The health information technology movement focuses much of its energy on the use of electronic medical records by clinicians, but the use of information technology by patients carries equal promise. Outside of health care, the public routinely uses computers and smart phones to access information and perform tasks with a click of a button. Patients seek similar ease in accessing health information, but health care has been slow to develop information tools for patients of comparable functionality.1
A technology that could respond to this need is the personal health record. A model for shifting personal health records to become patient centered, which stratifies these interactions by arbitrarily defined levels, is depicted in the FIGURE. Initially, personal health records were merely an electronic substitute for the home medical file. The simplest function of the personal health record is to store similar information, often entered by the patient (first level). The user may be asked prompting questions about health behaviors and diagnoses, but the answers come mainly from the user’s memory or home records. Although patients are the ultimate authority on some details, such as eating habits and symptoms, they may not be as precise about diagnoses, medications, and laboratory values.
Figure.
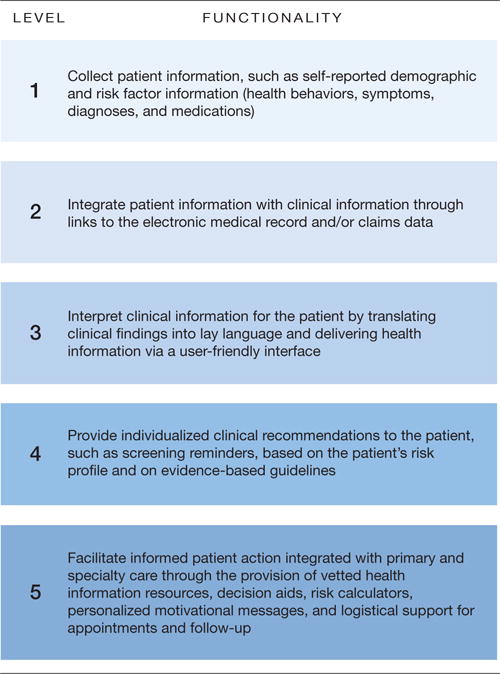
Potential Functionalities for a Patient-Centered Health Information System
More advanced personal health records address this problem by linking electronically to clinical information in electronic health records or claims data (second level).2 These systems provide a portal to clinical information, but too many deliver unmodified content to the patient, who may have difficulty understanding the terminology or putting the information in context. For example, a patient may not know whether to be concerned about a creatinine level outside of the normal reference range.
A higher function of personal health records is to interpret content—to explain technical information in language that patients easily understand (third level)—or to render clinical advice (fourth level), as when personal health records call attention to overdue screening tests or the need to reduce blood pressure or serum lipid levels.
The highest level of functionality is to help patients take action (fifth level). Information is plentiful on the Internet, but some personal health records give patients vetted information, such as a health encyclopedia or hyperlinks to useful resources. Some personal health records personalize information for the individual patient and some can incorporate motivational messages to help patients take action to confront challenges, such as weight loss or smoking. The personal health record offers a platform for applications, such as Framingham or Gail Model calculators or decision aids that help patients weigh difficult tradeoffs.3 By assisting with self-management, offering logistical support for appointments, and providing follow-up (eg, reminders), personal health records can extend care beyond the clinical encounter. This must be done in coordination with the patient’s physician, a level of functionality that many standalone systems lack.4 Trust comes when the personal health record has the endorsement of the physician and is designed to interface seamlessly with care delivery, as when output is shared and the personal health record refers patients back to their physician for assistance or helps them prepare for upcoming office visits.
No existing products do all of this. Relatively few patients use personal health records, perhaps because most products only have first- or second-level capabilities. Higher functionality exists in some high-end systems, but even these cannot deliver the full spectrum of services, and their developers report slow adoption.5,6 The typical personal health record takes an oversimplified approach, such as issuing a blanket reminder for mammograms without considering the many factors that influence whether screening is indicated. The power of smart technology enables personal health records to be far more refined and thereby more appealing to patients.
Personal health records that lack this sophistication are potentially harmful at every level of functionality. They can accept erroneous information from patients at the first level or from electronic health records at the second level. Patients who view unmodified content through a portal may be confused or experience undue anxiety without adequate context. At the third and fourth levels, the system’s explanation of findings and clinical advice may be spurious, depart from evidence-based guidelines, or include generic advice—correct for the general population, but wrong for the individual patient. At the fifth level, systems may refer patients to dubious resources, motivational messages may lack balance or scientific support, and recommendations may work at cross purposes with the clinician and disrupt care delivery.
The methodological and technical work to overcome these difficulties is formidable.7 For example, excellence at the fourth level requires the developer to apply reputable guidelines, program the output for diverse clinical scenarios, make updates as guidelines change, explain conflicting guidelines, and collect sufficient clinical data to properly individualize recommendations. Excellence at the fifth level requires exhaustive programming to personalize messages about numerous patient characteristics, provide cultural competency, identify appropriate self-management resources, and integrate with clinical workflows.
Solutions to these challenges are emerging in cutting-edge patient-centered systems that seek to deliver functions at the first through fifth levels. One such system, which helps patients to manage preventive and chronic care, collects relevant demographic and risk factor data from patients at the first level and clinical data from electronic health records at the second level, interprets the findings in lay language and an attractive user interface at the third level, personally advises patients of tests and other services recommended for their risk profile by the US Preventive Services Task Force and other major groups at the fourth level, and provides reference information from reputable sites, and adds tailored, motivational messages—all with the imprimatur of sponsoring primary care practices at the fifth level. In a recently completed randomized trial, 2250 patients who had been invited by practices to use this system were more up-to-date with preventive services than those who received usual care.8
Uptake of information technology by patients will languish until a new generation of systems is designed expressly to serve their needs at all levels of functionality. To be truly patient-centered, the technology must do more than help patients access health information—it must also interpret data from multiple sources and serve as a tool to facilitate action. The personal health record is a legacy term— the modern patient has more to do than keep records. Information technology holds great promise in empowering patients to manage their health, but the patient must become the focus of the design if the technology is to be used or fulfill its potential.
Acknowledgments
Funding/Support: This work was supported in part by grants R18 HS17046-01, R21 HS018811-01, and RFTO 17, 290-07-100113 from the Agency for Healthcare Research and Quality.
Role of the Sponsor: The sponsor had no role in the preparation, review, or approval of the manuscript.
Footnotes
Conflict of Interest Disclosures: Both authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. However, the development of the patient-centered system mentioned at the end of this Commentary has been supported by grants from the Agency for Healthcare Research and Quality. The sole conflict reported is that Virginia Commonwealth University holds intellectual property rights to the patient-centered system mentioned at the end of this Commentary. Although the university and developers are entitled to the system’s revenue, the system is a noncommercial product, and no revenues have been generated other than grant funding.
Additional Contributions: We thank Stephen Rothemich, MD, MS, and Anton Kuzel, MD, MPHE, Department of Family Medicine, and Daniel Longo ScD, and John Loomis, Virginia Commonwealth University, and Eric Peele at RTI International, Research Triangle Park, North Carolina, for contributing to the patient-centered health information system model, all of whom received salary support through grant funding.
References
- 1.Connecting for Health. Americans overwhelmingly believe electronic personal health records could improve their health. New York, NY: Markle Foundation; Jun, 2008. http://www.connectingforhealth.org/resources/ResearchBrief-200806.pdf. Accessed December 2010. [Google Scholar]
- 2.Tang PC, Ash JS, Bates DW, Overhage JM, Sands DZ. Personal health records: definitions, benefits, and strategies for overcoming barriers to adoption. J Am Med Inform Assoc. 2006;13(2):121–126. doi: 10.1197/jamia.M2025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.O’Connor AM, Légaré F, Stacey D. Risk communication in practice: the contribution of decision aids. BMJ. 2003;327(7417):736–740. doi: 10.1136/bmj.327.7417.736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tang PC, Lee TH. Your doctor’s office or the Internet? two paths to personal health records. N Engl J Med. 2009;360(13):1276–1278. doi: 10.1056/NEJMp0810264. [DOI] [PubMed] [Google Scholar]
- 5.Ralston JD, Coleman K, Reid RJ, Handley MR, Larson EB. Patient experience should be part of meaningful-use criteria. Health Aff (Millwood) 2010;29(4):607–613. doi: 10.1377/hlthaff.2010.0113. [DOI] [PubMed] [Google Scholar]
- 6.Silvestre AL, Sue VM, Allen JY. If you build it, will they come? the Kaiser Permanente model of online health care. Health Aff (Millwood) 2009;28(2):334–344. doi: 10.1377/hlthaff.28.2.334. [DOI] [PubMed] [Google Scholar]
- 7.Robinson TN, Patrick K, Eng TR, Gustafson D. Science Panel on Interactive Communication and Health. An evidence-based approach to interactive health communication: a challenge to medicine in the information age. JAMA. 1998;280(14):1264–1269. doi: 10.1001/jama.280.14.1264. [DOI] [PubMed] [Google Scholar]
- 8.Krist AH, Woolf SH, Rothemich SF, et al. Improving care through AHRQ health IT tools. http://www.ahrq.gov/about/annualconf10/krist_rosenthal/krist.HTM. Accessed December 22, 2010.


