Abstract
Background
Women in many countries are advised to use folic acid supplements before and early during pregnancy to reduce the risk of neural tube defects in their infants. This study aimed to update the prevalence and to identify possible determinants of preconception folic acid supplement use in Italian women.
Methods
The study was based on cross-sectional data from seven maternity clinics located in six Italian regions from January to June, 2012. Data on maternal characteristics and supplement use were collected for 2,189 women using a self-administered questionnaire.
Results
Preconception folic acid use was reported by 23.5 % (n = 515) of the participants. Of these, 479 (93 %) women had taken folic acid supplements on a daily basis as recommended by the health authorities. Women who both had intended their pregnancy and had requested a preconception health visit to a doctor/gynecologist were substantially more likely than the reference group to initiate folic acid supplementation before their pregnancy (48.6 versus 4.8 %). Preconception folic acid use was also associated with higher maternal age, higher education, marriage/cohabitation, lower parity, infertility treatments, and chronic disease.
Conclusions
Data from seven maternity clinics located in six Italian regions indicate that preconception folic acid supplement use in many Italian women is low. Women who do not plan their pregnancy or do not request a preconception health visit to their doctor have among the lowest prevalence of preconception folic acid use. Improving folate status in these and other supplemental non-users may have important disease preventive effects.
Keywords: Folic acid, Italy, Neural tube defects, Predictors, Pregnancy, Supplementation
Background
Health authorities in many countries around the World recommend women of reproductive age to use folic acid supplements before and early in pregnancy to reduce the risk of having a baby with a neural tube defect [1–3]. The recommendations usually indicate a dose of 0.4 mg folic acid daily from at least one month before pregnancy until the third month of gestation. In addition to such recommendations, a number of countries have also introduced mandatory food fortification of grains with folic acid to increase intake of this B-vitamin in fertile women. In these countries, a risk reduction of neural tube defect has been reported [4–7].
Mandatory food fortification with folic acid has not yet been introduced in any European country [3, 8]. Enhanced sources of folate are only available from folic acid supplements, voluntary fortification, and intake of foods rich in folates, such as vegetables and fruits. Although the prevalence of preconception folic acid supplementation in Europe has increased after many years of delivered recommendations, a large portion of women still does not follow the recommendations and many start supplementation to late with respect to neural tube defect prevention [9]. Additionally, the total prevalence of neural tube defects in Europe has not declined markedly over the years [3, 10, 11]. This has led to a debate regarding the efficiency of folic acid recommendations in Europe and other countries [12, 13].
In order to identify groups of women who do not follow the recommendations, many researchers have explored the possible determinants of use or non-use of folic acid supplements. Typically, pregnancy intention, preconception health visit to a doctor, and higher educational level are strong correlates for taking folic acid supplements [14–18], while higher parity, shorter and longer interpregnancy intervals, maternal smoking before pregnancy, and lower maternal age are often associated with less use [15–19]. Such information is valuable and can be used to design intervention programs to improve the preconception folic acid supplement use overall and in subgroups of women related to low use.
In Italy, the official recommendations from April 2004 state that all women planning a pregnancy and those who do not actively exclude the possibility of becoming pregnant should take a daily folic acid supplement of at least 0.4 mg from one month before conception and continue throughout the first trimester [20, 21]. With a prescription from a doctor, this dose or higher is free of charge in Italy since 2005 [22]. Since the folic acid recommendations were issued in 2004, information on the determinants of supplement use in Italian women is limited [14, 23, 24]. This study, therefore, aimed to update the Italian prevalence and to identify possible determinants of preconception folic acid supplement use in Italian women using data from a recent Italian multicenter survey on preconception health.
Methods
Study population
The current study drew on resources of a multicenter study initially established to examine the prevalence and the determinants of a variety of preconception risk factors (including preconception folic acid supplement use) in Italian women [25]. It was conducted between January and June, 2012, in seven maternity clinics located in six different regions: Castelli Hospital (Verbania, Piemonte), Vaio Hospital (Fidenza, Emilia-Romagna), Galliera Hospital (Genova, Liguria), Santa Chiara Hospital (Pisa, Toscana), S. Giovanni Calibita Fatebenefratelli Hospital, and Santo Spirito Hospital (Roma, Lazio), Rummo Hospital (Benevento, Campania). The study was approved by the ethical committee of the S. Giovanni Calibita Fatebenefratelli Hospital (parere 55/2011).
The data collection of the present study has been described elsewhere [25]. All women eligible for the study were invited to fill in a self-administered questionnaire comprising 35 initial questions on various topics, including vitamin supplement use, pregnancy-related risk factors, and maternal background characteristics. Personal information such as names, address, or birth date was not recorded. In Verbania (n = 320), women were recruited during pregnancy (usually at their first prenatal visits), while in the other six maternity clinics (n = 1,892) mothers were recruited during hospitalization after giving birth [25]. Mothers of newborns with any congenital malformation or low birth weight (<2,500 g), with children who were delivered preterm (<37 weeks gestation), or mothers with children admitted to the neonatal intensive care unit were initially not invited to participate to avoid subjecting them to unnecessary stress. Also, women not speaking Italian were excluded from the study.
The distribution of the 2,212 participants at the seven participating maternity clinics was as follows: Verbania (14.5 %), Genova (17.8 %), Fidenza (9.9 %), Pisa (9.1 %), Roma Fatebenefratelli (23.1 %), Roma Santo Spirito (10.8 %), and Benevento (14.7 %) [25]. Of the 2,212 participating women, we excluded 23 women who did not have information of folic acid supplement use (n = 5) or did not provide information on the time period of use (n = 18), leaving back 2,189 women for analyzes.
Folic acid supplement use
The women were asked to report data on supplemental use of folic acid and other vitamins by specifying the brand name, the frequency of use, as well as the time period of use. In this study, we defined folic acid supplement use as any use of supplements containing folic acid for at least once a week during the following predefined time periods: (a) at least one month before the last menstrual period to the end of the first trimester, (b) at least six months before the last menstrual period to the end of the first trimester, (c) soon after pregnancy confirmation to the end of the first trimester, (d) after the first trimester of pregnancy, or (e) no use at all. The main outcome variable under study was preconception folic acid supplement use, i.e., any use of folic acid supplements that had started before the last menstrual period (category (a) and (b) above). Note that our definition of preconception folic acid use differs somewhat from the official recommendations by allowing for a more moderate use as well, i.e., less than seven days a week.
Potential determinants
Based on the questionnaire, we abstracted data on the following relevant determinants of folic acid supplement use: maternal age at study recruitment (Verbania) or delivery (other regions), parity, maternal education, marital status, national citizenship, working activity, pregnancy intention, preconception health visit, infertility treatment, maternal smoking, prepregnancy body mass index (kg/m2), and chronic diseases. The pregnancy was classified as intended, mistimed or unintended on the basis of a score of the intensity of pregnancy planning effort developed by Morin et al. [26] The following categories were used: intended (score 9–12), mistimed (score 4–8) and unintended (score: 0–3). The preconception health visit was defined as any visit to a doctor/gynecologist within the last year before the onset of pregnancy to ask for any advice on the possible near future pregnancy, such as medical examinations to perform, medications and vitamins to take. Body mass index before pregnancy was categorized into four groups according to the criteria by the World Health Organization: underweight (<18.50 kg/m2), normal weight (18.50–24.99 kg/m2), pre-obese (25.00–29.99 kg/m2), obese (≥30.00 kg/m2). Parity was defined as the number of previous live births and stillbirths while maternal smoking was defined as any smoking around the time of the last menstrual period. Chronic diseases included diabetes, epilepsy, asthma, and hypertension.
Statistical analysis
Statistical analyzes were performed by using SAS (Statistical Analysis System) version 9.2 (SAS Institute, Inc., Cary, North Carolina) for Windows. Data were described as percentages or means with interquartile ranges (IQRs). The chi-square test was used to test for group difference in categorical variables. All P values were two-sided and values <0.05 were considered statistically significant. Associations of preconception folic acid use with the various maternal characteristics were estimated by prevalence ratios with 95 % confidence intervals (CIs) using log-binomial regression models with the log-link function. All prevalence ratios were estimated by crude models, as well as after adjustment for maternal age, parity, maternal education, marital status, national citizenship (here: Italian), pregnancy intention, preconception health visit, infertility treatment, and maternal smoking before pregnancy. All covariates have previously been strongly related to maternal folic acid supplement use. Additionally, the correlation between binary outcomes within the same maternity clinic was taken into account by using generalized estimating equations methodology, assuming an exchangeable working correlation structure. Women with missing data on covariates were excluded in multiple regression analyzes.
Results
Of the 2,189 participating women, the mean maternal age was 33 (IQR: 29–37; range 13–50) years; only 6 % were younger than 25 years while 40 % were older than 35 years (Table 1). We further estimated that 64 % of the women had intended their pregnancy and that 30 % had mistimed their pregnancy. Overall, 41 % of the women reported that they had requested a preconception health visit to a doctor/gynecologist whereas 7 % had reported that they had used an infertility treatment. Reported smoking prevalence before the onset of pregnancy was as high as 26 %.
Table 1.
Characteristics of the study sample
| Characteristic | No. of womena | ||
|---|---|---|---|
| n | % | ||
| Maternal age (years) | |||
| <25 | 130 | 5.9 | |
| 25–29 | 404 | 18.5 | |
| 30–34 | 724 | 33.1 | |
| 35–39 | 660 | 30.2 | |
| 40 or more | 209 | 9.5 | |
| Parity | |||
| 0 | 1,246 | 56.9 | |
| 1 | 730 | 33.3 | |
| 2 | 171 | 7.8 | |
| 3 or more | 42 | 1.9 | |
| Educational level | |||
| Primary school | 331 | 15.1 | |
| Secondary school | 960 | 43.9 | |
| University | 890 | 40.7 | |
| Marital status | |||
| No partner | 213 | 9.7 | |
| Married/cohabiting | 1,957 | 89.4 | |
| Citizenship | |||
| Non-Italian | 319 | 14.6 | |
| Italian | 1,867 | 85.3 | |
| Working activity | |||
| Studying | 106 | 4.8 | |
| Working | 1,683 | 76.9 | |
| Working at home | 283 | 12.9 | |
| Not working | 94 | 4.3 | |
| Pregnancy intention | |||
| Unintended | 121 | 5.5 | |
| Mistimed | 646 | 29.5 | |
| Intended | 1,392 | 63.6 | |
| Preconception health visit | |||
| No | 1,266 | 57.8 | |
| Yes | 907 | 41.4 | |
| Infertility treatment | |||
| No | 2,001 | 91.4 | |
| Ovulation inductor use, no ART | 31 | 1.4 | |
| ART | 128 | 5.8 | |
| Maternal smoking before pregnancy | |||
| No | 1,614 | 73.7 | |
| Yes | 575 | 26.3 | |
| BMI before pregnancy | |||
| Underweight | 180 | 8.2 | |
| Normal weight | 1,573 | 71.9 | |
| Pre-obese | 303 | 13.8 | |
| Obese | 122 | 5.6 | |
| Chronic disease | |||
| No | 1,959 | 89.5 | |
| Yes | 208 | 9.5 | |
Abbreviation: ART assisted reproductive technology, BMI body mass index
aPercentages do not add to 2,189 and 100 % due to missing data: 62 women on maternal age, 8 women on educational level, 19 women on marital status, 3 women on citizenship, 23 women on working activity, 30 women on pregnancy intention, 16 women on preconception health visit, 29 women on infertility treatment, 11 women on body mass index before pregnancy, and 22 women with chronic disease
Overall, 84 % (n = 1,838) of the participating women had taken folic acid supplements at some time point before and/or during pregnancy while only 23.5 % (n = 515) of the participants had reported the use of folic acid supplements before the onset of pregnancy. Specifically, 11.7 % (n = 256) of all women had initiated use, at least, one month before pregnancy, 11.8 % (n = 259) had initiated use, at least, six months before pregnancy, 54.9 % (n = 1201) had initiated after pregnancy confirmation during the first trimester, and 5.6 % (n = 122) reported starting folic acid use after the first trimester of pregnancy (Fig. 1).
Fig. 1.
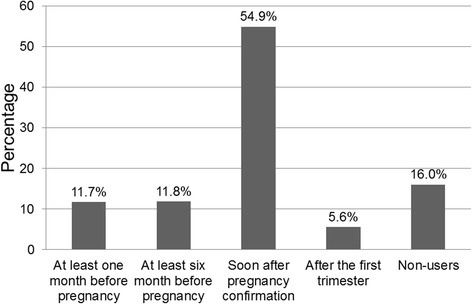
The prevalence of folic acid supplement users according to time periods of use (n = 2,189). Time periods of use were defined as at least one month before the last menstrual period to the end of the first trimester, at least six months before the last menstrual period to the end of the first trimester, soon after pregnancy confirmation to the end of the first trimester, after the first trimester of pregnancy, or no use at all
For all subgroups of women, intake of folic acid use was low during the preconception period and highest after pregnancy confirmation (Table 2). In particular, the initiation of supplement use in women younger than 25 years of age was only 5.4 % before pregnancy and 63 % soon after pregnancy confirmation.
Table 2.
Prevalence of folic acid supplement users according to maternal characteristics and time periods of usea
| Characteristic | No. of women | Folic acid supplement users, %b | ||||
|---|---|---|---|---|---|---|
| At least one month before pregnancy (n = 256) | At least six months before pregnancy (n = 259) | Soon after pregnancy confirmation (n = 1,201) | After the first trimester (n = 122) | |||
| Maternal age (years) | ||||||
| <25 | 130 | 5.4 | 0 | 63.1 | 7.7 | |
| 25–29 | 404 | 11.4 | 7.4 | 58.7 | 4.7 | |
| 30–34 | 724 | 13.5 | 10.9 | 54.4 | 6.2 | |
| 35–39 | 660 | 12.3 | 15.8 | 51.1 | 5.2 | |
| 40 or more | 209 | 10.5 | 19.1 | 53.1 | 4.8 | |
| Parity | ||||||
| 0 | 1,246 | 12.4 | 14.4 | 52.8 | 4.5 | |
| 1 | 730 | 11.6 | 8.6 | 58.8 | 6.4 | |
| 2 | 171 | 8.2 | 8.8 | 55.0 | 9.4 | |
| 3 or more | 42 | 4.8 | 2.4 | 47.6 | 7.1 | |
| Educational level | ||||||
| Primary school | 331 | 3.9 | 5.4 | 53.5 | 8.2 | |
| Secondary school | 960 | 11.3 | 10.2 | 56.3 | 6.9 | |
| University | 890 | 15.1 | 16.1 | 54.2 | 3.3 | |
| Marital status | ||||||
| No partner | 213 | 5.6 | 6.6 | 62.9 | 7.5 | |
| Married/cohabiting | 1,957 | 12.3 | 12.5 | 54.2 | 5.4 | |
| Citizenship | ||||||
| Non-Italian | 319 | 8.2 | 6.0 | 53.0 | 10.0 | |
| Italian | 1,867 | 12.3 | 12.9 | 55.2 | 4.8 | |
| Working activity | ||||||
| Studying | 106 | 10.4 | 7.5 | 61.3 | 5.7 | |
| Working | 1,683 | 12.4 | 12.7 | 55.0 | 5.4 | |
| Working at home | 283 | 8.5 | 8.8 | 53.7 | 6.0 | |
| Not working | 94 | 10.6 | 13.8 | 50.0 | 7.4 | |
| Pregnancy intention | ||||||
| Unintended | 121 | 4.1 | 2.5 | 57.0 | 9.1 | |
| Mistimed | 646 | 4.3 | 4.0 | 62.4 | 7.3 | |
| Intended | 1,392 | 15.8 | 16.4 | 51.1 | 4.4 | |
| Preconception health visit | ||||||
| No | 1,266 | 5.1 | 5.0 | 63.6 | 6.8 | |
| Yes | 907 | 21.2 | 21.6 | 42.9 | 3.9 | |
| Infertility treatment | ||||||
| No | 2,001 | 11.0 | 9.9 | 57.0 | 5.5 | |
| Ovulation inductor use, no ART | 31 | 6.5 | 41.9 | 32.3 | 12.9 | |
| ART | 128 | 22.7 | 35.2 | 30.5 | 2.3 | |
| Maternal smoking before pregnancy | ||||||
| No | 1,614 | 12.5 | 13.1 | 53.5 | 5.4 | |
| Yes | 575 | 9.4 | 8.3 | 58.6 | 6.1 | |
| BMI before pregnancy | ||||||
| Underweight | 180 | 11.1 | 12.2 | 53.9 | 6.1 | |
| Normal weight | 1,573 | 12.4 | 12.3 | 54.2 | 5.6 | |
| Pre-obese | 303 | 11.2 | 9.9 | 59.4 | 4.3 | |
| Obese | 122 | 5.7 | 9.8 | 54.9 | 6.6 | |
| Chronic disease | ||||||
| No | 1,959 | 11.2 | 11.0 | 55.4 | 5.8 | |
| Yes | 208 | 14.4 | 19.7 | 50.0 | 3.8 | |
Abbreviation: ART assisted reproductive technology, BMI body mass index
aTime periods were defined as (a) at least one month before the last menstrual period to the end of the first trimester, (b) at least six months before the last menstrual period to the end of the first trimester, (c) soon after pregnancy confirmation to the end of the first trimester, (d) after the first trimester of pregnancy, or (e) no use at all
bPercentage of “no use at all” not shown in the table
Preconception folic acid use was reported by 23.5 % (n = 515) of the participants. Of these, 479 (93 %) women had taken folic acid supplements on a daily basis as recommended by the health authorities, 25 (4.9 %) women had taken the supplements 4–6 times a week while 6 (1.2 %) women had taken them 1–3 times a week. Five women (0.9%) did not report the frequency of use.
Unadjusted and adjusted regression analyses showed that age over 25 years, being pregnant for the first time, having a university degree/secondary school, being married/cohabiting, intending the pregnancy, requesting preconception health visit to a doctor/gynecologist, using infertility treatments, and having chronic diseases were all statistically significant determinants of preconception folic acid use (Table 3). Italian citizenship, ovulation inductor use, and non-smoking before pregnancy were not significant determinants after adjustment for covariates. Working status and body mass index before pregnancy were insignificant determinants both before and after covariate adjustments (Table 3).
Table 3.
Prevalence and association of preconception folic acid supplement according to reported maternal characteristics
| Characteristic | No. of women | No. of supplement usersa | Crudeb | Adjustedc | ||||
|---|---|---|---|---|---|---|---|---|
| Prevalence ratio | 95 % confidence interval | Prevalence ratio | 95 % confidence interval | |||||
| N | n | % | ||||||
| Maternal age (years) | ||||||||
| <25d | 130 | 7 | 5.4 | 0.23 | 0.07, 0.80 | 0.31 | 0.12, 0.80 | |
| 25–29 | 404 | 76 | 18.8 | 0.78 | 0.60, 1.01 | 0.94 | 0.79, 1.11 | |
| 30–34 | 724 | 177 | 24.4 | 1 | 1 | |||
| 35–39 | 660 | 185 | 28.0 | 1.13 | 1.03, 1.23 | 1.05 | 0.96, 1.15 | |
| 40 or more | 209 | 62 | 29.7 | 1.18 | 1.03, 1.36 | 0.98 | 0.85, 1.14 | |
| Parity | ||||||||
| 0d | 1,246 | 335 | 26.9 | 1 | 1 | |||
| 1 | 730 | 148 | 20.3 | 0.74 | 0.63, 0.86 | 0.86 | 0.77, 0.95 | |
| 2 | 171 | 29 | 17.0 | 0.65 | 0.56, 0.76 | 0.82 | 0.57, 1.18 | |
| 3 or more | 42 | 3 | 7.1 | 0.24 | 0.08, 0.72 | 0.66 | 0.29, 1.51 | |
| Educational level | ||||||||
| Primary schoold | 331 | 31 | 9.4 | 1 | 1 | |||
| Secondary school | 960 | 206 | 21.5 | 1.99 | 1.73, 2.29 | 1.69 | 1.46, 1.95 | |
| University | 890 | 277 | 31.1 | 2.80 | 2.41, 3.26 | 1.90 | 1.62, 2.22 | |
| Marital status | ||||||||
| No partnerd | 213 | 26 | 12.2 | 1 | 1 | |||
| Married/cohabiting | 1,957 | 485 | 24.8 | 2.26 | 1.86, 2.75 | 1.44 | 1.21, 1.72 | |
| Citizenship | ||||||||
| Non-Italiand | 319 | 45 | 14.1 | 1 | ||||
| Italian | 1,867 | 470 | 25.2 | 2.32 | 1.21, 4.42 | 1.40 | 0.99, 1.97 | |
| Working activity | ||||||||
| Studyingd | 106 | 19 | 17.9 | 1 | 1 | |||
| Working | 1,683 | 422 | 25.1 | 1.47 | 0.89, 2.42 | 1.00 | 0.73, 1.36 | |
| Working at home | 283 | 49 | 17.3 | 1.15 | 0.68, 1.96 | 1.10 | 0.77, 1.58 | |
| Not working | 94 | 23 | 24.5 | 1.49 | 0.73, 3.06 | 1.31 | 0.88, 1.97 | |
| Pregnancy intention | ||||||||
| Unintendedd | 121 | 8 | 6.6 | 1 | 1 | |||
| Mistimed | 646 | 54 | 8.4 | 1.34 | 0.79, 2.28 | 1.02 | 0.61, 1.70 | |
| Intended | 1,392 | 448 | 32.2 | 4.87 | 2.51, 9.43 | 2.40 | 1.14, 5.05 | |
| Preconception health visit | ||||||||
| Nod | 1,266 | 127 | 10.0 | 1 | 1 | |||
| Yes | 907 | 388 | 42.8 | 4.21 | 3.09, 5.72 | 2.90 | 2.21, 3.82 | |
| Infertility treatment | ||||||||
| Nod | 2,001 | 418 | 20.9 | 1 | 1 | |||
| Ovulation inductor use, no ART | 31 | 15 | 48.4 | 2.11 | 1.35, 3.29 | 1.00 | 0.62, 1.60 | |
| ART | 128 | 74 | 57.8 | 2.75 | 2.08, 3.64 | 1.35 | 1.08, 1.68 | |
| Maternal smoking before pregnancy | ||||||||
| Nod | 1,614 | 413 | 25.6 | 1 | 1 | |||
| Yes | 575 | 102 | 17.7 | 0.70 | 0.59, 0.82 | 0.92 | 0.79, 1.07 | |
| BMI before pregnancy | ||||||||
| Underweightd | 180 | 42 | 23.3 | 1 | 1 | |||
| Normal weight | 1,573 | 389 | 24.7 | 1.11 | 0.89, 1.38 | 0.97 | 0.75, 1.25 | |
| Pre-obese | 303 | 64 | 21.1 | 1.01 | 0.81, 1.27 | 0.97 | 0.75, 1.26 | |
| Obese | 122 | 19 | 15.6 | 0.77 | 0.53, 1.11 | 0.84 | 0.54, 1.31 | |
| Chronic disease | ||||||||
| Nod | 1,959 | 436 | 22.3 | 1 | 1 | |||
| Yes | 208 | 71 | 34.1 | 1.47 | 1.17, 1.85 | 1.22 | 1.09, 1.37 | |
Abbreviation: ART assisted reproductive technology, BMI body mass index
aAny supplement use that started before the last menstrual period
bCrude prevalence ratio was estimated by log-binomial regression models
cAdjusted for maternal age, parity, maternal education, marital status, Italian citizenship, pregnancy intention, preconception health visit, infertility treatment, and maternal smoking before pregnancy
dReference category
Of the 515 women who had initiated use of folic acid-containing supplements before the onset of pregnancy, we had exact folic acid dose information on 506 women (98.2 %). Of these, 71.5 % had taken the usual dose of 0.4 mg, 20.9 % had taken 0.4 mg to 5.0 mg while 7.5 % had taken more than 5.0 mg (Fig. 2).
Fig. 2.
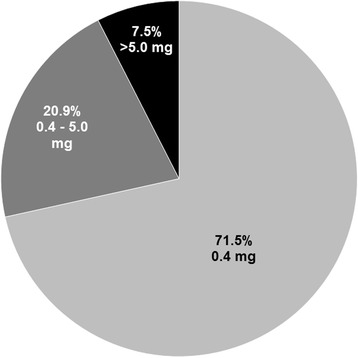
The distribution of reported folic acid dose (mg) among preconception supplement users (n = 515). Preconception folic acid supplement use was defined as any use of folic acid supplements that had started before the last menstrual period
One-third of the women (n = 712) reported that they had both intended their pregnancy and had requested a preconception health visit to a doctor/gynecologist (Table 4). These women were eight times more likely to start folic acid supplementation before pregnancy compared with those who did not intend and did not request a preconception health visit (48.6 versus 4.8 %; adjusted prevalence ratio = 7.90 [95 % CI: 4.62, 13.5]).
Table 4.
Prevalence and association of preconception folic acid supplement use according to status of preconception health visit to a doctor/gynecologist and status of pregnancy intention
| Preconception health visit | Pregnancy intentiona | No. of womenb | No. of supplement usersc | Cruded | Adjustede | |||
|---|---|---|---|---|---|---|---|---|
| Prevalence ratio | 95 % confidence interval | Prevalence ratio | 95 % confidence interval | |||||
| n | n | % | ||||||
| Nof | Nof | 584 | 28 | 4.8 | 1.00 | 1.00 | ||
| No | Yes | 659 | 97 | 14.7 | 2.98 | 1.93, 4.61 | 2.87 | 1.72, 4.79 |
| Yes | No | 188 | 39 | 20.7 | 4.35 | 2.33, 8.12 | 4.08 | 2.29, 7.28 |
| Yes | Yes | 712 | 346 | 48.6 | 9.69 | 5.68, 16.5 | 7.90 | 4.62, 13.5 |
aStatus of pregnancy intention was defined as intended (yes) and unintended/mistimed (no)
bData were missing for 30 women on pregnancy intention and 16 women on preconception health visit
cAny supplement use that started before the last menstrual period
dCrude prevalence ratio was estimated by log-binomial regression models
eAdjusted for maternal age, parity, maternal education, marital status, Italian citizenship, infertility treatment, and maternal smoking before pregnancy
fReference category
Of 188 pregnancies that were not planned but in which the mother had consulted a doctor/gynecologists on preconception health advice (Table 4), 92 % (173/188) were classified as mistimed. The prevalence of folic acid supplement use in these 173 mistimed pregnancies was 21.4 % (not shown).
Finally, the estimated prevalence of preconception folic acid supplement use in the specific group of resourceful women (those who aged over 25 years, had a university degree, were married/cohabiting, had Italian citizenship, intended their pregnancy, requested a preconception visit) was 58.0 % [95 % CI: 52 %, 64 %], which was twice as high as the preconception prevalence of 23.5 % estimated for the total population.
Discussion
Our study showed that 84 % of women had taken folic acid supplements at some time point before and/or during the pregnancy but that only 23.5 % of the participants had initiated use before the onset of pregnancy. In general, the percentage of initiation of folic acid supplement use was low before the onset of pregnancy and highest soon after pregnancy confirmation. This pattern was seen in all subgroups of women and suggests that the majority of women acquire folic acid information firstly after the onset of pregnancy. The most important determinants of folic acid use before the onset of pregnancy were preconception health visit to a doctor and pregnancy intention.
This is among the largest studies to examine the prevalence and determinants of maternal preconception folic acid supplement use in Italy. Strengths of the study include the detailed data on frequency, dose, and timing of folic acid supplement use, the analysis of a large number of maternal characteristics as determinants of supplement use, and the multicenter design in which data were collected through seven maternity clinics from six regions in Italy (three in the north, three in the center, and one in the south). However, our study sample may not be representative of all women giving birth in Italy. Women who did not comprehend the Italian language, those who delivered before 37 weeks of gestation or had an infant with birth weight below 2,500 g were not invited to participate. In addition, mothers with the lowest educational level may have been underrepresented in our study [27]. As these factors have been related to low use, our study might have overestimated the prevalence of preconception folic acid supplement use. Our prevalence estimate is still close to that reported in a previous study, which was 25.4 % in Italians [23].
Our findings on determinants of preconception folic acid use are generally consistent with those found in numerous other studies. Higher maternal age, having higher education, being married/cohabiting, having lower parity, using infertility treatments, and having a chronic disease have all been identified as statistically significant determinants of preconception folic acid use in previous studies [15–19]. In contrast to some findings, we did not identify national citizenship [17] and maternal smoking before pregnancy [15, 16] as significant independent factors after adjusting for covariates. Also, the association of ovulation inductor use was substantially attenuated after covariate adjustments, particularly after adjustment of preconception health visit and pregnancy intention (not shown). Consistent with two other large studies [15, 16], prepregnancy body mass index was not important determinants of preconception folic acid use in our study, neither was working status.
We identified preconception health visit to a doctor/gynecologist and pregnancy intention as the most important determinants of preconception folic acid supplement use. Obviously, women who intend their pregnancy or seek preconception advice from their doctor before pregnancy may be more informed on the benefits and timing of folic acid. Still, only 48.6 % (346/712) of all those who had requested preconception health visit and also had intended their pregnancy were using folic acid before pregnancy (see Table 4). An explanation for the low proportion of preconception folic acid users in this highly motivated group may be that recommendations on folic acid supplement use were not sufficiently provided to women by their doctors or that, in spite of sufficient information, women forgot or choose not to follow the doctor’s advice. These and other specific reasons for not taking folic acid supplements despite pregnancy planning and preconception health visits should be further investigated in studies to gain new insight on how to improve supplement use in these women [14].
As many as 27 % (584/2,189) women did not intend their pregnancy and did not request a preconception health visit (see Table 4). Of these, only 5 % (28/584) used folic acid-containing supplements before the onset of pregnancy. Clearly, information on the benefits of folic acid had not reached out to this large group of women, questioning the efficiency of the official recommendations to fertile women. To improve folate status in fertile women and particularly in women with unintended pregnancies, many countries, including the United States and Canada, have decided to fortify their foods with folic acid. In these countries, a risk reduction of neural tube defects has been reported [4–7]. Many countries refrain mandatory folic acid fortification, partly because of the risk of masking anemia related to a B12 deficiency in the elderly and partly because of unknown cancer risks in the non-pregnant population [9]. Recent results, however, show that folic acid in fortified foods and supplements does not interfere with vitamin B12 metabolism at the cellular level in a healthy population [28]. Additionally, a recent meta-analysis showed no significant risk (reduced or increased) of overall or site-specific cancers in nearly 50,000 individuals from 13 different randomized clinical trials of folic acid supplement use [29]. Given that Italy does not fortify food with folic acid and as many as 36 % mothers do not plan their pregnancy [25], new effective strategies for increasing supplement use in these pregnancies are strongly needed.
Of 188 pregnancies that were not planned but in which the mother had consulted a doctor/gynecologists on preconception health advice (see Table 4), 92 % (173/188) were classified as mistimed. This suggests that many women seeking preconception health advice had not necessarily decided to become pregnant at the time of the visit, but were open to the possibility of becoming pregnant in the near future. The prevalence of folic acid supplement use in these women was only 21.4 % and might be substantially improved by more direct measures by their doctors.
Folates occur naturally in foods, predominantly in green leafy vegetables, fruits, and cereal products. Although the typical Mediterranean diet constitutes a large portion of vegetables and fruits rich in folate it is uncertain whether this contributes to improved blood folate levels in Italian fertile women. In the European Prospective Investigation into Cancer and Nutrition cohort, women in South Europe, including Italy, appeared to have higher plasma folate concentrations than those in the northern, but not in the more central regions of Europe [30]. Furthermore, in a recent Italian study excluding vitamin B supplement users [31], only a small portion of women in childbearing age reached adequate levels of serum folate and red blood cell folate according to estimated thresholds for neural tube defect prevention [31, 32]. In light of this, supplementation with folic acid appears to be an important aspect also in countries with Mediterranean diets.
Conclusions
In conclusion, like many women in other countries, many Italian women start folic acid supplement use too late with respect to neural tube defect prevention. Particularly, women who do not plan their pregnancy and do not request a preconception health visit to the doctor before the pregnancy have among the lowest prevalence of preconception folic acid use. Increased folic acid promotion during preconception health visits combined with an even higher rate of both planned pregnancies and preconception health visits might help improve supplement use in Italian women. Alternatively, mandatory food fortification with folic acid might be an option for improving folate status, but more information on the overall intake of folate from foods and supplements in Italy is needed before considering such interventions.
Abbreviations
ART, assisted reproductive technologyl; BMI, body mass index; CI, confidence interval; IQR, interquartile range
Acknowledgements
This paper has been prepared in the framework of the project “Prevenire patologie e disabilità congenite attraverso strategie di comunicazione efficaci”, CODICE CUP: I85J12001480001 funded by CCM of the Italian Ministry of Health.
Funding
This study has no funding.
Availability of data and materials
Given that we are presently preparing other manuscripts involving preconception risk factors in this study sample, we elected to not share the raw data from this manuscript.
Authors’ contributions
PM and EL have made substantial contributions to conception, design, and planning of the study; RMN and PM made substantial contributions to drafting the first version of the manuscript and revising the manuscript critically for important intellectual content; EL and RMN have made substantial contribution to data management, statistical analysis and interpretation of data; PG, VA, RA, FF, FF, EF, PG, and GS provided data to the study and made their contribution in drafting and revising the manuscript. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Contributor Information
Roy M. Nilsen, Phone: (+47) 55 97 60 88, Email: roy.nilsen@uib.no
Emanuele Leoncini, Email: ema.leoncini@gmail.com.
Paolo Gastaldi, Email: paolo.gastaldi@asl-rme.it.
Valentina Allegri, Email: v.allegri@inwind.it.
Rocco Agostino, Email: rocco.agostino@uniroma1.it.
Francesca Faravelli, Email: Francesca.Faravelli@gosh.nhs.uk.
Federica Ferrazzoli, Email: federicaferra@hotmail.com.
Enrico Finale, Email: enrico.finale@gmail.com.
Paolo Ghirri, Email: pghirri@med.unipi.it.
Gioacchino Scarano, Email: gioacchino.scarano@ao-rummo.it.
Pierpaolo Mastroiacovo, Email: mk4340@mclink.it.
References
- 1.Recommendations for the use of folic acid to reduce the number of cases of spina bifida and other neural tube defects. MMWR Recomm Rep. 1992;41(No. RR.14). [PubMed]
- 2.De Wals P, Rusen ID, Lee NS, Morin P, Niyonsenga T. Trend in prevalence of neural tube defects in Quebec. Birth Defects Res A Clin Mol Teratol. 2003;67:919–23. doi: 10.1002/bdra.10124. [DOI] [PubMed] [Google Scholar]
- 3.EUROCAT . Special Report: Prevention of Neural Tube Defects by Periconceptional Folic Acid Supplementation in Europe (Updated version December 2009) 2009. [Google Scholar]
- 4.Honein MA, Paulozzi LJ, Mathews TJ, Erickson JD, Wong LY. Impact of folic acid fortification of the US food supply on the occurrence of neural tube defects. JAMA. 2001;285:2981–6. doi: 10.1001/jama.285.23.2981. [DOI] [PubMed] [Google Scholar]
- 5.Lopez-Camelo JS, Orioli IM, da Graca Dutra M, Nazer-Herrera J, Rivera N, Ojeda ME, et al. Reduction of birth prevalence rates of neural tube defects after folic acid fortification in Chile. Am J Med Genet A. 2005;135:120–5. doi: 10.1002/ajmg.a.30651. [DOI] [PubMed] [Google Scholar]
- 6.De Wals P, Tairou F, Van Allen MI, Uh SH, Lowry RB, Sibbald B, et al. Reduction in neural-tube defects after folic acid fortification in Canada. N Engl J Med. 2007;357:135–42. doi: 10.1056/NEJMoa067103. [DOI] [PubMed] [Google Scholar]
- 7.Williams J, Mai CT, Mulinare J, Isenburg J, Flood TJ, Ethen M, et al. Updated estimates of neural tube defects prevented by mandatory folic Acid fortification - United States, 1995–2011. MMWR Morb Mortal Wkly Rep. 2015;64:1–5. [PMC free article] [PubMed] [Google Scholar]
- 8.EFSA . ESCO report prepared by the EFSA. Scientific Cooperation Working Group on Analysis of Risks and Benefits of Fortification of Food with Folic Acid. 2009. [Google Scholar]
- 9.Eichholzer M, Tonz O, Zimmermann R. Folic acid: a public-health challenge. Lancet. 2006;367:1352–61. doi: 10.1016/S0140-6736(06)68582-6. [DOI] [PubMed] [Google Scholar]
- 10.Botto LD, Lisi A, Robert-Gnansia E, Erickson JD, Vollset SE, Mastroiacovo P, et al. International retrospective cohort study of neural tube defects in relation to folic acid recommendations: are the recommendations working? BMJ. 2005;330:330–571. doi: 10.1136/bmj.38336.664352.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Khoshnood B, Loane M, de Walle H, Arriola L, Addor MC, Barisic I, et al. Long term trends in prevalence of neural tube defects in Europe: population based study. BMJ. 2015 doi: 10.1136/bmj.h5949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Botto LD, Lisi A, Bower C, Canfield MA, Dattani N, De Vigan C, et al. Trends of selected malformations in relation to folic acid recommendations and fortification: an international assessment. Birth Defects Res A Clin Mol Teratol. 2006;76:693–705. doi: 10.1002/bdra.20307. [DOI] [PubMed] [Google Scholar]
- 13.Bestwick JP, Huttly WJ, Morris JK, Wald NJ. Prevention of neural tube defects: a cross-sectional study of the uptake of folic acid supplementation in nearly half a million women. PLoS One. 2014 doi: 10.1371/journal.pone.0089354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.De Santis M, Quattrocchi T, Mappa I, Spagnuolo T, Licameli A, Chiaradia G, et al. Folic acid use in planned pregnancy: an Italian survey. Matern Child Health J. 2013;17:661–6. doi: 10.1007/s10995-012-1047-2. [DOI] [PubMed] [Google Scholar]
- 15.Nilsen RM, Vollset SE, Gjessing HK, Magnus P, Meltzer HM, Haugen M, et al. Patterns and predictors of folic acid supplement use among pregnant women: the Norwegian Mother and Child Cohort Study. Am J Clin Nutr. 2006;84:1134–41. doi: 10.1093/ajcn/84.5.1134. [DOI] [PubMed] [Google Scholar]
- 16.Timmermans S, Jaddoe VW, Mackenbach JP, Hofman A, Steegers-Theunissen RP, Steegers EA. Determinants of folic acid use in early pregnancy in a multi-ethnic urban population in The Netherlands: the Generation R study. Prev Med. 2008;47:427–32. doi: 10.1016/j.ypmed.2008.06.014. [DOI] [PubMed] [Google Scholar]
- 17.Tort J, Lelong N, Prunet C, Khoshnood B, Blondel B. Maternal and health care determinants of preconceptional use of folic acid supplementation in France: results from the 2010 National Perinatal Survey. BJOG. 2013;120:1661–7. doi: 10.1111/1471-0528.12414. [DOI] [PubMed] [Google Scholar]
- 18.Nelson CR, Leon JA, Evans J. The relationship between awareness and supplementation: which Canadian women know about folic acid and how does that translate into use? Can J Public Health. 2014;105:e40–6. doi: 10.17269/cjph.105.4155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nilsen RM, Mastroiacovo P, Gunnes N, Alsaker ER, Bjorke-Monsen AL, Eussen SJ, et al. Folic acid supplementation and interpregnancy interval. Paediatr Perinat Epidemiol. 2014;28:270–4. doi: 10.1111/ppe.12111. [DOI] [PubMed] [Google Scholar]
- 20.Network Italiano Promozione Acido Folico per la Prevenzione Primaria di Difetti Congeniti. Raccomandazione per la riduzione del rischio di difetti congeniti. Available from: www.iss.it/cnmr (Accessed August 24, 2015).
- 21.Salerno P, Bianchi F, Pierini A, Baldi F, Carbone P, Mantovani A, et al. Folic acid and congenital malformation: scientific evidence and public health strategies. Ann Ig. 2008;20:519–30. [PubMed] [Google Scholar]
- 22.Mastroiacovo P, Addis A. Folic acid: a public-health challenge. Lancet. 2006 doi: 10.1016/S0140-6736(06)68918-6. [DOI] [PubMed] [Google Scholar]
- 23.Lauria L, Lamberti A, Buoncristiano M, Bonciani M, Andreozzi S. Percorso nascita: promozione e valutazione della qualità di modelli operativi. Le indagini del 2008–2009 e del 2010–20112012. Instituto Superiore di Sanità. 2012.
- 24.Dante G, Morani L, Bronzetti D, Garutti P, Neri I, Calapai G, et al. Poor Folate Intake in a North Italian Pregnant Population: an Epidemiological Survey. Paediatr Perinat Epidemiol. 2015;29:501–4. doi: 10.1111/ppe.12226. [DOI] [PubMed] [Google Scholar]
- 25.Mastroiacovo P, Nilsen RM, Leoncini E, Gastaldi P, Allegri V, Boiani A, et al. Prevalence of maternal preconception risk factors: an Italian multicenter survey. Ital J Pediatr. 2014 doi: 10.1186/s13052-014-0091-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Morin P, Payette H, Moos MK, St-Cyr-Tribble D, Niyonsenga T, De Wals P. Measuring the intensity of pregnancy planning effort. Paediatr Perinat Epidemiol. 2003;17:97–105. doi: 10.1046/j.1365-3016.2003.00461.x. [DOI] [PubMed] [Google Scholar]
- 27.Lauria L, Lamberti A, Grandolfo M. Smoking behaviour before, during, and after pregnancy: the effect of breastfeeding. ScientificWorldJournal. 2012 doi: 10.1100/2012/154910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mills JL, Carter TC, Scott JM, Troendle JF, Gibney ER, Shane B, et al. Do high blood folate concentrations exacerbate metabolic abnormalities in people with low vitamin B-12 status? Am J Clin Nutr. 2011;94:495–500. doi: 10.3945/ajcn.111.014621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vollset SE, Clarke R, Lewington S, Ebbing M, Halsey J, Lonn E, et al. Effects of folic acid supplementation on overall and site-specific cancer incidence during the randomised trials: meta-analyses of data on 50,000 individuals. Lancet. 2013;381:1029–36. doi: 10.1016/S0140-6736(12)62001-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Eussen SJ, Nilsen RM. Midttun O, Hustad S, N IJ, Meyer K et al. North–south gradients in plasma concentrations of B-vitamins and other components of one-carbon metabolism in Western Europe: results from the European Prospective Investigation into Cancer and Nutrition (EPIC) Study. Br J Nutr. 2013;110:363–74. doi: 10.1017/S0007114512004990. [DOI] [PubMed] [Google Scholar]
- 31.Zappacosta B, Persichilli S, Iacoviello L, Di Castelnuovo A, Graziano M, Gervasoni J, et al. Folate, vitamin B12 and homocysteine status in an Italian blood donor population. Nutr Metab Cardiovasc Dis. 2013;23:473–80. doi: 10.1016/j.numecd.2011.10.001. [DOI] [PubMed] [Google Scholar]
- 32.Crider KS, Devine O, Hao L, Dowling NF, Li S, Molloy AM, et al. Population red blood cell folate concentrations for prevention of neural tube defects: Bayesian model. BMJ. 2014 doi: 10.1136/bmj.g4554. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Given that we are presently preparing other manuscripts involving preconception risk factors in this study sample, we elected to not share the raw data from this manuscript.


