. 2007 Mar;142(3):242–246. doi: 10.1001/archsurg.142.3.242. [DOI] [PubMed] [Google Scholar]
- 23.Katz SJ, Hofer TP, Hawley S, et al. Patterns and correlates of patient referral to surgeons for treatment of breast cancer. J Clin Oncol. 2007 Jan 20;25(3):271–276. doi: 10.1200/JCO.2006.06.1846. [DOI] [PubMed] [Google Scholar]
- 24.Freedman RA, Kouri EM, West DW, Keating NL. Racial/Ethnic Disparities in Knowledge about One’s Breast Cancer Characteristics. Cancer. 2014 doi: 10.1002/cncr.28977. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ayanian JZ, Chrischilles EA, Fletcher RH, et al. Understanding cancer treatment and outcomes: the Cancer Care Outcomes Research and Surveillance Consortium. J Clin Oncol. 2004 Aug 1;22(15):2992–2996. doi: 10.1200/JCO.2004.06.020. [DOI] [PubMed] [Google Scholar]
- 26.Chew LD, Griffin JM, Partin MR, et al. Validation of screening questions for limited health literacy in a large VA outpatient population. J Gen Intern Med. 2008 May;23(5):561–566. doi: 10.1007/s11606-008-0520-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Katz JN, Chang LC, Sangha O, Fossel AH, Bates DW. Can comorbidity be measured by questionnaire rather than medical record review? Med Care. 1996 Jan;34(1):73–84. doi: 10.1097/00005650-199601000-00006. [DOI] [PubMed] [Google Scholar]
- 28.Marin G, Sabogal F, Vanoss Marin B, Otero-Sabogal F, Perez-Stable E. Development of a short acculturation scale for Hispanics. Hispanic Journal of Behavioral Sciences. 1987;9:183–205. [Google Scholar]
- 29.American Association for Public Opinion Research. Response rate: an overview. [Accessed October 2, 2014]; http://www.aapor.org/Response_Rates_An_Overview1/3720.htm#.VAXD503D-fA. [Google Scholar]
- 30.Little R. Direct standardization: a tool for teaching linear models for unbalanced data. Am Statistician. 1982;36:38–43. [Google Scholar]
- 31.Levinson W, Kao A, Kuby A, Thisted RA. Not all patients want to participate in decision making. A national study of public preferences. J Gen Intern Med. 2005 Jun;20(6):531–535. doi: 10.1111/j.1525-1497.2005.04101.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kaplan SH, Gandek B, Greenfield S, Rogers W, Ware JE. Patient and visit characteristics related to physicians' participatory decision-making style. Results from the Medical Outcomes Study. Med Care. 1995 Dec;33(12):1176–1187. doi: 10.1097/00005650-199512000-00002. [DOI] [PubMed] [Google Scholar]
- 33.Tortolero-Luna G, Byrd T, Groff JY, Linares AC, Mullen PD, Cantor SB. Relationship between English language use and preferences for involvement in medical care among Hispanic women. J Womens Health (Larchmt) 2006 Jul-Aug;15(6):774–785. doi: 10.1089/jwh.2006.15.774. [DOI] [PubMed] [Google Scholar]
- 34.Kinchen KS, Cooper LA, Levine D, Wang NY, Powe NR. Referral of patients to specialists: factors affecting choice of specialist by primary care physicians. Annals of family medicine. 2004 May-Jun;2(3):245–252. doi: 10.1370/afm.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Barnett ML, Keating NL, Christakis NA, O'Malley AJ, Landon BE. Reasons for choice of referral physician among primary care and specialist physicians. J Gen Intern Med. 2012 May;27(5):506–512. doi: 10.1007/s11606-011-1861-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mukamel DB, Weimer DL, Mushlin AI. Referrals to high-quality cardiac surgeons: patients' race and characteristics of their physicians. Health Serv Res. 2006 Aug;41(4 Pt 1):1276–1295. doi: 10.1111/j.1475-6773.2006.00535.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dimick J, Ruhter J, Sarrazin MV, Birkmeyer JD. Black patients more likely than whites to undergo surgery at low-quality hospitals in segregated regions. Health Aff (Millwood) 2013 Jun;32(6):1046–1053. doi: 10.1377/hlthaff.2011.1365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kaiser Permanente. Fast facts about Kaiser Permanente. [Accessed August 25, 2014]; http://share.kaiserpermanente.org/article/fast-facts-about-kaiser-permanente/ [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.