Abstract
Persistent Müllerian duct syndrome (PMDS) is a condition in which a 46, XY male displays masculine external genitalia, but internally retains developed Müllerian duct structures (uterus, fallopian tubes, and upper two-thirds vagina). Thoughtful operative consideration is needed to maximize the therapeutic benefit while minimizing the risk of hypogonadism, infertility, and erectile dysfunction. We report a 53-year-old male with a pelvic mass incidentally discovered on routine ultrasound, intra-operatively discovered to be PMDS.
PMDS is a rare condition that may present late in life. The primary operative consideration is performing orchiopexy for cancer surveillance or orchiectomy if orchiopexy is not possible. Additional considerations include surveillance and counseling of infertility, hypogonadism, and assessment of the potential need for involvement of psychiatry. Removal of Müllerian remnants is a subject to debate. If possible, discuss with the patient their risks and options in the preoperative setting to guide operative planning.
Keywords: Infertility, Müllerian, persistent Müllerian duct syndrome
INTRODUCTION
Persistent Müllerian duct syndrome (PMDS) is a condition in which a karyotypic male (46, XY) displays masculine external genitalia, but internally retains developed Müllerian duct structures.[1] It is a rare condition (<1 in 200,000) initially described by Nilson in 1939.[2]
Thoughtful operative planning of patients with PMDS is paramount as operative intervention may affect fertility, erectile function, cancer surveillance, and mental health. We report a 53-year-old male with an incidentally discovered, late-presenting diagnosis of PMDS focusing on the operative decision-making.
CASE REPORT
A 53-year-old dark-skinned male, who has provided consent for his case to be published, presented to establish care with nephrology for reported chronic kidney disease and hypertension. Baseline renal and bladder ultrasound were obtained and revealed a large pelvic mass for which he was referred to urology.
The patient denied any systemic symptoms. His only urologic complaint was erectile dysfunction that responded well to phosphodiesterase inhibitors (PDEIs). At an outside institution 10 years ago, he underwent right orchiectomy and left orchiopexy for bilateral undescended testicles. However, the patient's path report read “connective tissue without atypia” without mention of a testicle.
Genitourinary examination was consistent with a virilized male [Figure 1a]. Pertinent findings included an empty scrotal sac, bilateral inguinal scars, a small palpable gonad in the distal left inguinal canal, and a 20cc smooth prostate gland.
Figure 1.
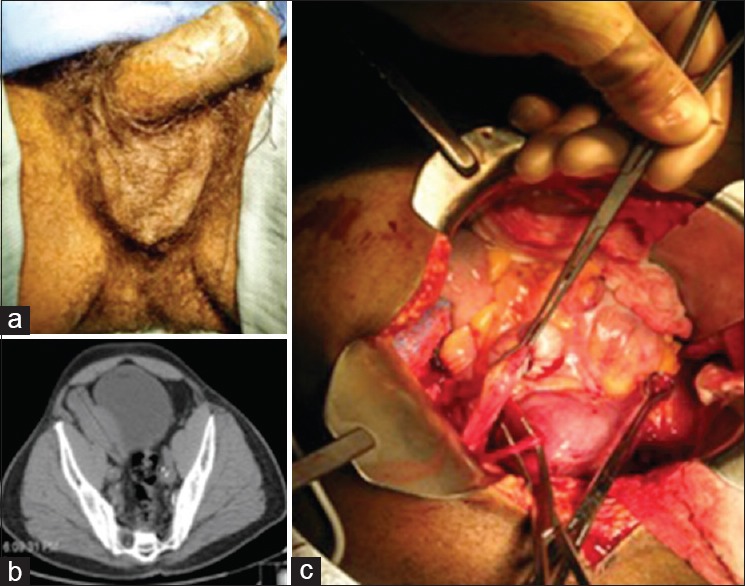
(a) Phenotypic androgenized male genitalia with empty scrotal sac; (b) noncontrast computed tomography scan of pelvic mass; (c) intra-operative photo of persistent Müllerian duct structures: surgeon hand holding right fallopian tube adjacent to right testicle, right-angle beneath right vas deferens, unheld Babcock holding left fallopian tube
Noncontrast computed tomography of the abdomen and pelvis revealed an 11 cm complex pelvic mass that appeared to originate near the right seminal vesicle [Figure 1b]. Given, the unclear history of the right orchiectomy, testicular malignancy was of significant concern. Chest X-ray and serum testicular tumor markers were normal.
We discussed with the patient that we still lacked a definitive diagnosis and could not yet determine the malignant potential of the radiologic finding. Because of a recent divorce and separation from his daughter, he was homeless but currently residing in a nearby mission. Given his unsteady social situation, all involved parties felt it best to proceed with exploratory surgery.
Intra-operatively, a uterus was discovered with the evidence of a gonad situated near the right fallopian tube [Figure 1c]. The right gonad was removed due to inadequate vascular length to bring it to the scrotum. Because the pelvic mass was the primary source of his anxiety, gynecology was consulted intra-operatively for assistance with resection of the Müllerian structures, taking particular care not to disturb the blood flow to the remaining left gonad. Given his good preoperative erectile function on PDEIs, the dissection was carried just short of the prostate.
Final pathology confirmed that the right gonad was indeed the right testicle with an attached vas deferens, and the remaining organs were consistent with bilateral fallopian tubes and uterus with fibroids. A karyotype was sent revealing 46, XY.
DISCUSSION
Over the past 50 years, about 200 cases of PMDS have been reported.[3] Most often, these phenotypic and genotypic males present with unilateral or bilateral undescended testes.[1,4] Surgical repair of the undescended testicle often leads to the incidental discovery of the Müllerian structures.
The anatomic findings of PMDS are likely the result of errors in the production or signaling of MIS – a substance that serves to regress the Müllerian structures during normal male development.[5,6] To make the diagnosis of PMDS, a karyotype is required. Other disorders of sexual differentiation may present anatomically similar but with a different karyotype, particularly mixed gonadal dysgenesis.[7]
Because affected patients are male regarding karyotype and external reproductive anatomy, the treatment goal is essentially orchiopexy.[1,3,4,7,8] Unlike patients with testicular dysgenesis, patients with PMDS do not appear to harbor a heightened risk of gonadoblastoma. They do however have a heightened risk (~18%) for testicular malignancy related to their cryptorchidism, most often seminoma.[3,7] For this reason, the primary goal of the surgery is to bring the testicle to a position capable of surveillance, or remove it if this is not possible.
Historic recommendations endorse preservation of the Müllerian structures to minimize the risk of infertility associated with damaging the vas which lies in close proximity to the uterus and vagina in PMDS patients.[1,8] Although a vast majority of PMDS patients are infertile, fertility has been reported in at least five cases.[7] Even in infertile patients; however, retaining the Müllerian structures is also believed to minimize the risk of losing the deferential blood supply to the testicle, an important vascular contributor to testicular viability in patients undergoing an orchiopexy.
The recommendation to not remove the Müllerian structures came before reports of gynecologic malignancy in the retained remnants. In more recent articles; however, there have been 11 case reports of PMDS patients developing malignancies in Müllerian remnants.[3] Three of these resulted in metastatic spread, and it is estimated that 3–8% of PMDS patients would develop malignancy in retained Müllerian structures.[3] Counseling the patient on potential risks of infertility as well as gynecologic malignancy is important. It is also important to be mindful that, although unlikely, PMDS patients have been reported to be fertile in the past, indicating an impossibility to conceive may result in an unnecessary emotional strain for the patient, particularly one with offspring.
Postoperatively, our patient recovered well. After discussing his pathology, we offered a psychiatry evaluation to assess any outpatient needs, but he declined. His outpatient course will include testosterone checks and self-examinations on his remaining left testicle. We discussed that he may be infertile, and it would be difficult to tell if his infertility were due to the operation or the PMDS without paternity testing of his daughter. He declined such testing and was not planning on additional children.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Diamond DA, Yu RN. 10th ed. Philadelphia, PA, USA: Elsevier Inc; 2012. Sexual Differentiation: Normal and Abnormal. Campbell-Walsh Urology; p. 32690. [Google Scholar]
- 2.Nilson O. Hernia uteri inguinalis beim Manne. Acta Chir Scand. 1939;83:231. [Google Scholar]
- 3.Farikullah J, Ehtisham S, Nappo S, Patel L, Hennayake S. Persistent Müllerian duct syndrome: Lessons learned from managing a series of eight patients over a 10-year period and review of literature regarding malignant risk from the Müllerian remnants. BJU Int. 2012;110(11 Pt C):E1084–9. doi: 10.1111/j.1464-410X.2012.11184.x. [DOI] [PubMed] [Google Scholar]
- 4.Sherwani AY, Shah AQ, Wani AM, Bashir AC, Bashir AK, Sofi FA, et al. Hysterectomy in a male?. A rare case report. Int J Surg Case Rep. 2014;5:1285–7. doi: 10.1016/j.ijscr.2014.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.MacLaughlin DT, Donahoe PK. Sex determination and differentiation. N Engl J Med. 2004;350:367–78. doi: 10.1056/NEJMra022784. [DOI] [PubMed] [Google Scholar]
- 6.Prakash N, Khurana A, Narula B. Persistent Müllerian duct syndrome. Indian J Pathol Microbiol. 2009;52:546–8. doi: 10.4103/0377-4929.56160. [DOI] [PubMed] [Google Scholar]
- 7.Alp BF, Demirer Z, Güragaç A, Babacan O, Sari E, Sari S, et al. Persistent Mullerian duct syndrome with transverse testicular ectopia and seminoma. Int Urol Nephrol. 2014;46:1557–62. doi: 10.1007/s11255-014-0667-4. [DOI] [PubMed] [Google Scholar]
- 8.Vandersteen DR, Chaumeton AK, Ireland K, Tank ES. Surgical management of persistent müllerian duct syndrome. Urology. 1997;49:941–5. doi: 10.1016/s0090-4295(97)00104-0. [DOI] [PubMed] [Google Scholar]


