Abstract
Background:
Ultrasound-guided transversus abdominis plane (TAP) block has been used for intra- and post-operative analgesia during abdominal operations and for ureteric shock wave lithotripsy (SWL) as well.
Aim:
This study aimed at comparing ultrasound-guided unilateral versus bilateral TAP blocks as analgesic techniques for unilateral ureteric SWL.
Settings and Design:
Prospective randomized comparative study.
Patients and Methods:
Sixty patients scheduled for unilateral ureteric SWL were randomly allocated into two groups: Group (U) received unilateral TAP block in the form of 25 ml of bupivacaine 0.25% (i.e., 62.5 mg), and Group (B) received bilateral TAP blocks in the form of 25 ml of bupivacaine 0.25% (i.e., 62.5 mg) on each side.
Statistical Analysis:
This was performed using SPSS program version 19 ((IBM Corp., Armonk, NY, USA) and EP 16 program.
Results:
The mean values of intra- and post-procedural visual analog scale at different time intervals were around (30), which was statistically insignificant between groups (P > 0.05). There were no significant differences between groups regarding cardiopulmonary stability, postanesthesia care unit time, the total amount of rescue fentanyl and patient satisfaction scores (P > 0.05). There were no significant side effects in both groups.
Conclusion:
Ultrasound-guided unilateral TAP block is as safe and effective analgesic technique as bilateral TAP blocks during unilateral ureteric SWL. It can be used as the sole analgesic technique during ureteric SWL.
Keywords: Extracorporeal shock wave lithotripsy, transversus abdominis plane block, ultrasound-guided
INTRODUCTION
The transversus abdominis plane (TAP) block technique was first described by Kuppuvelumani et al. in 1993[1] and formally documented by Rafi in 2001.[2] It is suggested as a part of the multimodal anesthetic approach for the management of surgical abdominal pain by injecting local anesthetics into the plane between the internal oblique (IO) and transversus abdominis (TA) muscles.[2,3] Ultrasound was introduced to improve the accuracy and success rate of TAP blocks and to prevent complications.[4] TAP block has been proved to be a safe and effective postoperative analgesic technique in a variety of general,[5,6] gynecological,[7] urological,[8] and laparoscopic surgeries.[9,10]
Different analgesic agents and techniques, such as general anesthesia, regional anesthesia, patient-controlled analgesia, and monitored anesthesia care, have been used to manage the pain induced by shock wave lithotripsy (SWL).[11] Previously, we proved in a study the safety and effectiveness of ultrasound-guided unilateral TAP block as an analgesic technique during ureteric SWL. It provided optimal analgesia, less rescue analgesia, less intra- and post-procedural sedation, early ambulation, and early discharge from postanesthesia care unit (PACU) without significant side effects.[12]
The aim of this study was to evaluate the analgesic efficacy and safety of ultrasound-guided unilateral TAP block compared to bilateral TAP blocks as an analgesic technique during ureteric SWL.
PATIENTS AND METHODS
After approval of the Medical Ethics Committee, sixty patients American Society of Anesthesiologists (ASA) physical status Class I, II, and III were enrolled in this prospective randomized, single-blinded clinical trial. Patients were between 18 and 60 years of age, of both genders, with single radio-opaque unilateral ureteric stone scheduled for elective unilateral ureteric SWL.
This study was conducted at the Department of Urology, Dr. Soliman Fakeeh Hospital, Jeddah, KSA. Written informed consent was obtained from all patients before participating in the study. Exclusion criteria were: Patient's refusal, coagulopathy, psychological abnormalities, severe cardio-respiratory, renal or liver diseases, chronic alcohol/drug abusers and those allergic to any of the medications to be used in the study.
On patient's arrival at the SWL unit, preoperative check-up was done, and the procedure was explained. Each patient was instructed on the use of a standard 100 mm linear visual analog scale (VAS) with “0” as no pain and “100” as the worst imaginable pain. Patients were advised not to move during the procedure and to ask for analgesia for discomfort or intolerable pain.
Baseline measurements of heart rate (HR), mean arterial pressure (MAP), respiratory rate (RR) and room air oxygen saturation (SpO2) were obtained using an electrocardiogram, a “Dinamap” automated blood pressure monitor and a pulse oximeter, respectively. Those parameters were recorded for all patients after performing the TAP block and then every 10 min during the procedure and at the PACU time.
Venous access was secured by 20G intravenous (IV) cannula. Paracetamol 1 g (Perfalgan™, Bristol-Myer's-Squibb) was infused to alleviate visceral pain. Ringer's lactate drip (10 ml/kg/h) was started, oxygen face mask (6 L/min) was applied, and IV midazolam (0.05 mg/kg) was given as a premedication.
Patients were randomized, following a sealed envelope method, to receive either ultrasound-guided unilateral TAP block (Group U; n = 30) or ultrasound-guided bilateral TAP blocks (Group B; n = 30). Intra- and post-operative data were recorded by a physician blinded to the study groups.
In Group (U), the unilateral TAP block was performed in a supine position, at the same side of the stone, 10 min before the procedure. Using a portable ultrasound device (SonoSite™, Bothell, WA, USA), a linear 6–13 MHz ultrasound transducer, covered with a sterile plastic sheath, was placed midway between the 12th rib and the iliac crest at the level of the anterior axillary line, after skin preparation with an antiseptic solution. The initial image was optimized by sliding the probe antero-posteriorly, and/or tilting in a cephalad – caudad direction until the plane between the IO and TA muscles was clearly distinguished on screen. Using an in-plane approach, skin entry was 1–2 cm away from the transducer. After local infiltration of the skin with 1 ml lidocaine 2%, an 80 mm 20G needle (B-Braun Stimuplex, Melsungen, Germany) was advanced into the TAP. Once the needle tip was visualized to be in the plane between the IO and TA muscles, and after negative pressure aspiration, 25 ml of bupivacaine 0.25% (62.5 mg) was injected in 5 ml increments. In Group (B), the same approach was done bilaterally, injecting 25 ml of bupivacaine 0.25% (62.5 mg) on each side.
Before starting with SWL, decreased sensation in the appropriate dermatomal levels was confirmed by pinprick. SWL was performed by SWL machine (Lithoskop™; combined X-ray/shock wave C-arm system, Siemens, Germany). The shock wave emitter was applied on the patient's anterior abdominal wall at the same side of the stone. Hemodynamic (HR and MAP) and respiratory (RR and SpO2) variables and VASs were recorded at 10 min-intervals, both intra-operatively as well as in the PACU. Patients who developed intra- or post-operative pain (VAS >30) received fentanyl 0.5 mcg/kg IV, which was repeated on demand. The total amount of rescue fentanyl was noted.
At the end of the procedure, patients were transferred to the PACU for observation until fulfilling our local discharge criteria (i.e., fully conscious, hemodynamically stable, having no nausea or vomiting, and pain-free). Variables related to the urologic procedure (e.g., side, site, and size of the stone, its fragmentation degree, the total number of shockwaves, their maximum power, and the total duration of the procedure) as well as the length of PACU stay were all recorded and considered for statistical analysis. All patients were closely observed for nausea and/or vomiting, signs and symptoms of local anaesthetic toxicity and side effects of fentanyl, for example, bradycardia (HR <50 beats/min), hypotension (MAP <20% of baseline), bradypnea (RR <10 breaths/min), hypoxia (SpO2 <93%), and pruritus.
Before discharge to the ward, patient's satisfaction was assessed using the 7-point Likert scale[13] as follows: 1 = extremely dissatisfied, 2 = dissatisfied, 3 = somewhat dissatisfied, 4 = undecided, 5 = somewhat satisfied, 6 = satisfied, 7 = extremely satisfied.
Sample size was calculated according to a confidence interval of 95% and power of the test of 80%; considering the primary outcome of this study as the VAS for pain evaluation. Based on a previous investigation, 25 patients per group was the minimum sample size required to demonstrate a statistically significant difference in the VASs. In our study, we included sixty patients, thirty in each group.
Statistical analysis was performed using SPSS program version 19 (IBM Corp., Armonk, NY, USA) and EP16 program. Student's t-test, Chi-square test, Mann–Whitney U-test, and Fisher's exact test were used for statistical analysis as appropriate. Data are presented as a mean ± standard deviation, median, numbers, and frequencies as appropriate. Statistical significance was determined at P < 0.05.
RESULTS
Out of 64 consecutive patients scheduled for unilateral ureteric SWL, 4 were excluded; 2 in Group U (due to failure of TAP block because of marked obesity) and 2 in Group B (failed TAP block in one patient and the other patient asked for general anesthesia while performing the block). Hence, sixty patients were enrolled in the study (thirty patients randomly allocated in each group) to be considered for analysis [Figure 1].
Figure 1.
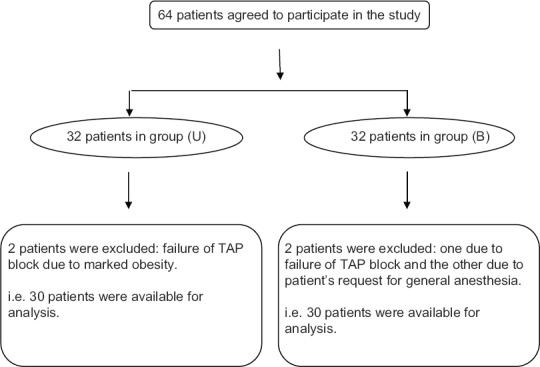
Flow chart of the study
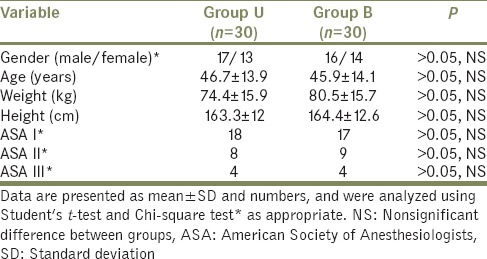
Demographic data (age, gender, weight, height, and ASA classification) were comparable, and no statistically significant differences were observed between groups (P > 0.05) [Table 1].
Table 1.
Demographic data of patients
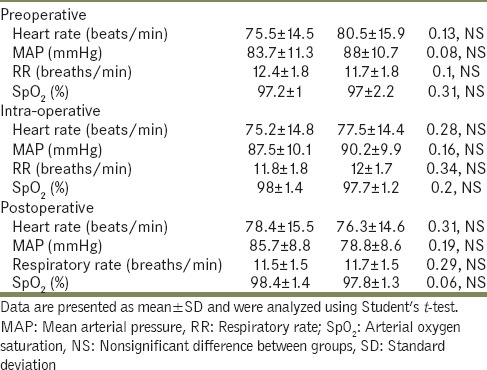
Pre-, intra- and post-operative mean values of HR (beats/min), mean blood pressure (mmHg), RR (breaths/min) and arterial oxygen saturation (%) were comparable between the two groups (P > 0.05) [Table 2].
Table 2.
Mean values of perioperative vital signs
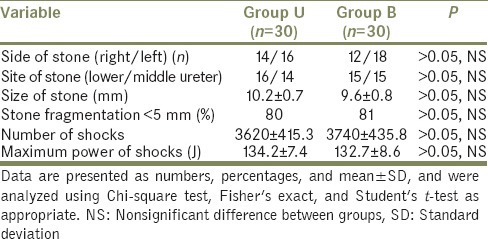
Variables of the urologic procedure (e.g., side, site, and size of the ureteric stone, its fragmentation percentage, the number of shocks required to crush the stone and the maximum power of shocks), were all insignificant between groups (P > 0.05) [Table 3].
Table 3.
Variables of the urologic procedure
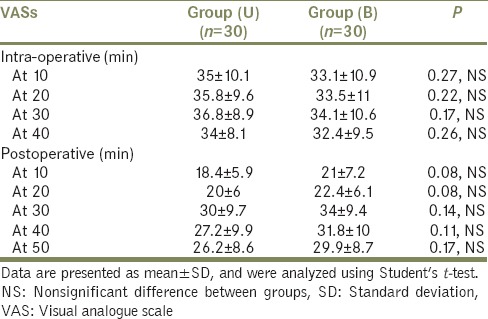
The mean values of intra- and post-procedural VAS at different time intervals showed no statistically significant differences between groups (P > 0.05) [Table 4].
Table 4.
Intra- and post-procedural visual analogue scales
Rescue analgesia (fentanyl 0.5 μg/kg IV) was promptly given (at a VAS >30). The mean values of the total amount of fentanyl given were comparable between both groups (46.8 ± 11.2 μg in Group U versus 48 ± 15.8 μg in Group B) (P > 0.05) [Table 5].
Table 5.
Procedure duration, postanesthesia care unit time, total fentanyl consumption and patient satisfaction scores
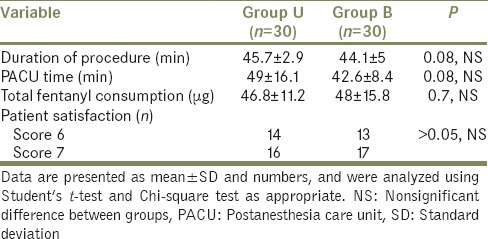
Furthermore, there were no statistically significant differences between groups regarding the duration of the procedure and PACU stay, and patient satisfaction scores (P > 0.05) [Table 5].
We reported four patients who had nausea (two patients in each group), which was managed conservatively by ondansetron 4 mg IV.
There were no reported cases of bradycardia (HR <50 beats/min), hypotension (MAP <20% of baseline), hypoxia (SpO2 <93%), respiratory depression (RR <10 breaths/min), pruritus or signs of local anesthetic toxicity in either group.
DISCUSSION
In this study, we compared unilateral TAP block against bilateral blocks (both done under ultrasound guidance) as an analgesic technique during unilateral ureteric SWL. We found that both techniques offered a very good analgesia during and after the procedure, cardiopulmonary stability, no significant side effects, and high patient satisfaction.
TAP blocks have been used as a part of multimodal analgesia in many clinical trials for patients undergoing abdominal operations,[5] radical prostatectomy,[8] inguinal herniorrhaphy, and laparoscopic surgeries.[10] The analgesic effect of ultrasound-guided TAP block results from blockage of the nerve supply to the anterior abdominal wall which arises from the lower six thoracic, first lumber, iliohypogastric, and ilioinguinal nerves. These nerves pass in the fascial plane between the IO and TA muscles where they are blocked.[14,15]
Using computerized tomography and magnetic resonance imaging to study the spread of “iopamidol” contrast (injected within the TAP into three volunteers), the contrast spread from the superior margin of the iliac crest up to the costal margin and extended posteriorly until the quadratus lumborum muscle.[14] In a cadaveric study, 20 ml of aniline blue dye was injected into the TAP at the mid-axillary line; the dye spread between the iliac crest, the costal margin and the lateral border of the rectus abdominis sheath.[15]
In a previous study, we proved that ultrasound-guided unilateral TAP block using 25 ml of bupivacaine 0.25% (62.5 mg) was an effective analgesic alternative to IV fentanyl (1.5 μg/kg) during ureteric SWL, as it offered a satisfying analgesia during and after the procedure, significantly less requirements for rescue pethidine, lower sedation scores, and shorter PACU stay without significant side effects.[12]
In our previous study, we noticed that although part of the shockwave emitter crossed the midline of the abdominal wall in some cases, the quality of analgesia was not affected.[12] This can be explained by the fact that shockwaves emerging from the center of the emitter would still be on the same side of the stone, even if the emitter partly crossed the midline. This explanation, indeed, supports the results obtained in this study: No significant differences between unilateral versus bilateral TAP blocks during ureteric SWL regarding intra- and post-procedural pain scores, total doses of rescue fentanyl during and after the procedure, duration of PACU stay and overall patient satisfaction scores.
One of the limitations of this study is that it was extended only till the end of PACU time. In addition, there was no control group for proper comparison. However, I considered the unilateral TAP block group to be the control since it was proven in a previous study that it is a safe and effective analgesic technique during ureteric SWL.[2]
CONCLUSION
Ultrasound-guided unilateral TAP block is as safe and effective analgesic technique as bilateral blocks during unilateral ureteric SWL. It can be used as the sole analgesic technique during ureteric SWL, for its beneficial analgesia during and after the procedure, cardiopulmonary stability, insignificant side effects and high patient satisfaction scores.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors would like to thank Dr. Ahmad Elnady, Consultant of Anesthesia for generous support and valuable viewpoints in language correction and evaluation of the study.
REFERENCES
- 1.Kuppuvelumani P, Jaradi H, Delilkan A. Abdominal nerve blockade for postoperative analgesia after caesarean section. Asia Oceania J Obstet Gynaecol. 1993;19:165–9. doi: 10.1111/j.1447-0756.1993.tb00368.x. [DOI] [PubMed] [Google Scholar]
- 2.Rafi AN. Abdominal field block: A new approach via the lumbar triangle. Anaesthesia. 2001;56:1024–6. doi: 10.1046/j.1365-2044.2001.02279-40.x. [DOI] [PubMed] [Google Scholar]
- 3.Aveline C, Le Hetet H, Le Roux A, Vautier P, Cognet F, Vinet E, et al. Comparison between ultrasound-guided transversus abdominis plane and conventional ilioinguinal/iliohypogastric nerve blocks for day-case open inguinal hernia repair. Br J Anaesth. 2011;106:380–6. doi: 10.1093/bja/aeq363. [DOI] [PubMed] [Google Scholar]
- 4.Jankovic Z. Transversus abdominutesis plane block: The holy grail of anaesthesia for (lower) abdominutesal surgery. Period Biol. 2009;111:203–8. [Google Scholar]
- 5.Sharma P, Chand T, Saxena A, Bansal R, Mittal A, Shrivastava U. Evaluation of postoperative analgesic efficacy of transversus abdominis plane block after abdominal surgery: A comparative study. J Nat Sci Biol Med. 2013;4:177–80. doi: 10.4103/0976-9668.107286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Johns N, O’Neill S, Ventham NT, Barron F, Brady RR, Daniel T. Clinical effectiveness of transversus abdominis plane (TAP) block in abdominal surgery: A systematic review and meta-analysis. Colorectal Dis. 2012;14:e635–42. doi: 10.1111/j.1463-1318.2012.03104.x. [DOI] [PubMed] [Google Scholar]
- 7.Champaneria R, Shah L, Geoghegan J, Gupta JK, Daniels JP. Analgesic effectiveness of transversus abdominis plane blocks after hysterectomy: A meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2013;166:1–9. doi: 10.1016/j.ejogrb.2012.09.012. [DOI] [PubMed] [Google Scholar]
- 8.Elkassabany N, Ahmed M, Malkowicz SB, Heitjan DF, Isserman JA, Ochroch EA. Comparison between the analgesic efficacy of transversus abdominis plane (TAP) block and placebo in open retropubic radical prostatectomy: A prospective, randomized, double-blinded study. J Clin Anesth. 2013;25:459–65. doi: 10.1016/j.jclinane.2013.04.009. [DOI] [PubMed] [Google Scholar]
- 9.Keller DS, Ermlich BO, Schiltz N, Champagne BJ, Reynolds HL, Jr, Stein SL, et al. The effect of transversus abdominis plane blocks on postoperative pain in laparoscopic colorectal surgery: A prospective, randomized, double-blind trial. Dis Colon Rectum. 2014;57:1290–7. doi: 10.1097/DCR.0000000000000211. [DOI] [PubMed] [Google Scholar]
- 10.De Oliveira GS, Jr, Castro-Alves LJ, Nader A, Kendall MC, McCarthy RJ. Transversus abdominis plane block to ameliorate postoperative pain outcomes after laparoscopic surgery: A meta-analysis of randomized controlled trials. Anesth Analg. 2014;118:454–63. doi: 10.1213/ANE.0000000000000066. [DOI] [PubMed] [Google Scholar]
- 11.Gupta NP, Kumar A. Analgesia for pain control during extracorporeal shock wave lithotripsy: Current status. Indian J Urol. 2008;24:155–8. doi: 10.4103/0970-1591.40607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Elnabtity AM, Tawfeek MM, Keera AA, Badran YA. Is unilateral transversus abdominis plane block an analgesic alternative for ureteric shock wave lithotripsy? Anesth Essays Res. 2015;9:51–6. doi: 10.4103/0259-1162.150177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kamper SJ, Maher CG, Mackay G. Global rating of change scales: A review of strengths and weaknesses and considerations for design. J Man Manip Ther. 2009;17:163–70. doi: 10.1179/jmt.2009.17.3.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McDonnell JG, O’Donnell BD, Farrell T, Gough N, Tuite D, Power C, et al. Transversus abdominis plane block: A cadaveric and radiological evaluation. Reg Anesth Pain Med. 2007;32:399–404. doi: 10.1016/j.rapm.2007.03.011. [DOI] [PubMed] [Google Scholar]
- 15.Tran TM, Ivanusic JJ, Hebbard P, Barrington MJ. Determination of spread of injectate after ultrasound-guided transversus abdominis plane block: A cadaveric study. Br J Anaesth. 2009;102:123–7. doi: 10.1093/bja/aen344. [DOI] [PubMed] [Google Scholar]


