Abstract
Study Objective:
This study aimed to evaluate the effects of zolpidem CR (controlled release) on sleep and nocturnal ventilation in patients with congestive heart failure, a population at risk for insomnia and poor sleep quality.
Methods:
Fifteen patients with heart failure (ischemic cardiomyopathy) and ejection fraction ≤ 45% in NYHA functional class I or II were evaluated with full polysomnography in a placebo-controlled, double-blind, randomized trial. Patients underwent three tests: (1) baseline polysomnography and, after randomization, (2) a new test with zolpidem CR 12.5 mg or placebo, and after 1 week, (3) a new polysomnography, crossing the “medication” used.
Results:
A 16% increase in total sleep time was found with the use of zolpidem CR and an increase in stage 3 NREM sleep (slow wave sleep). The apnea hypopnea index (AHI) did not change with zolpidem CR even after controlling for supine position; however, a slight but significant decrease was observed in lowest oxygen saturation compared with baseline and placebo conditions (83.60 ± 5.51; 84.43 ± 3.80; 80.71 ± 5.18, P = 0.002).
Conclusion:
Zolpidem CR improved sleep structure in patients with heart failure, did not change apnea hypopnea index, but slightly decreased lowest oxygen saturation.
Citation:
Gatti RC, Burke PR, Otuyama LJ, Almeida DR, Tufik S, Poyares D. Effects of zolpidem CR on sleep and nocturnal ventilation in patients with heart failure. SLEEP 2016;39(8):1501–1505.
Keywords: heart failure, polysomnography, zolpidem CR, sleep
Significance.
Sleep disorders are common in patients with heart failure (HF). Caution is recommended when prescribing sedative-hypnotic drugs in this population, they may cause depression of ventilation. Given the high prevalence of HF and insomnia; the deleterious nature of this association; the need of treatment alternatives to improve sleep; and the low potential of zolpidem to cause respiratory depression, we report data from our randomized, placebo-controlled, crossover trial, showing that a single dose of zolpidem CR was safe, improved sleep, did not change RDI, but caused a slight but significant decrease in lowest SpO2 in a homogeneous sample of HF patients. Despite zolpidem CR having an acute safe profile, its long-term effect in HF patients who complain of insomnia deserves further study.
INTRODUCTION
Cardiovascular diseases are the most prevalent chronic diseases in the world1 and result in heart failure (HF) symptoms,2 associated comorbidities, and poor quality of life.
Sleep disorders are common in HF patients, with approximately 75% of patients reporting poor sleep. Among these disorders, insomnia and sleep apnea4 are the most common.4 Insomnia occurs in 25% to 56% of patients with HF,5 and sleep apnea occurs in 47% to 83% of cases, as they have common pathophysiological processes, such as increased sympathetic activation and increased sodium and water retention.6 In addition, insomnia is associated with an increased risk for cardiovascular disease possibly mediated by hypertension or elevated resting heart rate,7 which could negatively affect HF patients' clinical outcomes.
In many of these patients, HF itself, associated with sleep disturbances, leads to nocturnal sleep disruption and consequent poor sleep quality, exacerbating heart condition symptoms.8 Eventually, this clinical picture, associated with complaints of insomnia and/or excessive daytime sleepiness, makes these patients seek medical help to try to circumvent the problem.9
Among the most commonly prescribed hypnotics are benzodiazepines; however, these drugs may present potential depressant effects on the ventilatory responses of elderly patients or in those for whom this response is already compromised; these types of medication may also result in addiction.10 In contrast to benzodiazepines, zolpidem is a non-benzodiazepine GABA-A receptor agonist that has been widely prescribed to treat insomnia.11 A recent review reported the results of 2 studies in severe obstructive sleep apnea patients using 10 to 20 mg of zolpidem. Compared with placebo, zolpidem did not worsen AHI; however, 20 mg reduced lowest oxygen saturation without changing the oxygen desaturation index.12 Since sleep-disordered breathing, either obstructive and central, and insomnia are prevalent among HF patients,3–6,8 and no studies have evaluated the effect of non-benzodiazepine GABA-A receptor agonists on breathing during sleep in patients with HF of ischemic etiology, we sought to evaluate the effects of zolpidem on sleep and nocturnal ventilation in this group. Our hypothesis is that zolpidem CR improves polysomnographic nocturnal sleep parameters in patients with New York Heart Association (NYHA) Class I or II HF.
METHODS
Population
A total of 15 consecutive patients aged over 30 were evaluated. They were recruited from the outpatient clinic of the Sao Paulo Cardiomyopathy Division, Sao Paulo Hospital, Universidade Federal de Sao Paulo, after clinical and laboratory evaluations and diagnosis of ischemic cardiomyopathy and ejection fraction ≤ 45% in NYHA functional class I or II. Patients who had regularly used benzodiazepines or other medication to induce sleep in the previous month were excluded. In addition, we excluded patients with laboratory test changes suggestive of liver and/or kidney failure. Therefore, plasma creatinine values ≥ 1.3 mg/dL led to exclusion from the protocol. Fifteen patients were included in the final sample. All patients were taking medication, including β-blockers, for treatment of their heart condition in accordance with the standard outpatient treatment protocol.
Sociodemographic data, such as body mass index (BMI), age, gender, and neck circumference, and echocardiographic data, such as the diameter of the heart cavities, cardiac mass index, and ejection fraction, were also evaluated.
Study Design
This study was a double-blind, randomized, placebo-controlled, crossover trial. Patients underwent baseline polysomnography and were randomized into two groups. A further polysomno-gram was then performed after taking 12.5 mg zolpidem CR or placebo. After a further week, another polysomnogram was performed, switching the “medication” used on the second examination day. There was a washout period of one week between polysomnograms. Bedtime was stipulated preferably by the patient according to their routine and was evaluated using a sleep diary.
Polysomnography
Full polysomnography was performed at the Sleep Institute laboratory (AFIP, Sao Paulo, Brazil), Sleep Medicine Division, Psychobiology Department, (Universidade Federal de Sao Paulo, Brazil), at three points: the first evaluation was performed on the first test day (baseline), and the other two evaluations were performed with intervals of one week between them (treatment with zolpidem CR or placebo).
The overnight polysomnography was performed using an EMBLA digital system (17 channels, Medicare Medical Devices). The following variables were monitored: electroencephalogram (4 channels), electrooculogram (2 channels), electromyogram (2 channels: submental and anterior tibialis muscles), electrocardiogram (one channel D2 modified), snoring, and body position. The airflow was monitored using a thermocouple and a nasal pressure transducer (Pro-Tech Services Inc., Mukilteo, Washington). Chest and abdominal piezo-sensors monitored the respiratory effort of each patient. Arterial oxygen saturation (SpO2) and pulse were recorded using a pulse oximeter (Nonin, model 9500, Plymouth, USA). All of the polysomnograms were performed and scored by an experienced sleep technician who followed the American Academy of Sleep Medicine (AASM) guidelines for sleep studies13 and were reviewed by a sleep medicine physician.
Sleep Quality Questionnaires
On the first day of baseline polysomnography, patients completed the following questionnaires: the Epworth Sleepiness Scale (ESS)14; the Pittsburgh Sleep Quality Index (PSQI)15; the New York Heart Association Functional Classification (NYHAFC)16; dyspnea scales17; and the Modified Medical Research Council (MMRC) scale.18
Statistical Analysis
The software Statistica v12 (Statsoft, Tulsa, OK, USA) was used for data analysis. All demographic, anthropometric, echocardiographic, and polysomnographic data are presented as means ± standard deviations or frequencies. To compare the means of the polysomnographic data, analysis of variance (ANOVA) for repeated measures was used followed by the Bonferroni a posteriori test when needed. The significance level adopted was P ≤ 0.05.
RESULTS
Demographic, Anthropometric, and Echocardiographic Evaluations
No adverse event was reported with zolpidem CR or placebo in this trial, with the exception of a mild morning headache episode in one patient.
The descriptive characteristics of the sample are presented in Table 1. Table 1 shows that the population studied presented borderline sleepiness score on the Epworth Sleepiness Scale (ESS), which was 9.73 ± 5.15 points (excessive sleepiness is considered when > 10). However, the population exhibited a score of 9.13 ± 5.20 on the Pittsburgh Sleep Quality Index (PSQI), suggesting poor sleep quality. Scores on the Medical Research Council scale, which measures dyspnea during exercise, of 1.47 ± 1.30, and on the modified Borg scale of 1.93 ± 2.31, indicate mild to moderate weariness, reinforcing the condition presented by our sample of 1.73 ± 0.97 on the NYHA functional class scale (data presented in Table 1).
Table 1.
Demographic and anthropometric data (n = 15).
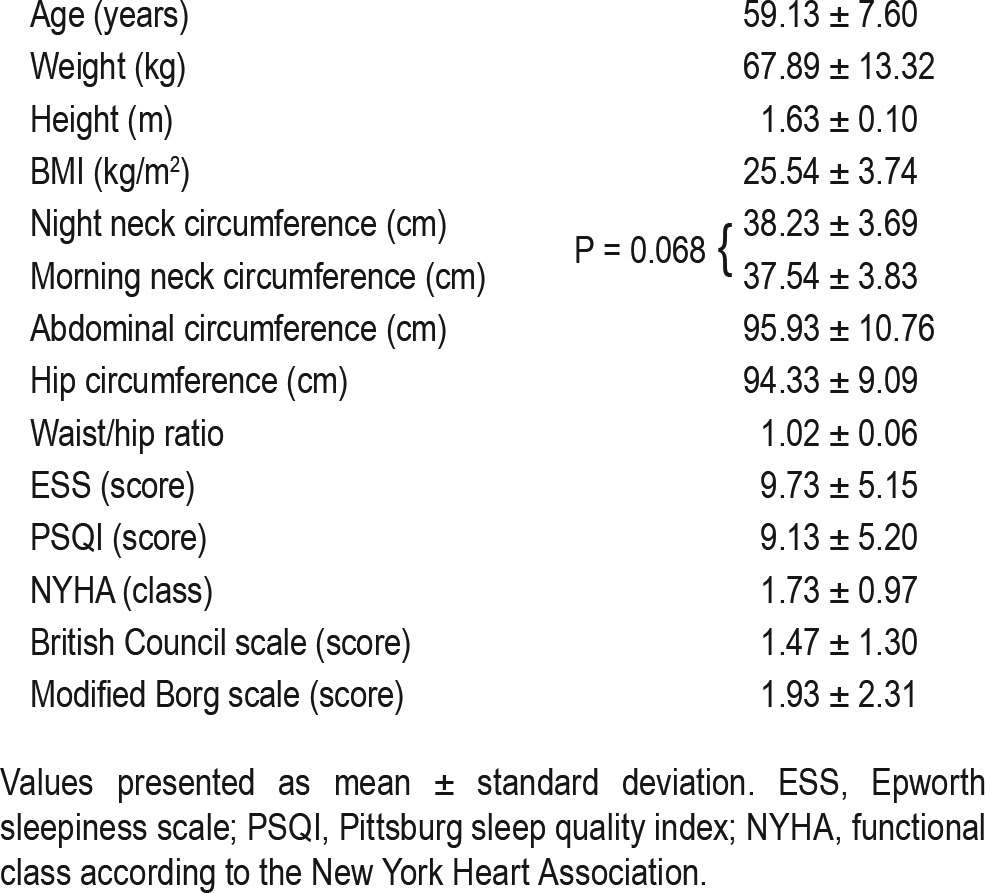
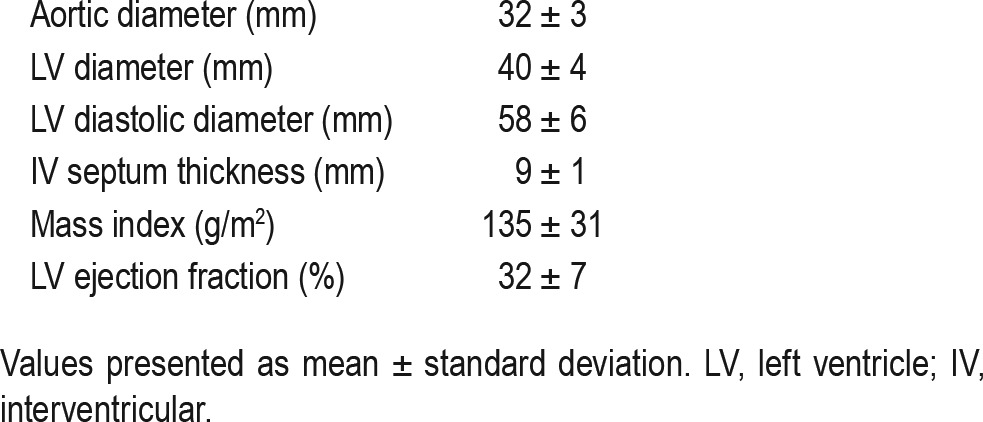
Table 2 shows the echocardiographic parameters of the HF patients. As expected, they had low ejection fraction, left ventricular dilation, and reduced cardiac mass index, characterizing cardiac involvement.
Table 2.
Echocardiographic data (n = 15).
Polysomnography
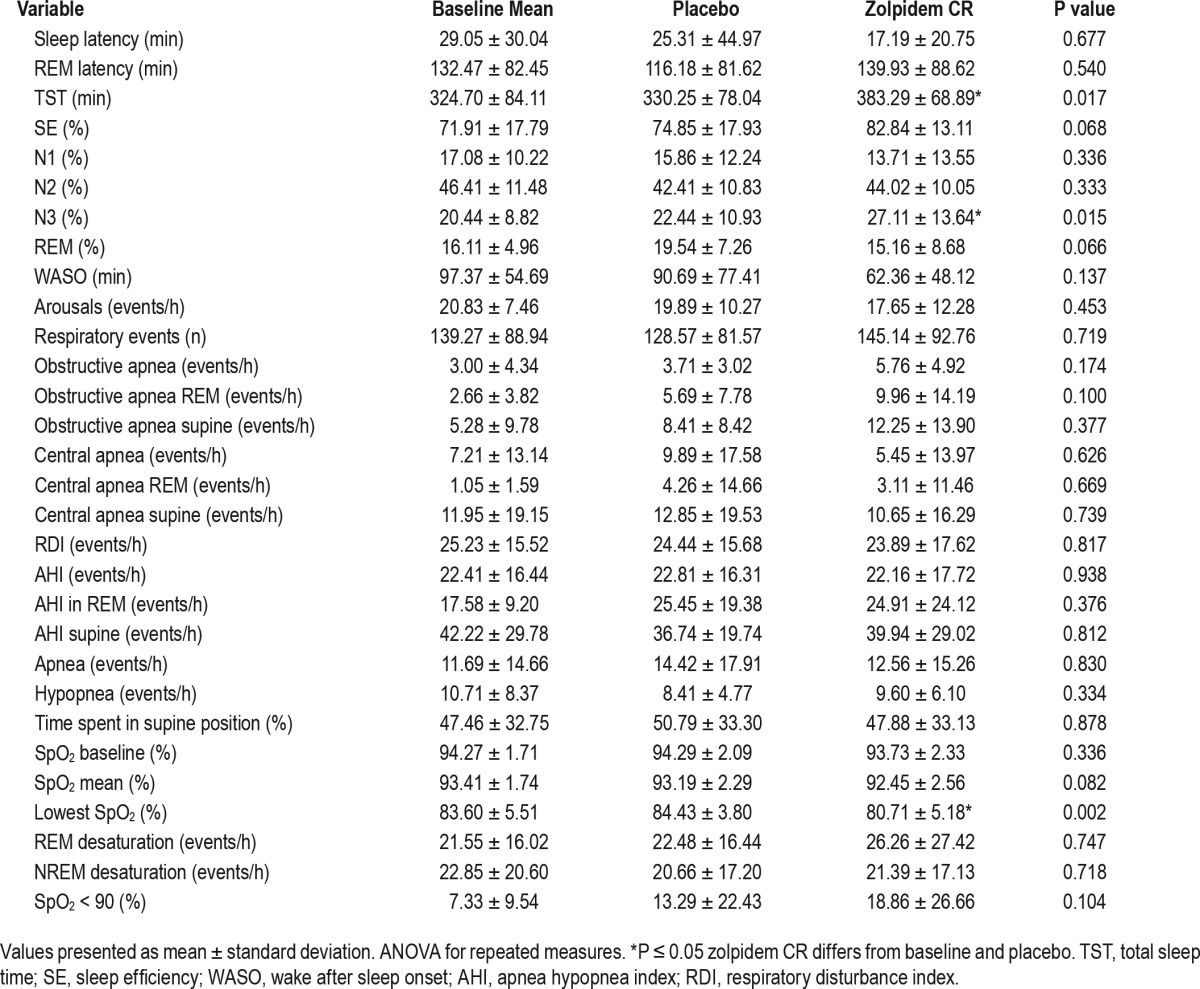
The patients' polysomnographic data obtained after the three tests are shown in Table 3. Significant differences can be observed in the N3 stage and TST, which increased with the use of zolpidem CR (P = 0.01 for both). The other sleep architecture parameters did not differ between treatments. In relation to respiratory sleep parameters, no significant change was detected in the apnea-hypopnea index (AHI), the respiratory disturbance index (RDI), or the central or obstructive respiratory event index during REM sleep, NREM sleep, or sleep in the supine position between treatments. Minimum O2 saturation was lower in the zolpidem CR group (P = 0.002); however, the percentage of time with oxygen saturation less than 90% and the mean saturation did not differ significantly between treatments.
Table 3.
Comparison of polysomnographic data: baseline, placebo and zolpidem CR conditions (n = 15).
DISCUSSION
This is the first study, to the best of our knowledge, assessing the acute effect of a non-benzodiazepine GABA-A receptor agonist, in this case zolpidem CR, in HF patients with reduced ejection fraction. Overall results suggest that zolpidem increased total sleep time and N3 NREM sleep compared with placebo and baseline. We did not find significant changes in AHI and RDI, even after controlling for supine position. However, a slight but significant decrease in lowest SpO2 was found with zolpidem compared with placebo and baseline conditions.
There have been a number of reports in the literature on HF patients suggesting that they have poor sleep quality as assessed by PSQI,19,20 and fragmented sleep for various reasons, such as sleep apnea and insomnia.4,5 Similarly, we found poor sleep quality using similar questionnaire, a mean baseline AHI of 22.41 ± 16.44, and fragmented sleep as evidenced by increased WASO and arousal index in our population.
There is no consensus on the best sleep-inducing medication for patients with HF. As zolpidem is one of the most commonly prescribed hypnotics,21 and reported to be safe with few dose-dependent adverse events,22 in this study we decided to evaluate its effects in a homogeneous sample of patients with HF of ischemic origin, which, with hypertension, is the most common etiology of HF.23 Patients did not report significant adverse events after a single dose of zolpidem CR, with the exception of a mild morning headache episode in one patient.
Unlike benzodiazepines, in healthy controls, zolpidem has little effect on sleep stages.24 Zolpidem is as effective as benzodiazepines in decreasing sleep latency and prolonging TST in patients with insomnia.25,26 In fact, our study showed that in patients with ischemic HF, zolpidem CR prolongs TST by an average of 16% compared to placebo. We also observed a trend toward an increase in sleep efficiency compared with placebo (P = 0.06). As for sleep stages, there was a significant increase in N3 in the zolpidem CR group. The combination of increased TST and increased N3 stage (slow wave sleep) indicates an improvement in the sleep pattern, which in theory could be beneficial for patients with HF, since N3 is a sleep stage where cardiac demand is at its lowest for the day, as a lower heart rate, blood pressure, and respiratory rate are observed.27 REM sleep, however, did not change significantly with the use of zolpidem CR. Together, these results suggest an improvement in sleep architecture in patients with HF acutely treated with zolpidem CR.
With regard to potential breathing effects, zolpidem has been reported as having fewer muscle-relaxant effects than benzodiazepine hypnotics, which has been mostly studied in animals.28 In our study, zolpidem CR showed a slight but statistically significant reduction in lowest oxygen saturation. A previous study also showed similar results in severe OSA patients without HF; a slight reduction in lowest oxygen saturation with no changes in AHI with a higher than usual therapeutic dose, 20 mg of zolpidem.29 Moreover, studies show that another GABA-A agonist, eszopiclone, may not change30 or may even improve breathing patterns during sleep, especially for individuals whose sleep is highly fragmented, and thus for whom the ventilatory drive becomes unstable.31
However, some guidelines suggest that this drug should not be used in patients with respiratory depression.32 This effect could be attributed to an effect within the central chemoreflex loop at the central chemoreceptors,33 which could actually reduce respiratory events in patients with HF and central sleep apnea. Zolpidem has been reported as devoid of muscle-relaxant effects, thus unlikely to affect oropharyngeal muscles24; and does not cause respiratory depression in insomnia patients.26 Similarly, our study revealed that in patients with ischemic HF, no significant increase in obstructive respiratory events, in overall AHI or RDI, or in OSA and CSA indices per hour were detected compared with placebo and baseline conditions. The only study, to the best of our knowledge, evaluating the long-term effects of zolpidem on sleep parameters in patients with OSA treated with CPAP, reported an improvement in sleep latency and arousal index, without affecting AHI, ODI, and lowest SpO2, compared with placebo.34
Another issue to be considered when computing the number of obstructive or central apneas is the time spent in the supine position, which is known to possibly increase obstructive and even central events.35 In our study, we also evaluated the respiratory disturbance indices during sleep in the supine position and found no differences.
Potential limitations of this study include the relatively small sample size, although other studies evaluating populations with sleep-disordered breathing and the use of sleep aids used similar or smaller samples including sample sizes calculation to detect a significant difference in AHI of 5 per hour.34 In addition, we did not evaluate the duration of respiratory events but did control for supine position and type of events. Lastly, our data refer only to a single dose. Despite zolpidem CR having an acute safe profile, its long-term effect in HF patients who complain of insomnia deserves further study.
CONCLUSIONS
The hypnotic zolpidem CR improves sleep structure because it increases N3, a deep sleep phase, and TST. Zolpidem CR also tends to increase sleep efficiency, which can be beneficial for the cardiovascular system. Furthermore, zolpidem CR did not increase the overall rate of apneas and hypopneas and decreased lowest oxygen saturation without affecting respiratory events of central origin.
DISCLOSURE STATEMENT
This was not an industry supported study. This work was undertaken at Sao Paulo hospital, and received financial support from Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) and Associação Fundo Incentivo a Pesquisa (AFIP). Dr. Poyares consults for Sanofi-Aventis, Libbs Pharmaceuticals, and EMS Pharmaceuticals, developing educational presentations. The other authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
The authors thank the volunteers, Dr. Silvia Ihara and the staff of the Sleep Institute. Study supported by Associação Fundo Incentivo a Pesquisa (AFIP), Sao Paulo, Brazil.
REFERENCES
- 1.Dhingra A, Garg A, Kaur S, et al. Epidemiology of heart failure with preserved ejection fraction. Curr Heart Fail Rep. 2014;11:354–65. doi: 10.1007/s11897-014-0223-7. [DOI] [PubMed] [Google Scholar]
- 2.Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics--2014 update: a report from the American Heart Association. Circulation. 2014;129:e28–292. doi: 10.1161/01.cir.0000441139.02102.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Redeker NS, Stein S. Characteristics of sleep in patients with stable heart failure versus a comparison group. Heart Lung J Crit Care. 2006;35:252–61. doi: 10.1016/j.hrtlng.2005.10.007. [DOI] [PubMed] [Google Scholar]
- 4.Gilat H, Vinker S, Buda I, et al. Obstructive sleep apnea and cardiovascular comorbidities: a large epidemiologic study. Medicine. 2014;93:e45. doi: 10.1097/MD.0000000000000045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Broström A, Strömberg A, Dahlström U, et al. Sleep difficulties, daytime sleepiness, and health-related quality of life in patients with chronic heart failure. J Cardiovasc Nurs. 2004;19:234–42. doi: 10.1097/00005082-200407000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Kasai T, Floras JS, Bradley TD. Sleep apnea and cardiovascular disease: a bidirectional relationship. Circulation. 2012;126:1495–510. doi: 10.1161/CIRCULATIONAHA.111.070813. [DOI] [PubMed] [Google Scholar]
- 7.Spiegelhalder K, Scholtes C, Riemann D. The association between insomnia and cardiovascular diseases. Nat Sci Sleep. 2010;2:71–8. doi: 10.2147/nss.s7471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Redeker NS, Jeon S, Muench U, et al. Insomnia symptoms and daytime function in stable heart failure. Sleep. 2010;33:1210–6. doi: 10.1093/sleep/33.9.1210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Taranto Montemurro L, Floras JS, Picton P, et al. Relationship of heart rate variability to sleepiness in patients with obstructive sleep apnea with and without heart failure. J Clin Sleep Med. 2014;10:271–6. doi: 10.5664/jcsm.3526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Critical issues in the management of insomnia: investigators report on estazolam. Am J Med; Proceedings of a symposium; June 3, 1989; Dallas, Texas. 1990. pp. 1S–48S. [PubMed] [Google Scholar]
- 11.Bertisch SM, Herzig SJ, Winkelman JW, et al. National use of prescription medications for insomnia: NHANES 1999-2010. Sleep. 2014;37:343–9. doi: 10.5665/sleep.3410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mason M, Cates CJ, Smith I. Effects of opioid, hypnotic and sedating medications on sleep-disordered breathing in adults with obstructive sleep apnoea. Cochrane Database Syst Rev. 2015;7:CD011090. doi: 10.1002/14651858.CD011090.pub2. [DOI] [PubMed] [Google Scholar]
- 13.Iber C, Ancoli-Israel S, Chesson A, Quan SQ. Westchester, IL: American Academy of Sleep Medicine; 2007. The AASM manual for the scoring of sleep and associated events: rules, terminology and technical specifications. [Google Scholar]
- 14.Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14:540–5. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 15.Buysse DJ, Reynolds CF, Monk TH, et al. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 16.The Criteria Committee of the New York Heart Association. Boston, MA: Little, Brown and Company; 1964. Diseases of the heart and blood vessels: nomenclature and criteria for diagnosis. [Google Scholar]
- 17.Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc. 1982;14:377–81. [PubMed] [Google Scholar]
- 18.Pratter MR, Curley FJ, Dubois J, et al. Cause and evaluation of chronic dyspnea in a pulmonary disease clinic. Arch Intern Med. 1989;149:2277–82. [PubMed] [Google Scholar]
- 19.Príncipe-Rodríguez K, Strohl KP, Hadziefendic S, et al. Sleep symptoms and clinical markers of illness in patients with heart failure. Sleep Breath. 2005;9:127–33. doi: 10.1007/s11325-005-0023-0. [DOI] [PubMed] [Google Scholar]
- 20.Zuurbier LA, Luik AI, Leening MJG, et al. Associations of heart failure with sleep quality: the Rotterdam Study. J Clin Sleep Med. 2015;11:117–21. doi: 10.5664/jcsm.4454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.IMS National Prescription Audit. Top 25 US Pharmaceutical Products by Dispensed Prescriptions. [Accessed September 18, 2015]. Available from: https://www.imshealth.com/files/web/Corporate/News/Top-Line%20Market%20Data/US_Top_25_Medicines_Dispensed_Prescriptions.pdf.
- 22.Zammit G. Comparative tolerability of newer agents for insomnia. Drug Saf. 2009;32:735–48. doi: 10.2165/11312920-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 23.Levy D, Larson MG, Vasan RS, et al. The progression from hypertension to congestive heart failure. JAMA. 1996;275:1557–62. [PubMed] [Google Scholar]
- 24.Scharf MB, Roth T, Vogel GW, et al. A multicenter, placebo-controlled study evaluating zolpidem in the treatment of chronic insomnia. J Clin Psychiatry. 1994;55:192–9. [PubMed] [Google Scholar]
- 25.Declerck A, Smits M. Zolpidem, a valuable alternative to benzodiazepine hypnotics for chronic insomnia? J Int Med Res. 1999;27:253–63. doi: 10.1177/030006059902700601. [DOI] [PubMed] [Google Scholar]
- 26.Holm KJ, Goa KL. Zolpidem: an update of its pharmacology, therapeutic efficacy and tolerability in the treatment of insomnia. Drugs. 2000;59:865–89. doi: 10.2165/00003495-200059040-00014. [DOI] [PubMed] [Google Scholar]
- 27.Fung MM, Peters K, Redline S, et al. Decreased slow wave sleep increases risk of developing hypertension in elderly men. Hypertension. 2011;58:596–603. doi: 10.1161/HYPERTENSIONAHA.111.174409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tanaka M, Suemaru K, Watanabe S, et al. Comparison of short-and long-acting benzodiazepine-receptor agonists with different receptor selectivity on motor coordination and muscle relaxation following thiopental-induced anesthesia in mice. J Pharmacol Sci. 2008;107:277–84. doi: 10.1254/jphs.fp0071991. [DOI] [PubMed] [Google Scholar]
- 29.Cirignotta F, Mondini S, Zucconi M, et al. Zolpidempolysomnographic study of the effect of a new hypnotic drug in sleep apnea syndrome. Pharmacol Biochem Behav. 1988;29:807–9. doi: 10.1016/0091-3057(88)90212-2. [DOI] [PubMed] [Google Scholar]
- 30.Rosenberg R, Roach JM, Scharf M, et al. A pilot study evaluating acute use of eszopiclone in patients with mild to moderate obstructive sleep apnea syndrome. Sleep Med. 2007;8:464–70. doi: 10.1016/j.sleep.2006.10.007. [DOI] [PubMed] [Google Scholar]
- 31.Eckert DJ, Owens RL, Kehlmann GB, et al. Eszopiclone increases the respiratory arousal threshold and lowers the apnoea/ hypopnoea index in obstructive sleep apnoea patients with a low arousal threshold. Clin Sci Lond Engl 1979. 2011;120:505–14. doi: 10.1042/CS20100588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Aurora RN, Chowdhuri S, Ramar K, et al. The treatment of central sleep apnea syndromes in adults: practice parameters with an evidence-based literature review and meta-analyses. Sleep. 2012;35:17–40. doi: 10.5665/sleep.1580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nieuwenhuijs D, Sarton E, Teppema LJ, et al. Respiratory sites of action of propofol: absence of depression of peripheral chemoreflex loop by low-dose propofol. Anesthesiology. 2001;95:889–95. doi: 10.1097/00000542-200110000-00017. [DOI] [PubMed] [Google Scholar]
- 34.Berry RB, Patel PB. Effect of zolpidem on the efficacy of continuous positive airway pressure as treatment for obstructive sleep apnea. Sleep. 2006;29:1052–6. doi: 10.1093/sleep/29.8.1052. [DOI] [PubMed] [Google Scholar]
- 35.Menon A, Kumar M. Influence of body position on severity of obstructive sleep apnea: a systematic review. ISRN Otolaryngol. 2013;2013:670381. doi: 10.1155/2013/670381. [DOI] [PMC free article] [PubMed] [Google Scholar]


