Abstract
Since late 2001, U.S. military forces have been engaged in conflicts around the globe, most notably in Iraq and Afghanistan. These conflicts have exacted a substantial toll on soldiers, marines, sailors, and airmen, and this toll goes beyond the well-publicized casualty figures. It extends to the stress that repetitive deployments can have on the individual servicemember and his or her family. This stress can manifest itself in different ways—increased divorce rates, spouse and child abuse, mental distress, substance abuse—but one of the most troubling manifestations is suicide, which is increasing across the U.S. Department of Defense (DoD). The increase in suicides among members of the military has raised concern among policymakers, military leaders, and the population at large. While DoD and the military services have had a number of efforts under way to deal with the increase in suicides among their members, the Assistant Secretary of Defense for Health Affairs asked RAND to review the current evidence detailing suicide epidemiology in the military, identify “state-of-the-art” suicide-prevention programs, describe and catalog suicide-prevention activities in DoD and across each service, and recommend ways to ensure that the activities in DoD and across each service reflect state-of-the-art prevention science.
Since late 2001, U.S. military forces have been engaged in conflicts around the globe, most notably in Iraq and Afghanistan. These conflicts have exacted a substantial toll on soldiers, marines, sailors, and airmen, and this toll goes beyond the well-publicized casualty figures. It extends to the stress that repetitive deployments can have on the individual servicemember and his or her family. This stress can manifest itself in different ways—increased divorce rates, spouse and child abuse, mental distress, substance abuse—but one of the most troubling manifestations is suicides, which are increasing across the U.S. Department of Defense (DoD). The increase in suicides among members of the military has raised concern among policymakers, military leaders, and the population at large. While DoD and the military services have had a number of efforts under way to deal with the increase in suicides among their members, they have also asked what more might be done and posed this question to the RAND National Defense Research Institute (NDRI). DoD asked NDRI to do the following:
Review the current evidence detailing suicide epidemiology in the military.
Identify “best-practice” suicide-prevention programs.
Describe and catalog suicide-prevention activities in DoD and across each service.
Recommend ways to ensure that the activities in DoD and across each service reflect best practices.
The RAND research team approached this task by reviewing all relevant policy and materials, as well as through key informant interviews with persons knowledgeable about suicide-prevention activities within DoD and with experts in the field of suicidology.
The Epidemiology of Suicide in the Military
The RAND research team took an epidemiological approach to answering questions of keen interest to DoD policymakers.
What Is the Suicide Rate in Military Services?
Suicide rates are typically reported in number of cases per 100,000 people. Figure 1 shows the suicide rate among active-duty personnel for each military service and for DoD overall and reflects the published rate among active-duty military through 2008. It shows that, in 2008, the U.S. Marine Corps (USMC) and the U.S. Army have the highest rates (19.5 and 18.5, respectively), and the Air Force and the Navy have the lowest rates (12.1 and 11.6, respectively).
Figure 1.
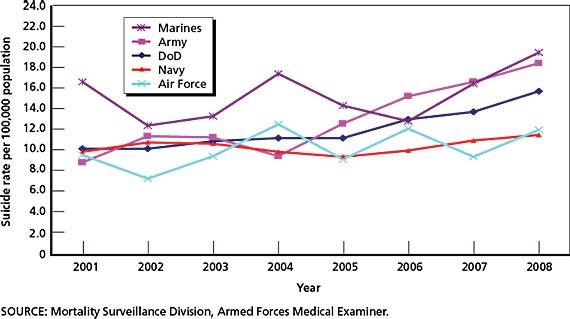
U.S. Department of Defense and Service Suicide Rates, 2001–2008
The figure also indicates that the suicide rate across DoD has been climbing, rising from 10.3 in 2001 to 15.8 in 2008, which represents about a 50-percent increase. The increase in the DoD suicide rate is largely attributable to a doubling of the rate in the Army. There is evidence that the suicide rate in DoD in calendar year (CY) 2007 was higher than those in CYs 2001 and 2002. There is also evidence that the rate in CY 2008 was higher than the annual rate between CYs 2001 and 2005 and higher than the average rate for CYs 2001 through 2008. Across services, there are significant differences in only the Army's suicide rate over time. Specifically, the Army suicide rates for CYs 2006 and 2007 were higher than in 2001 and 2004, and the rate in CY 2008 was higher than in it was between CY 2001 and CY 2005 and higher than the average rate for CYs 2001 through 2008.
How Does the Military Suicide Rate Compare with That of the U.S. Population?
An important question is how the rate in the military compares with that of the general population. The estimated annual suicide rate in the general population for 2001–2006 hovers at around 10 per 100,000 (CDC, 2010), notably lower than that in DoD. But these populations are not necessarily comparable, because the military and the national population differ so much in terms of age, sex, and racial makeup and, in part, because the procedures for reporting suicide data also vary, both between states and regions and between the nation and DoD. To derive a comparable population, RAND researchers calculated an adjusted suicide rate for a synthetic national population having the same demographic profile as DoD personnel and as each service. Figure 2 shows the results of comparing DoD with the comparable segment of the U.S. population for the years 2001–2006 (the most recent year for which data are available about suicides in the general U.S. population is 2006; see CDC, 2010). These results show that the suicide rate in the synthetic civilian population is both fairly constant and substantially higher than that in DoD. Of concern, however, is that the gap between DoD and the general population is closing. The most-pronounced increases in the DoD suicide rate occurred in 2007 and 2008, so, assuming that the national rate remains relatively stable in these years, the gap between the rate in DoD and the general population may be even narrower.
Figure 2.
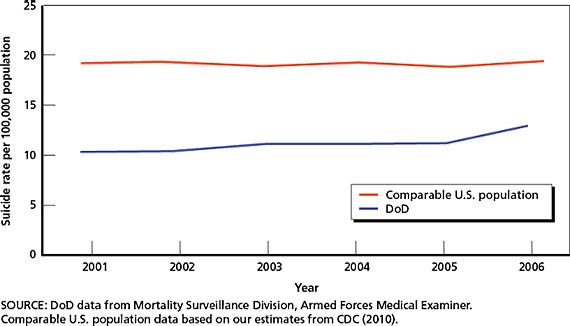
Suicides in Adjusted U.S. Population and U.S. Department of Defense
Who Dies by Suicide in the Military?
One of the reasons that the synthetic population rates presented in Figure 2 are higher than in the general population is because they represent the demographic profile of servicemembers in DoD, who are disproportionately male. In the United States, males are more likely to die by suicide than females—thus, the expected suicide rate based on this demographic characteristic alone is higher than for the country as a whole.
Who Is at Risk?
A review of the scientific literature revealed that those who are at a higher risk of dying by suicide fall into the following categories.
Prior Suicide Attempts. Although the majority of suicide deaths occur on individuals' first attempts and the majority of those who make a nonfatal suicide attempt do not go on to die by suicide, a prior suicide attempt is the strongest predictor of subsequent death by suicide (Isometsä and Lönnqvist, 1998; Harris and Barraclough, 1997).
Mental Disorders. Certain mental disorders that carry an increased risk of suicide, such as schizophrenia, are of minimal concern to the military because many learning, psychiatric, and behavioral disorders are cause for rejection at enlistment and during training. However, the continuing deployments of U.S. military personnel to Iraq and Afghanistan have highlighted the emergence of specific mental health concerns that are relevant to this population: depression and anxiety disorders (including posttraumatic stress disorder, or PTSD). The Institute of Medicine (IOM) estimates that approximately 4 percent of those with depression will die by suicide (Goldsmith et al., 2002), and, though the same figure is not yet known for those with PTSD, community-based surveys indicate that persons with PTSD are more likely than those without the disorder to report past suicide attempts and ideation (Kessler, Borges, and Walters, 1999; Sareen et al., 2005; Farberow, Kang, and Bullman, 1990).
Substance-Use Disorders. People with substance-use disorders and heavy users of alcohol and other drugs face an increased risk for suicide, depending on the presence of a disorder and the type of drug that they use. While drug use is not prevalent in the military largely due to routine screening, approximately 20 percent of servicemembers report heavy alcohol use (drinking five or more drinks per typical drinking occasion at least once per week) (Bray and Hourani, 2007).
Head Trauma/Traumatic Brain Injury (TBI). Evidence also indicates that persons with concussions, cranial fractures, or cerebral contusions or traumatic intracranial hemorrhages had higher rates of suicide mortality than the general population (Teasdale and Engberg, 2001; Simpson and Tate, 2002, 2005). TBI is of particular concern among deployed military personnel who may sustain blast or other concussive injuries as a result of an explosion or blast of an improvised explosive device (IED).
Those Suffering from Hopelessness, Aggression and Impulsivity, and Problem-Solving Deficits. Although mental and substance-use disorders are common among those who die by suicide, the majority of those with such disorders do not die this way (Harris and Barraclough, 1997; Wilcox, Conner, and Caine, 2004; Goldsmith et al., 2002). Researchers have conducted studies to see how persons with the same mental disorders differ with respect to a history of suicide attempts and death by suicide. Those with high levels of hopelessness are at increased risk, and there is some evidence that higher levels of aggression and impulsivity, as well as those with problem-solving deficits, are also at increased risk for suicide (McMillan et al., 2007; Mann et al., 1999; Rudd, Rajab, and Dahm, 1994).
Life Events, Precipitating Events, and Triggers. There is some concern about specific life events (e.g., death of family member, relationship problems) among servicemembers who die by suicide. While there is some evidence suggesting that particular life events differentially increase the risk of suicide (Luoma and Pearson, 2002), such studies have not been conducted among military personnel. Most of the scientific literature suggests that it is the interaction with underlying vulnerabilities, such as behavioral health problems, that influence a suicidal response to these relatively common events (Yen et al., 2005; Joiner and Rudd, 2000).
Firearm Access. Consistent evidence indicates that availability of firearms correlates positively with suicide (Matthew Miller, Lippmann, et al., 2007; Matthew Miller, Azrael, et al., 2006). Military personnel have access to firearms, particularly when deployed, and are more likely to own a personal gun than are members of the general population (Hepburn et al., 2007). Thus, military personnel who are considering suicide are more likely to have access to a firearm, one of the most lethal ways people can kill themselves.
Suicides of Others and Reporting of Suicides. For youth and young adults, there is evidence of contagion—that a suicide may lead to subsequent suicides (Insel and Gould, 2008). There is evidence of suicide clusters primarily among teens (Gould, 1990; Gould, Wallenstein, and Kleinman, 1990; Gould, Wallenstein, Kleinman, et al., 1990), though such clusters generally account for less than 5 percent of youth suicides (Insel and Gould, 2008). Media reporting of suicides, particularly coverage that lasts for a long time, is featured prominently, and is covered extensively in newspapers, is also associated with increases in suicide (Gould, 2001), though adhering to media guidelines on such reporting can mitigate any possible contagion (Pirkis et al., 2006).
Best Practices
RAND researchers reviewed a wide range of prevention programs, assessing them for their application to the military. These programs included universal programs that target entire populations and selected or indicated programs that focus on specific groups at high risk. They also considered self-care (i.e., maintaining one's personal health), making the environment safer, and postvention, which refers to the way an organization or media outlet treats a death by suicide. Taken together, these programs form a continuum of prevention activities ranging from programs delivered on a broad scale at a relatively small cost per person to treatment programs delivered to few at high expense.
The challenge in identifying best practices for suicide prevention is the lack of data on the effectiveness of programs. A best practice for suicide prevention would be one supported by empirical evidence showing that it causally reduced suicides. Currently, only a handful of programs would meet this definition. The bulk of the strong evidence about effectiveness concentrates at the selected prevention end of the spectrum, focusing on interventions or treatments for those who have displayed past suicidal behavior or those deemed to be at increased risk for suicide.
Universal programs with specific suicide-prevention activities generally fall into two categories: those that raise awareness and teach skills and those that provide screening and referral for mental health problems and suicidal behavior. Selected programs also fall into two categories: those that target groups at high risk by virtue of a known risk factor (e.g., mental illness) and those that work directly with suicide attempters who come to the attention of health providers because of their suicidal behavior. Environmental safety programs attempt to identify the means by which people kill themselves in a particular population and then to make these means less available. Examples of such initiatives include policies that restrict access to firearms to prevent self-inflicted gunshot wounds, use of blister packs (which require an individual to extract each pill from a sealed plastic pocket) for lethal medications to prevent intentional overdoses, bridge safeguards to prevent fatal falls, and constructing shower-curtain rods so as to prevent fatal hangings. Postvention efforts primarily have to do with establishing rules and responsibilities for community organizations following a suicide. Postvention also includes training the media on guidelines for proper reporting of suicides to reduce the possibility of imitative suicides. Such training includes not glorifying the death or describing the means by which suicide victims ended their lives.
Our assessment of these various programs indicates that promising practices exist, but much remains unknown about what constitutes a best practice. Our assessment of the literature and conversations with experts in the field indicate that a comprehensive suicide-prevention program should include the following six practices:
Raise awareness and promote self-care. One clear finding that emerges from the literature is that a focus on skill building may be important at all stages of prevention. Reducing known risk factors, such as substance abuse and mental health problems, is often included as one aspect of integrated approaches.
Identify those at high risk. Selected or indicated prevention is a fundamental component of a public health approach to disease prevention and is predicated on identifying those at higher risk. Thus, a comprehensive suicide-prevention program should have means by which this may occur, such as screening for mental health problems, one of the strongest risk factors for suicide, in primary care or through the use of gatekeepers.
Facilitate access to quality care. Access to quality behavioral health care is an integral component of many suicide-prevention programs. Past research highlights that a number of barriers obstruct such access, including some barriers that are specific to the military. Although reducing barriers to mental health care has not been specifically correlated with reducing suicides except as part of broad, integrated programs, facilitating access to effective care will help ensure that those at increased risk will receive quality care and thus reduce suicides.
Provide quality care. The types of interventions with the strongest empirical support for effectively preventing suicide involve quality mental health treatment and specific interventions focused on suicidality. The need to ensure quality of behavioral health services is a critical and often overlooked component of suicide prevention.
Restrict access to lethal means. There is evidence that restricting access to lethal means is an effective way to prevent suicide. Universal means restriction might be difficult in the U.S. military, with weapons readily available to deployed soldiers. However, selected or indicated programs that limit gun availability to persons deemed to be at high risk of suicide should be considered.
Respond appropriately. Given evidence of possible imitative suicides, suicide-prevention programs must have in place a strategy for responding to a suicide. Such a strategy should focus on how details of the suicide are communicated in the media, as well as how the information is passed on to groups to which the deceased individual belonged (e.g., classmates, colleagues, military unit).
Suicide Prevention in the U.S. Department of Defense and Across the Services
Each of the services is engaged in a variety of suicide-prevention activities. For each service, we amassed information on the underlying philosophy (stated or not) behind that service's suicide-prevention program, and a description of programs and initiatives along with information about how each service supports suicide-prevention activities (i.e., official documentation bearing on suicide, organizations responsible for suicide prevention, how suicide-prevention programs and initiatives are funded).
Suicide Prevention in the U.S. Department of Defense
There are five cross-service suicide-prevention initiatives sponsored by DoD. First, the DoD Suicide Prevention and Risk Reduction Committee is a committee of key stakeholders, including each service's suicide-prevention program manager (SPPM), that meets monthly to provide input on policy, develop joint products, and share information. Second, in 2008, the Defense Centers of Excellence for Psychological Health and Traumatic Brain Injury (DCoE) began funding the Real Warriors Campaign, a public education initiative to address the stigma of seeking psychological care and treatment. Third, in 2009, DoD established a congressionally directed DoD Task Force on the Prevention of Suicide by Members of the Armed Forces, which is expected to release its findings in the summer or fall of 2010. Fourth, in 2008, all services began conducting surveillance on suicide events (suicides and attempts or ideation that results in hospitalization or evacuation) using the same surveillance tool: the Department of Defense Suicide Event Report (DoDSER). Finally, since 2002, DoD has sponsored an annual suicide-prevention conference; in 2009 and 2010, the conference was jointly sponsored by DoD and the U.S. Department of Veterans Affairs (VA).
Suicide Prevention in the Army
The Army's current approach to suicide prevention revolves around programs that encourage “soldiers to take care of soldiers” and those that offer a holistic approach to promote resiliency. This information is dispensed primarily through public awareness campaigns and training and education offered to both leaders and soldiers. The message is exemplified by the Army's Ask, Care, Escort (ACE) program that serves as the cornerstone of most current suicide-prevention efforts. Resiliency programs are offered to persons before deploying and upon returning from deployment. New approaches to facilitate access to care include public-awareness campaigns designed to eliminate stigma associated with seeking behavioral health-care treatment and locating behavioral health-care professionals in nontraditional settings, such as primary care and in theater.
In the past, the Deputy Chief of Staff for Army Personnel (G-1) provided the funding required for the Army Suicide Prevention Program (ASPP) to execute its suicide-prevention mission. However, since the establishment of the Suicide Prevention Task Force in March 2009 and the added emphasis placed on suicide prevention, there is a dedicated line of funding in the Army's fiscal year (FY) 2011 budget for suicide prevention and some elements that support it. Nonetheless, suicide-prevention activities are developed, managed, and run across multiple organizations within the Army, including the suicide-prevention program office within G-1 and the U.S. Army Center for Health Promotion and Preventive Medicine (CHPPM, which is in the process of changing to the U.S. Army Public Health Command; see APHC, 2010), Deputy Chief of Staff for Army Operations (G-3), and from such senior leaders as the Vice Chief of Staff of the Army.
Suicide Prevention in the Navy
The Navy's approach to suicide prevention is guided by a model that sees stress on a continuum and in which suicide represents an extreme endpoint on the continuum. The model emphasizes early intervention to prevent and manage stress, particularly in the face of challenging life events (e.g., relationship or financial difficulties). This information is conveyed via media campaigns and educational programs and trainings, the cornerstone of which is Operational Stress Control. The Navy also places behavioral health-care providers in nontraditional settings, such as providing community-based outreach coordinators for reservists or placing psychologists on aircraft carriers.
The majority of suicide-prevention initiatives in the Navy are funded by the responsible agencies and organizations, though there will be some dedicated funding for suicide prevention in FY 2010. The Navy SPPM serves in this capacity on a part-time basis.
Suicide Prevention in the Air Force
The Air Force approach to preventing suicide is based on initiating cultural changes in attitudes and actions pertaining to suicide and implementing these changes through the highest-ranking Air Force officials. The program is comprised of 11 tenets outlined in an Air Force pamphlet (AFPAM 44–160). These tenets require training and education for all airmen, but also include policies and procedures for monitoring individuals for suicidal behavior following an investigative interview and, in these cases, protect the confidentiality of those receiving treatment from a psychotherapist. The Air Force program also established entities at the installation, major command (MAJCOM), and Air Force levels called the Integrated Delivery System (IDS), which is a conglomeration of Air Force organizations engaged in suicide prevention and related activities that organize and coordinate prevention programs and are guided by the Community Action Information Boards (CAIBs). Guidance to Air Force behavioral health-care providers on assessing and managing suicidal risk is provided through a published guide created by the Air Force and a one-time training that was offered in 2007 with an accompanying plan for sustainment via chain-teaching. There is published evidence to suggest that the implementation of the Air Force Suicide Prevention Program (AFSPP) was associated with a 33-percent risk reduction in suicide (Knox et al., 2003). It has been reviewed by the National Registry of Evidence-Based Programs and Practices, which found that research methods were strong enough to support these claims (SAMHSA, 2010).
Agencies and organizations are responsible for using internal funds to support their responsibilities outlined for that organization, though there is also a full-time Air Force SPPM and a dedicated stream of funding for suicide prevention.
Suicide Prevention in the Marine Corps
The Marine Corps approach to suicide prevention relies primarily on programs in which members of the USMC community are trained to identify and refer marines at risk for suicide to available resources (e.g., a commander, chaplain, mental health professional). The core of the Marine Corps approach occurs via education and training that all marines receive annually both during their required martial-arts training and from their local commands. Special training is offered to all new marines (officers and enlisted) and their drill instructors, front-line leaders (noncommissioned officers [NCOs] and lieutenants), and civilian employees who have regular direct contact with a large proportion of the force. Public-awareness messages disseminated via videos, posters, and brochures aim to reduce the stigma of getting help. Behavioral health providers and chaplains who serve marines were also offered a one-time voluntary training on assessing and managing suicidal risk. Finally, there is also a program to support marines before, after, and during deployment, and behavioral health professionals are embedded in infantry regiments to increase marines' access to behavioral health services.
Agencies and organizations are responsible for using internal funds to support the responsibilities outlined for that organization, though there is also a full-time Marine Corps SPPM and four full-time staff dedicated to suicide prevention at USMC Headquarters.
Conclusions
We assessed how each of the services was performing across the six domains of a comprehensive suicide-prevention program. Their performance is outlined in Figure 3.
Figure 3.
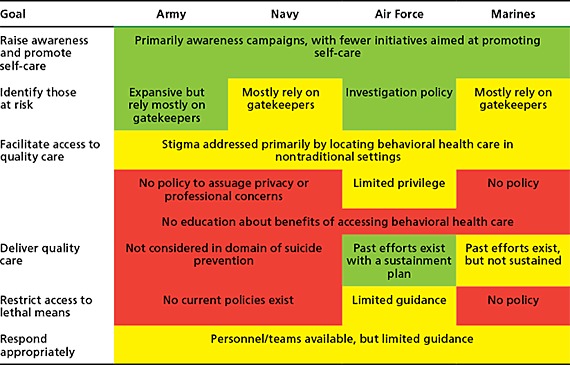
Assessment of Suicide-Prevention Activities Across Services
Raise Awareness and Promote Self-Care
The services use media campaigns, training and educational courses, and messages from key personnel to raise awareness and promote self-care. Most of the messages conveyed focus on raising awareness, which has limited evidence of creating behavior change. Across services, there are fewer messages disseminated with respect to promoting self-care; those that do exist are generally geared toward deploying personnel or those returning from deployments. Few programs teach strategies to help servicemembers build skills that would help them care for themselves, including the ability to self-refer when needed.
Identify Those at High Risk
The Army, Navy, and Marine Corps generally rely on “gatekeepers” to identify people at increased risk for suicide and actively refer those in distress to follow-up care. There is insufficient evidence to date indicating that these training programs are effective at reducing suicides. An alternative strategy for identifying those at high risk of suicide is to monitor the aftermath of high-risk events. The Air Force does this by monitoring those under investigation, and the Army, Navy, and Air Force all have programs that attempt to monitor servicemembers after deployment to mitigate potentially negative consequences of deployment. The Army and Air Force also have programs that promote mental health screening in primary care. Only the Air Force and Marines have trained behavioral health-care professionals in suicide risk assessment and management, which some experts we interviewed considered to be a promising practice.
Programs aimed at identifying those at high risk should be based on research that discerns those at high risk; the Army is actively pursuing research that could provide information about Army-specific risk factors, and the Air Force has a consultation tool by which any Air Force commander can request an investigation to assess his or her unit's well-being.
Facilitate Access to Quality Care
Across the services, most of the initiatives in place to facilitate access to quality care fall under the domain of eliminating stigma: Initiatives that raise awareness about suicide and promote self-care can reduce stigma, as can locating behavioral health care in nontraditional settings, including in primary care and in theater. There are fewer initiatives focused on assuaging servicemembers' career and privacy concerns, and there are few initiatives under the purview of suicide prevention that seek to dispel myths about the ineffectiveness of behavioral health care, both of which are well-established barriers to such care among military personnel, though such information is conveyed in the Air Force's and Marine Corps' annual training. In addition, the recently launched Real Warriors campaign does begin to fill this gap.
Provide Quality Care to Those in Need
Providing quality care is a fundamental component of suicide prevention. It was beyond the scope of the current research project to evaluate the quality of care offered by behavioral health-care providers, though only the Air Force and Marine Corps made us aware of programs aimed at improving the skills of behavioral health-care providers with respect to assessing and managing suicidal patients. However, in both services, these programs were one-time offerings with no plan for additional training. But the Air Force teaches this material informally in its internship and residency programs, as well as by providing a manual, training videos, and assessment measures to each clinic.
Restrict Access to Lethal Means
Across the services, there are no known specific policies in place in which access to lethal means is restricted for the purposes of reducing suicides, either universally or for those at increased or imminent risk of suicide. The Air Force provides limited guidance to leaders on means restriction when managing personnel in severe distress.
Respond Appropriately to Suicides and Suicide Attempts
Each service has a team or personnel on whom leaders can call to assist them after a suicide specifically or traumatic event more generally. However, no policies or guidance provide details on what should be done if and when a unit experiences the loss of one of its own to suicide.
Recommendations
We make 14 recommendations pertinent to all services:
Track suicides and suicide attempts systematically and consistently. The recent initiatives to use the DoDSER and establish a common nomenclature across all services will help ensure that communication on suicide is consistent within DoD and foster information sharing between the services. However, this will also require that the services and each installation are using the same criteria for determining who requires a DoDSER.
Evaluate existing programs and ensure that new programs contain an evaluation component when they are implemented. Evaluation provides a basis for decisionmaking and helps ensure that resources are used effectively and to achieve anticipated outcomes. Current initiatives should be evaluated, and an evaluation plan should be a required component of any new initiative.
Include training in skill building, particularly help-seeking behavior, in programs and initiatives that raise awareness and promote self-care. Most universal prevention programs in the services focus on raising awareness about suicide, provide resources to which a servicemember can turn when he or she (or someone he or she knows) is feeling suicidal, and may include messages about the importance of peer gatekeepers. There is no evidence to indicate that any of these strategies is effective on its own. A limitation of these kinds of programs is that they do not teach the skills that servicemembers may need to refer themselves to behavioral health professionals or chaplains.
Define the scope of what is relevant to preventing suicide, and form partnerships with the agencies and organizations responsible for initiatives in other areas. Behavioral health problems (e.g., mental disorders, harmful substance-using behaviors) are risk factors for suicide, and prevention efforts across all of these domains have the potential to affect suicides in DoD. Thus, it is important that suicide-prevention programs within each service create partnerships with the organizations responsible for these other areas to ensure consistent messaging, create jointly sponsored projects, and avoid duplication.
Evaluate gatekeeper training. The services rely heavily on gatekeeper training, a prevention technique for which there is no evidence of effectiveness (though for which there have been few evaluations). Gatekeeper training is intuitively appealing because it can reach a wide number of people, and the use of nonmilitary gatekeepers might help reduce the stigma associated with recognizing and referring a peer in uniform. On the other hand, it may send the message that suicide is always another person's problem, and some individuals will not be good gatekeepers and should not be relied on to serve in this capacity. Servicemembers may also not intervene out of fear that their actions could jeopardize a fellow servicemember's military career. Evaluation of gatekeeper programs is needed to help clarify these issues.
Develop prevention programs based on research and surveillance; selected and indicated programs should be based on clearly identified risk factors specific to military populations and to each service. Most services produce reports that provide descriptive information about servicemembers who have killed themselves but cannot identify the factors that actually place individuals at risk of killing themselves, which would require a well-defined control group. Identifying risk factors is critical in the development of selected and indicated prevention programs, which are important components of a public health approach to suicide prevention.
Ensure that continuity of services and care are maintained when servicemembers or their caregivers transition between installations in a process that respects servicemembers' privacy and autonomy. Because military personnel transition frequently between installations and commands, as well as between active and reserve status, it is important that they know of the resources available at each new command. For those receiving formal behavioral health care or counseling from a chaplain, efforts should be made to help ensure that the servicemember continues to receive the necessary care when he or she (or his or her caregiver) transfers. We recommend that patients themselves manage this process, with support from behavioral health-care providers and chaplains. For example, behavioral health-care providers and chaplains should provide clients moving to a new installation with the contact information for analogous resources at the new installation, encourage their clients to make appointments soon after arriving, and occasionally check in with them.
Make servicemembers aware of the benefits of accessing behavioral health care and specific policies and repercussions for accessing such care, and conduct research to inform this communication. Military personnel share a widespread belief that behavioral health care is ineffective and a concern that seeking behavioral health care could harm their career. There are no explicit policies with respect to repercussions across the services for accessing this care. Research is needed to discern the effect that seeking behavioral health care has on a servicemember's military career.
Make servicemembers aware of the different types of behavioral health caregivers available to them, including information on caregivers' credentials, capabilities, and the confidentiality afforded by each. The behavioral health-care workforce in the military is diverse and varies with respect to education, licensing, and certification or credentialing. Each service also relies heavily on chaplains who are embedded in military units and often serve as front-line responders for persons under psychological or emotional duress. Educating military personnel about the differences among referral specialists with respect to each professional's credentials and professional capabilities is important. Also, each provider is responsible for knowing what type of care he or she is capable of providing and to refer as appropriate. Confidentiality is noted to be a specific barrier to care among this population and is not uniform across providers: For example, chaplains offer total confidentiality, but command staff has access to information about servicemembers' access of professional mental health services (i.e., care offered in a clinical setting). Servicemembers should therefore also be made aware of the confidentiality afforded by different organizations and individuals.
Improve coordination and communication between caregivers and service providers. Those who offer behavioral health care should work as a team to ensure that the emotional well-being of those for whom they care is maintained. There were conflicting reports about the relationship between these professionals on military bases. For example, some interviewees reported open communication and collegiality between chaplains and behavioral health-care providers, while others reported a more acrimonious relationship. Improved communication and collaboration between professionals helps create a trustworthy hand-off to ensure that individuals do not fall through the cracks when going from one form of care to another.
Assess whether there is an adequate supply of behavioral health-care professionals and chaplains available to servicemembers. Effective suicide prevention in the military will rely on persons accessing quality behavioral health care and counseling. Messages promoting these resources assume a capacity of providers and chaplains who can deliver quality care to those who request it. There appears to be a need for research to address this concern: Chaplains, for example, reported that they thought they were understaffed, though they did not have empirical basis for this assumption. There is also a shortage of behavioral health-care providers in the United States generally, and DoD has faced challenges in recruiting and retaining adequately trained behavioral health-care providers.
Mandate training on evidence-based or state-of-the-art practices for behavioral health generally and in suicide risk assessment specifically for chaplains, health-care providers, and behavioral health-care professionals. Programs that promote behavioral health-care providers and chaplains often operate under the assumption that these individuals are sufficiently trained in assessing and managing suicidal patients. Unfortunately, this assumption may not be valid: Few providers are adequately trained in effective ways to assess risk and manage patients at varying levels of risk. Guides do exist that, while not evidence-based, offer helpful guidelines to providers. Both the Air Force and Marine Corps have independently conducted training, but these efforts were one-time occurrences with no future plans. There is also an implicit assumption that these professionals are trained to provide more general high-quality care and counseling. Unfortunately, research from the civilian sector indicates that the provision of quality care for behavioral health is not universal across mental health-care providers, and there is no reason to think that services in the military are any different. There is almost no evidence on the quality of counseling offered by chaplains. The quality of mental health care and counseling offered in DoD is unknown, and efforts to improve quality, such as training providers in evidence-based practice, are not integrated into the system of mental health care offered in DoD treatment facilities. Training all health-care providers on mental health awareness and quality behavioral health care is also an important component of provider training.
Develop creative strategies to restrict access to lethal means among military servicemembers or those indicated to be at risk of harming themselves. A comprehensive suicide-prevention strategy should have considered ways to restrict access to the means by which servicemembers could try to end their own lives. Due to the prevalence of firearms as a means by which military servicemembers die by suicide, initiatives to restrict access to firearms should be considered. Although restricting firearms among military personnel seems daunting or even impossible, there is some precedent for such policies in both the Veterans Health Administration (VHA) and DoD. In particular, selected or indicated prevention strategies may include restricting access to firearms specifically among those identified to be at risk of harming themselves.
Provide formal guidance to commanders about how to respond to suicides and suicide attempts. Responding to a suicide appropriately not only can help acquaintances of the suicide victim grieve but also can prevent possible imitative suicides, as well as serve as a conduit to care for those at high risk. Across services, there is no direct policy regarding appropriate ways in which a leader should respond to a suicide within his or her unit. Fear of imitative suicides may also hinder many leaders from openly discussing suicides in their units. There also needs to be guidance for leaders to help care for and integrate servicemembers back into units who have made suicide attempts or expressed suicidal ideation, as there are anecdotal reports of servicemembers being ostracized or ridiculed after seeking behavioral health care or having been treated for suicidal behavior. Not only does this increase the risk of another suicide attempt, but it also creates a hostile and stigmatizing environment for others in the unit who may be under psychological or emotional duress.
Suicide is a tragic event, though the research suggests that it can be prevented. The recommendations represent the ways in which the best available evidence suggests that some of these untimely deaths could be avoided.
Reference
- AFPAM 44–160—see U.S. Department of the Air Force (2001).
- APHC—see U.S. Army Public Health Command (Provisional).
- Bray, Robert M., and Hourani Laurel L., “Substance Use Trends Among Active Duty Military Personnel: Findings from the United States Department of Defense Health Related Behavior Surveys, 1980–2005,” Addiction, Vol. 102, No. 7, July 2007, pp. 1092–1101. [DOI] [PubMed] [Google Scholar]
- CDC—see Centers for Disease Control and Prevention.
- Centers for Disease Control and Prevention, “Welcome to WISQARS™,” last updated March 4, 2010. As of November 17, 2009: http://www.cdc.gov/injury/wisqars/
- Farberow, N. L., Kang H. K., and Bullman T. A., “Combat Experience and Postservice Psychosocial Status as Predictors of Suicide in Vietnam Veterans,” Journal of Nervous and Mental Disease, Vol. 178, No. 1, January 1990, pp. 32–37. [DOI] [PubMed] [Google Scholar]
- Goldsmith, Sara K., Pellman T. C., Kleinman A. M., and Bunney W. E., eds., Reducing Suicide: A National Imperative, Washington, D.C.: National Academies Press, 2002. [PubMed]
- Gould, Madelyn S., “Teenage Suicide Clusters,” Journal of the American Medical Association, Vol. 263, No. 15, April 18, 1990, p. 2051. [PubMed] [Google Scholar]
- Gould, Madelyn S., “Suicide and the Media,” Annals of the New York Academy of Sciences, Vol. 932, April 2001, pp. 200–221; discussion pp. 221–204. [DOI] [PubMed] [Google Scholar]
- Gould, Madelyn S., Wallenstein Sylvan, and Kleinman Marjorie, “Time-Space Clustering of Teenage Suicide,” American Journal of Epidemiology, Vol. 131, No. 1, January 1990, pp. 71–78. [DOI] [PubMed] [Google Scholar]
- Gould, Madelyn S., Wallenstein Sylvan, Kleinman Marjorie H., O'Carroll P., and Mercy J., “Suicide Clusters: An Examination of Age-Specific Effects,” American Journal of Public Health, Vol. 80, No. 2, February 1990, pp. 211–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris, E. C., and Barraclough B., “Suicide as an Outcome for Mental Disorders: A Meta-Analysis,” British Journal of Psychiatry, Vol. 170, March 1997, pp. 205–228. [DOI] [PubMed] [Google Scholar]
- Hepburn, L., Miller M., Azrael D., and Hemenway D., “The US Gun Stock: Results from the 2004 National Firearms Survey,” Injury Prevention, Vol. 13, No. 1, February 2007, pp. 15–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Insel, Beverly J., and Gould Madelyn S., “Impact of Modeling on Adolescent Suicidal Behavior,” Psychiatric Clinics of North America, Vol. 31, No. 2, June 2008, pp. 293–316. [DOI] [PubMed] [Google Scholar]
- Isometsä, E. T., and Lönnqvist J. K., “Suicide Attempts Preceding Completed Suicide,” British Journal of Psychiatry, Vol. 173, December 1998, pp. 531–535. [DOI] [PubMed] [Google Scholar]
- Joiner, Thomas E. Jr., and Rudd M. David, “Intensity and Duration of Suicidal Crisis Vary as a Function of Previous Suicide Attempts and Negative Life Events,” Journal of Consulting and Clinical Psychology, Vol. 68, No. 5, October 2000, pp. 909–916. [DOI] [PubMed] [Google Scholar]
- Kessler, R. C., Borges G., and Walters E. E., “Prevalence of and Risk Factors for Lifetime Suicide Attempts in the National Comorbidity Survey,” Archives of General Psychiatry, Vol. 56, No. 5, July 1999, pp. 617–626. [DOI] [PubMed] [Google Scholar]
- Knox, Kerry L., Litts David A., Talcott G. Wayne, Feig Jill Catalano, and Caine Eric D., “Risk of Suicide and Related Adverse Outcomes After Exposure to a Suicide Prevention Programme in the US Air Force: Cohort Study,” BMJ, Vol. 327, No. 7428, December 13, 2003, p. 1376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luoma, Jason B., and Pearson Jane L., “Suicide and Marital Status in the United States, 1991–1996: Is Widowhood a Risk Factor?” American Journal of Public Health, Vol. 92, No. 9, September 2002, pp. 1518–1522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mann, J. John, Waternaux Christine, Haas Gretchen L., and Malone Kevin M., “Toward a Clinical Model of Suicidal Behavior in Psychiatric Patients,” American Journal of Psychiatry, Vol. 156, February 1999, pp. 181–189. [DOI] [PubMed] [Google Scholar]
- McMillan, Dean, Gilbody Simon, Beresford Emma, and Neilly Liz, “Can We Predict Suicide and Non-Fatal Self-Harm with the Beck Hopelessness Scale? A Meta-Analysis,” Psychological Medicine, Vol. 37, No. 6, June 2007, pp. 769–778. [DOI] [PubMed] [Google Scholar]
- Miller, Matthew, Azrael Deborah, Hepburn L., Hemenway David, and Lippmann Steven J., “The Association Between Changes in Household Firearm Ownership and Rates of Suicide in the United States, 1981–2002,” Injury Prevention, Vol. 12, No. 3, June 2006, pp. 178–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller, Matthew, Lippmann Steven J., Azrael Deborah, and Hemenway David, “Household Firearm Ownership and Rates of Suicide Across the 50 United States,” Journal of Trauma, Vol. 62, No. 4, April 2007, pp. 1029–1034; discussion pp. 1034–1025. [DOI] [PubMed] [Google Scholar]
- Mortality Surveillance Division, Armed Forces Medical Examiner System—see Pearse, 2006.
- Pearse, Lisa, “Numbers Count: Apples, Oranges and the Occasional Banana,” Mortality Surveillance Division, Armed Forces Medical Examiner System, Armed Forces Institute of Pathology, undated briefing. As of March 8, 2010: http://www.ha.osd.mil/2008mspc/downloads/NumbersCount-PearseApr08-red_POST_Pearse.pdf [Google Scholar]
- Pirkis, Jane, Blood R. Warwick, Beautrais Annette, Burgess Philip, and Skehan Jaelea, “Media Guidelines on the Reporting of Suicide,” Crisis, Vol. 27, No. 2, 2006, pp. 82–87. [DOI] [PubMed] [Google Scholar]
- Rudd, M. David, Rajab M. Hasan, and Dahm P. Fred, “Problem-Solving Appraisal in Suicide Ideators and Attempters,” American Journal of Orthopsychiatry, Vol. 58, No. 1, January 1994, pp. 136–149. [DOI] [PubMed] [Google Scholar]
- SAMHSA—see Substance Abuse and Mental Health Services Administration.
- Sareen, J., Houlahan T., Cox B. J., and Asmundson G. J., “Anxiety Disorders Associated with Suicidal Ideation and Suicide Attempts in the National Comorbidity Survey,” Journal of Nervous and Mental Disease, Vol. 193, No. 7, July 2005, pp. 450–454. [DOI] [PubMed] [Google Scholar]
- Simpson, Grahame, and Tate Robyn, “Suicidality After Traumatic Brain Injury: Demographic, Injury and Clinical Correlates,” Psychological Medicine, Vol. 32, No. 4, 2002, pp. 687–697. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration, “NREPP: SAMHSA's National Registry of Evidence-Based Programs and Practices,” last updated February 18, 2010. As of March 11, 2010: http://www.nrepp.samhsa.gov/
- U.S. Army Public Health Command (Provisional), “Clinical Features of Suicide Attempts After Traumatic Brain Injury,” Journal of Nervous and Mental Disease, Vol. 193, No. 10, October 2005, pp. 680–685. [DOI] [PubMed] [Google Scholar]
- Teasdale, T. W., and Engberg A. W., “Suicide After Traumatic Brain Injury: A Population Study,” Journal of Neurology, Neurosurgery and Psychiatry, Vol. 71, No. 4, 2001, pp. 436–440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of the Air Force, The Air Force Suicide Prevention Program: A Description of Program Initiatives and Outcomes, Air Force pamphlet 44–160, April 2001. As of March 8, 2010: http://afspp.afms.mil/idc/groups/public/documents/afms/ctb_056459.pdf
- U.S. Army Public Health Command (Provisional), home page, last updated April 7, 2010. As of March 30, 2010: http://usachppm.apgea.army.mil/APHC
- Wilcox, Holly C., Conner Kenneth R., and Caine Eric D., “Association of Alcohol and Drug Use Disorders and Completed Suicide: An Empirical Review of Cohort Studies,” Drug and Alcohol Dependence, Vol. 76, Suppl. 1, December 7, 2004, pp. S11–S19. [DOI] [PubMed] [Google Scholar]
- Yen, S., Pagano M. E., Shea M. T., Grilo C. M., Gunderson J. G., Skodol A. E., McGlashan T. H., Sanislow C. A., Bender D. S., and Zanarini M. C., “Recent Life Events Preceding Suicide Attempts in a Personality Disorder Sample: Findings from the Collaborative Longitudinal Personality Disorders Study,” Journal of Consulting and Clinical Psychology, Vol. 73, No. 1, February 2005, pp. 99–105. [DOI] [PMC free article] [PubMed] [Google Scholar]


