Abstract
Insurers and purchasers of health care in the United States are on the verge of potentially revolutionary changes in the approaches they use to pay for health care. Recently, purchasers and insurers have been experimenting with payment approaches that include incentives to improve quality and reduce the use of unnecessary and costly services. The Patient Protection and Affordable Care Act of 2010 is likely to accelerate payment reform based on performance measurement. This article provides details of the results of a technical report that catalogues nearly 100 implemented and proposed payment reform programs, classifies each of these programs into one of 11 payment reform models, and identifies the performance measurement needs associated with each model. A synthesis of the results suggests near-term priorities for performance measure development and identifies pertinent challenges related to the use of performance measures as a basis for payment reform. The report is also intended to create a shared framework for analysis of future performance measurement opportunities. This report is intended for the many stakeholders tasked with outlining a national quality strategy in the wake of health care reform legislation.
Background
Insurers and purchasers of health care in the United States are on the verge of potentially revolutionary changes in the approaches they use to pay for health care (Rosenthal, 2008). While the traditional fee-for-service payment model has been altered or joined by payment reforms, including prospective payment for hospitals in the 1980s and health plan and medical group capitation in the 1990s, critics continue to assert that the persistent use of fee-for-service payment is increasing the volume and intensity of services without enhancing the quality of care or its efficiency. Specifically, fee-for-service payment may contribute to the overuse of services with little or no health benefit and does not foster coordination of care across providers or care delivery organizations (Miller, 2009; Mechanic and Altman, 2009).
Recently, purchasers and insurers have been experimenting with payment approaches that include incentives to improve quality and reduce the use of unnecessary and costly services (Mechanic and Altman, 2009; Fisher et al., 2009; Lee, Berenson, and Tooker, 2010). The federal government has given a new impetus to these payment approaches within the Patient Protection and Affordable Care Act (PPACA) of 2010 (Thorpe and Ogden, 2010). These payment approaches are designed to achieve two interrelated goals: quality improvement and cost containment (Figure 1). Cost containment is to be achieved by reversing the incentives under fee-for-service payment to increase the use of services by shifting some amount of financial risk to providers, spurring them to consider the costs of their decisions. The introduction of financial risk in payment models may have mixed consequences for quality. On the one hand, financial risk may promote high quality by motivating providers to reduce rates of overuse of inappropriate services. On the other hand, financial risk may lead providers to reduce services that are important to high-quality care or impede access to care.
Figure 1.

Goals of Payment Reform Models
To address the risks to quality that may emerge in the transition away from fee-for-service payment, proposed new payment reform models (PRMs) do more than simply introduce new ways to pay for services. They include explicit measures of quality and tie payment to performance on those measures so that quality improvement will be driven by financial incentives to providers for the use of clinically appropriate services, efforts to make care more patient-centered through coordination and integration of a patient's care among providers, and incentives to invest in patient safety.
As this discussion implies, PRMs will have to be designed and implemented carefully in order to ensure that both the cost containment and quality goals are achieved. Furthermore, performance measurement and reporting are a crucial component of new payment models. The potential reliance on performance measures to address both cost containment and quality goals is already placing new demands on the performance measure development enterprise. Measures will be needed to perform several important functions in new payment systems, including two that are central to this report:
Setting performance-based payment incentives. New PRMs typically create performance incentives by adjusting payment amounts based on measured performance (e.g., determining whether a payment occurs and the amount of a payment or determining nonpayment for services if they are linked to poor-quality care).
Protecting against unintended adverse consequences of cost containment. PRMs may create unintended adverse consequences, such as avoidance of some high-risk or high-cost patients by providers, other barriers to access, and underuse of evidence-based services. Measurement approaches will be needed to identify and ameliorate these unintended consequences.
The purpose of this report is to provide information about the current status of performance measurement in the context of payment reform and to identify near-term opportunities for performance measure development. The report is intended for the many stakeholders tasked with outlining a national quality strategy in the wake of health care reform legislation. Through a subcontract to the National Quality Forum (NQF), a team of investigators at RAND used a rigorous and selective process to create a catalog of payment reform programs that includes both demonstration projects and those outlined in legislation. Based on the features of these programs, each was categorized into one of 11 PRMs. Next, each model and its programs were analyzed to describe the rationale for performance measurement, identify the performance measures available to the model, and assess its unmet measure needs. Finally, a set of near-term measure development opportunities and implementation challenges were explored to inform the direction of future measure development.
The uses of performance measurement and reporting in health care are a vast and complex topic. Performance measures have many other functions in addition to their use to set payment incentives. Of necessity, this report focuses on the two functions noted above and limits the scope of discussion to these functions. The report does not address the following issues:
Measures of “financial performance,” such as total spending on services or resource use that may be used by payers to negotiate payment amounts with providers, are not addressed. These “accounting” measures are a focus of the report only if they are closely linked to quality measures within an efficiency framework.
-
Other applications of performance measurement and reporting are not addressed unless they are an intrinsic part of the PRMs. These other applications include the use of performance measures to
monitor progress toward improvement goals
inform consumers and purchasers to enable selection of providers
stimulate competition among providers
stimulate innovation
promote the “values” of the health system.
Variations in the implementation of actual incentives and the distribution of payments between health plans, hospitals, provider groups, and individual providers are beyond the scope of the report. Many payment models are complex and not yet fully specified, making it difficult to assume any special configuration of payers, providers, and incentives. However, where such configurations would affect performance measure development and implementation, we note this.
PRMs relevant to hospitals, physicians, and other medical providers are emphasized. Long-term care, home health, ambulatory surgery, and many other delivery organizations are obviously critically important. These organizations have participated in payment reform experiments, and they are addressed in health reform legislation. Nevertheless, to make the scope of the discussion manageable, we have elected to focus on hospital and physician PRMs. Results and lessons from these models could be applicable to payment reform programs developed for these other organizations.
Key Findings
Payment Reform Models
We identified and catalogued 90 payment reform programs, classifying them into 11 general PRMs.
The PRMs are diverse with respect to the targeting of payment to performance goals, the bundling of services, and the level at which payment is made to organizations and individual providers.
While three types of care delivery entities have been prominently featured in PRMs (the hospital, the ambulatory group practice, and the individual physician), performance-based payment reform will involve other types of providers (long-term care, ambulatory surgical centers, and others).
Payment reform programs frequently blend elements of the 11 PRMs.
Additional blending of PRMs seems likely as programs are implemented in the future.
Implications of the Use of Performance Measurement to Support the Emerging Payment Reform Models
The number and sophistication of measures in use varies widely across programs within each PRM, suggesting ongoing experimentation to determine optimal approaches.
Many available performance measures are not yet in use in current payment reform programs.
Measure development should be guided by a longitudinal care framework rather than a focus on discrete clinical services.
Complex organizational types may benefit from complex measurement strategies that support internal incentive and quality improvement models.
Composite measures will be important, especially in assessing episodes of care.
Efficiency-of-care measures may be useful in PRMs that are not based on global or capitated payment.
Blended payment models will rely on blended performance measurement strategies.
Structure-of-care measures will be required for some models, at least in the near term.
Priority Areas for Further Measure Development
The following measure types offer promising opportunities for further measure development and refinement across many of the PRMs we identified:
-
health outcome measures that can be used to assess care for populations:
health status measures (functional status and quality of life)
safety outcomes (preventable harms attributable to health care)
care coordination measures (including measures that assess care transitions)
measures of patient and caregiver engagement (measures that assess the participation of patients and caregivers in their care)
measures of structure (particularly management measures and health information technology [HIT] utilization measures that address new organizational types)
composite measures that combine outcome, process, structure, patient experience, cost, and other measure types
efficiency measures that combine quality and resource use measures.
To minimize the risk that new PRMs will increase disparities in care, additional measure development may be useful in two specific areas:
clinical and sociodemographic risk profiles of providers' patient populations
measures of access to care and measures to detect provider avoidance of high-risk patients.
Project Methods
The goal of the project was to describe the performance measurement needs created by current and emerging payment reform approaches, to assess the suitability of existing performance measures to support these needs, and to suggest near-term priority areas for performance measure development that would support these needs effectively going forward. To achieve the goal, RAND, in consultation with NQF staff, carried out the following tasks (see Figure S.2):
Figure 2.
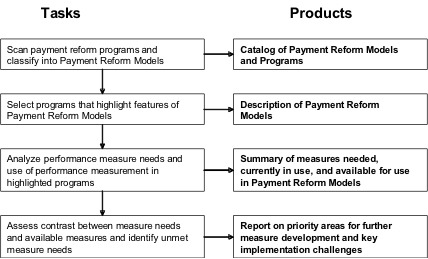
Tasks and Products
scan of payment reform programs to derive payment reform models (PRMs)
selection of payment reform programs to highlight features of PRMs
analysis of the rationale for use of performance measures in the model and the suitability of available performance measures
assessment of the gap between measures needed and available measures to identify unmet measure needs.
For each PRM, we describe
the rationale guiding selection of performance measures, payment incentive-specific uses of measurement in the PRM, and the special need for measures created by the model
an analysis of available measures, including the contrast between available measures, the unmet measure needs of the PRM, and the implementation challenges associated with measure implementation.
Across the PRMs, we summarize the key opportunities for measure development and the common implementation challenges associated with implementing performance measurement.
Results
We grouped the reviewed payment reform programs into 11 PRMs that create demand for performance measures.
These 11 models vary widely in the extent to which they alter current payment methods, the scope of patients and services affected, and the providers subject to the new payment arrangements. Therefore, the model incentives and purposes of performance measurement also vary substantially between models. Even within a particular model, different implementations may vary widely on these dimensions. However, there are some general patterns of relationships between the models that can be helpful in comparing their performance measurement needs.
Description of Payment Reform Models and Uses of Performance Measures
Model 1: Global Payment
A single per-member per-month payment is made for all services delivered to a patient, with payment adjustments based on measured performance and patient risk.
Determining based on measured performance whether bonus payments will be made and the amount of those payments (using a pay-for-performance [P4P] mechanism)
Assessing negative consequences, such as avoidance of patients with complex conditions, greater severity of disease, or other risk factors
Informing strategic decisions by payers about the design and implementation of the payment program (e.g., assessing the impact of the payment model on cost and quality)
Assisting providers to identify opportunities for quality improvement and greater efficiency of care delivery
Model 2: ACO Shared Savings Program
Groups of providers (known as accountable care organizations [ACOs]) that voluntarily assume responsibility for the care of a population of patients share payer savings if they meet quality and cost performance benchmarks.
Similar to global payment model:
Determining based on measured performance whether bonus payments will be made and the amount of those payments (using a P4P mechanism)
Assessing negative consequences, such as avoidance of patients with complex conditions, greater severity of disease, or other risk factors
Informing strategic decisions by payers about the design and implementation of the payment program (e.g., assessing the impact of the payment model on cost and quality)
Assisting providers to identify opportunities for quality improvement and greater efficiency of care delivery
Model 3: Medical Home
A physician practice or other provider is eligible to receive additional payments if medical home criteria are met. Payment may include calculations based on quality and cost performance using a P4P-like mechanism.
Evaluating whether practices meet medical home qualification criteria, which may include multiple tiers of achievement
Evaluating practice impact on quality and resource use
Supporting practice-based quality improvement activities
Model 4: Bundled Payment
A single “bundled” payment, which may include multiple providers in multiple care settings, is made for services delivered during an episode of care related to a medical condition or procedure.
Making adjustments to providers' episode-based payment rates based on quality of care
Determining whether providers meet performance criteria for participation in a bundled payment program
Assessing negative consequences, including avoidance of certain types of patients or cases, particularly through patient experience measures
Assisting providers to identify opportunities for quality improvement and greater efficiency of care delivery
Model 5: Hospital-Physician Gainsharing
Hospitals are permitted to provide payments to physicians that represent a share of savings resulting from collaborative efforts between the hospital and physicians to improve quality and efficiency.
Determining if hospitals and affiliated physicians are eligible to participate in a gainsharing program
Ensuring that the quality of patient care is not compromised
Ensuring that the payment incentives lead to improved hospital operational and financial performance (e.g., efficiency)
Detecting increases in the volume of referrals for services not covered within the gainsharing arrangement
Assessing adverse consequences, such as hospital or physician avoidance of patients with adverse risk characteristics
Making information available to providers about opportunities for improvement
Model 6: Payment for Coordination
Payments are made to providers furnishing care coordination services that integrate care between providers
Determining whether providers receive performance-related bonuses (in some programs)
Evaluating the effectiveness of programs that seek to improve coordination-related performance. The approaches taken by programs within this PRM have tended to offer flexible financing to multidisciplinary teams of providers and then measure cost and health outcome measures to assess how cost and quality change over time.
Assessing negative consequences, including avoidance of certain types of patients or cases, particularly through patient experience measures
Assisting providers to identify opportunities for quality improvement and greater efficiency of care delivery
Model 7: Hospital P4P
Hospitals receive differential payments for meeting or missing performance benchmarks.
Determining the amount of bonus payments or adjustments to the diagnosis-related groups (DRG) payment schedule
Measuring unintended adverse consequences of the PRM and monitoring performance trends in areas not targeted by P4P
Assisting hospitals to identify opportunities for quality improvement and greater efficiency of care delivery
Model 8: Payment Adjustment for Readmissions
Payments to hospitals are adjusted based on the rate of potentially avoidable readmissions.
Determining which readmissions are considered preventable
Determining which hospitals will be subjected to a payment penalty
Assisting hospitals to identify opportunities to improve the discharge transition
Measuring unintended adverse consequences of the PRM, such as assignment of admitting diagnoses to avoid the penalty
Model 9: Payment adjustment for Hospital-Acquired Conditions
Hospitals with high rates of hospital-acquired conditions are subject to a payment penalty, or treatment of hospital-acquired conditions or serious reportable events is not reimbursed.
Determining whether a payment is adjusted
Assisting hospitals to identify opportunities to improve safety
Measuring unintended adverse consequences of the PRM and monitoring performance trends in areas not targeted by the payment adjustment
Model 10: Physician P4P
Physicians receive differential payments for meeting or missing performance benchmarks.
Determining adjustments to bonus payments or to fee schedules
Measuring unintended adverse consequences of payment models and monitoring trends in performance for areas not targeted by P4P
Identifying opportunities for quality improvement
Model 11: Payment for Shared Decisionmaking
Payment is made for the provision of shared decisionmaking services.
Evaluating the use of shared decisionmaking tools in improving patient decisionmaking and better aligning treatment choices with patient preferences
Certification of patient decision aids
Assessing the potential for unintended adverse consequences of tying payments to the shared decisionmaking process
Table 1 describes the 11 models with regard to four attributes relevant to performance measurement and performance-based incentives: (1) whether performance is measured for a predefined population, (2) whether performance is measured for a predefined episode of care, (3) whether performance is measured across more than one type of care delivery organization, and (4) whether the PRM incentive is a fee-for-service payment applied to one or more newly specified services.
Table 1.
Attributes of Payment Reform Models
| Model | Attributes | |||
|---|---|---|---|---|
| Performance Measured for a Population | Performance Measured for an Episode of Care | Performance Measured Across More Than One Type of Delivery Organization | Fee-for-Service Payment Applied to One or More Newly Specified Services | |
| Model 1: Global payment | ✓✓ | ✓ | ✓✓ | |
| Model 2: ACO shared savings program | ✓✓ | ✓ | ✓✓ | |
| Model 3: Medical home | ✓✓ | ✓ | ✓ | ✓ |
| Model 4: Bundled payment | ✓ | ✓✓ | ✓✓ | ✓ |
| Model 5: Hospital-physician gainsharing | ✓ | ✓ | ✓ | |
| Model 6: Payment for coordination | ✓ | ✓ | ✓ | ✓✓ |
| Model 7: Hospital P4P | ✓ | |||
| Model 8: Payment adjustment for readmissions | ✓ | ✓ | ||
| Model 9: Payment adjustment for hospital-acquired conditions | ✓ | |||
| Model 10: Physician P4P | ✓ | |||
| Model 11: Payment for shared decisionmaking | ✓ | ✓✓ | ||
NOTES: ✓✓ = key attribute of the PRM, ✓ = may be an attribute of the PRM, none = unlikely to be an attribute of the PRM.
The PRMs toward the top of the table tend to represent payment made to a group of providers and/or provider organizations to provide high-quality and efficient care to a defined population over time. The performance goals generally include a broader and more comprehensive set of services than the goals defined for the models toward the bottom of the table. The PRMs at the top of the table may incorporate and combine elements of PRMs from rows at the bottom of the table. At the bottom of the table, payment is generally used to achieve relatively narrowly defined performance goals, and the payment is more frequently made to individual providers, rather than groups. PRMs in the middle of the table are blended with respect to each of the three dimensions. These models generally focus payment on specific sets (e.g., bundles) of services that are delivered during an episode of care.
Next, we briefly describe the near-term performance measurement needs defined by each PRM. The lists of near-term performance measurement needs are not intended to be comprehensive or exclusive. For each PRM, it is possible to imagine a program that includes all possible measures. Because the devotion of resources to measure development and implementation is likely to be limited, such a perspective would be uninformative. Instead, we have selected those measure needs that are likely to be of greatest interest within the context of each specific PRM.
The Special Performance Measure Needs Created by Payment Reform Models
Model 1: Global Payment
Reflect the broad range of care services delivered and the multiple care delivery settings that participate in providing care to a population under the global payment (i.e., measures for physician groups, hospitals, emergency departments, post-acute care, and any other setting that may provide care under the global payment)
Include key indicators (such as health outcomes attributable to the care provided under the global payment), composite measures, or measure sets
Enable longitudinal, population-based measurement of the care services provided to the population covered by the global payment
-
Can be used within or across global payment programs that vary with respect to
the length of the time period addressed by longitudinal measurement and whether this time period is fixed or variable
the provider holding the global payment (e.g., integrated delivery system, hospital, or ambulatory provider group)
the range of providers that participate in the global payment
the range of services providers deliver under the global payment.
Model 2: ACO Shared Savings Program
Reflect the broad range of care services delivered and the multiple care delivery settings that participate in the ACO (i.e., measures for physician groups, hospitals, emergency departments, post-acute care, and any other setting that may be included in the ACO)
Include key indicators (such as health outcomes attributable to the care provided under the global payment), composite measures, or measure sets
Enable longitudinal, population-based measurement of the care services provided to the population enrolled in the ACO
-
Can be used within or across ACOs that vary with respect to
the length of the time period addressed by longitudinal measurement and whether this time period is fixed or variable
the features of the ACO management responsible for allocating the shared savings (e.g., integrated delivery system, hospital, or ambulatory provider group)
the range of providers that participate in the ACO
the range of services that providers deliver within the ACO.
Model 3: Medical Home
Reflect the adoption of care processes and structural capabilities (management features and health information technology) that enhance continuity and coordination of care
Assess whether care is patient-centered, including the outcomes of primary care, the patient experience, and patient and caregiver engagement with primary care
Model 4: Bundled Payment
Are related to the conditions targeted by the bundles
Are tailored to the care delivery settings that participate in delivering components of the care bundle (i.e., measures for hospitals as well as for individual physicians) or that can be used effectively across multiple care delivery settings in an episode-of-care framework
Can be used to detect negative consequences of the payment model (e.g., bundle-specific measures of appropriateness of care and the patient experience of care)
Assess coordination of care within and across episodes (or bundles)
Model 5: Hospital-Physician Gainsharing
Apply to both the hospital and individual physicians covered by the gainsharing arrangement
Evaluate the specific treatments or procedures covered by the gainsharing arrangement
Are treatment-specific or procedure-specific, particularly to evaluate adverse consequences, such as avoidance of high-risk patients
Include patient health and safety outcomes. Measures of process should be chosen carefully to avoid the potential to “lock in” care processes that have acceptable or superior substitutes.
Assess care coordination, access, cost, and utilization
Model 6: Payment for Coordination
Assess whether care coordination activities are accomplished
Assess costs, service utilization, patient experience, and health outcomes of patients who receive care coordination services
Model 7: Hospital P4P
Measure sets may be narrowly or broadly defined, depending on the number of performance goals included in the performance incentive.
A narrowly constructed set may focus on a specific domain of measurement, such as health care-associated infections (HAI). Other P4P measure sets may focus on patient outcomes, patient experience, costs of care, or access to care. For example, measurement may focus on the evidence-based safety processes associated with avoidance of preventable complications, such as HAI.
A broadly constructed measure set will blend payment incentives on measures from multiple domains.
P4P programs may also be included as components of other PRMs, such as the global payment or ACO shared savings PRMs. Hospital P4P may also be layered on top of a bundled payment program with hospital episodes defining bundles of care and performance measures defining the P4P adjustment to a bundled payment.
Structural capabilities of a hospital or credentials of hospital-based clinicians may determine eligibility for participation in a P4P program or eligibility for a differential payment.
Model 8: Payment Adjustment for Readmissions
Emphasize aspects of care under the hospital's control and account for the clinical and sociodemographic risk characteristics of the hospital's patient population
Can be used to assess adverse outcomes (such as patient experience measures)
Can be used to understand the processes that influence the risk of readmission and can help to redesign the discharge transition to reduce readmission rates
Model 9: Payment Adjustment for Hospital-Acquired Conditions
Enable identification and documentation of the occurrence of hospital-acquired conditions (e.g., treatment complications and other safety outcomes). Performance measurement within this model is used to document the occurrences of preventable hospital-acquired conditions. While the NQF publishes a list of serious reportable events that are considered preventable, these are rare events.
Provide an assessment of the preventability of these conditions. Hospital-acquired conditions used in measurement should be associated with evidence that they are preventable (Pronovost, Goeschel, and Wachter, 2008).
Enable meaningful aggregation of conditions to form composite measures. In addition, measures of safety processes that can prevent such events may enable stakeholders to implement the PRM so that it is more likely to reduce the incidence of hospital-acquired conditions over time.
Model 10: Physician P4P
Assess delivery of evidence-based chronic disease management, including care processes, patient outcomes, patient experience, and access to care
Include composites of measures across conditions to assure that clinicians do not focus on some aspects of care delivery to the detriment of others
Assess structural capabilities of physician practices to determine eligibility to participate in a P4P program or eligibility for a differential payment
Can be used to evaluate the quality of episodes of care (in combination with the bundled payment model)
Assess the appropriateness of care and efficiency of care delivery
Model 11: Payment for Shared Decisionmaking
Can be used to assess patient and caregiver experience and patient and caregiver engagement
Include structural aspects of care, such as criteria for the certification of patient decision aids
Assess the process used to enable shared decisionmaking
The Potential Impact of Payment Reform Models on Performance Measure Development
Any portfolio of performance measures generally reflects those quality problems that are concerning to health care stakeholders. Frequently, the concerns arise in relation to the payment mechanisms used to purchase health care services. During the past decade, performance measure developers have tended to specify measures for either a fee-for-service payment environment or a capitated health plan environment. Early efforts to develop measures for use in capitated health plans tended to focus on assessing underuse of preventive services and chronic care. Fewer measures focused on inappropriate service delivery, and very few prior measurement efforts have addressed the efficiency of care delivery. Our analysis suggests that new initiatives to base payment on performance measurement may create a new set of demands on performance measure developers.
There are several implications of the shift to a focus on measurement to support the emerging PRMs.
Measure Development Should Be Guided by a Longitudinal Care Framework Rather Than a Discrete Service Focus
Many past performance measures have tended to focus on the delivery of discrete clinical services, such as preventive services, medications, or other treatments delivered at a specific point in time. Exceptions include the chronic disease measurement sets that address care processes delivered during a specified time frame (e.g., one year). Some of the PRMs we studied are built on a longitudinal care framework for services delivered to a population (global payment, ACO shared savings, medical home, bundled payment, and hospital-physician gainsharing). Episode-based measurement is not a new construct. Risk-adjusted mortality after hospitalization or surgery is an outcome measure that is used to assess an episode of hospitalization or surgery. However, developing and refining a variety of quality measures to address episodes of care will be an important step. Using a longitudinal measurement framework to develop measures will naturally emphasize health outcomes. In particular, the measurement of changes in functional status, morbidity, and quality of life will be attractive to clinicians to the extent that these results can guide clinical care. The selection of process measure sets should also be informed by the longitudinal framework.
Complex Organizational Types May Benefit from Complex Measurement Strategies That Support Internal Incentive and Quality Improvement Models
Some of the PRMs encompass a broad range of clinical activities and organizational types that must coordinate with one another (e.g., global payment and ACO shared savings) in contrast to others that target relatively narrowly specified goals for a specific organizational type (e.g., reducing hospital-acquired conditions or promoting the use of shared decisionmaking tools). Although it is also possible to set performance incentives on a few key indicators (e.g., population outcomes), the complex organizational types (meaning those organizations that encompass multiple specialized services that have not traditionally been merged together outside of integrated delivery systems) may have expansive measure needs in order to set incentives to providers internally (including outcome, process, and other measure types). While each organization could develop its own measures for internal use, nonstandardized measurement approaches may defeat the use of results for other purposes (such as public reporting). Standardized but flexible measure sets including both outcome and process that can serve P4P and other PRMs (independent of the ACO or medical home context) will also be useful to complex organizations.
Priorities for measure development may be unclear until these delivery models and their patient populations are more specifically defined. For example, it will be difficult to specify measures for an ACO without knowing the range of providers and delivery organizations that will participate. The creation of composite measures may be especially challenging until the ACO organization is better defined.
Composite Measures Will Be Important in an Episode-Based Payment Framework
Composite measures that combine clinical process measures or process and outcome measures longitudinally will be desirable in an episode-based measurement framework. A recent paper summarizes some of the considerations in choosing composite measure sets for specific purposes (Peterson et al., 2010).
Efficiency of Care Measures May Be Useful
Containing costs is a goal of most of the PRMs either directly (through the fixed base payment of models, such as the global payment PRM) or indirectly (through bonuses that improve quality and reduce the need for future care, such as the physician P4P PRM). While assessment of costs may be necessary to set or negotiate payment amounts, measurement of costs is not necessary once a cost-containing incentive is established. In the context of the cost-containing incentive, performance measurement is used primarily to counteract the potential quality deficits that could arise from actions taken to reduce costs (e.g., reducing services). Given the challenges of developing measures of efficiency, some observers have favored measuring cost or resource use (especially relative resource use). Cost and resource use can be difficult to interpret in the absence of accompanying measures of quality (to form efficiency measures) or case-mix or risk adjustment. Setting payment adjustments based on reductions in resource use or cost may undermine quality.
Identifying and rewarding efficient care is desirable. Efficiency measures could be useful (Hussey et al., 2009). However, few efficiency measures have been developed to date, and such measures are very challenging to develop. Measuring appropriateness or overuse of services can be useful in some of the PRMs (e.g., hospital and physician P4P). For example, P4P bonuses could be set based on efficiency measure results. The bundled payment PRM requires payers to establish payment amounts that account for the cost of a bundle of services delivered efficiently. Thus, the bundle includes an implicit efficiency consideration by defining an optimal set of services (and their associated cost) to set a payment rate. Gainsharing programs set implicit targets related to cost but do not define efficiency explicitly.
Blended Payment Models Will Rely on Blended Measurement Strategies
Where payment models are blended, the measurement strategies may be adapted across models. Addition of P4P to a global payment strategy has been accomplished under the Alternative Quality Contract of Blue Cross Blue Shield of Massachusetts. Likewise, the use of bundled payment may be readily combined with other payment models. The measures developed for use in these other payment models can be readily integrated into the more complex payment models.
Structure-of-Care Measures Will Be Required for Some Models, at Least in the Near Term
Some of these measures will take the traditional form of structure used in accreditation programs. These typically assess the presence or absence of a feature without further assessing its functionality. For example, computerized order entry systems can be present but not used. The recent approach in legislation that defines “meaningful use” of health information technology (HIT; translated by the Department of Health and Human Services into operational criteria for functionality) represents an example of this more sophisticated approach to assessing the structure of care (Donabedian, 1980). The medical home, payment for care coordination, and payment for shared decisionmaking models require the specification of criteria to enable certification that a provider or organization has basic capabilities. Medical home criteria define capabilities related to care management, access, and HIT. Shared decisionmaking payments will depend on the use of certified decision aids and, possibly, processes, and payments for care coordination will require criteria for certifying the coordinating provider or organization.
Conclusions
The signing of PPACA into law in 2010 is likely to accelerate payment reform based on performance measurement. This technical report is intended to inform multiple stakeholders about the principal PRMs and the status of performance measures in these models and programs. The report summarizes the characteristics of PRMs and the performance measure needs they will generate. Finally, the report identifies the near-term measure development opportunities that may best accelerate the successful implementation of performance measurement in these models.
The report is also intended to create a shared framework for analysis of future performance measurement opportunities. Much measure development, implementation, and evaluation remains to be accomplished. Even for models with a track record of implemented programs and evaluation (such as the hospital and physician P4P models), measure sets have not reached their full potential. These programs were important first steps showing that payment based on performance is feasible even with the relatively limited measure sets available today. Barriers to a fully operational performance measurement system in health care can be overcome with careful planning and integration of care delivery systems, investments in measure development and testing, and investments in the development of valid and reliable data sources that have adequate clinical data to support new measures.
Ongoing and planned demonstration projects and their evaluations will offer valuable lessons about the measures needed to implement these and future PRMs. Investing in infrastructure that improves the available data for performance measurement will be a necessary precursor to successful deployment of new types of measures. Carefully bridging payment reform and performance measurement while attending to the potential adverse unintended consequences should optimize the health of Americans and assure that care is affordable in the future.
Reference
- Rosenthal MB, “Beyond Pay for Performance—Emerging Models of Provider-Payment Reform,” New England Journal of Medicine, Vol. 359, No. 12, September 18, 2008, pp. 1197–1200. [DOI] [PubMed] [Google Scholar]
- Miller HD, “From Volume to Value: Better Ways to Pay for Health Care,” Health Affairs (Millwood), Vol. 28, No. 5, September-October 2009, pp. 1418–1428. [DOI] [PubMed] [Google Scholar]
- Mechanic RE and Altman SH, “Payment Reform Options: Episode Payment Is a Good Place to Start,” Health Affairs, Vol. 28, No. 2, January 27, 2009, pp. w262–w271. [DOI] [PubMed] [Google Scholar]
- Fisher ES, MCClellan MB, Bertko J, Lieberman SM, Lee JJ, Lewis JL, and Skinner JS, “Fostering Accountable Health Care: Moving Forward in Medicare,” Health Affairs, Vol. 28, No. 2, January 27, 2009, pp. w219–w231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee PV, Berenson RA, and Tooker J, “Payment Reform—The Need to Harmonize Approaches in Medicare and the Private Sector,” New England Journal of Medicine, Vol. 362, No. 1, January 7, 2010, pp. 3–5. [DOI] [PubMed] [Google Scholar]
- Thorpe KE and Ogden LL, “Analysis and Commentary: The Foundation That Health Reform Lays for Improved Payment, Care Coordination, and Prevention,” Health Affairs (Millwood), Vol. 29, No. 6, June 2010, pp. 1183–1187. [DOI] [PubMed] [Google Scholar]
- Pronovost PJ, Goeschel CA, and Wachter RM, “The Wisdom and Justice of Not Paying for ‘Preventable Complications,’” Journal of the American Medical Association, Vol. 299, No. 18, May 14, 2008, pp. 2197–2199. [DOI] [PubMed] [Google Scholar]
- Peterson ED, DeLong ER, Masoudi FA, O'Brien SM, Peterson PN, Rumsfeld JS, Shahian DM, and Shaw RE, “ACCF/AHA 2010 Position Statement on Composite Measures for Healthcare Performance Assessment: A Report of American College of Cardiology Foundation/American Heart Association Task Force on Performance Measures (Writing Committee to Develop a Position Statement on Composite Measures),” Journal of the American College of Cardiology, Vol. 55, No. 16, April 20, 2010, pp. 1755–1766. [DOI] [PubMed] [Google Scholar]
- Hussey P, de Vries H, Romley J, Wang MC, Chen SS, Shekelle PG, and McGlynn EA, “A Systematic Review of Health Care Efficiency Measures,” Health Services Research, Vol. 44, No. 3, June 2009, pp. 784–805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donabedian A, The Definition of Quality and Approaches to Its Assessment, Ann Arbor: Health Administration Press, 1980.


