Abstract
Objective
University students with influenza-like illness (ILI) were assessed to determine whether symptom severity, duration, or missed days of school or work varied according to etiology.
Participants
Sixty persons presenting to a university health clinic with ILI symptoms during 3 consecutive influenza seasons completed baseline survey and viral testing; 51 (85%) completed follow-up.
Methods
Influenza viral culture and polymerase chain reaction and respiratory virus immunofluorescence assay testing were performed. Information collected at baseline and follow-up included symptom occurrence, severity, duration, and numbers of days of work and school missed.
Results
Influenza virus was confirmed in 63% of participants. Influenza-positive individuals were no more likely to report any symptom or miss more days of school or work. Self-reported severity and durations of symptoms were similar between groups.
Conclusions
Students with influenza-associated ILI were similar to those with noninfluenza ILI with respect to severity, duration, and numbers of days of school and work missed.
Keywords: clinical medicine, health education, influenza (human), adolescent medicine
Acute community acquired upper respiratory infections (URIs) are a major cause of morbidity in college and university students.1 URI episodes include both colds, characterized by upper respiratory symptoms without fever, and influenza-like illness (ILI). ILI is characterized by a fever of 100°F (37.8°C) or greater plus cough. ILI has been shown to have a greater impact on school and work performance than colds in this population.1 Nevertheless, the amount of ILI that is associated with influenza virus infection as opposed to other respiratory viruses among college and university students is not well characterized.1 Influenza virus infection is estimated to account for 30% of acute viral respiratory illnesses and up to 79% of illnesses with fever and cough in healthy adults,2–4 although there is no single, accurate clinical case definition predictive of influenza virus infection.2,5–9 Influenza virus is a common etiology of ILI in adults, but studies indicate that other etiologies of ILI may have health outcomes comparable to those attributed to influenza.2,3,9 It is possible that the role of influenza virus infection as the cause of ILI may be overestimated and the role of other viruses, such as rhinovirus, underestimated.3,5,10
Public health prevention efforts have tended to focus on influenza as a cause of acute respiratory illness, particularly during likely transmission seasons, because of influenza’s potential for high morbidity and excess mortality in vulnerable populations. In contrast, public health efforts targeting other types of respiratory infections are relatively ignored. Recently, the economic costs of ILI have received attention in terms of lost productivity and benefits of influenza vaccination among healthy adult populations using health outcomes such as missed work or cost indices.11 Improved understanding of the role of influenza virus infection in ILI in different populations could guide both public policy and individual diagnostic and treatment recommendations. Furthermore, understanding the nature of seasonal influenza in subpopulations may be very important in light of the recent emergence of pandemic 2009 H1N1.
Here, we evaluate influenza-related ILI as compared to noninfluenza ILI among 18- to 24-year-olds. We are not aware of previous studies that investigate ILI based on etiology in the university setting. Specifically, we sought to determine if symptom occurrence, symptom severity, symptom duration, and the number of days of missed school and work differed among those who were positive for influenza virus and those with other types of ILI.
METHODS
The data presented were derived from a prospective study of influenza immunology. Participants were recruited from the University of Pittsburgh Student Health Service during the active flu seasons of 2006–2007, 2007–2008, and 2008–2009. Eligible subjects were patients presenting with ILI symptoms, defined by fever greater than 100°F (37.8°C) and cough during the previous week; were over 18 years of age, able to provide adequate blood samples; and were not pregnant or immunocompromised. Clinicians notified the research assistant when an eligible patient was seen. We estimate that approximately 70% of all patients presenting with ILI during these weeks were informed of the study and about 50% of the total were recruited. Participants 25 years of age and older were excluded from the current analysis. Nasopharyngeal swabs were obtained from each participant for viral influenza culture, influenza polymerase chain reaction (PCR), and indirect immunoflourescence assay (IFA) testing for adenovirus, parainfluenza 1–3, and respiratory syncytial virus. Influenza infection was defined as having a positive culture, a positive PCR result, or both. Treatment decisions at the time of enrollment were left to the participant’s medical provider. This study was approved by the Institutional Review Board of the University of Pittsburgh. It should be noted that enrollment of new subjects ended approximately 1 month prior to the emergence of H1N1 2009 in April 2009.
All participants provided written informed consent. Subjects completed a baseline questionnaire ascertaining age, gender, race and ethnicity, smoking status, receipt of influenza vaccination, school and work attendance, prescriptions given, the occurrence of symptoms, and the duration and severity of each symptom experienced. Specifically, subjects were asked whether they had experienced the following symptoms within the past week: fever, cough, runny nose/congestion, sore throat, myalgia, feel weak all over, decreased activity, irritability, vomiting, diarrhea, and headache. Subjects self-reported the severity of each symptom experienced on a scale of 1 (mild) to 10 (severe) and reported the duration (in days) of each symptom experienced. The survey was pilot tested by students at the health center and modified to ensure that terms were understandable in the target population. No validated measure of symptoms or symptom severity has been used for ILI. Therefore, the symptom measures used here were chosen to be consistent with symptoms used in prior studies of influenza symptomatology with regards to clinical diagnosis of influenza.4,8,12,13
Participants were contacted 2 weeks after the initial visit and baseline survey and asked to complete a follow-up survey. At this time, individuals reported the total duration in days of each symptom experienced, the maximum severity of each symptom experienced, and the total number of days of school and work missed as a result of the ILI episode. The survey did not capture whether weekends or holidays occurred during the illness and so could not be accounted for in the analysis.
Associations between symptom occurrence at baseline and influenza status were measured using χ2 or Fisher’s exact test. The means of symptom severities at baseline, the mean duration of each symptom, and the mean number of days of school and work missed as reported on the follow-up survey were compared between influenza-positive and influenza-negative groups using t tests. All analyses were performed using SAS version 9.1 (Cary, NC).
RESULTS
A total of 60 participants between the ages of 18 and 24 years of age completed the baseline questionnaire and viral testing. Of these, 51 (85%) completed the follow-up questionnaire. The age, gender, and ethnicity of the group at baseline are summarized in Table 1 as well as employment, student, and smoking status. A positive influenza viral culture and/or PCR was obtained from 38 (63.3%) individuals. Of the influenza-positive samples, 31 (81%) were positive for influenza A and 7 (18%) for influenza B. Participants who completed the follow-up survey did not differ from the baseline with respect to gender, ethnicity, student status, employment status, smoking, or age (Table 1). Individuals who completed the follow-up were more likely to be positive for influenza (p = .006). Influenza virus infection was not associated with age, gender, ethnicity, smoking status, being employed, or a being a student. Two participants reported having received a seasonal influenza vaccine in the same season in which they became ill, and one of these was influenza positive. No samples were positive for respiratory syncytial virus, parainfluenza 1, 2, or 3, or adenovirus by indirect immunoflourescence assay testing.
TABLE 1.
Characteristics of Influenza-Positive and -Negative Participants at Baseline
| Variable | Mean | All participants (n = 60)
|
Influenza negative (n = 22, 36.7%)
|
Influenza positive* (n = 38, 63.3%)
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 95% CI | N | % | Mean | 95% CI | N | % | Mean | 95% CI | N | % | p value | ||
| Age in years | 20.1 | 19.7–20.4 | 20.3 | 19.6–21.0 | 20.0 | 19.6–20.4 | .36 | ||||||
| Female gender | 30 | 50.00 | 12 | 54.60 | |||||||||
| Ethnicity | .75 | ||||||||||||
| Black | 6 | 10.00 | 3 | 13.60 | 3 | 7.9 | |||||||
| White | 49 | 81.70 | 17 | 77.30 | 32 | 84.2 | |||||||
| Asian | 5 | 8.33 | 2 | 9.09 | 3 | 7.9 | |||||||
| Employed | 26 | 43.30 | 7 | 31.80 | 19 | 50.0 | .17 | ||||||
| Smoker | 8 | 13.30 | 2 | 9.10 | 6 | 15.8 | .70 | ||||||
Influenza positive defined as positive viral culture, positive PCR, or both.
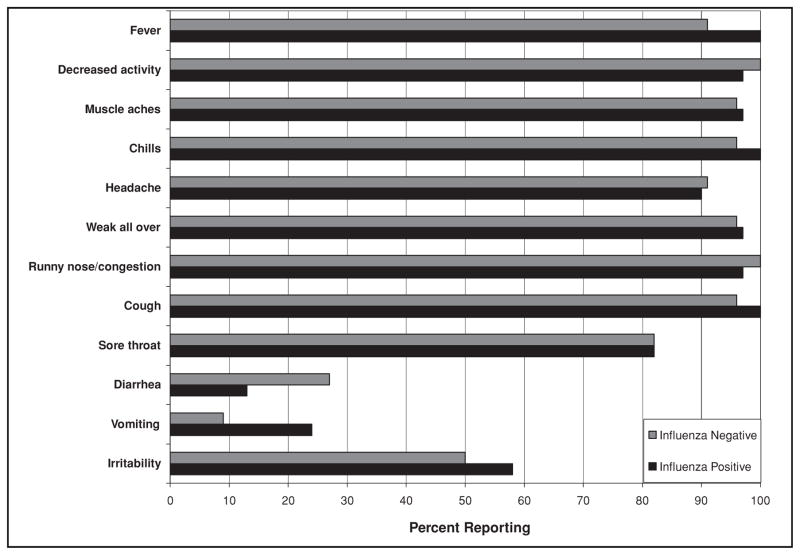
No single symptom occurrence was associated with being positive for influenza at baseline (Figure 1). The most common symptoms reported by all participants at baseline, other than cough and fever, were chills, decreased activity, and runny nose/congestion. Influenza-positive and influenza-negative groups had similar durations of symptoms at presentation. Overall, influenza-positive and influenza-negative participants reported experiencing similar severities of symptoms at their initial presentation to their health care provider (Table 2). Only the severity of irritability was different between groups, with influenza-positive subjects reporting higher levels of irritability (flu-positive mean severity 5.68 [95% confidence interval, CI 4.97–6.40] and flu-negative mean 3.91 [95% CI 3.09–4.73]; p = .002).
FIGURE 1.
Percent of influenza-positive (n = 38) and influenza-negative (n = 22) participants reporting symptoms. Influenza positive defined as positive viral culture, positive PCR, or both.
TABLE 2.
Mean Severity of ILI Symptoms at Baseline and Mean Duration in Days of Symptoms, Missed Work, and Missed School at Follow-Up as Reported by Participants at Baseline
| Symptom | Severity at baseline
|
Duration in days at follow-up
|
||||||
|---|---|---|---|---|---|---|---|---|
| Influenza positive (n = 38)
|
Influenza negative (n = 22)
|
Influenza positive (n = 36)
|
Influenza negative (n = 15)
|
|||||
| Mean | 95% CI | Mean | 95% CI | Mean | 95% CI | Mean | 95% CI | |
| Fever | 7.95 | 7.01–8.89 | 7.55 | 6.97–8.14 | 3.53 | 2.60–4.45 | 4.45 | 2.60–6.48 |
| Decreased activity | 7.19 | 6.06–8.32 | 7.27 | 6.57–7.97 | 5.79 | 3.79–7.80 | 6.71 | 4.92–8.50 |
| Muscle aches | 6.90 | 6.10–7.70 | 6.73 | 6.08–7.38 | 5.09 | 3.11–7.06 | 6.38 | 4.21–8.56 |
| Chills | 6.86 | 5.86–7.86 | 7.11 | 6.49–7.72 | 3.94 | 2.27–5.62 | 4.36 | 2.58–6.18 |
| Headache | 6.80 | 5.83–7.66 | 6.09 | 5.33–6.85 | 5.39 | 3.27–7.50 | 6.92 | 4.66–9.19 |
| Weak all over | 6.71 | 5.91–7.52 | 7.70 | 7.19–8.22 | 4.86 | 3.40–6.32 | 5.61 | 3.40–7.83 |
| Runny nose/Congestion | 6.57 | 4.52–6.57 | 5.89 | 5.11–6.67 | 7.34 | 5.41–9.27 | 7.13 | 5.69–9.27 |
| Cough | 6.19 | 5.30–7.09 | 6.92 | 6.24–7.60 | 7.61 | 5.53–9.69 | 9.14 | 7.31–10.98 |
| Sour throat | 5.48 | 4.47–6.97 | 5.48 | 4.66–6.31 | 5.07 | 2.89–7.23 | 6.42 | 4.59–8.24 |
| Diarrhea | 4.50 | 3.93–5.07 | 5.40 | 3.98–6.82 | 2.33 | 1.25–3.42 | 6.00 | 0.05–11.96 |
| Vomiting | 4.00 | −8.71–16.71 | 5.00 | 2.93–7.07 | 1.78 | 1.03–2.52 | 6.00 | N/A** |
| Irritability* | 3.91 | 3.09–4.73 | 5.68 | 4.97–6.40 | 5.25 | 3.47–7.03 | 6.25 | 3.73–8.77 |
| Days of school missed | N/A | N/A | 3.06 | 2.19–3.92 | 3.00 | 1.77–4.23 | ||
| Days of work missed | N/A | N/A | 1.89 | 1.28–2.50 | 1.80 | 0.76–2.84 | ||
Note. Influenza positive defined as positive viral culture, positive PCR, or both. Severity is measured on a scale of 1 (least severe) to 10 (most severe).
p = .002 for severity.
One participant reporting vomiting.
The mean durations of symptoms reported at follow-up were similar for both the influenza-positive and influenza-negative groups (Table 2). The difference in duration was only significant for vomiting (p = .0003), although it should be noted that only 1 influenza-negative participant reported vomiting. Influenza-positive students missed a mean of 3.06 (95% CI 2.19–3.92) days of school as compared to 3.00 (95% CI 1.77–4.23) days for students who tested negative, and this difference was not significant (p = .94). Among those who reported being employed, influenza-positive and -negative employees missed means of 1.89 (95% CI 1.28–2.50) and 1.80 (95% CI 0.76–2.84) days of work, respectively (p = .85).
COMMENT
The findings suggest that infections with agents other than influenza are similar to influenza in terms of their contribution to ILI-related outcomes among college and university students. Influenza and noninfluenza etiologies of ILI resulted in a similar number of missed days of school and work among our cohort of college-aged individuals. Additionally, students positive for influenza had similar symptoms, symptom severity, and symptom durations as those who were influenza negative. The one exception to our symptom comparisons was that irritability was more common in persons with influenza. Therefore, assessment of irritability may be helpful for clinicians who are attempting to identify influenza, although this finding should be confirmed in additional studies.
Nichol et al. compared missed school and work in university students with URIs and ILIs.1 In their study, ILI episodes were associated with a greater number of days of school and work missed than were URIs; specifically, students with ILI reported a mean of 0.77–1.01 days of missed work and a mean of 1.24–1.74 days of missed school, as compared to 0.24–0.34 days of missed work and 0.43–0.56 days of missed school reported by those with URIs.1 The longer length of absenteeism in the present study may be explained by influenza strain, timing of illness, or the use of self-reported ILI in the previous work versus laboratory confirmed influenza as measured here. In a recent systematic review, Keech and Beardsworth found that adults with ILI symptoms and laboratory confirmed influenza virus infection missed between 1.5 and 4.9 days of work per episode, which is consistent with the current data.14
We identified few studies that tested for multiple respiratory pathogens in individuals with ILI, as opposed to the broader category of URI, using current diagnostic techniques.5,6,9 A study of viral etiology of ILI in healthy adults showed that influenza was detected via PCR in 30.9% of ILI cases and rhinovirus in 19.6%; most (86.9%) of the influenza-positive patients had ILI symptoms.5 An additional study of viral etiology of URI (including, but not limited to, ILI) identified influenza virus infection with PCR in 38% of individuals.6 Our current study suggests that pathogens other than influenza contribute to ILI and, furthermore, suggests that this holds true in the university student population. Additional studies are needed to confirm this finding.
Influenza positivity was defined as a positive result on either culture or PCR. Culture has long been considered the laboratory standard, but there is evidence that PCR may have increased sensitivity for diagnosis of influenza and correlates well with serologic testing.6,15,16 PCR- and culture-positive results have been shown to be positively correlated with length and severity of illness in ILI patients,15 although measures of severity have not been consistent across studies.4,7,8 We found no significant differences in the duration of reported symptoms at baseline and therefore we do not expect test results to have been influenced by length of illness at the time of testing.
The lack of significant differences between influenza-positive and -negative groups in the study has implications for evaluations of vaccine effectiveness among healthy young adults. Vaccine effectiveness studies typically use clinical case definitions of influenza or absenteeism to measure effectiveness and cost benefits of vaccination. Typically, these studies estimate the proportion of individuals with ILI who are likely to actually be infected with influenza as anywhere from 30% to 70%.3,4,6,11,17–26 The accuracy of estimates of true influenza infection depends on whether there is an active influenza outbreak and the clinical definition used.8 During the 3 combined active influenza seasons in this study, 63% of persons presenting with ILI were positive for influenza. The proportion of influenza-positive subjects found here is within the range of previous estimates, and indicates that these estimates can apply to the university student population.
Nevertheless, the approximately 37% of individuals with ILI who were negative for influenza missed similar numbers of days of school and work as those who were positive. In addition, influenza-negative individuals reported experiencing similar symptoms as those who were positive, as well as similar durations of symptoms. The finding that severity of irritability was higher in influenza-positive students indicates that this symptom may be of some clinical usefulness for predicting influenza virus infection in this population. If this proportion of ILI associated with influenza virus infection holds true across populations, and individuals with noninfluenza ILI are experiencing similar outcomes as those with influenza, then investigation into the etiology of noninfluenza ILI is warranted. Also, public health messages aimed at healthy young adults should stress the importance of prevention of all respiratory viruses, not only influenza.
Limitations
Although this study suggests that ILI resulting from non-influenza infections is significant in college and university students, the limitations should be addressed. The relatively small sample size of 60 participants at baseline and 51 at follow-up provides limited power to detect differences between groups and therefore we may not have detected smaller differences in symptom prevalence in persons with influenza versus other etiologies. Influenza outbreaks, as measured by peak influenza activity, were only present for 2 to 3 weeks of each year, thus limiting the number of eligible participants. To our knowledge, however, this is the first report comparing the outcomes of missed school and work among college students with ILI who were tested for influenza and other respiratory viruses.
Measures of symptom severity are limited by the use of self-report, although we are not aware of a validated measure of symptom severity for ILI. The generalizability of this study is somewhat limited by the sampling of only 1 site; however, sampling across 3 transmission seasons allows for some variation in influenza virus strains.
Conclusions
To our knowledge this is the first investigation to compare severity and duration of symptoms and missed school and work for various etiologies of ILI in college students. Overall, university students with ILI due to influenza virus infections did not differ substantially from those with non–influenza-related ILI with respect to symptom occurrence or duration, missed work, or missed school. The one exception to our symptom comparisons was that irritability was more common in persons with influenza. Therefore, assessment of irritability may be helpful for clinicians who are attempting to identify influenza, although this finding should be confirmed in additional studies. Future studies should attempt to determine the specific etiology of noninfluenza ILI so that clinical and prevention strategies can be developed and targeted for these illnesses.
Contributor Information
Dr. Jocelyn Mullins, Department of Epidemiology and Biostatistics at the University of Florida in Gainesville, Florida.
Dr. Robert Cook, Department of Epidemiology and Biostatistics at the University of Florida in Gainesville, Florida.
Dr. Charles Rinaldo, Department of Infectious Diseases and Microbiology at the University of Pittsburgh Graduate School of Public Health in Pittsburgh, Pennsylvania.
Dr. Eric Yablonsky, Department of General Internal Medicine at the University of Pittsburgh School of Medicine in Pittsburgh, Pennsylvania.
Dr. Rachel Hess, Department of General Internal Medicine at the University of Pittsburgh School of Medicine in Pittsburgh, Pennsylvania.
Dr. Paolo Piazza, Department of Infectious Diseases and Microbiology at the University of Pittsburgh Graduate School of Public Health in Pittsburgh, Pennsylvania.
References
- 1.Nichol KL, D’Heilly S, Ehlinger E. Colds and influenza-like illnesses in university students: impact on health, academic and work performance, and health care use. Clin Infect Dis. 2005;40:1263–1270. doi: 10.1086/429237. [DOI] [PubMed] [Google Scholar]
- 2.Monto AS. Epidemiology of viral respiratory infections. Am J Med. 2002;112(suppl 6A):4S–12S. doi: 10.1016/s0002-9343(01)01058-0. [DOI] [PubMed] [Google Scholar]
- 3.Nichol KL, D’Heilly S, Ehlinger EP. Influenza vaccination among college and university students: impact on influenzalike illness, health care use, and impaired school performance. Arch Pediatr Adolesc Med. 2008;162:1113–1118. doi: 10.1001/archpedi.162.12.1113. [DOI] [PubMed] [Google Scholar]
- 4.Boivin G, Hardy I, Tellier G, Maziade J. Predicting influenza infections during epidemics with use of a clinical case definition. Clin Infect Dis. 2000;31:1166–1169. doi: 10.1086/317425. [DOI] [PubMed] [Google Scholar]
- 5.Bellei N, Carraro E, Perosa A, Watanabe A, Arruda E, Granato C. Acute respiratory infection and influenza-like illness viral etiologies in Brazilian adults. J Med Virol. 2008;80:1824–1827. doi: 10.1002/jmv.21295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Louie JK, Hacker JK, Gonzales R, et al. Characterization of viral agents causing acute respiratory infection in a San Francisco University Medical Center Clinic during the influenza season. Clin Infect Dis. 2005;41:822–828. doi: 10.1086/432800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Navarro-Mari JM, Perez-Ruiz M, Cantudo-Munoz P, Petit-Gancedo C, Jimenez-Valera M, Rosa-Fraile M. Influenza-like illness criteria were poorly related to laboratory-confirmed influenza in a sentinel surveillance study. J Clin Epidemiol. 2005;58:275–279. doi: 10.1016/j.jclinepi.2004.08.014. [DOI] [PubMed] [Google Scholar]
- 8.Nichol KL, Mendelman P. Influence of clinical case definitions with differing levels of sensitivity and specificity on estimates of the relative and absolute health benefits of influenza vaccination among healthy working adults and implications for economic analyses. Virus Res. 2004;103:3–8. doi: 10.1016/j.virusres.2004.02.005. [DOI] [PubMed] [Google Scholar]
- 9.Santamaria C, Uruena A, Videla C, et al. Epidemiological study of influenza virus infections in young adult outpatients from Buenos Aires, Argentina. Influenza Other Respi Viruses. 2008;2:131–134. doi: 10.1111/j.1750-2659.2008.00048.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Monto AS. Viral respiratory infections in the community: epidemiology, agents, and interventions. Am J Med. 1995;99:24S–27S. doi: 10.1016/S0002-9343(99)80307-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kumpulainen V, Makela M. Influenza vaccination among healthy employees: a cost-benefit analysis. Scand J Infect Dis. 1997;29:181–185. doi: 10.3109/00365549709035881. [DOI] [PubMed] [Google Scholar]
- 12.Stein J, Louie J, Flanders S, et al. Performance characteristics of clinical diagnosis, a clinical decision rule, and a rapid influenza test in the detection of influenza infection in a community sample of adults. Ann Emerg Med. 2005;46:412–419. doi: 10.1016/j.annemergmed.2005.05.020. [DOI] [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention. [Accessed December 13, 2005];clinical description and diagnosis. Available at: http://www.cdc.gov/flu/professionals/diagnosis/index.htm. Published 2005.
- 14.Keech M, Beardsworth P. The impact of influenza on working days lost: a review of the literature. Pharmacoenomomics. 2008;26:911–924. doi: 10.2165/00019053-200826110-00004. [DOI] [PubMed] [Google Scholar]
- 15.Zambon M, Hayes J, Webster A, Newman R, Keene O. Diagnosis of Influenza in the community. Arch Intern Med. 2001;161:2116–2122. doi: 10.1001/archinte.161.17.2116. [DOI] [PubMed] [Google Scholar]
- 16.Ruest A, Michaud S, Deslandes S, Frost E. Comparison of the Directigen Flu A+B test, the QuickVue influenza test, and clinical case definition to viral culture and reversetranscription-PCR for rapid diagnosis of influenza virus infection. J Clin Microbiol. 2003;41:3487–3493. doi: 10.1128/JCM.41.8.3487-3493.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bridges CB, Thompson WW, Meltzer MI, et al. Effectiveness and cost-benefit of influenza vaccination of healthy working adults: a randomized controlled trial. JAMA. 2000;284:1655–1663. doi: 10.1001/jama.284.13.1655. [DOI] [PubMed] [Google Scholar]
- 18.Lee PY, Matchar DB, Clements DA, Huber J, Hamilton JD, Peterson ED. Economic analysis of influenza vaccination and antiviral treatment for healthy working adults. Ann Intern Med. 2002;137:225–231. doi: 10.7326/0003-4819-137-4-200208200-00005. [DOI] [PubMed] [Google Scholar]
- 19.Muennig PA, Khan K. Cost-effectiveness of vaccination versus treatment of influenza in healthy adolescents and adults. Clin Infect Dis. 2001;33:1879–1885. doi: 10.1086/324491. [DOI] [PubMed] [Google Scholar]
- 20.Nichol KL. Clinical effectiveness and cost effectiveness of influenza vaccination among healthy working adults. Vaccine. 1999;17(suppl 1):S67–S73. doi: 10.1016/s0264-410x(99)00110-3. [DOI] [PubMed] [Google Scholar]
- 21.Nichol KL. Cost-benefit analysis of a strategy to vaccinate healthy working adults against influenza. Arch Intern Med. 2001;161:749–759. doi: 10.1001/archinte.161.5.749. [DOI] [PubMed] [Google Scholar]
- 22.Nichol KL. Influenza vaccine for healthy working adults. JAMA. 2001;285:290. author reply 292. [PubMed] [Google Scholar]
- 23.Nichol KL. The efficacy, effectiveness and cost-effectiveness of inactivated influenza virus vaccines. Vaccine. 2003;21:1769–1775. doi: 10.1016/s0264-410x(03)00070-7. [DOI] [PubMed] [Google Scholar]
- 24.Nichol KL, Mallon KP, Mendelman PM. Cost benefit of influenza vaccination in healthy, working adults: an economic analysis based on the results of a clinical trial of trivalent live attenuated influenza virus vaccine. Vaccine. 2003;21:2207–2217. doi: 10.1016/s0264-410x(03)00029-x. [DOI] [PubMed] [Google Scholar]
- 25.Rothberg MB, Rose DN. Vaccination versus treatment of influenza in working adults: a cost-effectiveness analysis. Am J Med. 2005;118:68–77. doi: 10.1016/j.amjmed.2004.03.044. [DOI] [PubMed] [Google Scholar]
- 26.Nichol KL, Lind A, Margolis KL, et al. The effectiveness of vaccination against influenza in healthy, working adults. N Engl J Med. 1995;333:889–893. doi: 10.1056/NEJM199510053331401. [DOI] [PubMed] [Google Scholar]