Abstract
Purpose
This study evaluated spatial access to mammography centers in Appalachia using both traditional access measures and the two-step floating catchment area (2SFCA) method.
Methods
Ratios of county mammography centers to women age 45 and older, driving time to nearest mammography facility, and various 2SFCA approaches were compared throughout Pennsylvania, Ohio, Kentucky, and North Carolina.
Results
Closest travel time measures favored urban areas. The 2SFCA method produced varied results depending on the parameters chosen. Appalachia areas had greater travel times to their closest mammography center. Appalachia areas in OH and NC had worse 2SFCA scores than non-Appalachia areas of the same states.
Conclusion
A relative 2SFCA approach, the spatial access ratio (SPAR) method, was recommended because it helped minimize the differences between various 2SFCA approaches.
1. Introduction
The Appalachia region of the U.S. spans a 13 state region from Alabama to New York. The region has been designated as a special population of interest by the National Cancer Institute because of disparities in cancer outcomes and treatment patterns (Lane et al., 2012; Lengerich et al., 2005). An example of these disparities are higher mortality rates for lung and bronchus, colon, and cervical cancer (Blackley, Behringer, & Zheng, 2012); reduced mammography screening (Bhanegaonkar et al., 2012); and lower rates of breast conserving surgery, rather than mastectomy (Freeman, Huang, & Dragun, 2012). Human population in Appalachia is sparse, with 42 percent of the population classified as rural, as compared to a national average of 20 percent (ARC, 2014). The region also has a lower per capita income and a higher poverty rate than the national average (Pollard & Jacobson, 2014). Because of Appalachia’s rural population, distressed economic indicators, and mountainous terrain, reduced access to care has been implicated in the region’s cancer disparities (Paskett et al., 2011).
Access to care is a multidimensional concept that consists of both spatial and nonspatial factors. Nonspatial factors included age, socioeconomic status, and ethnicity, for example (Wang & Luo, 2005). Spatial access is instead focused on the geographic distribution of healthcare providers and the populations they serve (Wang, 2012). Some researchers further distinguish between potential spatial access, referring to the geographic possibility that a service will be utilized, and realized access, which refers to the actual service used (McGrail, 2012). This study focuses on potential spatial access (further termed ‘spatial access’ for brevity.).
Traditionally, spatial access was calculated as a provider to population ratio, often using counties as the geographic boundaries (Wang, 2012). The method is simple to compute, requiring only population statistics (e.g., U.S. Census data) and the number of healthcare providers working in that county. The current Health Professional Shortage Area (HPSA) designation by the U.S. Department of Health and Human Services (DHHS) relies on this technique (DHHS, 2010). DHHS sets a threshold of one physician per 3,000 people in a rational service area to define HPSAs. With more widespread use of geographic information systems (GIS) technologies, researchers began using travel time or travel distance between population and providers as a measure of spatial access (Wang & Lou, 2005). This allowed more specificity, as individual patient and provider addresses could be geocoded into GIS software.
Although these two methods are the most widely used, they have noted limitations (Guagliardo, 2004). The fixed boundaries of provider to population ratios do not match real world healthcare utilization. Ratios also fail to account for travel impediments within their fixed boundary, giving equal weight to providers and populations on opposite ends of a boundary as those geographically closer. While travel time or distance GIS calculations overcome the latter problem of travel impediments, the calculations fail to capture the supply and demand element of healthcare.
The two-step floating catchment area (2SFCA) has emerged as an additional measure of spatial access to care that overcomes some of the limitations of the original methods (Luo & Wang, 2003; Wang & Luo, 2005). The first step of the 2SFCA identifies the populations that each healthcare provider serves. This area is called a catchment and can range from a 30 to 60 minute travel time, or longer, depending on the type of care. A provider to population ratio is computed for each physician’s catchment. Step two moves to each population area and searches for all service providers within that population’s catchment, also set at 30 to 60 minutes, or longer. The step one ratios within a population’s catchment are then summed, resulting in an access score for each population location.
There are limitations to the original 2SFCA method, however (Luo & Whippo, 2012; Wang, 2012). The step one and step two catchments still suffer from the boundary problem described for traditional provider to population ratios. For some service providers a 30 minute catchment may be accurate, but others will serve a smaller area (downtown urban providers) or larger area (rural community providers). Also, within the step one and step two catchments, the original 2SFCA fails to account for travel impediments, also termed distance decay. During step one, for example, a population 5 minutes from a provider is deemed as likely to use the service as a population 25 minutes away.
In response to these limitations, several researchers have modified the original 2SFCA (Luo & Qi, 2009; McGrail & Humphreys, 2009). A distance decay function was added to distinguish between different geographic distances within a catchment. The catchment can be broken into distinct zones (e.g., 0–10 min., 10–20 min, 20–30 min.), with a unique weight applied at each zone (Luo & Qi, 2009). A continuous function has also been used (McGrail & Humphreys, 2009) where there is no drop at the end of the zone. Weights are applied smoothly at each increase in travel time or distance. Another addition has been the use of variable catchment sizes. One technique is to define a desired provider to population ratio (e.g., 1:3,000) and expand a catchment until that ratio is met (Luo & Whippo, 2012). Another technique is to cap the number of providers a population can access (e.g., 100), and when that limit is reached the catchment ends (McGrail & Humphreys, 2009). Taking a different approach, another group of researchers (Wan et al., 2012) created the spatial access ratio (SPAR) score, which can use any of the modified 2SFCA methods mentioned by taking a population’s (i.e., census tract) 2SFCA score and dividing it by the mean 2SFCA score of an entire region. The SPAR score represents a relative comparison that may be useful when researchers are unsure how much of a travel impediment exists and therefore which decay weights to use (Wan et al., 2012).
The 2SFCA method, despite its noted benefits, has never been used to study access to care in Appalachia. Outside of Appalachia, only a limited amount of research has compared and contrasted the effects of the newer 2SFCA parameters (i.e., distance decay and variable catchment sizes) on resulting access to care scores (McGrail, 2012; Wang, 2012). These comparisons generally occur in the context of primary care. Thus, researchers in Appalachia who study spatial access to more specialized cancer care need guidance on which methods are most appropriate and which parameters to choose.
The primary goal of this study was to explore patterns of potential spatial access to mammography centers in Appalachia. We compared results across the measures of provider to population ratios, travel times between populations and providers, and the newer 2SFCA method. Within the 2SFCA method, we compared the effects of added distance decay functions and variable catchment sizes on the resulting access scores. Finally, we evaluated the differences in access to mammography centers between Appalachia and non-Appalachia areas of the same states, using all three spatial access measures.
2. Study area and data
We focused on a four state region of Appalachia: PA, OH, KY, and NC. All U.S. Food and Drug Administration (FDA)-accredited non-mobile mammography facilities in the four states during the year 2008 were obtained. There were 1,181 mammography centers in the four state study region, and each center had a street address that was able to be geocoded into GIS software. We did not include mammography centers of bordering states, which can affect access scores of populations near state borders. Our mammography dataset did not include total capacity at each center.
Population data were extracted from the 2010 U.S. Census at the census block group level. Block groups usually have between 600 and 3,000 people, with an ideal size of 1,500. Much prior research measuring spatial access to care aggregated population data at larger geographic areas, generally zip codes (Dai, 2010) and census tracts (Wan et al., 2012). Using census block groups is more computationally intensive but allows greater precision in geographic estimation. Following previous research (Luo & Wang, 2003), we used the population weighted centroid of each block group, rather than the geographic centroid (U.S. Census Bureau, 2014). Centroid locations are given as latitude and longitude, which allows for integration into GIS software. Unlike mammography centers, we did include populations in neighboring states to simulate more accurate spatial access along state borders. We explore this edge effect in greater detail in the discussion.
The Appalachia Regional Commission’s (ARC) county designations were used to distinguish Appalachia and non-Appalachia areas. There were 28,418 total block groups, although only 28,357 had residents. Of those, there were 8,707 block groups in Appalachia regions of the four states and 19,650 block groups in non-Appalachia regions. There were 10,717,421 people living in Appalachia regions and 27,392,443 people living in non-Appalachia regions. Further designation of rural and non-rural areas was used when comparing spatial access scores. Urban-rural designation is done by census tract, with census RUCA codes of 7–10 considered rural and codes 1–6 considered urban-suburban (Weeks et al., 2004). The rural population was 2,971,896 people and the urban population was 35,137,968 people. There are additional, multifaceted ways to describe a population along the rural-urban spectrum, but for ease of interpretation we chose to use a simple rural-urban classification. We used descriptive statistics and t-tests to compare access scores between Appalachia and non-Appalachia regions and between rural and urban regions.
3. Methodology
3.1 Provider to population ratios
We calculated provider to population ratios at the county level. The number of mammography centers in each county was divided by the population of women age 45 and older in that county. Guidelines called for mammography screening beginning at age 40 (U.S. Preventive Service Task Force, 2009). However, the 2010 Census used age groups 35–44 and 45–54. We chose to use women age 45 and older, consistent with prior research (Anderson et al., 2014). Each census block group, our primary unit of analysis, was then assigned a county ratio based on the geographic county it resided in.
3.2 Travel time
Mammography centers and census block groups were geocoded into ArcGIS (Version 10.1, ESRI Inc., Redlands, CA). We used the Origin-Destination (OD) cost matrix function of the ArcGIS Network Analyst extension to compute travel times between the population weighted centroid of each block group and each mammography center, only including pairs within one hour of each other. A recent 10-state cancer registry study (Henry et al., 2011) with over 160,000 breast cancer patients found that the average travel time to a patient’s diagnosing mammography facility was 16.5 minutes and 97% of patients lived within one hour of their diagnosing facility. Along with travel time to the closest facility, we also computed the average travel time to the three closest facilities.
3.3 Two-step floating catchment area
The first step of the original 2SFCA method identifies all populations (k) within a service provider’s (j) maximum catchment (do), set as a maximum of 60 minutes driving time. Although other 2SFCA mammography studies have used a 30 minute max catchment size (Lian et al., 2012), we felt the rural nature of Appalachia warranted a 60 minute maximum catchment size (McGrail & Humphreys, 2009). A population to provider ratio (Rj) is then computed using the total service providers (Sj) and total population (Pk) within catchment j:
Step 1: Rj =Sj / Σk ε {djk < do} Pk
Step 2 of the 2SFCA identifies all service providers (j) within the maximum travel time (do) of a population location (i) and sums all of the eligible service providers’ step 1 ratios (Rj), resulting in that population location’s access score (Ai):
Step 2: Ai = Σj ε {dij < do} Rj
We also examined three additional versions of the 2SFCA. The first included an added distance decay function across catchment time zones (Luo & Qi, 2009). Catchments were divided into four time zones: 0–10 minutes, 11–20 minutes, 21–30 minutes, and 31–60 minutes. Weights were applied at each zone in order to simulate the travel impediment as travel time increased. We used fast-step weightings and slow-step weightings, chosen from prior research (McGrail, 2012; Wan et al., 20120):
Fast-decay weights (w) = 1, 0.60, 0.25, 0.05
Slow-decay weights (w) = 1, 0.80, 0.55, 0.15
Thus, each population location (k) in step one and each physician ratio (Rj) during step two are discounted by an above weight, depending on the travel time between population and provider (i.e., above weights correspond to 0–10, 11–20, 21–30, and 31–60 minute time zones):
Step 1: Rj =Sj / Σk ε {djk < do} Pk w
Step 2: Ai = Σj ε {dij < do} Rj w
The second version of the 2SFCA we examined included both distance decay weights and varying catchment sizes. For step one of the 2SFCA, we used local population characteristics to determine how far to expand a service provider’s catchment, and thereby whether or not to apply the distance decay weights mentioned above (McGrail & Humphreys, 2009b). If a population was within 10 minutes of a service provider, no decay weight was applied. If the service provider was one of the five closest providers, no weight was applied because that provider will likely provide service to populations with few other choices. Prior research (McGrail & Humphreys, 2009b) set this limit to the closest 25 services, but that study examined primary care, not mammography centers, which are less abundant. Finally, if the service provider’s town population was greater than 5,000 and the population center’s town population was less than half of the service provider’s, no weight was applied. This rule represents situations where the service provider is in a larger town that likely provides services to smaller nearby communities. To estimate town populations, we linked mammography centers and census block groups with their closest Census Designated Place (CDP). CDPs are meant represent the settled concentration of populations as either a city, town, village, or borough, and can cross county boundaries (U.S. Census Bureau, 2014). For step two of the 2SFCA, we capped the number of services a population center could access at 20. Thus, the first 20 services were weighted according to the distance decay rules above, but services after the first 20 closest were not included in that population’s catchment. The cap represented the point where additional services do not offer increasing access. Again, prior primary care research set this cap at 100 (McGrail & Humphreys, 2009), but due to lesser numbers of mammography centers we set the cap at 20.
When evaluating the combination of 2SFCA distance decay and variable catchment sizes, we also included a continuous decay weighting scheme to contrast with the slow-decay and fast-decay weights (McGrail & Humphreys, 2009). The continuous weighting scheme followed the same rules and caps as above. But, when travel times (d) between population and provider were greater than 10 minutes and less than 60 minutes, and a slow or fast-decay weight would be applied, the following continuous weighting (w) was applied instead:
Continuous-decay weights (w) = ((60-d) / (60-10)) ^ 1.5
The final 2SFCA version we considered was the spatial access ratio (SPAR) score (Wan et al., 2012). SPAR was created in response to the subjectivity of distance decay weights and varying catchment sizes. SPAR is simple to calculate, being the ratio between a block group’s 2SFCA score and the mean of all block group 2SFCA scores.
In sum, each census block group was assigned 10 spatial access scores for comparison: 1) County mammography facility to women age 45 years and older ratio; 2) Travel time to closest mammography center; 3) Original 2SFCA score; 4) Slow-decay 2SFCA score; 5) Fast-decay 2SFCA score; 6) Slow-decay and variable catchment 2SFCA score; 7) Fast-decay and variable catchment 2SFCA score; 8) Continuous-decay and variable catchment 2SFCA score; 9) Slow-decay and variable catchment SPAR score; 10) Fast-decay and variable catchment SPAR score. We mapped spatial access scores over their geographic area to visualize the resulting access within our study region.
4. Results
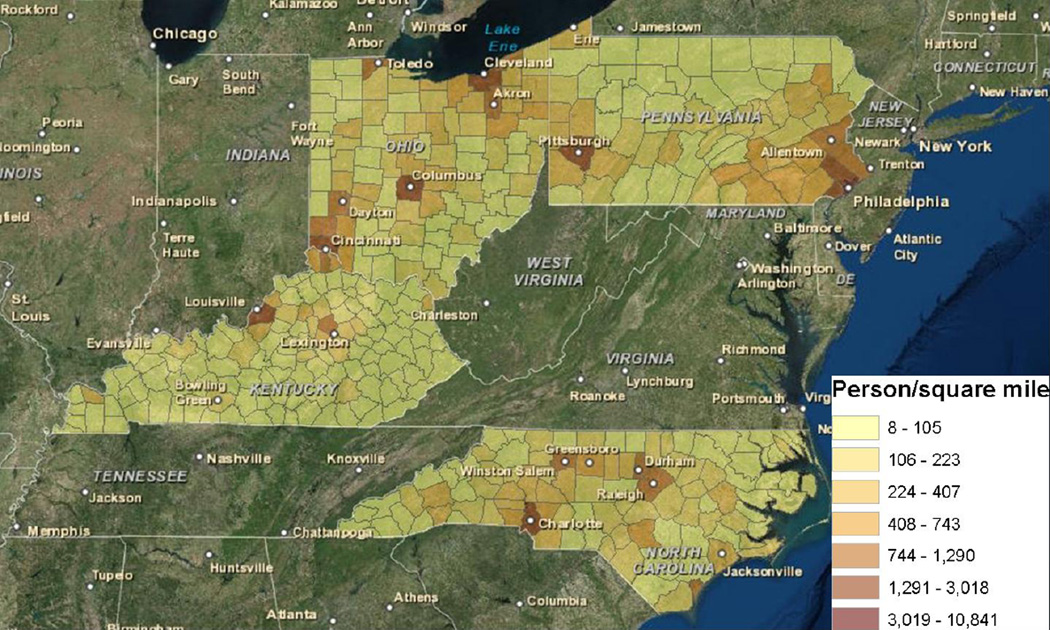
The regions with the highest population density included Philadelphia and surrounding southeastern Pennsylvania; the Pittsburgh area of western Pennsylvania; the Ohio cities of Cleveland, Akron, Columbus, and Cincinnati; Louisville and Lexington in Kentucky, and the smaller cities of central North Carolina (Fig. 1). The least populated areas were north central Pennsylvania and eastern Kentucky.
Fig 1.
Population density across the counties of PA, OH, KY, and NC.
Spearman correlations were statistically significant between each of the 10 spatial access measures (Table 1). Increases in the provider to population ratio and the 2SFCA scores signal increasing spatial access, thus the negative correlation of both those measures with travel time to the closest mammography center, where decreasing travel times signal increasing spatial access. Travel time and population to provider ratio had the weakest correlation (rho = −0.115). Slightly stronger correlations occurred between travel time and the 2SFCA measures (−0.522 ≤ rho ≤ −0.180) and between provider to population ration and the 2SFCA measures (0.351 ≤ rho ≤ 0.5450). Expectedly, the strongest correlations occurred between the various 2SFCA scores. The original 2SFCA score had a moderately strong correlation (0.599 ≤ rho ≤ 0.753) with the modified 2SFCA approaches, while each of the modified 2SFCA approaches were strongly correlated (0.777 ≤ rho ≤ 1).
Table 1.
Spearman correlations* between 10 spatial access to care measures across PA, OH, KY, and NC
| Prov. - Pop. Ratio |
1 | |||||||||
| Travel Time | −0.115 | 1 | ||||||||
| Original 2SFCA | 0.351 | −0.180 | 1 | |||||||
| Slow 2SFCA | 0.510 | −0.416 | 0.753 | 1 | ||||||
| Fast 2SFCA | 0.545 | −0.522 | 0.640 | 0.948 | 1 | |||||
| Slow - Var. Catch. 2SFCA a |
0.541 | −0.243 | 0.619 | 0.835 | 0.818 | 1 | ||||
| Fast - Var. Catch. 2SFCA b |
0.503 | −0.485 | 0.603 | 0.882 | 0.909 | 0.901 | 1 | |||
| Cont. - Var. Catch. 2SFCA c |
0.537 | −0.212 | 0.599 | 0.790 | 0.777 | 0.953 | 0.836 | 1 | ||
| Slow - Var. Catch. SPAR |
0.541 | −0.243 | 0.619 | 0.835 | 0.818 | 1.000 | 0.901 | 0.953 | 1 | |
| Fast - Var. Catch. SPAR |
0.503 | −0.485 | 0.603 | 0.882 | 0.909 | 0.901 | 1.000 | 0.836 | 0.901 | 1 |
| Prov. - Pop. Ratio |
Travel Time |
Original 2SFCA |
Slow 2SFCA |
Fast 2SFCA |
Slow - Var. Catch. 2SFCA |
Fast - Var. Catch. 2SFCA |
Cont. - Var. Catch. 2SFCA |
Slow - Var. Catch. SPAR |
Fast - Var. Catch. SPAR |
2SFCA, Two-Step Floating Catchment Area; SPAR, Spatial Access Ratio
All correlations significant at the 0.01 level
Slow - Var. Catch. 2SFCA: Both slow-decay weightings and varying catchment size rules
Fast - Var. Catch. 2SFCA: Both fast-decay weightings and varying catchment size rules
Cont. - Var. Catch. 2SFCA: Both continuous-decay weightings and varying catchment size rules
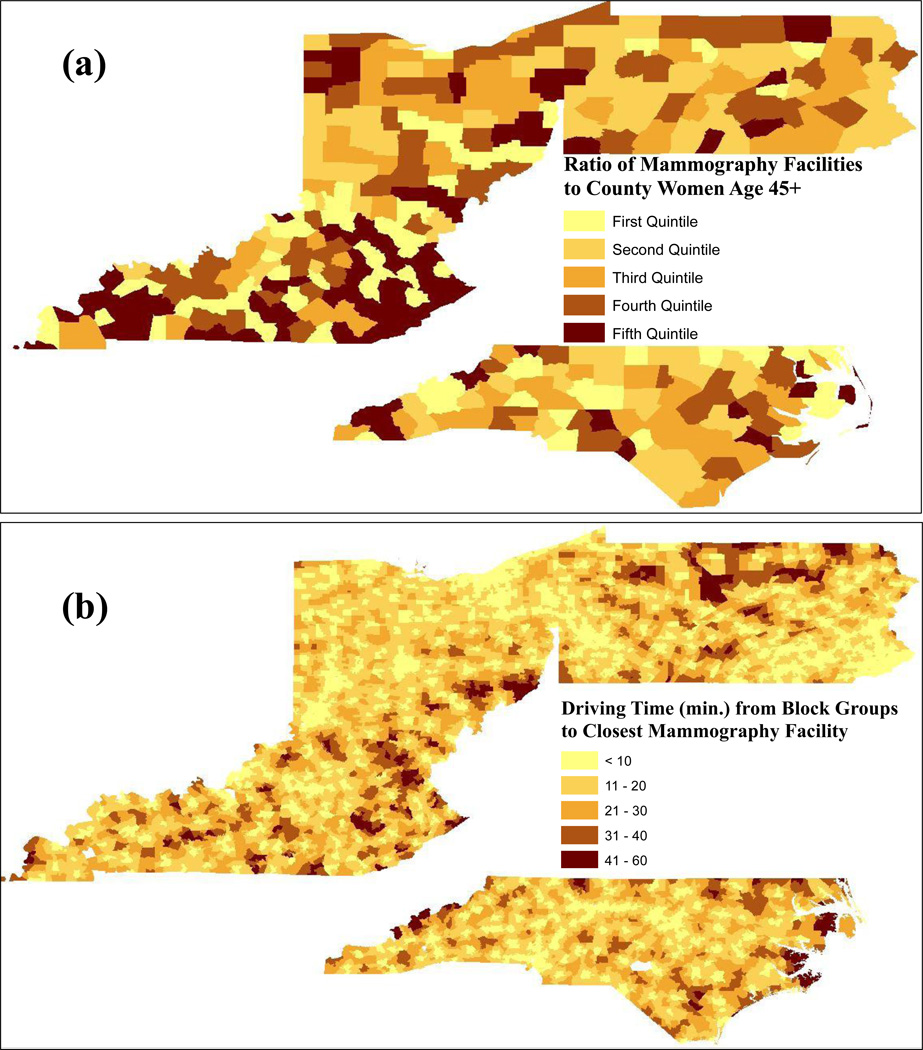
County provider to population ratios are shown in Figure 2, with darker colors representing larger ratios in the higher quintile groups, and therefore greater spatial access. Many of the highest scores are found in Kentucky, where lower populations result in higher ratios.
Figure 2.
Spatial Access to Mammography centers by (a) county provider to population ratio, broken into quintiles, and (b) closest driving time from census block groups
The largest population centers—the Pittsburgh and Philadelphia regions—have mediocre scores, despite having the greatest number of mammography facilities. Rigid boundary differences are present, especially in Kentucky, where scores from the largest and smallest quintiles border each other.
The largest driving times between census block groups and their closest mammography facility occurred in north central Pennsylvania, eastern Ohio, and eastern Kentucky (Fig. 2). The Cleveland-Akron to Pittsburgh corridor, the Philadelphia area, and central North Carolina had the shortest travel times. The shortest travel time measure had more gradual transitions from higher to lower access, compared to the county ratio measure.
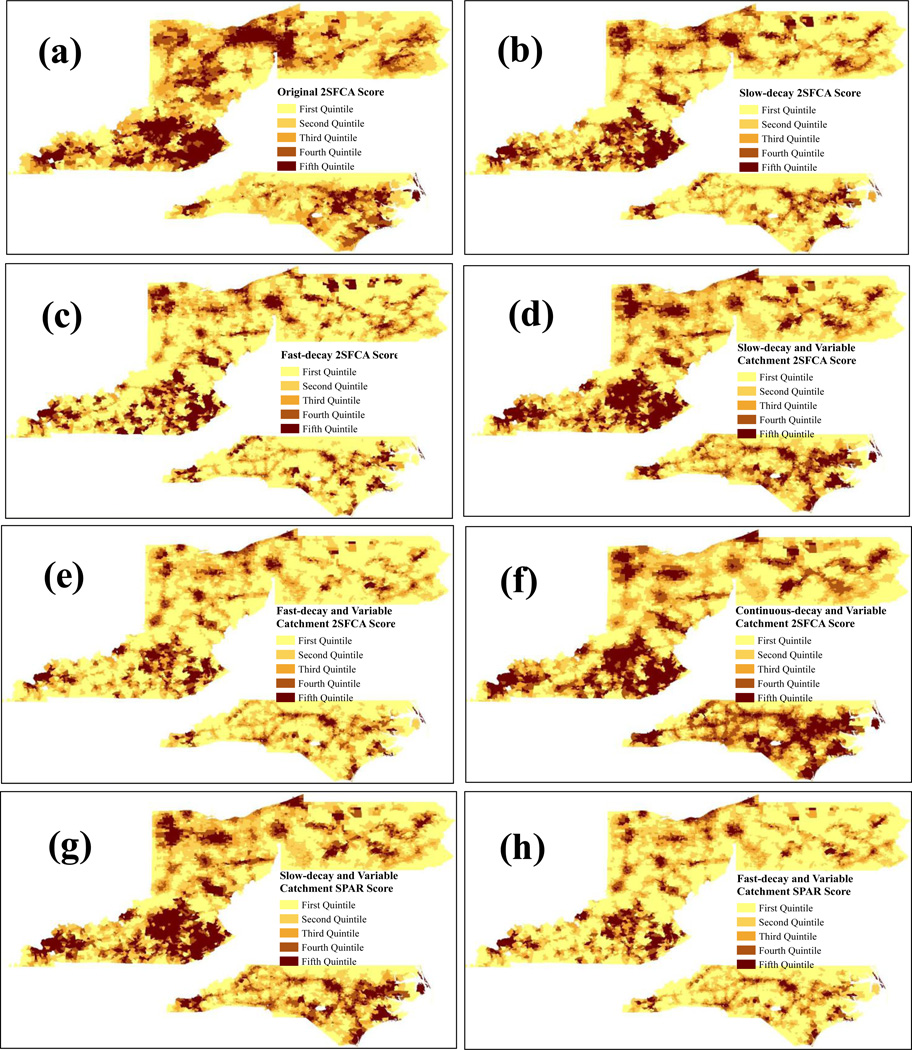
The census block groups with the highest original 2SFCA scores were in the Cleveland-Akron-Pittsburgh corridor, as well as central and eastern Kentucky (Fig. 3a). When slow (Fig. 3b) and fast (Fig. 3c) distance decay functions were added, higher access scores became more dispersed and less clustered in contiguous areas, with the greatest difference occurring between the original and fast-decay 2SFCA scores. The differences were more subtle when varying the catchment sizes on the slow-decay (Fig. 3d) and fast-decay (Fig 3e) scores. For the slow-decay scores, using a variable catchment decreased access in the northern corridor of Cleveland-Youngstown-Pittsburg because populations were only allowed to access the first 20 providers. These metropolitan areas had more than 20 mammography centers (e.g., the greater Pittsburgh area has about 60), and without a limit on the number of providers their populations can access their scores increase. Conversely, using variable catchments comparatively increased the slow-decay access for the NC cities Greensboro and Charlotte because those cities do not have a surplus of mammography centers (e.g., the greater Greensboro area has about 20), and thus their access scores did not drastically decrease when limiting catchment sizes.
Figure 3.
Spatial access of census block groups in PA, OH, KY, and NC to mammography centers by (a) original 2SFCA scores; (b) slow-decay 2SFCA scores; (c) fast-decay 2SFCA scores; (d) slow-decay and variable catchment 2SFCA scores; (e) fast-decay and variable catchment 2SFCA scores; (f) continuous-decay and variable catchment 2SFCA scores; (g) slow-decay and variable catchment SPAR scores; (h) fast-decay and variable catchment SPAR scores. Scores are broken into quintiles, with larger quintiles representing greater spatial access.
The most noticeable difference when varying catchment sizes within fast-decay scores (Fig. 3e) was reduced access in northwest Ohio, the Youngstown-Pittsburg corridor, and rural central PA. Using a continuous-decay function along with varying catchments (Fig. 3f) resulted in scores more similar to the slow-decay and variable catchment 2SFCA scores, rather than the fast-decay and variable catchment 2SFCA scores. The greatest difference with the continuous-decay scores was the increase in scores throughout much of NC. The difference between slow-decay, variable catchment and fast-decay, variable catchment SPAR scores mirrored the differences between their corresponding 2SFCA scores, despite previous evidence of SPAR scores being robust against changes in decay weightings (Wan et al., 2012).
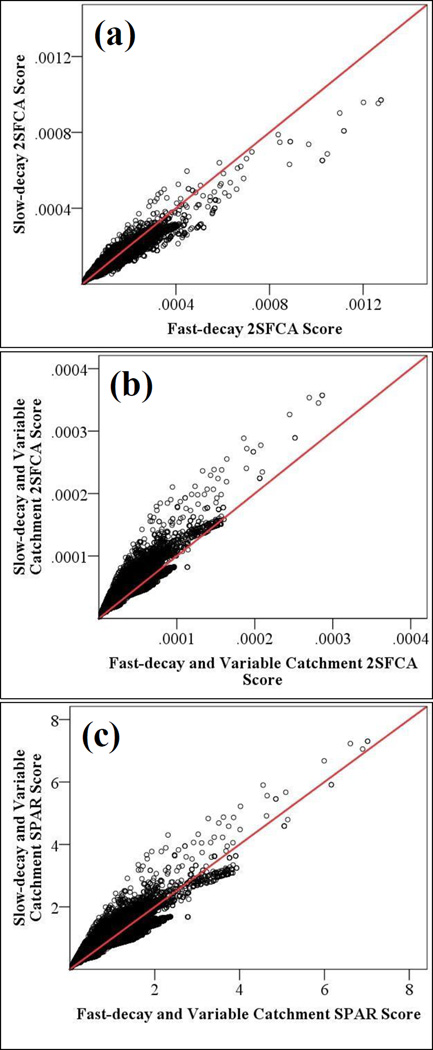
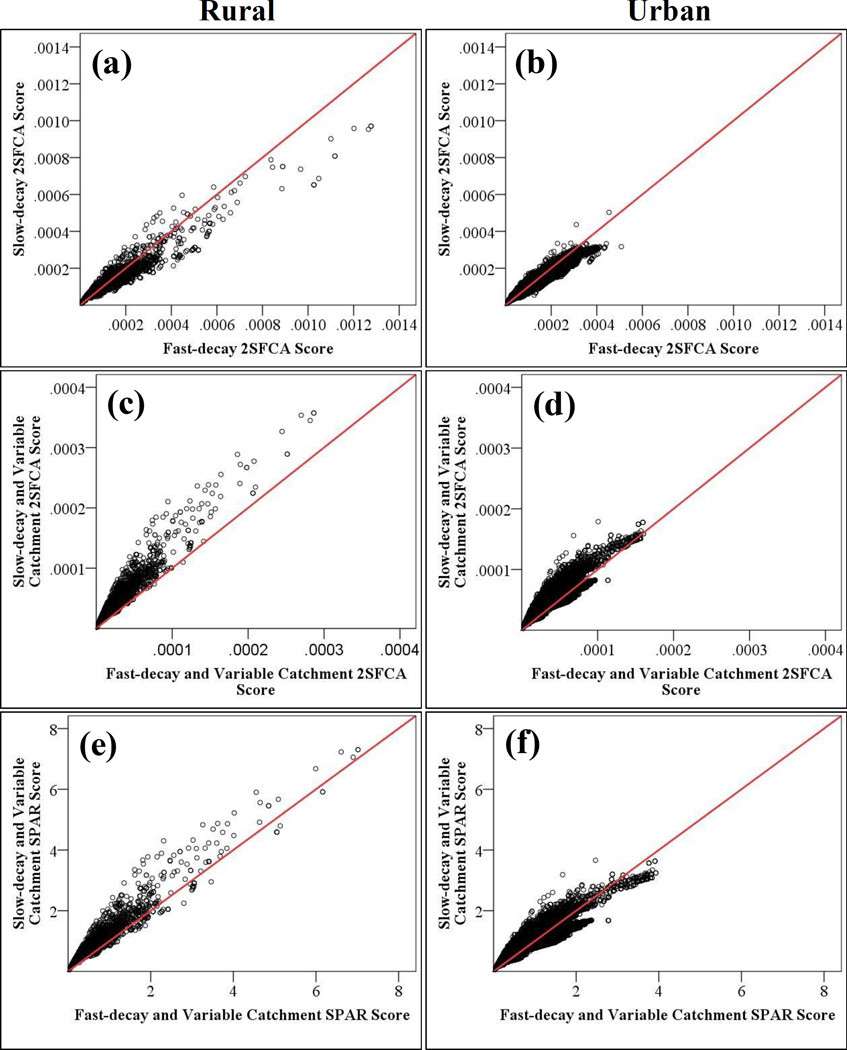
It is also helpful to compare the actual change in value for a 2SFCA score at the same population center after changing the decay weighting scheme. Figure 4 plots the different 2SFCA and SPAR values at each census block group by the varying slow- and fast-decay weightings. When using only the distance decay approach (Fig. 4a), there was no uniform increase or decrease based on slow or fast decay weightings. The only exception were the highest outlier scores, where the fast-decay weighting always increased scores. The distance decay and variable catchment size approach (Fig. 4b) produced a uniform result where nearly all block groups had reduced scores when using the fast-decay, variable catchment technique. The SPAR distance decay and variable catchment approach (Fig. 4c) moderated scores to some extent, compared to the similar 2SFCA approach, but a noticeable decrease in scores after using the fast decay, variable catchment technique still occurred for a majority of block groups.
Figure 4.
Comparison of spatial accessibilty across each census block group between (a) slow-decay and fast-decay 2SFCA scores; (b) Slow-decay, variable catchment and fast-decay, variable catchment 2SFCA scores; (c) Slow-decay, variable catchment and fast-decay, variable catchment SPAR scores
Figure 5 distinguishes between urban and rural census block groups when comparing the change in value for 2SFCA scores after changing the decay weighting scheme. The most noticeable difference is that the highest scores across each approach were always from rural block groups (the scales are the same between urban and rural). The lower population pressure of rural areas in step one of the 2SFCA likely results in their increased scores compared to urban areas. For urban block groups, the SPAR distance decay and variable catchment approach (Fig. 5f) was closer to achieving its intended effect of not letting decay weights uniformly impact scores. For rural block groups, however, scores were uniformly decreased with the fast-decay, variable catchment technique (Fig. 5e). Mammography centers are generally farther distances from rural block groups, thus faster decay weightings appear to have more impact.
Figure 5.
Comparison of spatial accessibilty across rural and urban census block groups between (a-b) slow-decay and fast-decay 2SFCA scores; (c-d) Slow-decay, variable catchmentand and fast-decay, variable catchment 2SFCA scores; (e-f) Slow-decay, variable catchment and fast-decay, variable catchment SPAR scores
Continuing with the urban-rural divide, Table 2 compares the mean values across all spatial access measures between urban and rural block groups. Rural block groups had a higher provider to population ratio across each state. Conversely, travel time to the closest mammography center favored urban block groups, who on average had between an 11.15 minute (PA) and 6.17 minute (KY) shorter travel time than rural block groups. In PA, the 2SFCA and SPAR measures were either very similar between urban and rural block groups, or urban block groups had larger scores (e.g., slow-decay 2SFCA and fast-decay 2SFCA). In OH and NC, scores were higher for urban block groups across each 2SFCA and SPAR measure. In KY, rural block groups generally had larger scores, with the exception of the fast-decay, variable catchment 2SFCA and the fast-decay, variable catchment SPAR. Kentucky’s urban areas are smaller than the other study states, and the increasing population demands are not balanced with substantially greater numbers of mammography centers.
Table 2.
Descriptive statistics of mammography center spatial access scores between rural and urban census block groups of PA, OH, KY, and NC.
| Spatial Access Measures | All States | Pennsylvania | Ohio | Kentucky | North Carolina | ||||
|---|---|---|---|---|---|---|---|---|---|
| Mean (SD) | Rural | Urban | Rural | Urban | Rural | Urban | Rural | Urban | |
| Provider to Population Ratio | 0.0000148 (0.000073) |
0.000154 (0.000070) |
0.000134 (0.000039) |
0.000174 (0.000084) |
0.000158 (0.000066) |
0.000283 (0.000194) |
0.000164 (0.000093) |
0.000164 (0.000111) |
0.000123 (0.000052) |
| Travel Time to Closest Mammograpy Center (min.) |
8.67 (7.83) |
17.93 (11.58) |
6.78 (6.39) |
14.08 (9.95) |
6.81 (5.85) |
16.42 (11.36) |
10.25 (8.95) |
17.21 (10.81) |
10.48 (7.71) |
| Origianl 2SFCA | 0.000129 (0.000049) |
0.000101 (0.000037) |
0.000115 (0.000039) |
0.000109 (0.000034) |
0.000144 (0.000040) |
0.000197 (0.000116) |
0.000147 (0.000058) |
0.000098 (0.000041) |
0.000120 (0.000038) |
| Slow-decay 2SFCA | 0.000136 (0.000058) |
0.000105 (0.000052) |
0.000124 (0.000046) |
0.000113 (0.000047) |
0.000150 (0.000049) |
0.000207 (0.000145) |
0.000156 (0.000066) |
0.000108 (0.000061) |
0.000124 (0.000047) |
| Fast-decay 2SFCA | 0.000140 (0.000070) |
0.000112 (0.000077) |
0.000128 (0.000053) |
0.000122 (0.000066) |
0.000154 (0.000060) |
0.000221 (0.000188) |
0.000159 (0.000079) |
0.000120 (0.000090) |
0.000127 (0.000058) |
| Slow-decay, variable catchment 2SFCA |
0.000049 (0.000024) |
0.000038* (0.000018) |
0.000038 (0.000020) |
0.000046 (0.000019) |
0.000050 (0.000014) |
0.000078 (0.000054) |
0.000069 (0.000033) |
0.000044 (0.000023) |
0.000054 (0.000021) |
| Fast-decay, Variable Catchment 2SFCA |
0.000041 (0.000023) |
0.000023 (0.000015) |
0.000032 (0.000017) |
0.000029 (0.000015) |
0.000047 (0.000017) |
0.000049 (0.000042) |
0.000056 (0.000035) |
0.000028 (0.000019) |
0.000042 (0.000021) |
| Continuous-decay, Variable Catchment 2SFCA |
0.000046 (0.000024) |
0.000036 (0.000018) |
0.000034 (0.000019) |
0.000041 (0.000018) |
0.000043 (0.000013) |
0.000074 (0000054) |
0.000064 (0.000029) |
0.000048 (0.000025) |
0.000058 (0.000020) |
| Slow-decay, Variable Catchment SPAR |
1.00 (0.49) | 0.77* (0.37) |
0.77 (0.41) | 0.93 (0.39) | 1.03 (0.28) | 1.60 (1.11) | 1.41 (0.68) | 0.89 (0.47) | 1.10 (0.42) |
| Fast-decay, Variable Catchment SPAR |
1.00 (0.55) | 0.57 (0.37) | 0.79 (0.41) | 0.71 (0.37) | 1.15 (0.42) | 1.20 (1.03) | 1.38 (0.85) | 0.68 (0.47) | 1.03 (0.52) |
2SFCA, Two-Step Floating Catchment Area; SPAR, Spatial Access Ratio
Not siginificant at p < 0.05; all other Rural and Urban comparisons were significant at P < 0.01 .
Finally, the mean values of spatial access scores between Appalachia and non-Appalachia block groups were compared (Table 3). Appalachia block groups had a higher provider to population ratio across each state, similar to the rural block groups in Table 2. Travel time, though, was greater for Appalachia areas, ranging from an increase of only 1.02 minutes in NC to 7.23 minutes in KY. In PA and KY, Appalachia block groups had higher 2SFCA and SPAR scores than non-Appalachia block groups. The difference in scores was closer in OH, but generally the non-Appalachia scores were higher. In NC, all 2SFCA and SPAR measures were higher in non-Appalachia block groups.
Table 3.
Descriptive statistics of mammography center spatial access scores between Appalachia and non-Appalachia census block groups of PA, OH, KY, and NC.
| Spatial Access Measures | All States | Pennsylvania | Ohio | Kentucky | North Carolina | ||||
|---|---|---|---|---|---|---|---|---|---|
| Mean (SD) | App | Non-App | App | Non-App | App | Non-App | App | Non-App | |
| Provider to Population Ratio | 0.0000148 (0.000073) |
0.00146 (0.000048) |
0.000125 (0.000031) |
0.000189 (0.000124) |
0.000153 (0.000043) |
0.000244 (0.00019) |
0.000170 (0.000093) |
0.000128* (0.000082) |
0.000126 (0.000056) |
| Travel Time to Closest Mammograpy Center (min.) |
8.67 (7.83) |
9 . 7 7 (8.68) |
5.00 (4.19) |
11.31 (9.36) |
6.39 (5.20) |
16.79 (11.77) |
9.56 (8.14) |
11.98 (8.17) |
10.96 (8.35) |
| Origianl 2SFCA | 0.000129 (0.000049) |
0.000132 (0.000037) |
0.000097 (0.000033) |
0.000129 (0.000044) |
0.000145 (0.000039) |
0.000202 (0.000109) |
0.000141 (0.000052) |
0.000099 (0.000032) |
0.000122 (0.000039) |
| Slow-decay 2SFCA | 0.000136 (0.000058) |
0.000138 (0.000050) |
0.000109 (0.000038) |
0.000144 (0.000073) |
0.000149 (0.000042) |
0.000204 (0.000134) |
0.000153 (0.000064) |
0.000109 (0.000044) |
.000126 (0.000049) |
| Fast-decay 2SFCA | 0.000140 (0.000070) |
0.000140 (0.000061) |
0.000115 (0.000043) |
0.000157 (0.000098) |
0.000151 (0.000049) |
0.000208 (0.000172 |
0.000159 (0.000079) |
0.000115 (0.000059) |
0.000129 (0.000062) |
| Slow-decay, Variable Catchment 2SFCA |
0.000049 (0.000024) |
0.000046 (0.000021) |
0.000029 (0.000014) |
0.000048 (0.000018) |
0.000050 (0.000013) |
0.000079 (0.000050) |
0.000068 (0.000033) |
0.000047 (0.000018) |
0.000055 (0.000022) |
| Fast-decay, Variable Catchment 2SFCA |
0.000041 (0.000023) |
0.000035 (0.000019) |
0.000028 (0.000013) |
0.000037 (0.000021) |
0.000048 (0.000016) |
0.000049 (0.000039) |
0.000057 (0.000036) |
0.000032 (0.000016) |
0.000043 (0.000022) |
| Continuous-decay, Variable Catchment 2SFCA |
0.000046 (0.000024) |
0.000043 (0.000020) |
0.000025 (0.000012) |
0.000043* (0.000016) |
0.000043 (0.000013) |
0.000075 (0.000049) |
0.000063 (0.000030) |
0.000050 (0.000019) |
0.000059 (0.000021) |
| Slow-decay, Variable Catchment SPAR |
1.00 (0.49) | 0.95 (0.42) | 0.60 (0.29) | 0.98 (0.37) | 1.03 (0.26) | 1.62 (1.02) | 1.39 (0.68) | 0.95 (0.36) | 1.12 (0.44) |
| Fast-decay, Variable Catchment SPAR |
1.00 (0.55) | 0.87 (0.47) | 0.69 (0.33) | 0.91 (0.52 | 1.17 (0.39) | 1.21 (0.95) | 1.39 (0.87) | 0.78 (0.40) | 1.04 (0.54) |
2SFCA, Two-Step Floating Catchment Area; SPAR, Spatial Access Ratio
Not siginificant at p < 0.05; all other Appalachia and Non-Appalachia comparisons were significant at P < 0.01 .
Discussion
Substandard access to care is implicated in cancer incidence and treatment patterns throughout Appalachia, yet no prior studies have evaluated the latest spatial access to care measures in the region. This study evaluated spatial access methods across a four-state region of Appalachia, compared differences between measures, and evaluated access between Appalachia and non-Appalachia areas of the same states. All access measures were significantly correlated with each other, although the strongest correlations occurred between variations of the 2SFCA method. Measuring travel time to closest mammography centers produced expected results. Urban-core areas were all within 10 minutes of their closest mammography center, while rural parts of north central PA, eastern OH, and eastern KY comprised the majority of areas with travel times greater than 40 minutes. Appalachia populations across each state had longer average travel times than non-Appalachia populations. Provider to population ratios were more unpredictable and abrupt. Adjacent areas of rural KY, for example, comprised the lowest and highest quintile scores because of rigid county boundaries. Clear geographic differences emerged when comparing the various iterations of the 2SFCA method. It was difficult, however, discern easily identifiable patterns corresponding to the 2SFCA parameters because of the study region’s size and varying population distribution.
A consistent finding of the original 2SFCA, in regards to primary care physicians, was that urban areas had the highest access scores (Wang & Luo, 2005). In regards to mammography centers in Appalachia, our results partly confirm this trend. Urban areas in western PA, throughout Ohio, and in central NC all had among the highest original 2SFCA access scores. The largest urban area, the Philadelphia region, contradicted that trend with mostly poor to moderate scores. Also surprising was that rural eastern KY comprised a large portion of the highest access scores, likely because of the low population density and a geographically consistent distribution of mammography centers through the state.
The concept of distance-decay weights within catchments was originally proposed because researchers wanted to limit accessibility at the edge of physician catchments, which often occurred between major population centers (Luo & Qi, 2009). In our original 2SFCA scores, for example, the entire corridor between northeastern OH cities received the highest quintile of access scores. After adding distance-decay weights, though, distinct regions of lower access suburban and rural areas emerged between these urban areas, particularly when using faster decay weights.
When creating methods to vary catchment sizes in the 2SFCA approach, researchers wanted to further refine access scores, especially in rural areas (Luo & Whippo, 2012; McGrail, 2012). Within a realistic outer limit (e.g., 60 minutes), a rural population should be expected to travel farther for a service if that service is one of only several available. Following McGrail (2012), we did not apply distance decay weights for those closest provider and population connections when evaluating the total population that a provider serves. Our distance decay, variable catchment 2SFCA scores changed accordingly. In rural areas of each study state, mean access scores decreased when adding the variable catchments compared to only using distance-decay weights. Providers were assumed to serve more rural populations, thus the step 1 2SFCA provider-to-population ratios were lower. In step 2, summed provider ratios around each population center were lower, resulting in lower overall access scores.
Wan et al. (2012) created the SPAR technique because of a lack of guidance in the 2SFCA method when choosing decay weights within catchments. Across a nine county region of Texas, they showed that SPAR scores remained comparatively stable between populations despite using different decay weights. They applied SPAR to a 2SFCA model using only distance decay, not variable catchments, and in reference to primary care. Our application of SPAR in Appalachia to a distance decay, variable catchment model focusing on mammography centers largely achieved SPAR’s intended effect. When absolute scores for the SPAR and 2SFCA methods were used (e.g., Figures 4 and 5), rather than aggregated quintile values, the SPAR technique reduced the effects of choosing between a fast or slow decay weight. This was particularly true for urban populations, which represented 92% of our study population. (Our urban-rural classification placed many suburban areas in the urban category, for ease of interpretation over a large geographic area.) For these urban populations, there was no standard increase or decrease in SPAR scores corresponding to fast or slow decay weights. The SPAR technique was not as successful for rural populations, where moving from the slow to fast distance-decay, variable catchment SPAR technique did result in a more uniform decrease in scores. Nonetheless, this decrease was still less pronounced than the decrease seen when moving from slow to fast decay weights in the 2SFCA method.
Conceptually, our study had a number of strengths. To the best of our knowledge, it is the first time that the 2SFCA method has been used in Appalachia. Modern GIS software is making spatial access to care easier to measure, and public health research in the region needs to incorporate the latest techniques. Within broader work on the 2SFCA method, this study adds to a growing body of research applying the 2SFCA method to cancer care, rather than primary care (Diad, 2010; Lian et al., 2012; Wan et al., 2012). Methodologically, our study benefited from the use of a smaller population area (census block group) than many previous studies that used either zip code areas or census tracts when employing the 2SFCA method (Wang, 2012). Although more computationally intensive, this technique provided more specificity when interpreting results. Another methodological strength was our inclusion of variable catchment sizes, which are both a theoretical and empirical improvement over distance-decay functions alone. Many studies published since the creation of variable catchment sizes have failed to utilize the technique (Lian et al., 2012; Mao & Nekorchuk, 2013; Tao et al., 2014).
There were some important limitations to this study. We included populations from bordering states when computing service catchments in step 1 of the 2SFCA, but we did not include mammography centers from bordering states. This likely created an edge effect in our study region, particularly when adjacent urban areas likely included many additional mammography facilities (e.g., in New Jersey and Delaware for populations in Philadelphia). In other rural areas, such as western NC, there are unlikely to be many neighboring mammography centers along the rural Tennessee border. Another methodological limitation was our lack of information about the actual capacity of each mammography center. It is plausible that urban facilities have the capacity to serve many more women simultaneously than smaller rural facilities. By not including this distinction, there is a possibility that we underestimated 2SFCA access scores in urban areas. This omission may explain the Philadelphia region’s mediocre 2SFCA scores, as well as Table 2 more broadly.
Another limitation, and an area we believe warrants additional research, concerns our lack of representative patient healthcare utilization data. It is generally agreed that the 2SFCA needs to include travel impediments and service area variability (McGrail, 2012). Yet, the choice of which distance-decay weight to apply, or how to vary catchment sizes, is arbitrary. For instance, research needs to empirically validate that a service provider 40 minutes from a population should receive 1/12th of the weight of a provider 15 minutes away, as our fast-decay weighting scheme assumed. Similarly, it is difficult to decide where to cap the number of services that a population will consider, as we did when using 20 mammography centers as the upper limit when varying catchment sizes. Researchers need either direct evidence or expert opinion on how a population utilizes mammography centers to accurately estimate which distance-decay weight to apply or how to vary catchment sizes. In addition, research on a population’s preferred utilization patter is needed, as their actual utilization may be neither desired nor appropriate.
In conclusion, we recommend the SPAR technique when researchers do not have data on how far their study population travels or what their population’s travel preferences are. The SPAR technique, particularly for urban and suburban areas, reduces the impact of choosing a faster or slower weighting.
Acknowledgments
This research was funded by the National Cancer Institute and the NIH Office on Women’s Health through grant 1 R21 CA168479 (Balkrishnan, PI). The authors would like to acknowledge the suggestions of Drs. Kai Zheng, David Hanauer and Maureen Sartor, all at the University of Michigan who were members of Dr.Donohoe’s dissertation committee.
Footnotes
None of the authors have any conflicts of interest to disclose.
References
- Anderson RT, Yang TC, Matthews SA, Camacho F, et al. Breast Cancer Screening, Area Deprivation, and Later-Stage Breast Cancer in Appalachia: Does Geography Matter? Health Services Research. 2014;49:546–567. doi: 10.1111/1475-6773.12108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Appalachia Regional Commision (ARC) The Appalachia region. [Accessed October 10, 2014]; Available at: http://www.arc.gov/appalachian_region/TheAppalachianRegion.asp.
- Bhanegaonkar A, Madhavan S, Khanna R, Remick SC. Declining mammography screening in a State Medicaid Fee-for-Service Program: 1999–2008. Journal of Women’s Health. 2012;21(8):821–829. doi: 10.1089/jwh.2011.2748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blackley D, Behringer B, Zheng S. Cancer mortality rates in Appalachia: descriptive epidemiology and an approach to explaining differences in outcomes. J Community Health. 2012;37(4):804–813. doi: 10.1007/s10900-011-9514-z. [DOI] [PubMed] [Google Scholar]
- Dai D. Black residential segregation, disparities in spatial access to health care facilities, and late-stage breast cancer diagnosis in metropolitan Detroit. Health Place. 2010;16(5):1038–1052. doi: 10.1016/j.healthplace.2010.06.012. [DOI] [PubMed] [Google Scholar]
- Department of Health and Human Services. [Accessed October 15, 2014];Shortage Designation: Health Professional Shortage Areas & Medically Underserved Areas/Populations. 2008 Available at: http://www.hrsa.gov/shortage/
- Freeman AB, Huang B, Dragun AE. Patterns of Care With Regard to Surgical Choice and Application of Adjuvant Radiation Therapy for Preinvasive and Early Stage Breast Cancer in Rural Appalachia. Am J Clin Oncol. 2012;35(4):358–363. doi: 10.1097/COC.0b013e3182118d27. [DOI] [PubMed] [Google Scholar]
- Guagliardo MF. Spatial accessibility of primary care: concepts, methods and challenges. Int J Health Geogr. 2004;3:3. doi: 10.1186/1476-072X-3-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henry KA, Boscoe FP, Johnson CJ, Goldberg DW, Sherman R, Cockburn M. Breast cancer stage at diagnosis: Is travel time important? J. Community Health. 2011;1(36):933–942. doi: 10.1007/s10900-011-9392-4. [DOI] [PubMed] [Google Scholar]
- Lane N, Konrad R, Ricketts T, et al. Health Care Costs and Access Disparities in Apppalachia. Washington, DC: Appalachia Regional Commission; 2012. [Google Scholar]
- Lengerich EJ, Tucker TC, Powell RK, et al. Cancer Incidence in Kentucky, Pennsylvania, and West Virginia: Disparities in Appalachia. Journal of Rural Health. 2005;21(1):39–47. doi: 10.1111/j.1748-0361.2005.tb00060.x. [DOI] [PubMed] [Google Scholar]
- Lian M, Struthers J, Schootman M. Comparing GIS-Based Measures in Access to Mammography and Their Validity in Predicting Neighborhood Risk of Late-Stage Breast Cancer. PLoS ONE. 2012;7(8):e43000. doi: 10.1371/journal.pone.0043000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo W, Qi Y. An enhanced two-step floating catchment area (E2SFCA) method for measuring spatial accessibility to primary care physicians. Health Place. 2009;15:1100–1107. doi: 10.1016/j.healthplace.2009.06.002. [DOI] [PubMed] [Google Scholar]
- Luo W, Wang F. Measures of spatial accessibility to health care in a GIS environment: synthesis and a case study in the Chicago region. Environment and Planning B. 2003;30(6):865–884. doi: 10.1068/b29120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo W, Whippo TL. Variable catchment sizes for the two-step floating catchment area (2SFCA) method. Health Place. 2012;18:789–795. doi: 10.1016/j.healthplace.2012.04.002. [DOI] [PubMed] [Google Scholar]
- Mao L, Nekorchuk D. Measuring spatial accessibility to healthcare for populations with multiple transportation modes. Health Place. 2013;24:115–122. doi: 10.1016/j.healthplace.2013.08.008. [DOI] [PubMed] [Google Scholar]
- McGrail MR, Humphreys JS. The index of rural access: an innovative integrated approach for measuring primary care access. BMC Health Serv Res. 2009;9:124. doi: 10.1186/1472-6963-9-124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGrail MR, Humphreys JS. A new index of access to primary care services in rural areas. Aust NZ J Pub Health. 2009b;33:418–423. doi: 10.1111/j.1753-6405.2009.00422.x. [DOI] [PubMed] [Google Scholar]
- McGrail MR. Spatial accessibility of primary health care utilising the two step floating catchment area method: an assessment of recent improvements. Int J Health Geogr. 2012;16:11–50. doi: 10.1186/1476-072X-11-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paskett ED, Fisher JL, Lengerich EJ, et al. Disparities in underserved white populations: the case of cancer-related disparities in Appalachia. Oncologist. 2011;16(8):1072–1081. doi: 10.1634/theoncologist.2011-0145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollard K, Jacobson LA. The Appalachian Region: A Data Overview from the 2008–2012 American Community Survey. Appalachia Regional Commission. 2014 Retrieved from http://www.arc.gov/research/researchreportdetails.asp?REPORT_ID=109.
- Tao Z, Cheng Y, Dai T, Rosenberg MW. Spatial optimization of residential care facility locations in Beijing, China: maximum equity in accessibility. International Journal of Health Geographics. 2014;14:13–33. doi: 10.1186/1476-072X-13-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Census Bureau. [accessed June 5, 2014];Centers of Population. 2014 Available at: https://www.census.gov/geo/reference/centersofpop.html.
- U.S. Census Bureau. [Accessed June 5, 2014];Geographic Terms and Concepts – Place. 2014 Available at: https://www.census.gov/geo/reference/gtc/gtc_place.html.
- U.S. Preventive Services Task Force. Screening for breast cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2009;151:716–726. doi: 10.7326/0003-4819-151-10-200911170-00008. W-236. [DOI] [PubMed] [Google Scholar]
- Wan N, Zhan FB, Zou B, Chow E. A relative spatial access assessment approach for analyzing potential spatial access to colorectal cancer services in Texas. App Geography. 2012;12:291–299. [Google Scholar]
- Wang F. Measurement, Optimization, and Impact of Health Care Accessibility: A Methodological Review. Ann Assoc Am Geogr. 2012;102(5):1104–1112. doi: 10.1080/00045608.2012.657146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang F, Luo W. Assessing spatial and nonspatial factors for healthcare access: towards an integrated approach to defining health professional shortage areas. Health Place. 2005;11:131–146. doi: 10.1016/j.healthplace.2004.02.003. [DOI] [PubMed] [Google Scholar]
- Weeks WB, Kazis LE, Shen Y, et al. Differences in Health-Related Quality of Life in Rural and Urban Veterans. American Journal of Public Health. 2004;94(10):1762–1767. doi: 10.2105/ajph.94.10.1762. [DOI] [PMC free article] [PubMed] [Google Scholar]