Short abstract
This article investigates the characteristics of workplace wellness programs, their prevalence, their impact on employee health and medical cost, facilitators of their success, and the role of incentives in such programs.
Abstract
This article investigates the characteristics of workplace wellness programs, their prevalence, their impact on employee health and medical cost, facilitators of their success, and the role of incentives in such programs. The authors employ four data collection and analysis streams: a review of the scientific and trade literature, a national survey of employers, a longitudinal analysis of medical claims and wellness program data from a sample of employers, and five case studies of existing wellness programs in a diverse set of employers to gauge the effectiveness of wellness programs and employees' and employers' experiences.
Background
Over the last several decades, an epidemic of “lifestyle diseases” has developed in the United States: Unhealthy lifestyles, such as inactivity, poor nutrition, tobacco use, and frequent alcohol consumption, are driving up the prevalence of chronic disease, such as diabetes, heart disease, and chronic pulmonary conditions. These chronic conditions have become a major burden, as they lead to decreased quality of life, premature death and disability, and increased health care cost. Furthermore, although chronic disease was once thought to be a problem of older age groups, there is a shift toward onset during Americans' working age that adds to the economic burden, because of illness-related loss of productivity due to absence from work (absenteeism) and reduced performance while at work (presenteeism).
Out of concern about the impact of chronic disease on employee health and well-being, the cost of health care coverage, and competitiveness, employers are adopting health promotion and disease prevention strategies, commonly referred to as workplace wellness programs. Disease prevention programs aim either to prevent the onset of diseases (primary prevention) or to diagnose and treat disease at an early stage before complications occur (secondary prevention). Primary prevention addresses health-related behaviors and risk factors—for example, by encouraging a diet with lower fat and caloric content to prevent the onset of diabetes mellitus. Secondary prevention attempts to improve disease control—for example, by promoting medication adherence for patients with asthma to avoid symptom exacerbations that can lead to hospitalization. Health promotion is related to disease prevention in that it aims at fostering better health through behavior change. A broad range of benefits are offered under the label “workplace wellness,” from multi-component programs to single interventions, and benefits can be offered by employers directly, through a vendor, group health plans, or a combination of both.
Workplace wellness takes advantage of employers' access to employees at an age when interventions can still change their long-term health trajectory. The Patient Protection and Affordable Care Act (Affordable Care Act) supports this trend with several provisions regarding health promotion and also mandated this study.
Study Objectives and Research Approach
This article addresses the requirements of 2705(m)(1) of the Public Health Service Act and answers the following research questions:
What are the characteristics and prevalence of current workplace wellness programs?
What is the evidence for program impact?
What is the role of incentives under wellness programs?
What are key facilitators of successful wellness programs?
The project has four data collection and analysis streams:
a review of the scientific and trade literature to identify the prevalence of wellness programs, their key components, their use of incentives, their effectiveness, their return on investment, and best practices.
the RAND Employer Survey, a national survey of employers with at least 50 employees in the public and private sectors, including federal and state agencies, to assess program prevalence, type of wellness programs, information on incentives, and perceived program impacts.
statistical analyses of medical claims and wellness program data from a convenience sample of large employers in the Care Continuum Alliance (CCA) database to assess the effects of wellness programs on health and cost outcomes and the effect of incentives on program participation.
five case studies of existing wellness programs in a diverse set of employers to enhance our understanding of the effectiveness of wellness programs by providing specific examples and experiences of individual employers and employees.
Characteristics and Prevalence of Workplace Wellness Programs
According to the RAND Employer Survey conducted for this study, approximately half of U.S. employers offer wellness promotion initiatives, and larger employers are more likely to have more complex wellness programs. Programs often include wellness screening activities to identify health risks and interventions to reduce risks and promote healthy lifestyles. Most employers (72 percent of those offering a wellness program) characterize their wellness programs as a combination of screening activities and interventions. Wellness benefits can be offered by employers or a vendor to all employees or through their group health plans to plan members.
Screening activities use Health Risk Assessments (HRAs), self-administered questionnaires on health-related behaviors (e.g., exercise patterns) and risk factors (e.g., body weight) and may include clinical screenings to collect biometric data—for instance, height, weight, blood pressure, and blood glucose levels. The RAND Employer Survey data suggest that 80 percent of employers with a wellness program screen their employees for health risks, and our case study results show that employers use results for program planning and evaluation and for directing employees to preventive interventions that address their health risks.
Preventive interventions can aim at primary prevention by targeting employees with risk factors for chronic disease (lifestyle management) and at secondary prevention by improving disease control in employees with manifest chronic conditions (disease management). As Figure 1 shows, lifestyle management programs, which are offered by 77 percent of employers with a wellness program, target a broad range of risk factors, though nearly 80 percent offer nutrition and weight activities and 77 percent of employers offer smoking cessation programs. Similarly, all five case study employers offered some form of nutrition and weight loss intervention, such as onsite Weight Watchers group meetings, weight loss competitions, personalized phone support from health coaches, and smoking cessation activities through educational programs or telephonic counseling.
Figure 1.
Among Employers Offering a Lifestyle Management Program, Percentage Offering Specific Interventions
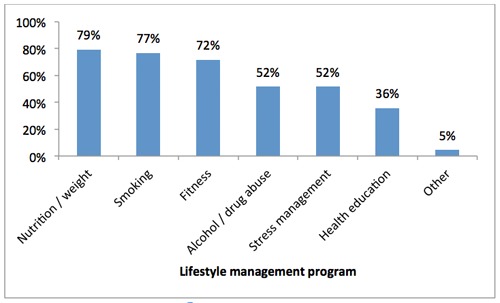
SOURCE: RAND Employer Survey, 2012.
NOTES: The graph represents information from employers with at least 50 employees that offer any lifestyle management intervention as a component of a wellness program. 51 percent of employers offer a wellness program, and 77 percent of those offer a lifestyle management intervention.
A wide variety of conditions is addressed through employer-sponsored disease management programs, as Figure 2 depicts: Disease management programs, which 56 percent of employers with wellness programs offer, most commonly target diabetes, followed by heart disease, chronic lung disorders, depression, and cancer.
Figure 2.
Among Employers Offering a Disease Management Program, Percentage Offering Programs for Specific Chronic Conditions
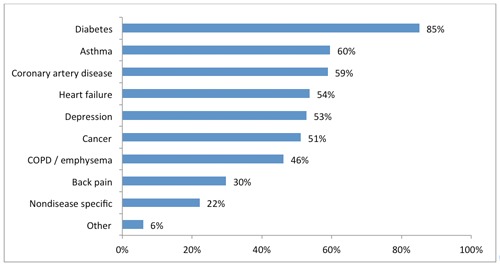
SOURCE: RAND Employer Survey, 2012.
NOTES: The graph represents information from employers with at least 50 employees that offer any disease management intervention as a component of a wellness program. 51 percent of employers offer a wellness program, and 56 percent of those offer a disease management intervention. COPD = chronic obstructive pulmonary disease.
Our survey results demonstrate that, in addition to those preventive interventions, employers offer health promotion activities (86 percent), such as on-site vaccinations, healthy food options, and other health and well-being related benefits (61 percent), such as Employee Assistance Plans and on-site clinics. Case study findings suggest that employers also use population-level strategies, like health-related campaigns and wellness events.
Evidence for Program Impact
Program Uptake
Our findings suggest that uptake of worksite wellness programs remains limited. According to the RAND Employer Survey, fewer than half of employees (46 percent) undergo clinical screening and/or complete an HRA, which are typically used to identify employees for interventions. Of those identified for an intervention based on screening results (for example, employees who report physical activity below their recommended level), a fifth or less chose to participate, as Figure 3 summarizes.
Figure 3.
Average Participation Rates of Employees Identified for Inclusion in Select Wellness Program Components
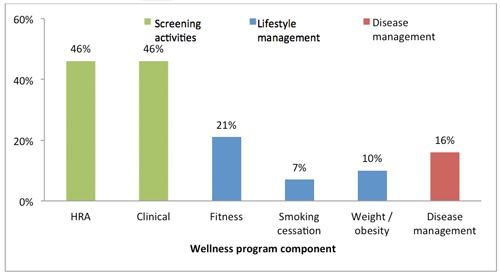
SOURCE: RAND Employer Survey, 2012.
NOTES: The graph represents information from employers with at least 50 employees that offer the specific component as part of a wellness program.
Program Impact on Health-Related Behaviors and Health Status
In an analysis of the CCA database, when comparing wellness program participants to statistically matched nonparticipants, we find statistically significant and clinically meaningful improvements in exercise frequency, smoking behavior, and weight control, but not cholesterol control. Those improvements are sustainable over an observation period of four years, and our simulation analyses point to cumulative effects with ongoing program participation. However, we caution that our analyses cannot account for unobservable differences between program participants and nonparticipants, such as differential motivation to change behavior.
51 percent of employers offer a wellness program; of those, 65 percent conduct an HRA, 49 percent offer clinical screenings, 55 percent have a fitness program, 59 percent have smoking cessation programs, 49 percent have weight/obesity management, and 56 percent have disease management interventions. In most cases, all employees are invited to participate in screening activities, but eligibility to participate in lifestyle and disease management interventions are based on risk factors identified through screenings and health conditions identified through medical claims data, respectively. Rates reflect employees who were determined eligible for each program component.
The results show that one year participation in a weight control program is significantly associated with a reduction of body mass index (BMI) (kg/m2) of about 0.15 in the same year, and the effect persists for two subsequent years. As illustrated in Figure 4, this change in the first three years corresponds to a weight loss of about 0.9 pound in an average woman of 165 pounds and five feet four inches in height, or about one pound in an average man of 195 pounds and five feet nine inches in height.
Figure 4.
Effect of One-Year Participation in a Weight Control Program on Body Weight in an Average Person
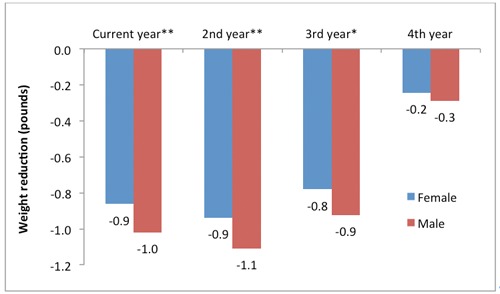
SOURCE: RAND analysis of health plan claims and screening and wellness program data in the CCA database, including 2005–2010 data from four employers and 3,924 propensity score matched pairs.
NOTES: The effects of program participation were translated to body weight reductions based on an average adult in the United States. According to the Centers for Disease Control, the average adult female is 63.8 inches tall and weighs 164.7 pounds; the corresponding numbers for an adult male are 69.4 inches and 194.7 pounds.
*p < 0.05; **p < 0.01.
The published literature, the results presented here, and our case studies corroborate the finding of positive effects of worksite wellness programs on health-related behavior and health risks among program participants. For example, a systematic review found that workplace interventions promoting smoking cessation, such as group and individual counseling and nicotine replacement therapy, increased smoking cessation rates compared to the control group. Other studies showed improvements in physical activity, higher fruit and vegetable consumption, and lower fat intake as well as a reduction in body weight, cholesterol levels, and blood pressure. One case study employer determined that roughly half of wellness program participants reported positive changes in their walking activities and eating habits, and a quarter of participants reported getting closer to a healthy weight.
Health Care Cost and Utilization
In the RAND Employer Survey, employers overwhelmingly expressed confidence that workplace wellness programs reduce medical cost, absenteeism, and health-related productivity losses. But at the same time, only about half stated that they have evaluated program impacts formally and only 2 percent reported actual savings estimates. Similarly, none of our five case study employers had conducted a formal evaluation of their programs on cost; only one employer had requested an assessment of cost trends from its health plan. Our statistical analyses suggest that participation in a wellness program over five years is associated with a trend toward lower health care costs and decreasing health care use. We estimate the average annual difference to be $157, but the change is not statistically significant (Figure 5).*
Figure 5.
Estimated Cumulative Effect of Wellness Program Participation on Total Monthly Medical Costs
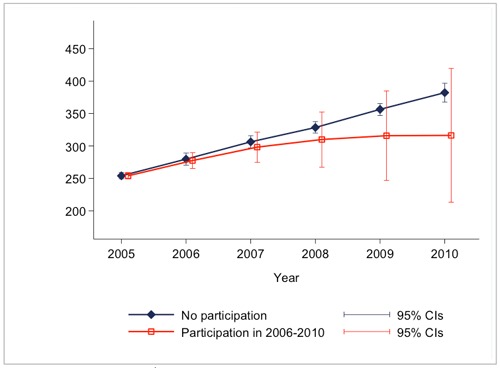
SOURCE: RAND analysis of health plan claims and screening and wellness program data in the CCA database.
NOTES: Simulation results are based on continuous participation in 2006–2010 of a population with the average characteristics of the estimation sample; p > 0.05 for all years in 2006–2010. CL = confidence interval.
Role of Incentives in Workplace Wellness Programs
Regulations on the Use of Incentives in Workplace Wellness Programs
A number of laws and regulations at the federal and state level impose requirements and regulate the use of financial incentives in certain types of wellness programs. With respect to certain employment-based wellness programs requiring that individuals satisfy health-related standards, the Health Insurance Portability and Accountability Act (HIPAA) and the Affordable Care Act, among other things, limit incentives and require the availability of a reasonable alternative standard for certain wellness programs if for an individual it is medically inadvisable to, or it is unreasonably difficult to, achieve the standard. The Affordable Care Act raises the permissible limit on incentives for achieving a health-related standard from the prior limit of 20 percent of the cost of coverage to 30 percent in 2014. In addition, final rules being contemporaneously published at the time of this article** allow employers with wellness programs designed to prevent or reduce tobacco use to charge tobacco users up to 50 percent more in premiums than nonusers (Federal Register, 2012).
Incentives may be provided in various forms, such as premium discounts, waivers of cost-sharing requirements, or improved benefits. However, incentives that require employees to meet a health-related standard, such as target body weight, may not exceed these limits when administered by an employer's group health plan, irrespective of whether the incentives take the form of a reward, a penalty, or a combination of both. Incentives that are not tied to a health-related standard, such as participation in a diagnostic testing program, are not held to these incentive limits, so long as the incentive is available to all similarly situated individuals, and comply with other applicable federal laws, such as the Genetic Information and Nondiscrimination Act (GINA) and the Americans with Disabilities Act (ADA), and state laws.
Overall Use and Administration of Incentives
The RAND Employer Survey results indicate that nationally, more than two-thirds of employers (69 percent) with at least 50 employees and workplace wellness programs use financial incentives to encourage program uptake, and 10 percent use incentives that are tied to health-related standards. About half of employers (49 percent) with wellness programs offer incentives directly to all employees,*** whereas 31 percent administer them through their group health plans. A fifth of employers (20 percent) administer incentives both directly and through their plans. Larger employers are more likely than smaller employers to administer their incentive schemes themselves.
We also find that results-based incentives are more commonly administered by the employer directly rather than through the health plan and linked to health coverage. According to the RAND Employer Survey, about 7 percent of employers that offer wellness programs reported administering results-based incentives through their health plans (Figure 6). The average amount of results-based incentives for these employers was less than 10 percent of the total cost of health coverage, far from the current regulatory threshold.
Figure 6.
Percentage of Employers with Wellness Programs Using Participation and Results-Based Incentives for Selected Health Behaviors
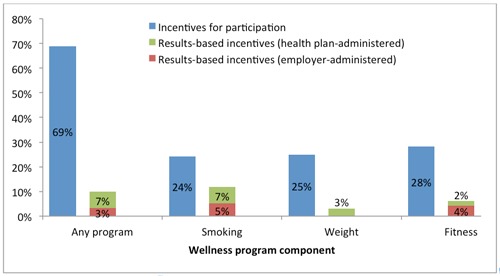
SOURCE: RAND Employer Survey, 2012.
NOTES: The graph represents information from employers with at least 50 employees with wellness programs or which offer lifestyle management as a component of a wellness program. 51 percent of employers offer a wellness program, and 77 percent of those have lifestyle management. Among employers with a lifestyle management intervention, 77 percent offer programs that target smoking, 79 percent target weight management, and 72 percent offer fitness programs.
Incentives for Participation in Screenings and Interventions
According to the RAND Employer Survey, the most common types of incentive triggers are HRA completion and participation in lifestyle management interventions; each is offered by about 30 percent of employers with a wellness program.
Incentives are typically framed as rewards, with 84 percent of employers reportedly using rewards rather than penalties. Incentives are offered in financial form (e.g., cash or health insurance premium surcharges) and novelty items (e.g., t-shirts or gift cards). Novelty items were used by nearly half of all employers who offer any incentives. Gym discounts (42 percent) and cash incentives (21 percent) were cited as common ways to reward program participants and/or health-related behaviors. Four out of five employers in our case studies reported using some form of financial incentive, and all five employers used novelties (e.g., t-shirts, tickets to events, and coffee mugs) as a strategy to engage employees (see Table 1)
Table 1.
Percentage of Employers That Offer Monetary Incentives to Encourage Participation in Wellness Activities
| Type of Component | % of All Employers That Offer a Wellness Program | % of All Employers |
|---|---|---|
| HRA completion | 31 | 16 |
| Clinical screening | 20 | 10 |
| Lifestyle management | 30 | 15 |
| Disease management | 4 | 2 |
| At least one component | 69 | 35 |
SOURCE: RAND Employer Survey, 2012.
NOTE: The table represents the subset of employers with at least 50 employees that offer a wellness program (51 percent).
According to the RAND Employer Survey, employers use incentives to increase employee participation in wellness screening activities (31 percent for HRA completion and 20 percent for clinical screenings) and encourage employees to join intervention programs (30 percent for lifestyle management and 4 percent for disease management). Employers who use incentives for screening activities report significantly higher participation rates than those who do not (63 percent versus 29 percent for HRA completion and 57 percent versus 38 percent for clinical screenings).
Analysis of the CCA data indicates that incentives for HRA completion are effective, particularly above a threshold of $50. Using a simulation model, we find that the incentive amount for HRA completion had a significant effect on HRA completion rates. On average, we estimate that an increase in the HRA incentive by $10 is associated with a 1.6 percentage point increase in the HRA completion rate for incentives in the range of $0–$100.
Incentives for Changes in Behavior and Health Standards
Data from the RAND Employer Survey indicate that smoking cessation is the behavior that is primarily targeted with incentives tied to health standards.**** About a fifth of employers with smoking cessation programs (19 percent) reward actual smoking cessation, almost as many as those that reward program participation (21 percent). For other behaviors (e.g., diet), in contrast, employers were three to four times more likely to reward participation in programs than behavior change or outcomes.
Smoking is also the only health risk behavior for which achieving the goal is rewarded with a higher incentive than participation in a program. According to the RAND Employer Survey, the average incentive ($682, or 12.6% of cost of insurance coverage*****) paid for stopping tobacco use is more than triple the incentive paid for program participation ($203). Similarly, four out of five case study employers penalized smokers, but only two had incentives tied to other health standards. The peer-reviewed literature indicates that financial incentives may attract individuals to enroll or participate in smoking cessation programs and increase initial quit rates, but they generally do not achieve long-term behavior change (Cahill and Perera, 2011; Osilla et al., 2012). Results from one randomized control trial found that large incentives (of up to $750 over the course of a year) were effective in improving abstinence rates, even when incentives were no longer offered (Volpp et al., 2009). See Figure 7.
Figure 7.
Average Incentive Amounts to Target Select Health Behaviors Among Employers Offering Incentives
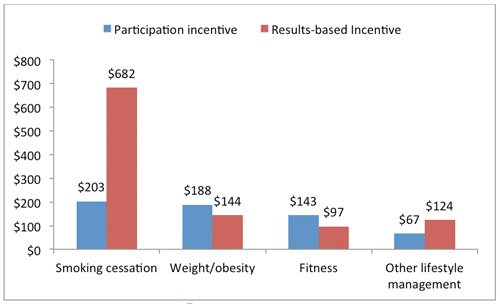
SOURCE: RAND Employer Survey, 2012.
NOTES: The graph represents information from employers with at least 50 employees that offer a monetary incentive for participation in a lifestyle management intervention or for improving health behaviors. 51 percent of employers offer a wellness program, and 77 percent of those include a lifestyle management intervention. Among employers with lifestyle management interventions, 77 percent target smoking, 79 percent target weight and obesity, and 72 percent target fitness.
With respect to effectiveness, our analyses of employer data in the CCA database imply that incentives for HRA completion and program participation can significantly reduce weight and smoking rates and increase exercise. However the size of these effects is small and unlikely to be clinically meaningful.******
Key Facilitators of Successful Wellness Programs
Five factors to promote wellness program success emerged from our case study analysis and the literature review:
Effective communication strategies: All five organizations in our case studies employ strategies to communicate wellness program information to employees, ranging from face-to-face interaction to mass dissemination. Employers cited the importance of broad outreach and clear messaging from organizational leaders, especially for those organizations with a large and geographically dispersed workforce.
Opportunity for employees to engage: Those included in the case study discussions revealed that making wellness activities convenient and easily accessible for all employees are strategies that employers use to raise the level of employee engagement. Some focus group participants cited limited access to wellness benefits because of wait times and rigid work schedules.
Leadership engaged at all levels: Evidence from case studies suggests that for programs to be a success, senior managers need to consider wellness an organizational priority to shift the company culture. Buy-in from direct supervisors is crucial to generate excitement and connect employees to available resources.
Use of existing resources and relationships: All organizations in our case studies leverage existing resources and build relationships, often with health plans, to expand offerings at little to no cost.
Continuous evaluation: Organizations from our case studies approach wellness with a continuous quality improvement attitude. Though no employers from our case studies conducted formal evaluations, all five solicit feedback from staff with the goal of improving future wellness programming. Three employers conducted needs assessments to develop an understanding of the wellness needs of their workforce.
Conclusions
This project represents the most comprehensive analysis of worksite wellness programs to date and evaluates current program participation, program effects, and the role of incentives. Our project combined a literature review, a national survey of employers, case studies of workplace wellness programs, and statistical analyses of medical claims and program data to assess the current use of workplace wellness programs in the United States, to estimate the effect of programs on employee health and health care cost, and to evaluate the role of incentives in program engagement.
Characteristics and Prevalence of Workplace Wellness Programs
We find that that workplace wellness programs have emerged as a common employer-sponsored benefit that is now available at about half of U.S. employers with 50 or more employees, a group that employs three-quarters of the U.S. workforce. Large employers are more likely than small employees to offer a wellness program and also tend to offer programs with a greater variety of options. Most employers are committed to long-term support of wellness programs, regarding them as a viable strategy to contain health care costs, thereby ensuring the affordability of health coverage. In spite of their popularity among employers, the impact of wellness programs are rarely formally evaluated.
Evidence on Program Impact
Consistent with prior research, we find that lifestyle management interventions as part of workplace wellness programs can reduce risk factors, such as smoking, and increase healthy behaviors, such as exercise. We find that these effects are sustainable over time and clinically meaningful. This result is of critical importance, as it confirms that workplace wellness programs can help contain the current epidemic of lifestyle-related diseases, the main driver of premature morbidity and mortality as well as health care cost in the United States. An important question for further research is how program design and implementation can improve program effects.
Our estimates of wellness program effects on health care cost are lower than most results reported in the literature, but we caution that our approach estimated the isolated effect of lifestyle management interventions, whereas many published studies captured the effect of an employer's overall approach to health and wellness. Although we do not detect statistically significant decreases in cost and use of emergency department and hospital care, the trends in health care costs und use of high-cost care for program participants and nonparticipants diverge over time. Therefore, there is reason to believe that a reduction in direct medical costs would materialize if employees continued to participate in a wellness program. Lacking access to proprietary information on program cost, we could not estimate program effects on overall cost of coverage directly, but judging by published program cost data, the programs would be cost-neutral after five program years (Baicker, Cutler, and Song, 2010).
Role of Incentives in Workplace Wellness Programs
Since limited employee engagement is regarded as an important obstacle to program success, employers are using incentives to increase employee engagement, as the RAND Employer Survey and other surveys suggest. Our statistical analyses show that incentives of over $50 appear effective in getting employees to complete an HRA. Although we cannot assess the effect of higher incentives systematically, as $100 was the maximum amount used by the employers in the CCA database, case study evidence suggests that larger incentives can be effective, such as the $50 per week that Employer D in our case studies used to achieve almost 100 percent participation in onsite clinical screenings. Modest incentives also seem to increase participation in and impact of lifestyle management programs.
The use of incentives tied to health standards remains uncommon. The RAND Employer Survey shows that nationally, only 10 percent of employers with 50 or more employees that offer a wellness program use any such incentives, and only 7 percent link the incentives to premiums for health coverage. For this subset, maximum incentive amounts average less than 10 percent of the employee premium for health care coverage. The one health risk factor for which results-based incentives are more common and involve higher amounts is smoking, as suggested by both the RAND Employer Survey and our case studies.
Limitations
We need to caution that our survey results may be subject to response bias, as some characteristics of respondents and nonrespondents differed significantly. Further, both the external and internal validity of the results based on the CCA data may be limited. The database represents a convenience sample of employers with long-standing commitment and substantial investment into wellness programs, implying that results may not be generalizable to all employers. As with any nonexperimental design, we cannot fully rule out that unobservable differences between program participants and nonparticipants have influenced our results. For example, differential motivation may have contributed to our estimated effect on health behaviors, such as exercise and smoking. Finally, the limited variation in incentive use among the employers in the CCA database prevents us from reaching definite conclusions regarding the effect of incentives on wellness program participation, health behaviors, and outcomes.
Opportunities for Future Research
This project represents the most comprehensive analysis of worksite wellness programs to date, and it evaluates current program participation, program impact, and the role of incentives. It also helps us to identify priority areas for future research:
Long-term impact of wellness programs. Given the long latency between health risks and development of manifest chronic diseases, a much longer follow-up period will be required to fully capture the effect of worksite wellness programs on health outcomes and cost.
Design of programs. Research is needed on program design features that are most likely to achieve wellness goals. Smoking cessation is an area where additional research could inform program development. A more granular look at different program components would provide valuable insights into the determinants of program success. For example, such analyses could compare the differential effects of modalities for program delivery (e.g., telephone, Internet, and in-person). Research into the relative impact of individual-level and workforce-level interventions could help to increase program efficiency.
Impact on a broad range of measures. Future studies should look at a broader range of outcomes, in particular work-related outcomes and health-related quality of life. Work-related outcomes, such as absenteeism, productivity, and retention, are of critical importance to employers as they directly affect business performance.
Contextual factors that modify program impact. Contextual factors will influence the effectiveness and cost-effectiveness of workplace wellness interventions. Employer characteristics, such as workplace culture and leadership support, might modify the effect of wellness programs. Understanding the role of such modifying factors should be considered for future research. Similarly, we need to understand better how employee demographic characteristics drive decisions about program uptake and how those factors interact with financial incentives.
Effect of financial incentives. “High-powered” incentives that tie a substantial proportion of the cost of coverage to specific health standards remain rare. Thus, comprehensive evaluation of the intended and unintended effects of such incentives and different incentive amounts may require a prospective or even experimental study. In addition, there is limited information on the differential impact of different incentive types (e.g., whether rewards have a different effect from penalties and whether premium reductions have a different effect from cash payments) and of changes in incentives over time.
Notes
Our sample size implies that the study was adequately powered to detect an average annual change in health care cost of $378, which is well within the range of previously published estimates.
The Departments of Health and Human Services, Labor, and the Treasury issued a Notice for Proposed Rulemaking regarding incentives for nondiscriminatory wellness programs in group health plans on November 26, 2012 (Federal Register, 2012). Final rules regarding incentives for nondiscriminatory wellness programs in group health plans are being contemporaneously published with this article (Federal Register, 2013).
HIPAA, wellness program rules, and the Affordable Care Act wellness program provisions relating to incentives for nondiscriminatory wellness programs apply with respect to incentives offered through both self-funded and insured group health plan coverage. Although Incentives that are not offered through group health plan coverage would not be subject to these requirements, other nondiscrimination and privacy laws may still apply with respect to employer practices relating to wellness programs operated outside the group health plan context.
To reduce the burden on respondents, the survey did not ask employers to specify in detail whether incentives are offered under their group health plans.
According to KFF/HRET (2011), “The average premium for single coverage in 2011 is $452 per month or $5,429 per year.”
Based on the Framingham Heart Study general cardiovascular disease risk model (Framingham Heart Study, undated), the effects of an incentive of $100 on BMI and smoking translate to an avoidance of 11.5 cases cardiovascular disease per 10,000 population in male and 2.3 cases in female, over a ten-year period.
Reference
- Baicker, K., Cutler D., et al. (2010). “Workplace wellness programs can generate savings.” Health Affairs 29 (2): 304–311. [DOI] [PubMed] [Google Scholar]
- Cahill, K., and Perera R. (2011). “Competitions and incentives for smoking cessation.” Cochrane Database of Systematic Reviews (4): CD004307. [DOI] [PubMed]
- Federal Register (2012). Incentives for Nondiscriminatory Wellness Programs in Group Health Plans. Washington, D.C. Proposed Rule: 77 Fed. Reg, 70620-70642. [PubMed]
- Federal Register (2013). Incentives for Nondiscriminatory Wellness Programs in Group Health Plans. Washington, D.C.: Final Rule: [Contemporaneously published]. [PubMed]
- Framingham Heart Study, “General CVD Risk Prediction,” undated. As of August 13, 2013: http://www.framinghamheartstudy.org/risk/gencardio_bmi.xls
- KFF/HRET (2011). Employer Health Benefits: 2011 Annual Survey. Menlo Park, Calif; Chicago, Ill.: Kaiser Family Foundation/Health Research and Educational Trust. [Google Scholar]
- Osilla, K. C., Van Busum K., et al. (2012). “Systematic review of the impact of worksite wellness programs.” The American Journal of Managed Care 18 (2): e68–e81. [PubMed] [Google Scholar]
- Volpp, K. G., Troxel A. B., et al. (2009). “A randomized, controlled trial of financial incentives for smoking cessation.” The New England Journal of Medicine 360 (7): 699–709. [DOI] [PubMed] [Google Scholar]


