Abstract
Esophageal and gastric cancer (GC) are related to obesity and bariatric surgery. Risk factors, such as gastroesophageal reflux and Helicobacter pylori, must be investigated and treated in obese population. After surgery, GC reports are anecdotal and treatment is not standardized. This review aims to discuss GC related to obesity before and after bariatric surgery.
Keywords: Obesity, bariatric surgery, stomach neoplasms, esophageal neoplasms
Introduction
Obesity remains an epidemic disease worldwide despite advanced clinical and surgical treatment over the past decades. Morbid obesity increases the risk of several diseases 1, including cancer, and can lead to increased morbidity related to cancer treatment 2, 3.
The relationship between cancer and obesity is known, but whether high body mass index (BMI) significantly affects overall cancer risk or whether intense weight loss postoperatively influences cancer incidence remains unclear. A recent meta-analysis demonstrated reduced cancer risk after bariatric surgery, but conclusion could not be drawn because of the high heterogeneity between studies 4. New research programs have focused on investigating proteins related to carcinogenesis that are hyper-expressed in obese patients and disappear after surgical weight loss.
Evidence of obesity as a risk factor for colon, breast, endometrial, and renal cell cancer is increasing 5, but different results are obtained related to gastric cancer (GC). A recent meta-analysis by Turati et al. 6 reviewed 22 studies and found a relative risk (RR) of 2.34 for BMI ≥30 kg/m 2 for cardia and esophageal adenocarcinoma. The European Prospective Investigation into Cancer and Nutrition conducted a multicenter study that included 23 centers and almost 400,000 patients with 11-year follow-up; this study showed the correlation of the abdominal waist circumference and visceral fat with greater risk to esophagus-gastric junction (EGJ) cancer 7.
In this context, we aim to review and discuss obesity and bariatric surgery and its risk factors related to GC.
Obesity as a risk factor for GC
Incidence of GC has decreased over the last decades. However, GC remains the fourth most common cancer worldwide and is usually in an advanced disease when it is diagnosed. This disease is classified into cardia and noncardia cancer, with distinct epidemiological and clinical characteristics and diverse treatment options 8.
Even though the relationship between obesity and GC remains controversial, with a recent meta-analysis showing no statistically significant association between obesity and non-cardia GC, data on cardia cancer are suggestive 9. A recent prospective study, including more than half a million people within the Me-Can Project 10, showed that high BMI is associated with an increased risk for esophageal adenocarcinoma, independently from other metabolic risk factors, such as blood pressure, glucose, cholesterol, and triglycerides.
Risk factors
Helicobacter pylori (H. pylori)
H. pylori is classified a type I carcinogen in humans and a well-established risk factor for GC 11. Following the continuity of gastritis, intestinal metaplasia, and dysplasia, H. pylori infection can lead to GC. Few studies have investigated the relationship between obesity and H. pylori infection 12, 13, and the evidence of obesity as a risk for gastric dysplasia is still poor 14. Kim et al. 15 studied more than 1,000 Korean patients to prove the association between obesity and GC regardless of H. pylori status. Their result showed an increased risk of early gastric cancer in men and gastric dysplasia in women, regardless of H. pylori infection.
Gastroesophageal reflux disease (GERD)
GERD and obesity are frequently related, and the prevalence of symptoms is correlated with high BMI 16. Super-obese patients with BMI ≥50 kg/m 2 exhibit higher prevalence of esophagitis compared with obese patients with BMI <40 kg/m 2 17.
Barrett's esophagus, a premalignant precursor, is also highly associated with obesity; however, given the low incidence of disease progression, obesity markers and predictors have been investigated 18, 19. Higher level of ghrelin is associated with an increased risk of Barrett's esophagus 20. Duggan et al. 21 proved that increased levels of leptin and insulin resistance in overweight patients are associated with high risk of progression from Barrett's esophagus to EGJ cancer.
The Barrett's and Esophageal Adenocarcinoma Consortium 22 study showed a positive association between heartburn/regurgitation symptoms and EGJ cancer. With regard to other risk factors, such as age, sex, and cigarette smoking, only BMI showed a different effect on stratified analysis with an increased risk for the obese group.
Inflammatory Factors
Obesity is associated with a low-grade chronic inflammation of white adipose tissue (WAT) that is related to insulin resistance and cardiovascular morbidity 23, 24. In obese patients, WAT activates the innate immune system and induces secretion of TNF-α and interleukin-6 25. In vivo and in vitro studies have shown that these cytokines are related to GC, inducing proliferation and inhibiting apoptosis of human GC cell lines 26.
Pathological findings
Several surgeons from different countries with high rates of GC, such as Japan, Korea, and Chile, suggested Roux-en-Y gastric bypass (RYGB) with resection of the distal stomach because accessing excluded stomach postoperatively is difficult 27, 28. Braghetto et al. 29 performed laparoscopic resectional gastric bypass in 112 obese patients, with 10.7% complication rate and only 2 duodenal stump leakages. Histological study found no GC and gastric dysplasia in only five patients.
Over the last 10 years, sleeve gastrectomy (SG) has gained popularity and provided an opportunity to examine the resected specimen, but no incidental finding of GC was reported. Several studies found high rates of gastritis and H. pylori infection on the pathological study of the resected stomach 30, 31; however, only case reports have described incidental findings of gastrointestinal stromal tumors (GIST) 32, 33. Given the scarce incidence of pathological findings, selective microscopic examination is endorsed as a safe and economic option, guided with clinical history and macroscopic examination 34.
Pre-operative screening
Current guidelines recommend routine upper gastrointestinal endoscopy (UGE) before bariatric surgery 35. As shown in Table 1 36- 48, several studies identified a wide range of findings, such as gastritis, esophagitis, hiatal hernia, and gastric or duodenal ulcers, but no study found incidental GC 36- 38. Routine UGE has been questioned because most of the findings are clinically irrelevant.
Table1.
Studies addressing routine upper gastrointestinal endoscopy before bariatric surgery
| Author | Year | Patients ( n) | Study format | Abnormal exam (%) | Gastric cancer ( n) |
| Verset et al. 36 | 1997 | 159 | Retrospective | 31-37 | 0 |
| Frigg et al. 37 | 2001 | 104 | Retrospective | 84.6 | 0 |
| Schirmer et al. 38 | 2002 | 536 | Retrospective | 4.9 | 0 |
| Sharaf et al. 39 | 2004 | 195 | Retrospective | 89.7 | 0 |
| Zeni et al. 40 | 2006 | 169 | Retrospective | 66.7 | 1 (GIST) |
| Korenkov et al. 41 | 2006 | 145 | Prospective | 10 | 0 |
| Azagury et al. 42 | 2006 | 319 | Retrospective | 46 | 0 |
| Almeida et al. 43 | 2007 | 162 | Retrospective | 77.2 | 0 |
| Loewen et al. 44 | 2008 | 447 | Retrospective | 31.5 | 0 |
| Peromaa-Haavisto et al. 45 | 2013 | 412 | Retrospective | 44.2 | 0 |
| Praveenraj et al. 46 | 2015 | 283 | Retrospective | 81 | 0 |
| Wiltberger et al. 47 | 2015 | 159 | Retrospective | 76 | 0 |
| Fernandes et al. 48 | 2016 | 613 | Retrospective | 56.3 | 0 |
Incidental findings without clinical suspicion can lead to unnecessary and morbid treatments, such as prophylactic gastrectomy for gastric polyposis that revealed as benign lesion 42. Fernandes et al. 48 were the first to address endoscopic findings and surgical complications. In regression analysis, endoscopic ulceration was the only predictor of postoperative complications.
GC after bariatric surgery
Reported cases of GC after bariatric surgery are anecdotal, with low level of evidence, arising between 1 and 10 years postoperatively. A recent meta-analysis showed 18 cases of GC after different bariatric procedures, with a mean diagnosis at 8.6 years and adenocarcinoma representing 83% of the cases ( Table 2) 49- 65.
Table2.
Data reported on gastric cancer after bariatric surgery
| Author | Age, years | Sex | Tumor site | Time after surgery (y) |
| Gastric bypass | ||||
| Khitin et al. 49 | 57 | F | Excluded stomach | 22 |
| Escalona et al. 50 | 51 | F | Excluded stomach | 8 |
| Trincado et al. 51 | 52 | F | Pouch | 5 |
| De Roover et al. 52 | 66 | M | - | 3 |
| Corsini et al. 53 | 57 | M | Excluded stomach | 4 |
| Babor R, Booth M 54 | 61 | F | Pouch | 29 |
| Harper et al. 55 | 45 | F | Excluded stomach | 1 |
| Watkins et al. 56 | 44 | M | Excluded stomach | 16 |
| Sun et al. 57 | 65 | M | Pouch | 5 |
| Vertical gastroplasty | ||||
| Zirak et al. 58 | 52 | F | Pouch | 2 |
| Papakonstantinou et al. 59 | 46 | M | Pylorus | 6 |
| Jain et al. 60 | 67 | F | Pouch | 15 |
| De Roover et al. 52 | 47 | F | - | 12 |
| Chebib et al. 61 | 60 | M | Pouch | 15 |
| Belhaj et al. 62 | 54 | F | Pylorus | 10 |
| Gastric banding | ||||
| Hackert et al. 63 | 62 | F | Pouch | 10 |
| Stroh et al. 64 | 65 | F | Pouch | 2.5 |
| Orlando et al. 65 | 37 | F | Lesser curvature | 0.5 |
Pathophysiological mechanism
Using the evidence of gastric stump cancer after Billroth II gastrectomy for peptic ulcer, anatomic changes after bariatric surgery may increase carcinogenic risk 66. However, according to tumor location, a different pathophysiological mechanism can be established.
RYGB is still the most common bariatric procedure and has the risk of cancer in the gastric pouch and the excluded stomach. Despite increasing evidence showing that RYGB has a positive role on GERD, with clinical and endoscopic improvement 67- 69, recent studies have proven the presence of bile reflux in the pouch; its presence can be related to cancer risk as alkaline reflux is widely accepted as a cause of esophagitis, Barrett's esophagus, and adenocarcinoma 70- 72.
The excluded stomach has no contact with food and its exogenous carcinogens; thus, pancreaticobiliary reflux may be responsible for cancer risk. Bile reflux in the excluded stomach is well known, and its attributed mucosal changes with atrophy, intestinal metaplasia, and chronic inflammation have been tested in experimental models 73. Endoscopic evaluation and cholescintigraphic study found bile in the excluded stomach in 68.6% and 36% of patients, respectively 74, 75.
For restrictive procedures, such as gastric banding and SG, the main mechanisms are GERD and its consequent mucosal transformations, food stasis causing chronic inflammation, and local irritation by the band. Previous studies showed that foreign body can lead to local pathological changes 76, but evidence also exists that the pressure applied by the gastric band can cause ischemia and metaplastic changes in the mucosa that can progress to malignancy 77.
Diagnostic assessment
Given the lack of surveillance program after bariatric surgery, a delay in diagnosis caused by unspecific symptoms is common. The most frequent complaints are dysphagia, nausea, vomiting, abdominal pain, and anemia, which are often attributed by physicians and patients to the effects of the bariatric surgery itself instead of a new disease 78.
UGE is the first and most important test if a patient is suspected of GC. This test must be carried out by experienced hands and with great criteria, as well as with photographic documentation and biopsy of any suspected area. If any strictures are observed, obtaining complete dilation is significant to perform complete evaluation of the stomach.
Computed tomography (CT) scan can help to locally access tumor extension and distant metastasis. In the case of RYGB, CT can be used as an initial diagnostic tool because excluded stomach is difficult to evaluate. It has an important role in evaluating gastric distention and greater tumors, but early lesions can be misdiagnosed and biopsy cannot be performed 56.
Several authors have reported different and innovative techniques to access the excluded stomach. Virtual gastroscopy was described in 2002 79 and has been performed through percutaneous and noninvasive techniques 80. Despite the better image quality of virtual gastroscopy, it has the same limitations to small lesions and histologic evaluation as the CT scan.
Endoscopic evaluation of the excluded stomach is described both via retrograde approach and double-balloon technique. Retrograde endoscopy has long been reported, but failures are frequent due to the angulations of the anastomosis 81. Double-balloon endoscopy was first described by Yamamoto et al. 82 in 2001. This technique can access the excluded stomach even with long limbs and shows high success rate (87.5%), as reported by Safatle-Ribeiro et al. 83.
Surgical treatment
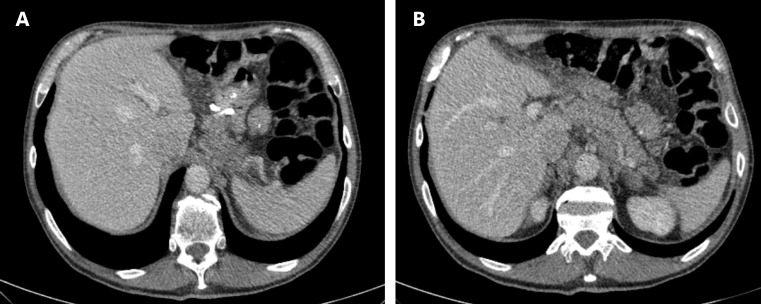
Given the unspecific symptoms and difficult diagnostic evaluation, several patients may present with locally advanced ( Figure 1) or metastatic disease 55. For these patients, multidisciplinary palliative treatment must be provided by surgeons, oncologists, radiotherapists, and nutritionists.
Figure1.
Computed tomography (CT) showing locally advanced gastric pouch cancer. (A) Pouch with silastic ring (B) Remanent stomach.
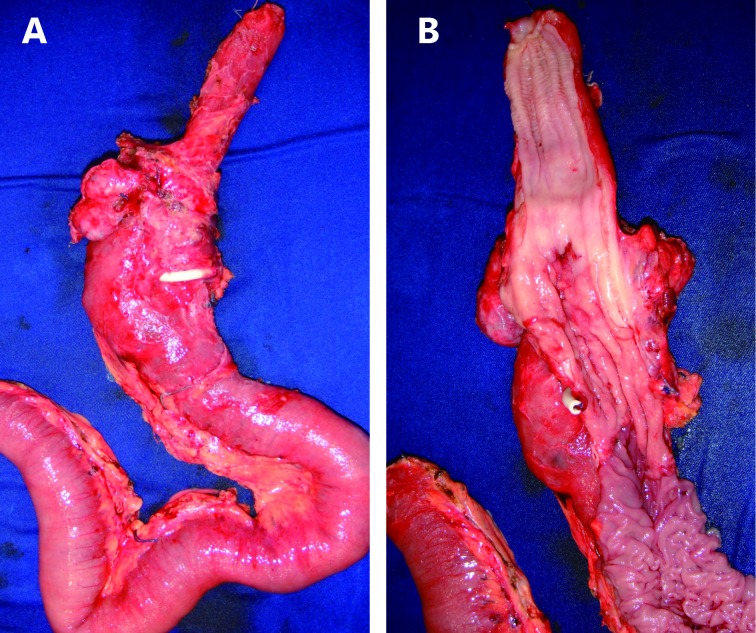
In cases amenable to surgical treatment, extent of resection is determined by tumor location 84. Tumors of the pouch can be treated similarly to EGJ tumors by removing the gastric pouch, esophagus, and regional lymph nodes ( Figure 2). In the case of a previous RYGB, the excluded stomach can be used for reconstruction and reach the neck for cervical anastomosis. Care must be taken to preserve the vascular supply of the greater curvature, particularly the right gastric and gastroepiploic arteries. If the bariatric procedure was a SG and the tumor is close to the cardia, a complete resection must be conducted and colon or jejunum can be used for reconstruction.
Figure2.
Surgical resection of gastric pouch cancer with subtotal esophagectomy. (A) Oesophagus, gastric pouch and alimentary limb (B) Detail of tumor in gastric pouch.
Neoplasms located in the excluded stomach are treated with total gastrectomy and D2 lymphadenectomy, following the same criteria for margins and extent of resection as GC treatment in general population. Nevertheless, resection of the Roux limb is unnecessary to preserve intestinal length and prevent nutritional complications.
Conclusions
Obesity is a risk factor for several types of cancer, including GC and EGJ. Reports of GC in gastric pouch or excluded stomach are rare, frequently asymptomatic and with incidental diagnosis. During bariatric surgery follow-up, late changes of symptoms, notably dysphagia, should be a warning sign for cancer diagnosis. Cancer treatment is ruled by current concepts, including surgical resection with D2 lymphadenectomy according to location with either gastrectomy of the excluded stomach or esophagectomy and pouch resection.
Conflict of interest statement
No potential conflicts of interest are disclosed.
References
- Samanic C, Chow WH, Gridley G, Jarvholm B, Fraumeni JF. Relation of body mass index to cancer risk in 362,552 Swedish men. Cancer Causes Control. 2006;17:901–9. doi: 10.1007/s10552-006-0023-9. [DOI] [PubMed] [Google Scholar]
- Parekh N, Chandran U, Bandera EV. Obesity in cancer survival. Annu Rev Nutr. 2012;32:311–42. doi: 10.1146/annurev-nutr-071811-150713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaidar-Person O, Bar-Sela G, Person B. The two major epidemics of the twenty-first century: obesity and cancer. Obes Surg. 2011;21:1792–7. doi: 10.1007/s11695-011-0490-2. [DOI] [PubMed] [Google Scholar]
- Casagrande DS, Rosa DD, Umpierre D, Sarmento RA, Rodrigues CG, Schaan BD. Incidence of cancer following bariatric surgery: systematic review and meta-analysis. Obes Surg. 2014;24:1499–509. doi: 10.1007/s11695-014-1276-0. [DOI] [PubMed] [Google Scholar]
- Boeing H. Obesity and cancer–the update 2013. Best Pract Res Clin Endocrinol Metab. 2013;27:219–27. doi: 10.1016/j.beem.2013.04.005. [DOI] [PubMed] [Google Scholar]
- Turati F, Tramacere I, La Vecchia C, Negri E. A meta-analysis of body mass index and esophageal and gastric cardia adenocarcinoma. Ann Oncol. 2013;24:609–17. doi: 10.1093/annonc/mds244. [DOI] [PubMed] [Google Scholar]
- Steffen A, Huerta JM, Weiderpass E, Bueno-De-Mesquita HB, May AM, Siersema PD, et al. General and abdominal obesity and risk of esophageal and gastric adenocarcinoma in the European Prospective Investigation into Cancer and Nutrition. Int J Cancer. 2015;137:646–57. doi: 10.1002/ijc.29432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rüdiger Siewert J, Feith M, Werner M, Stein HJ. Adenocarcinoma of the esophagogastric junction: results of surgical therapy based on anatomical/topographic classification in 1,002 consecutive patients. Ann Surg. 2000;232:353–61. doi: 10.1097/00000658-200009000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang P, Zhou Y, Chen B, Wan HW, Jia GQ, Bai HL, et al. Overweight, obesity and gastric cancer risk: results from a meta-analysis of cohort studies. Eur J Cancer. 2009;45:2867–73. doi: 10.1016/j.ejca.2009.04.019. [DOI] [PubMed] [Google Scholar]
- Lindkvist B, Johansen D, Stocks T, Concin H, Bjørge T, Almquist M, et al. Metabolic risk factors for esophageal squamous cell carcinoma and adenocarcinoma: a prospective study of 580,000 subjects within the Me-Can project. BMC Cancer. 2014;14:103. doi: 10.1186/1471-2407-14-103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. Some Industrial Chemicals. IARC Monogr Eval Carcinog Risks Hum. 1994;60:51–2. [Google Scholar]
- Kamada T, Hata J, Kusunoki H, Ito M, Tanaka S, Kawamura Y, et al. Eradication of helicobacter pylori increases the incidence of hyperlipidaemia and obesity in peptic ulcer patients. Dig Liver Dis. 2005;37:39–43. doi: 10.1016/j.dld.2004.07.017. [DOI] [PubMed] [Google Scholar]
- Torisu T. Atrophic gastritis, but not antibody to Helicobacter pylori, is associated with body mass index in a Japanese population. J Gastroenterol. 2008;43:762–6. doi: 10.1007/s00535-008-2219-0. [DOI] [PubMed] [Google Scholar]
- Kim HY. Metabolic syndrome is associated with gastric dysplasia. Eur J Gastroenterol Hepatol. 2011;23:871–5. doi: 10.1097/MEG.0b013e328349aa18. [DOI] [PubMed] [Google Scholar]
- Kim HJ, Kim N, Kim HY, Lee HS, Yoon H, Shin CM, et al. Relationship between body mass index and the risk of early gastric cancer and dysplasia regardless of Helicobacter pylori infection. Gastric Cancer. 2014;18:762–73. doi: 10.1007/s10120-014-0429-0. [DOI] [PubMed] [Google Scholar]
- Lagergren J, Bergström R, Lindgren A, Nyrén O. Symptomatic gastroesophageal reflux as a risk factor for esophageal adenocarcinoma. N Engl J Med. 1999;340:825–31. doi: 10.1056/NEJM199903183401101. [DOI] [PubMed] [Google Scholar]
- Santo MA, Quintanilha SR, Mietti CA, Kawamoto FM, Marson AG, de Cleva R. Endoscopic changes related to gastroesophageal reflux disease: comparative study among bariatric surgery patients. Arq Bras Cir Dig. 2015; 28 Suppl 1: 36-8.
- 18.Chang P, Friedenberg F. Obesity and GERD. Gastroenterol Clin North Am 2014;43:161-73.
- Kamat P, Wen S, Morris J, Anandasabapathy S. Exploring the association between elevated body mass index and Barrett's esophagus: a systematic review and meta-analysis. Ann Thorac Surg. 2009;87:655–62. doi: 10.1016/j.athoracsur.2008.08.003. [DOI] [PubMed] [Google Scholar]
- Thomas SJ, Almers L, Schneider J, Graham JE, Havel PJ, Corley DA. Ghrelin and leptin have a complex relationship with risk of barrett's esophagus. Dig Dis Sci. 2016;61:70–9. doi: 10.1007/s10620-015-3867-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duggan C, Onstad L, Hardikar S, Blount PL, Reid BJ, Vaughan TL. Association between markers of obesity and progression from Barrett's esophagus to esophageal adenocarcinoma. Clin Gastroenterol Hepatol. 2013;11:934–43. doi: 10.1016/j.cgh.2013.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook MB, Corley DA, Murray LJ, Liao LM, Kamangar F, Ye W, et al. Gastroesophageal reflux in relation to adenocarcinomas of the esophagus: a pooled analysis from the Barrett's and Esophageal Adenocarcinoma Consortium (BEACON) PLoS One. 2014; 9: e103508.
- Hotamisligil GS, Shargill NS, Spiegelman BM. Adipose expression of tumor necrosis factor-alpha: direct role in obesity-linked insulin resistance. Science. 1993;259:87–91. doi: 10.1126/science.7678183. [DOI] [PubMed] [Google Scholar]
- Cottam DR, Mattar SG, Barinas-Mitchell E, Eid G, Kuller L, Kelley DE, et al. The chronic inflammatory hypothesis for the morbidity associated with morbid obesity: implications and effects of weight loss. Obes Surg 2004; 14: 589-600.
- Bastard JP, Maachi M, Lagathu C, Kim MJ, Caron M, Vidal H, et al. Recent advances in the relationship between obesity, inflammation, and insulin resistance. Eur Cytokine Netw. 2006;17:4–12. [PubMed] [Google Scholar]
- Alemán JO, Eusebi LH, Ricciardiello L, Patidar K, Sanyal AJ, Holt PR. Mechanisms of obesity-induced gastrointestinal neoplasia. Gastroenterology. 2014;146:357–73. doi: 10.1053/j.gastro.2013.11.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Csendes A, Burdiles P, Papapietro K, Diaz JC, Maluenda F, Burgos A, et al. Results of gastric bypass plus resection of the distal excluded gastric segment in patients with morbid obesity. J Gastrointest Surg. 2005;9:121–31. doi: 10.1016/j.gassur.2004.05.006. [DOI] [PubMed] [Google Scholar]
- Kasama K, Tagaya N, Kanehira E, Oshiro T, Seki Y, Kinouchi M, et al. Laparoscopic sleeve gastrectomy with duodenojejunal bypass: technique and preliminary results. Obes Surg. 2009;19:1341–5. doi: 10.1007/s11695-009-9873-z. [DOI] [PubMed] [Google Scholar]
- Braghetto I, Csendes A, Korn O, Gutierrez L, Brunet L, Lanzarini E, et al. Laparoscopic resectional gastric bypass in patients with morbid obesity: experience on 112 consecutive patients. J Gastrointest Surg. 2011;15:71–80. doi: 10.1007/s11605-010-1383-8. [DOI] [PubMed] [Google Scholar]
- Almazeedi S, Al-Sabah S, Al-Mulla A, Al-Murad A, Al-Mossawi A, Al-Enezi K, et al. Gastric histopathologies in patients undergoing laparoscopic sleeve gastrectomies. Obes Surg. 2013;23:314–9. doi: 10.1007/s11695-012-0821-y. [DOI] [PubMed] [Google Scholar]
- Albawardi A, Almarzooqi S, Torab FC. Helicobacter pylori in sleeve gastrectomies: prevalence and rate of complications. Int J Clin Exp Med. 2013;6:140–3. [PMC free article] [PubMed] [Google Scholar]
- Beltran MA, Pujado B, Méndez PE, Gonzáles FJ, Margulis DI, Contreras MA, et al. Gastric gastrointestinal stromal tumor (GIST) incidentally found and resected during laparoscopic sleeve gastrectomy. Obes Surg. 2010;20:393–6. doi: 10.1007/s11695-009-0009-2. [DOI] [PubMed] [Google Scholar]
- Yuval JB, Khalaileh A, Abu-Gazala M, Shachar Y, Keidar A, Mintz Y, et al. The true incidence of gastric GIST-a study based on morbidly obese patients undergoing sleeve gastrectomy. Obes Surg. 2014;24:2134–7. doi: 10.1007/s11695-014-1336-5. [DOI] [PubMed] [Google Scholar]
- Abdullgaffar B, Raman L, Khamas A, Albadri F. Should we abandon routine microscopic examination in bariatric sleeve gastrectomy specimens. Obes Surg. 2016;26:105–10. doi: 10.1007/s11695-015-1726-3. [DOI] [PubMed] [Google Scholar]
- American Societyfor Gastrointestinal Endoscopy Standards of Practice Committee, Evans JA, Muthusamy VR, Acosta RD, Bruining DH, Chandrasekhara V, et al. The role of endoscopy in the bariatric surgery patient. Gastrointest Endosc. 2015;81:1063–72. doi: 10.1016/j.gie.2014.09.044. [DOI] [PubMed] [Google Scholar]
- Verset D, Houben JJ, Gay F, Elcheroth J, Bourgeois V, Van Gossum A. The place of upper gastrointestinal tract endoscopy before and after vertical banded gastroplasty for morbid obesity. Dig Dis Sci. 1997;42:2333–7. doi: 10.1023/a:1018835205458. [DOI] [PubMed] [Google Scholar]
- Frigg A, Peterli R, Zynamon A, Lang C, Tondelli P. Radiologic and endoscopic evaluation for laparoscopic adjustable gastric banding: preoperative and follow-up. Obes Surg. 2001;11:594–9. doi: 10.1381/09608920160557075. [DOI] [PubMed] [Google Scholar]
- Schirmer B, Erenoglu C, Miller A. Flexible endoscopy in the management of patients undergoing Roux-en-Y gastric bypass. Obes Surg. 2002;12:634–8. doi: 10.1381/096089202321019594. [DOI] [PubMed] [Google Scholar]
- Sharaf RN, Weinshel EH, Bini EJ, Rosenberg J, Sherman A, Ren CJ. Endoscopy plays an important preoperative role in bariatric surgery. Obes Surg. 2004;14:1367–72. doi: 10.1381/0960892042583806. [DOI] [PubMed] [Google Scholar]
- Zeni TM, Frantzides CT, Mahr C, Denham EW, Meiselman M, Goldberg MJ, et al. Value of preoperative upper endoscopy in patients undergoing laparoscopic gastric bypass. Obes Surg. 2006;16:142–6. doi: 10.1381/096089206775565177. [DOI] [PubMed] [Google Scholar]
- Korenkov M, Sauerland S, Shah S, Junginger T. Is routine preoperative upper endoscopy in gastric banding patients really necessary. Obes Surg. 2006;16:45–7. doi: 10.1381/096089206775222104. [DOI] [PubMed] [Google Scholar]
- Azagury D, Dumonceau JM, Morel P, Chassot G, Huber O. Preoperative work-up in asymptomatic patients undergoing Roux-en-Y gastric bypass: is endoscopy mandatory. Obes Surg. 2006;16:1304–11. doi: 10.1381/096089206778663896. [DOI] [PubMed] [Google Scholar]
- De Moura Almeida A, Cotrim HP, Santos AS, Bitencourt AG, Barbosa DB, Lobo AP, et al. Preoperative upper gastrointestinal endoscopy in obese patients undergoing bariatric surgery: is it necessary. Surg Obes Relat Dis. 2008;4:144–9; discussion 150-1. doi: 10.1016/j.soard.2007.12.006. [DOI] [PubMed] [Google Scholar]
- Loewen M, Giovanni J, Barba C. Screening endoscopy before bariatric surgery: a series of 448 patients. Surg Obes Relat Dis. 2008;4:709–12. doi: 10.1016/j.soard.2008.02.009. [DOI] [PubMed] [Google Scholar]
- Peromaa-Haavisto P, Victorzon M. Is routine preoperative upper GI endoscopy needed prior to gastric bypass. Obes Surg. 2013;23:736–9. doi: 10.1007/s11695-013-0956-5. [DOI] [PubMed] [Google Scholar]
- Praveenraj P, Gomes RM, Kumar S, Senthilnathan P, Parathasarathi R, Rajapandian S, et al. Diagnostic yield and clinical implications of preoperative upper gastrointestinal endoscopy in morbidly obese patients undergoing bariatric surgery. J Laparoendosc Adv Surg Tech A. 2015;25:465–9. doi: 10.1089/lap.2015.0041. [DOI] [PubMed] [Google Scholar]
- Wiltberger G, Bucher JN, Schmelzle M, Hoffmeister A, Dietrich A. Preoperative endoscopy and its impact on perioperative management in bariatric surgery. Dig Surg. 2015;32:238–42. doi: 10.1159/000381811. [DOI] [PubMed] [Google Scholar]
- Fernandes SR, Meireles LC, Carrilho-Ribeiro L, Velosa J. The role of rou.ine upper gastrointestinal endoscopy before bariatric surgery. Obes Surg. 2016 Jan 10 [Epub ahead of print].
- Khitin L, Roses RE, Birkett DH. Cancer in the gastric remnant after gastric bypass: a case report. Curr Surg. 2004;60:521–3. doi: 10.1016/S0149-7944(03)00052-7. [DOI] [PubMed] [Google Scholar]
- Escalona A, Guzmán S, Ibáñez L, Meneses L, Huete A, Solar A. Gastric cancer after Roux-en-Y gastric bypass. Obes Surg. 2005;15:423–7. doi: 10.1381/0960892053576668. [DOI] [PubMed] [Google Scholar]
- Trincado MT, Del Olmo JC, García Castaño J, Cuesta C, Blanco JI, Awad S, et al. Gastric pouch carcinoma after gastric bypass for morbid obesity. Obes Surg. 2005;15:1215–7. doi: 10.1381/0960892055002383. [DOI] [PubMed] [Google Scholar]
- De Roover A, Detry O, De Leval L, Coimbra C, Desaive C, Honoré P, et al. Report of two cases of gastric cancer after bariatric surgery: lymphoma of the bypassed stomach after Roux-en-Y gastric bypass and gastrointestinal stromal tumor (GIST) after vertical banded gastroplasty. Obes Surg. 2006;16:928–31. doi: 10.1381/096089206777822142. [DOI] [PubMed] [Google Scholar]
- Corsini DA, Simoneti CA, Moreira G, Lima SE, Garrido AB. Cancer in the excluded stomach 4 years after gastric bypass. Obes Surg. 2006;16:932–4. doi: 10.1381/096089206777822313. [DOI] [PubMed] [Google Scholar]
- Babor R, Booth M. Adenocarcinoma of the gastric pouch 26 years after loop gastric bypass. Obes Surg. 2006;16:935–8. doi: 10.1381/096089206777822223. [DOI] [PubMed] [Google Scholar]
- Harper JL, Beech D, Tichansky DS, Madan AK. Cancer in the bypassed stomach presenting early after gastric bypass. Obes Surg. 2007;17:1268–71. doi: 10.1007/s11695-007-9216-x. [DOI] [PubMed] [Google Scholar]
- Watkins BJ, Blackmun S, Kuehner ME. Gastric adenocarcinoma after Roux-en-Y gastric bypass: access and evaluation of excluded stomach. Surg Obes Relat Dis. 2007;3:644–7. doi: 10.1016/j.soard.2007.06.008. [DOI] [PubMed] [Google Scholar]
- Sun C, Jackson CS, Reeves M, Rendon S. Metastatic adenocarcinoma of the gastric pouch 5 years after Roux-en-Y gastric bypass. Obes Surg. 2008;18:345–8. doi: 10.1007/s11695-007-9394-6. [DOI] [PubMed] [Google Scholar]
- Zirak C, Lemaitre J, Lebrun E, Journé S, Carlier P. Adenocarcinoma of the pouch after silastic ring vertical gastroplasty. Obes Surg. 2002;12:693–4. doi: 10.1381/096089202321019701. [DOI] [PubMed] [Google Scholar]
- Papakonstantinou A, Moustafellos P, Terzis I, Stratopoulos C, Hadjiyannakis EI. Gastric cancer occurring after vertical banded gastroplasty. Obes Surg. 2002;12:118–20. doi: 10.1381/096089202321144694. [DOI] [PubMed] [Google Scholar]
- Jain PK, Ray B, Royston CM. Carcinoma in the gastric pouch years after vertical banded gastroplasty. Obes Surg. 2003;13:136–7. doi: 10.1381/096089203321136746. [DOI] [PubMed] [Google Scholar]
- Chebib I, Beck PL, Church NG, Medlicott SA. Gastric pouch adenocarcinoma and tubular adenoma of the pylorus: a field effect of dysplasia following bariatric surgery. Obes Surg. 2007;17:843–6. doi: 10.1007/s11695-007-9130-2. [DOI] [PubMed] [Google Scholar]
- Belhaj A, Memmo L, Memo L, Mehdi A, Mboti F, Closset J. Gastric adenocarcinoma following "silastic vertical ring gastroplasty": case report. Rev Med Brux. 2010;31:459–62. [PubMed] [Google Scholar]
- Hackert T, Dietz M, Tjaden C, Sieg A, Buchler MW, Schmidt J. Band erosion with gastric cancer. Obes Surg. 2004;14:559–61. doi: 10.1381/096089204323013622. [DOI] [PubMed] [Google Scholar]
- Stroh C, Hohmann U, Urban H, Manger T. Gastric cancer after laparoscopic adjustable gastric banding. Obes Surg. 2008;18:1200–2. doi: 10.1007/s11695-008-9473-3. [DOI] [PubMed] [Google Scholar]
- Orlando G, Pilone V, Vitiello A, Gervasi R, Lerose MA, Silecchia G, et al. Gastric cancer following bariatric surgery: a review. Surg Laparosc Endosc Percutan Tech. 2014;24:400–5. doi: 10.1097/SLE.0000000000000050. [DOI] [PubMed] [Google Scholar]
- Macdonald WC, Owen DA. Gastric carcinoma after surgical treatment of peptic ulcer: an analysis of morphologic features and a comparison with cancer in the nonoperated stomach. Cancer. 2001;91:1732–8. doi: 10.1002/1097-0142(20010501)91:9<1732::aid-cncr1191>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- Smith SC, Edwards CB, Goodman GN. Symptomatic and clinical improvement in morbidly obese patients with gastroesophageal reflux disease following Roux-en-Y gastric bypass. Obes Surg. 1997;7:479–84. doi: 10.1381/096089297765555205. [DOI] [PubMed] [Google Scholar]
- Nelson LG, Gonzalez R, Haines K, Gallagher SF, Murr MM. Amelioration of gastroesophageal reflux symptoms following Roux-en-Y gastric bypass for clinically significant obesity. Am Surg. 2005;71:950–3; discussion 953-4. [PubMed] [Google Scholar]
- Madalosso CA, Gurski RR, Callegari-Jacques SM, Navarini D, Mazzini G, Pereira Mda S. The impact of gastric bypass on gastroesophageal reflux disease in morbidly obese patients. Ann Surg. 2016;263:110–6. doi: 10.1097/SLA.0000000000001139. [DOI] [PubMed] [Google Scholar]
- Hak NG, Mostafa M, Salah T, El-Hemaly M, Haleem M, Abd El-Raouf A, et al. Acid and bile reflux in erosive reflux disease, non-erosive reflux disease and Barrett's esophagus. Hepatogastroenterology. 2008;55:442–7. [PubMed] [Google Scholar]
- Attwood SE, Demeester TR, Bremner CG, Barlow AP, Hinder RA. Alkaline gastroesophageal reflux: implications in the development of complications in Barrett's columnar-lined lower esophagus. Surgery. 1989;106:764–70. [PubMed] [Google Scholar]
- Gillen P, Keeling P, Byrne PJ, Healy M, O'moore RR, Hennessy TP. Implication of duodenogastric reflux in the pathogenesis of Barrett's oesophagus. Br J Surg. 1988;75:540–3. doi: 10.1002/bjs.1800750612. [DOI] [PubMed] [Google Scholar]
- Cunha Medeiros A, Meneses Rego A, Medeiros Azevedo I, Ferreira Carvalho M, Brasil Medeiros V, Araujo-Filho I. Metabolism and gastric remnant changes after Roux-en-Y gastric bypass in rats. J Invest Surg. 2011;24:109–14. doi: 10.3109/08941939.2011.557468. [DOI] [PubMed] [Google Scholar]
- Kuga R, Safatle-Ribeiro AV, Faintuch J, Ishida RK, Furuya CK, Garrido AB, et al. Endoscopic findings in the excluded stomach after Roux-en-Y gastric bypass surgery. Arch Surg. 2007;142:942–6. doi: 10.1001/archsurg.142.10.942. [DOI] [PubMed] [Google Scholar]
- Sundbom M, Hedenström H, Gustavsson S. Duodenogastric bile reflux after gastric bypass: a cholescintigraphic study. Dig Dis Sci. 2002;47:1891–6. doi: 10.1023/a:1016429603337. [DOI] [PubMed] [Google Scholar]
- Negri M, Bendet N, Halevy A, Halpern Z, Reif R, Bogokovsky H, et al. Gastric mucosal changes following gastroplasty: a comparative study between vertical banded gastroplasty and silastic ring vertical gastroplasty. Obes Surg. 1995;5:383–6. doi: 10.1381/096089295765557458. [DOI] [PubMed] [Google Scholar]
- Cariani S, Amenta E. Three-year results of Roux-en-Y gastric bypass-on-vertical banded gastroplasty: an effective and safe procedure which enables endoscopy and X-ray study of the stomach and biliary tract. Obes Surg. 2007;17:1312–8. doi: 10.1007/s11695-007-9234-8. [DOI] [PubMed] [Google Scholar]
- Scozzari G, Trapani R, Toppino M, Morino M. Esophagogastric cancer after bariatric surgery: systematic review of the literature. Surg Obes Relat Dis. 2013;9:133–42. doi: 10.1016/j.soard.2012.10.002. [DOI] [PubMed] [Google Scholar]
- Silecchia G, Catalano C, Gentileschi P, Elmore U, Restuccia A, Gagner M, et al. Virtual gastroduodenoscopy: a new look at the bypassed stomach and duodenum after laparoscopic Roux-en-Y gastric bypass for morbid obesity. Obes Surg. 2002;12:39–48. doi: 10.1381/096089202321144568. [DOI] [PubMed] [Google Scholar]
- Alva S, Eisenberg D, Duffy A, Roberts K, Israel G, Bell R. A new modality to evaluate the gastric remnant after Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2008;4:46–9; discussion 49. doi: 10.1016/j.soard.2007.09.008. [DOI] [PubMed] [Google Scholar]
- Sinar DR, Flickinger EG, Park HK, Sloss RR. Retrograde endoscopy of the bypassed stomach segment after gastric bypass surgery: unexpected lesions. South Med J. 1985;78:255–8. doi: 10.1097/00007611-198503000-00006. [DOI] [PubMed] [Google Scholar]
- Yamamoto H, Sekine Y, Sato Y, Higashizawa T, Miyata T, Iino S, et al. Total enteroscopy with a nonsurgical steerable double-balloon method. Gastrointest Endosc. 2001;53:216–20. doi: 10.1067/mge.2001.112181. [DOI] [PubMed] [Google Scholar]
- Safatle-Ribeiro AV, Kuga R, Iriya K, Ribeiro U, Faintuch J, Ishida RK, et al. What to expect in the excluded stomach mucosa after vertical banded Roux-en-Y gastric bypass for morbid obesity. J Gastrointest Surg. 2007;11:133–7. doi: 10.1007/s11605-006-0047-1. [DOI] [PubMed] [Google Scholar]
- Kuruba R, Jawad M, Karl RC, Murr MM. Technique of resection of esophageal adenocarcinoma after Roux-en-Y gastric bypass and literature review of esophagogastric tumors after bariatric procedures. Surg Obes Relat Dis. 2009;5:576–81. doi: 10.1016/j.soard.2009.02.009. [DOI] [PubMed] [Google Scholar]