INTRODUCTION
Posttraumatic stress disorder (PTSD) is an anxiety disorder with serious health consequences, including substantial ramifications for those with diabetes. PTSD is characterized by a traumatic event or events causing significant distress or impairment, resulting in re-experiencing of trauma, avoidance of reminders of trauma, negative cognitions and mood, and arousal (American Psychiatric Association, 2013). Individuals with PTSD and diabetes experience worse health outcomes than those with diabetes alone (Miller et al., 2011; Trief et al., 2006). American Indians (AIs) endure higher rates of both PTSD (Beals et al., 2005) and diabetes (Blackwell et al., 2014; CDC, 2011) than the general United States population. These disparities highlight the need to investigate the impact of PTSD on diabetes-related health outcomes for AIs. The purpose of this research is to determine the associations of comorbid PTSD and depressive symptoms on health-related outcomes for AI adults with type 2 diabetes.
PTSD status has been linked to a host of physical ailments, including cardiovascular disease (Boscarino & Chang, 1999; Spitzer et al., 2009; Pietrzak et al., 2011), pulmonary disease (Lauterbach et al., 2005; Spitzer et al., 2009), gastrointestinal problems (Schnurr et al., 2000; Pietrzak et al., 2011; Lauterbach et al., 2005) and general vascular problems (Dirkzwager et al., 2007). PTSD diagnosis and symptomology have also been associated with a higher risk of both circulatory and musculoskeletal disorders (Ouimette et al., 2004). Symptoms of PTSD have been associated with poorer self-rated health (Wolfe et al., 1994; Lauterbach et al., 2005), higher risk of impaired functioning and lower quality of life (Zatzick et al., 1997; Johansen et al., 2007), more short- and long-term disability, and suicide attempts (Sareen et al., 2007). A recent meta-analysis supported the relationship between PTSD and several health outcomes, including general symptoms and general medical conditions (Pacella et al., 2013). In a population of patients with major depressive disorder, a positive PTSD screen was associated with worse depressive symptomatology, lower social support, and more outpatient health care visits (Campbell et al., 2007). Diagnosed PTSD and self-reported PTSD symptoms are also associated with diabetes (Lukaschek et al., 2013; Weisberg et al., 2002), and this association persists independently of depression (Agyemang et al., 2011). Prior diagnosis of PTSD is associated with significantly increased odds of diabetes diagnosis later in life (Boyko et al., 2010).
Thus, PTSD is broadly associated with deleterious health outcomes, yet the impact of comorbid PTSD on diabetes-related health outcomes has been explored to a limited extent. We found only two studies addressing the impact of PTSD on diabetes-related health outcomes. In a cohort of low-income minority individuals with diabetes, lifetime PTSD symptoms were significantly associated with glycosylated hemoglobin values (a marker of long-term blood glucose control) above goal levels (Miller et al., 2011). Among male veterans with diabetes, those with diagnosed PTSD were more likely to have higher cholesterol values than those without PTSD (Trief et al., 2006). Interestingly, those with PTSD and depression had higher rates of substance use disorder and cholesterol values compared to PTSD alone, depression alone, or neither (Trief et al., 2006), pointing to the potential additive impact of PTSD with depression on health.
Others have argued for a more complete and holistic view of mental health to understand the common, unique, and potentially additive impact on health (Prisciandaro et al., 2011; Walls et al., 2014). In the National Comorbidity Survey, 88% of males and 79% of females with PTSD had another psychiatric disorder (Kessler et al., 1995). Considering this overlap, investigating the impact of PTSD in combination with other mental health conditions could be useful. Depression in particular has been shown to have a relationship with diabetes control and diabetes-related outcomes (de Groot, Anderson, Freedland, Clouse, & Lustman, 2001; Ciechanowski, Katon, & Russo, 2000; Egede, Zheng, & Simpson, 2002; Egede, 2004; Egede, Nietert, & Zheng, 2005; Egede, 2007). This relationship has also been shown among AIs with diabetes (Singh et al., 2004; Sahota, Knowler, & Looker, 2008; Walls, Aronson, Soper, & Johnson-Jennings, 2014; Knaster, Fretts, & Phillips, 2015).
AIs have over 2 times the odds of lifetime PTSD (Beals et al., 2005), and are over two times more likely to have diabetes (Blackwell et al., 2014; CDC, 2011) than the general United States population. AI groups in the US also experience higher rates of traumatic events than those in the general population (Manson et al., 2005; Evans-Campbell et al., 2006; Evans-Campbell, 2008; Robin et al., 1997; Ehlers et al., 2013a; Karmali et al., 2005; Sugarman & Grossman, 1996). Past estimates of depression among AI adults exceed those of the general population, and range from 20–30% (U.S. Department of Health and Human Services, 2001). However, it is necessary to consider the socio-historical context in order to understand AI health and health outcomes. A history of collectively endured traumatic assaults due to the practices and policies perpetuated by colonization has resulted in intergenerational exposure and transmission of trauma (Brave Heart & DeBruyn, 1998; Brave Heart, 1999; Brave Heart, 2003). These traumas are historical in their origins, yet the assaults on AI culture and ways of life are manifested and permeate aspects of daily living today (Whitbeck et al., 2004; Whitbeck et al., 2009; Walls & Whitbeck, 2011). Other contemporary traumas, such as racism, discrimination, and violence, interplay with historical traumas (Whitbeck et al. 2004, Evans-Campbell, 2008; Walls & Whitbeck, 2011; Ehlers et al., 2013b). While the focus of this research was not to understand historical trauma, it is important to recognize the possible interplay between historical trauma, contemporary trauma, PTSD, and health disparities more broadly.
The impact of PTSD on diabetes-related health outcomes for AIs is unclear, particularly when considering comorbid depression. Understanding the interplay between diabetes and PTSD is needed, considering the high prevalence of both conditions for AIs. In this study, we estimate the prevalence of screened PTSD in a clinic sample of AIs with type 2 diabetes, investigate the relationship between PTSD symptoms and symptoms of hyperglycemia, hospitalizations, and self-rated health status, and consider these relationships in the context of comorbid depressive symptoms.
METHODS
Study Design
The Mino Giizhigad (A Good Day) Study is a community-based participatory research (CBPR) project with the Lac Courte Oreilles and Bois Forte Bands of Chippewa (while the term “Chippewa” is a corruption of Ojibwe, this terminology is incorporated into the formal Band names for the two communities participating in the study) and the University of Minnesota Medical School-Duluth. Both tribal communities consented to be named in public dissemination of research findings. The purpose of this study was to identify and describe the impact of mental and behavioral health factors on diabetes treatment and outcomes among Ojibwe adults with type 2 diabetes. Tribal resolutions from both communities were obtained prior to application submission for funding. The project began with community feasts and forums to discuss the study goals, obtain community feedback, and establish Community Research Councils (CRCs). CRC and university team members were active participants in the entire research process, from methodological planning to final data collection and analysis. The university of Minnesota IRB and Indian Health Services (IHS) National IRB reviewed and approved the methodology included in this study.
Participants
The sampling frame for this study included AI adults with type 2 diabetes utilizing care at one of two reservation health clinics. Clinic staff were trained to randomly select potential participants from health records. Individuals were eligible to participate if they were 18 years of age or older, had a documented diagnosis of type 2 diabetes in the medical record, and self-identified as American Indian.
Measures
Mental Health Problems
Posttraumatic Stress Disorder
PTSD was estimated using the Primary Care PTSD (PC-PTSD), a four-item screen for PTSD (Prins et al., 2003). Items were scored ‘Yes’ or ‘No’ (Yes = 1, No = 0), with a possible range from 0 – 4, and a score of 3 or higher indicating a positive screen. A cutoff score of 3 or higher has been significantly correlated with diagnosed PTSD, has a sensitivity of 78%, a specificity of 87%, an efficiency of 85%, and good test retest-reliability (Prins et al., 2003). In other analyses of the PC-PTSD, a score of 3 or higher was found to be the optimal cutoff score, with good sensitivity, specificity, positive and negative predictive values, and diagnostic efficiency in both military (Bliese et al., 2008) and civilian primary care samples (Freedy et al., 2010). The internal consistency of the PC-PTSD as measured by Cronbach’s alpha was 0.89 in our sample.
Depressive Symptoms
Depressive symptoms were evaluated using the nine-item Patient Health Questionnaire (PHQ-9; Kroenke et al., 2001). Individuals were asked to report over the past two weeks if they have been bothered by different symptoms (0 = not at all, 1 = several days, 2 = more than half the days, and 3 = almost every day), with a possible range from 0 to 27. A cutoff score of 10 or higher was used as criterion of depressive symptoms (Gilbody et al., 2007; Manea et al., 2012). This cutoff has a sensitivity of 91.7%, and a specificity of 78.3% (Gilbody et al., 2007). Cronbach’s alpha for the PHQ-9 was 0.898 in this study.
Health-related Outcomes
We chose to investigate certain health outcomes due to their significance in diabetes-related complications and quality of life (symptoms of hyperglycemia), health care costs (hospitalization), and overall health and mortality (self-rated health status). Symptoms of hyperglycemia are related to glycosylated hemoglobin (Cox et al., 1983; Kleefstra et al., 2005). They are also associated with health-related quality of life (Goddijn et al., 1999), even independent of glycosylated hemoglobin (Kleefstra et al., 2005). In fact, some measures of diabetes-specific health-related quality of life include measures of symptoms due to their importance. Thus, not only are symptoms of hyperglycemia linked to other measures glycemic control, they have dramatic importance to patient wellbeing. Poorer self-rated health status is associated with functional limitation (Idler, Russell, & Davis, 2000), poorer objective health status (Wu et al., 2013) and mortality (Brunner et al., 2013; McGee et al., 1999; Idler & Benyamini, 1997; Miilunpalo et al., 1997).
Participants were asked how many times in the past month they had high blood sugar with associated symptoms (i.e., symptoms of hyperglycemia). Response categories were ‘0 times’ (0), ‘1 – 3 times’ (1), ‘4 – 6 times’ (2), ‘7 – 12 times’ (3), and ‘More than 12 times’ (4). Individuals were also asked if during the past year had been a patient in a hospital overnight (Yes = 1, No = 0). We asked a single item to assess self-rate health status, “In general, would you say your health status is,” with response options of ‘Excellent’ (4), ‘Very good’ (3), ‘Good’ (2), ‘Fair’ (1), and ‘Poor’ (0).
Covariates
Participants self-reported their age in years, and reported their gender as either male or female (female = 1, male = 0). Educational attainment was assessed by highest level of education completed (‘Less than high school’, ‘High school or GED’, ‘Some college, vocational or technical training’, ‘College graduate’ or ‘Advanced Degree’). Participants were also asked to indicate their annual household income within $10,000 ranges. Using the midpoint of this range and the number of people living within the household, the federal poverty calculation was used to categorize participants as above or below the federal poverty level. For multivariable analyses, we used the midpoint of this range divided by the number of people living within the household as the indicator of per capita annual household income. We asked individuals their age and how long they had diabetes. Participants indicated whether or not they lived on or off reservation lands (on = 1, off = 0).
Procedure
Selected patients were mailed a welcome letter, an informational project brochure, and a contact information card with mail and phone-in options to decline participation. After allowing time for declined notices, trained community interviewers contacted remaining recruits to schedule interviews. Consenting participants were given a pound of locally cultivated wild rice and a $30 cash incentive. Paper-and-pencil interviewer-administered surveys were completed in participants’ location of choice, most often in private spaces within homes. In addition to the interviewer-administered portion, participants completed a self-report section containing questions that may have been sensitive or personal. The time to complete each survey ranged between approximately 1.5 – 3 hours.
All identifying information was removed from surveys and replaced with an identification number by an on-site project coordinator prior to sending to the university-based team. All survey data was entered and verified in electronic format by university research assistants. Of the 300 randomly sampled individuals, 11 were determined to be ineligible to participate (i.e., did not meet study inclusion criteria). Out of a total initial eligible sample of 289 individuals, 218 participants completed surveys for a final study response rate of 75.4%.
Analyses
Data were analyzed using the Statistical Package for the Social Sciences (SPSS, Version 20). Chi-square difference tests were used to examine differences in screened PTSD among different demographic groups. We compared the prevalence of PTSD by gender, education level, income, and depressive symptoms. We used multivariable logistic and linear regression to determine the relationship between health outcomes (symptoms of hyperglycemia, hospitalization, and self-rated health status) and PTSD symptoms (i.e., PC-PTSD raw score) after controlling for gender, location, reservation status, income, years with diabetes, and age. Due to prior research suggesting a relationship between PTSD and depression, we conducted two-step hierarchical regressions, where depressive symptoms were entered on the second step. We further examined possible interactive effects of PTSD and depressive symptoms on outcomes. Additionally, we used Chi-square tests to investigate differences in health outcomes across four categories: 1) no screened PTSD and no depressive symptoms, 2) screened PTSD with no depressive symptoms, 3) depressive symptoms with no screened PTSD, and 4) both screened PTSD and depressive symptoms.
RESULTS
Table 1 displays the prevalence of PTSD symptoms by demographic characteristics. The mean age of participants was 56.5 years, with an average longevity of diabetes of 14.7 years. Over three quarters (76%) reported that they lived on reservation land. The average per capita household income was $10,331, and 44% were living below the federal poverty limit. Using a cutoff score of 3 or higher on the PC-PTSD, 45 (21.8%) participants screened positive for PTSD. Using a criterion score of 10 or more on the PHQ-9, 17.1% of participants were classified as experiencing depressive symptoms. In total, 23 (11.2%) were classified as screened PTSD only, 15 (7.3%) depressive symptoms only, and 21 (10.2%) both. Nearly a quarter of participants (22.1%) had a hospitalization in the past year. The majority of participants reported fair (28.2%) good (38.9%), or very good (20.4%) self-rated health status. Poor self-rated health status was reported by 10.6% of participants. Over half reported experiencing symptoms of hyperglycemia in the past month, with 27.6% reporting 1–3 times, 9.8% reporting 4–6 times, 7.5% reporting 7–12 times, and 8.9% reporting more than 12 times. We found significant age differences (p = 0.001) in prevalence of PTSD, the oldest cohort (65 and older) having the lowest proportion. A significantly higher proportion of individuals with depressive symptoms screened positive for PTSD (p < 0.001), compared to those who did not have depressive symptoms. No significant differences in PTSD rates by gender, educational, or income statuses were found.
Table 1.
Demographic characteristics of study participants
| Variable | Total % of sample | Positive screen for PTSD n (%) | p-valuea | |
|---|---|---|---|---|
|
| ||||
| Total | ||||
|
| ||||
| – | 45 (21.8%) | – | ||
|
| ||||
| Age | ||||
|
| ||||
| 18–49 | 33% | 24 (33.8%) | 0.001 | |
| 50–64 | 35.3% | 16 (22.5%) | ||
| 65 and older | 31.7% | 5 (7.8%) | ||
|
| ||||
| Gender | ||||
|
| ||||
| Female | 56.4% | 29 (24.8%) | 0.241 | |
| Male | 43.6% | 16 (18.0%) | ||
|
| ||||
| Educational Attainment | ||||
|
| ||||
| Less than high school | 11.1% | 5 (23.8%) | 0.128 | |
| High school or GED | 28.6% | 10 (16.7%) | ||
| Some college, vocational or technical training | 44.7% | 24 (26.1%) | ||
| College graduate or advanced degree | 15.7% | 9 (28.1%) | ||
|
| ||||
| Income | ||||
|
| ||||
| Less than federal poverty level | 44.4% | 23 (25%) | 0.359 | |
| Greater than federal poverty level | 55.6% | 22 (19.6%) | ||
|
| ||||
| Currently living on reservation lands | ||||
|
| ||||
| Yes | 77.5% | 32 (20.3%) | 0.316 | |
|
| ||||
| No | 22.5% | 13 (27.1%) | ||
|
| ||||
| Depressive symptoms | ||||
|
| ||||
| Yes | 17.1% | 21 (58.3%) | 0.000 | |
| No | 82.9% | 23 (13.6%) | ||
χ2 difference test
Regression analyses were conducted to evaluate the relationship between PTSD symptoms and health-related outcomes (i.e. quantity of past month symptoms of hyperglycemia, self-rated health status, and hospitalization in the past year) after controlling for several other variables as shown in Table 2. In the first model, these controls included age, gender, study location, residing on or off reservation lands, years with diabetes, and per capita income. The second model added depressive symptoms. PTSD symptoms were not significantly related to symptoms of hyperglycemia. Prior to controlling for depressive symptoms, PTSD symptoms were negatively related self-rated health status, and positively related to hospitalization. However, these relations were no longer significant after controlling for depressive symptoms. An interaction term between standardized PTSD and depressive symptom scores was non-significant in regression models for each dependent variable (not shown).
Table 2.
Regression Analyses of Health-related Outcomes
| Predictors | Symptoms of hyperglycemiaa | Self-rated health statusa | Hospitalizationb | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| Model 1 | Model 2 | Model 1 | Model 2 | Model 1 | Model 2 | |||||||
| B (SE) | β | B (SE) | β | B (SE) | β | B (SE) | β | B (SE) | OR | B (SE) | OR | |
| Age | −.03 (.01) | −.27d | −.02 (.01) | −.25d | .01 (.01) | .09 | .01 (.01) | .07 | .00 (.02) | 1.00 | .01 (.02) | 1.01 |
| Gender (female = 1) | .00 (.18) | .00 | −.04 (.18) | −.01 | −.10 (.14) | −.05 | −.06 (.13) | −.03 | .07 (.37) | 1.07 | .06 (.38) | 1.06 |
| Location | .11 (.19) | .04 | .03 (.18) | .01 | −.16 (.14) | −.08 | −.09 (.13) | −.05 | 1.22 (.42) | 3.40d | 1.18 (.42) | 3.26d |
| On/off reservation (on = 1) | .33 (.23) | .11 | .37 (.22) | .12 | .01 (.17) | .00 | −.03 (.16) | −.01 | −.21 (.43) | 0.81 | −.13 (.45) | 0.88 |
| Year with diabetes | .02 (.01) | .16c | .02 (.01) | .16c | −.01 (.01) | −.12 | −.01 (.01) | −.13 | .01 (.02) | 1.01 | .01 (.02) | 1.01 |
| Per capita income | .01 (.01) | .06 | .01 (.01) | .10 | .02 (.01) | .15c | .01 (.01) | .10 | −.02 (.02) | 0.98 | −.01 (.02) | 0.99 |
| PTSD symptoms | .06 (.06) | .07 | −.07 (.07) | −.07 | −.11 (.05) | −.17c | .02 (.05) | .02 | .31 (.12) | 1.36e | .19 (.14) | 1.21 |
| Depressive symptoms | .07 (.02) | .32e | −.07 (.01) | −.41e | .08 (.04) | 1.08c | ||||||
| Constant | 1.78 (.51) | 1.45 (.50) | 1.59 (.38) | 1.91 (.36) | −2.36 (1.03) | −3.00 (1.10) | ||||||
Linear regression;
Logistic regression;
P < 0.05;
P < 0.01;
P < 0.001
Figure 1 provides shows the differences between groups with neither screened PTSD nor depressive symptoms, screened PTSD alone, depressive symptoms alone, and both. Chi-square difference tests indicated significant differences between groups for any past month hypoglycemia symptoms (p = 0.030), past year hospitalization (p = 0.001), and poor self-rated health status (p = 0.002). The major contributor to each of these differences was a disproportionately high proportion of negative outcomes among those with both screened PTSD and depressive symptoms.
Figure 1.
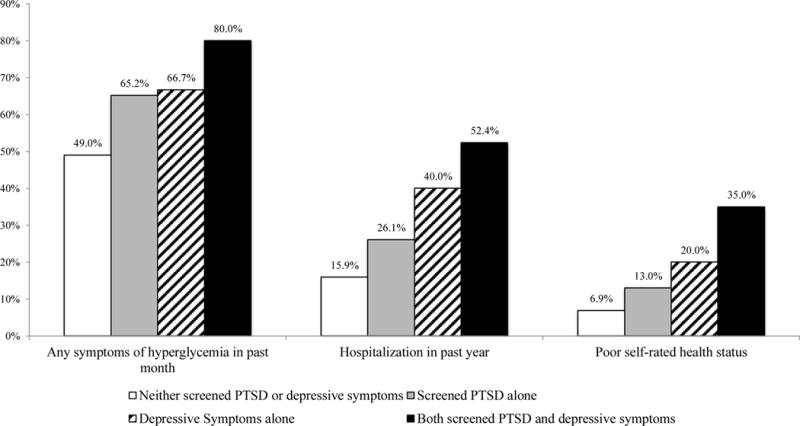
Percent Reporting Health-related Outcome by Mental Health Status
DISCUSSION
This cross-sectional study investigated the prevalence of screened PTSD among AI adults with type 2 diabetes, and explored the relationship between PTSD symptoms and health-related outcomes. Over 1 in 5 of the participants in this study (21.8%) screened positive for PTSD using a cutoff of 3 or higher on the PC-PTSD. The rate of screened PTSD using the PC-PTSD with a cutoff of 3 or higher has in past research ranged between 4.8% for United Kingdom military personnel in service during the 2003 Iraq War (Iversen et al., 2009), 10% for newly diagnosed breast cancer patients (Hegel et al., 2006), 13% for US soldiers returning from Operation Iraqi Freedom (Maguen et al., 2010), and 36% for a sample of depressed patients (Campbell et al., 2007). It is startling that our clinic sample of AIs with type 2 diabetes has such strikingly high rates of screened PTSD when compared to combat veterans and cancer patients. But this seems to be consistent with prior literature regarding PTSD among AIs compared to majority populations. For instance, a sample of tribal members aged 15–54 from the Northern Plains had over two times the odds of lifetime PTSD compared to a national sample (Beals et al., 2005).
In this study, younger participants and those with depressive symptoms were more likely to screen positive for PTSD. Prior literature has suggested that younger individuals experience higher levels of PTSD symptomatology (Kessler et al., 1995; Ditlevsen & Elklit, 2010). A possible explanation for this finding may exist in the emotional processing of memories. In an emotionally adaptive manner, older adults modify memories of past negative events to minimize unpleasant emotions to a greater extent than do younger adults (Boals et al., 2014). The cultural position of elders in AI communities, one of respect and reverence, may also explain this difference. Some prior literature suggests rates of PTSD differ by gender, with women having higher rates (Kessler et al., 1995; Ditlevsen & Elklit, 2010; Freedy et al., 2010). As noted, we found no significant differences in PTSD by gender. In some previous studies, rates of traumatic events for AIs were similar across gender (Flett et al., 2004; Manson et al., 2005; Klest et al., 2013), as were rates of PTSD (Robin et al., 1997), potentially indicating the impact of cultural and social factors on trauma and PTSD. Contrarily, Ehlers and colleagues (2013a) reported a larger proportion of AI women than men with diagnosed PTSD. This variation between AI groups may be explained by regional and cultural differences between different tribal groups.
Prior literature has purported PTSD to be associated with negative diabetes-related health outcomes, such as higher cholesterol levels (Trief et al., 2006) and worse blood glucose control (Miller et al., 2011). After controlling for several demographic variables, we found no relationship between PTSD symptoms and past month symptoms of hyperglycemia. This is consistent with findings from the Strong Heart Family Study, a large epidemiological study of cardiovascular disease among AI adults, which found no difference in glycemic control among those with diabetes between psychological trauma symptoms (i.e., no trauma, trauma but no symptoms, symptoms but no PTSD, and presumptive PTSD; Jacob et al., 2013). However, our findings suggest PTSD symptoms from a short screener are associated with self-rated health status and past year hospitalization, but not when also considering the influence of depressive symptoms. The co-linearity between PTSD symptoms and depressive symptoms in this study may partially explain the non-significance of PTSD symptoms in the complete model, but these findings suggest a potentially more complex relationship between mental health symptomatology and chronic disease outcomes.
Indeed, others have found a potential compounding of negative effects for individuals with multiple psychiatric diagnoses/symptoms. In a sample of male veterans with diabetes, those with PTSD and depression had higher cholesterol values and were 48% more likely to have glycosylated hemoglobin above goal level than individuals with PTSD alone (Trief et al., 2006). When dichotomizing mental health conditions on the basis of standard cut points, we found the highest rates of negative health outcomes for those with depressive symptoms and co-occurring screened PTSD, with 80% reporting any symptoms of hyperglycemia in the last 30 days, 52.4% having been hospitalized in the past year, and 35% reporting poor self-rated health. Our findings based upon categorical groupings of individuals suggest a cumulative or additive impact of depressive symptoms and screened PTSD on some health-related outcomes. However, the reduction of multiple independent variables, our continuous symptom scores, to dichotomous groups may produce spurious statistical significance (Maxwell & Delaney, 1993). The interaction term between these two mental health constructs as continuous variables was not significant in our multivariable models. Thus, the effects of comorbid screened PTSD on health do not appear to vary as a function of levels of depressive symptoms (or vice versa). Future research should further investigate the additive and unique impacts of mental health diagnoses on health outcomes for those with diabetes.
The results of this study must be juxtaposed with the limitations of the design. In this work we acknowledge the limitations of diagnostic categories and the socio-historical context of AI health, yet chose to operationalize PTSD as a means of understanding its impact on diabetes. While diagnostic categories such as PTSD include symptomatology that may be experienced by AIs, the categories do not fully explore intergenerational transmission of trauma from other individuals or within communities (Evans-Campbell, 2008), and they do not encompass culturally specific conceptions of mental health. While it is known that PTSD symptomology impacts Indigenous health (Nadew, 2012), current conceptions of PTSD fail to offer insights into the relationship between historical and contemporary trauma (Evans-Campbell, 2008). This study did not capture clinically diagnosed psychiatric conditions, and as such these results are limited. However, we did employ commonly used, validated screening instruments that assess current symptoms. These screeners may serve quite useful for primary care providers in a clinic setting in order to identify individuals for referral to mental health services. Another potential criticism of this work is the use of the cutoff of 3 or higher on the PC-PTSD to define a case. While we used the generally accepted cutoff in the literature, it may underestimate cases compared to a cutoff of 2 or higher. We relied upon self-report of symptoms of hyperglycemia and utilization of hospital services. It is possible that self-report bias or recall bias may have influenced the results, and that actual glycemic control or utilization may differ from what was reported by participants. Of particular note, hospitalizations in this study captured any hospitalization, diabetes-related or otherwise, meaning we cannot infer that poor diabetes control contributed to hospitalizations. While all-cause hospitalization is an important outcome given its connection to health and ramifications for health care costs, future work may investigate diabetes-related hospitalizations specifically. Additionally, the cross-sectional design of this study precludes causal inferences, thus our conclusions must be restrained to associations between mental health symptoms and health outcomes. Longitudinal studies are needed to determine the impact of PTSD and depression on diabetes related outcomes over time.
This study highlights a continued need to address the mental health needs of individuals with diabetes. Although level of PTSD symptoms did not have a significant relationship with symptoms of hyperglycemia, hospitalization, and self-rated health status after controlling for depressive symptoms, screened PTSD with comorbid depressive symptoms should be judiciously addressed in individuals with diabetes. Recommendations for treatment of PTSD include a multidisciplinary plan concentrated on trauma-focused psychotherapy and pharmacotherapy (Warner et al., 2013). Cognitive trauma therapy has proved useful in reducing PTSD, depression, and guilt among an ethnically diverse group of women who had been abused (Kubany et al., 2003; Kubany et al., 2004). Unfortunately, fear of talking to someone about trauma, and fear of medication side effects serve as reasons for not seeking help for trauma-related symptoms (Ghafoori et al., 2014). Other barriers to mental health treatment include feelings of fear and helplessness, distrust, low mental health literacy, and psychosocial issues (Bassett et al., 2012; Ghafoori et al., 2014). In order to address these barriers, AI and Alaska Native healers have identified culture as the primary vehicle for the delivery of trauma treatment (Bassett et al., 2012). Depression is traditionally treated with a variety of modalities that include a combination of antidepressant medication, psychotherapy, and other somatic therapies (American Psychiatric Association, 2010). Kaufman and colleagues (2013), who analyzed data from a large representative psychiatric epidemiological study among AIs in two reservation communities, found that depression was related to family, cultural, or community dynamics—most likely all three – which has implications for treatment considerations for depression in AI individuals. Treatment interventions that address interpersonal relationships and family dynamics may be effective in treating depression that is related to family factors (Dirmaier et al., 2012; Brakemeir & Frase, 2012). Culturally rooted and community developed means to address mental health conditions have significant potential to improve health (Gone, 2013; Kirmayer, Simpson, & Cargo, 2003).
Acknowledgments
The Mino Giizhigad Team includes Community Research Council members: Doris Isham, Julie Yaekel-Black Elk, Tracy Martin, Sidnee Kellar, Robert Miller, Geraldine Whiteman, Peggy Connor, Michael Connor, Stan Day, Pam Hughes, Jane Villebrun, Muriel Deegan, Beverly Steel, and Ray Villebrun. The authors respectfully acknowledge the commitment and participation of project team members in addition to their thoughtful review of this manuscript. The authors would also like to acknowledge the contributions of Garrett Soper to the conception and development of this manuscript.
Funding:
Research reported in this paper was supported by the National Institute of Mental Health under Award Number MH085852 (M. Walls, Principal Investigator). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Dr. Aronson gratefully acknowledges support from an American Foundation for Pharmaceutical Education Fellowship and a Health Services Dissertation Award (R36) from the Agency for Healthcare Research and Quality.
Footnotes
Conflict of interest statements: The authors declare no conflicts of interest.
Informed consent: All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all participants being included in the study.
References
- Agyemang C, Goosen S, Anujuo K, Ogedegbe G. Relationship between post-traumatic stress disorder and diabetes among 105 180 asylum seekers in the Netherlands. The European Journal of Public Health. 2012;22(5):658–662. doi: 10.1093/eurpub/ckr138. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th. Arlington, VA: American Psychiatric Association; 2013. [Google Scholar]
- American Psychiatric Association. Practice Guideline for the Treatment of Patients with Major Depressive Disorder. 3rd. Arlington, VA: American Psychiatric Association; 2010. [PubMed] [Google Scholar]
- Bassett D, Tsosie U, Nannauck S. “Our Culture Is Medicine”: Perspectives of Native Healers on Posttrauma Recovery Among American Indian and Alaska Native Patients. The Permanente Journal. 2012;16(1):19–27. doi: 10.7812/tpp/11-123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beals J, Novins DK, Whitesell NR, Spicer P, Mitchell CM, Manson SM. Prevalence of mental disorders and utilization of mental health services in two American Indian reservation populations: mental health disparities in a national context. American Journal of Psychiatry. 2005;162(9):1723–1732. doi: 10.1176/appi.ajp.162.9.1723. [DOI] [PubMed] [Google Scholar]
- Blackwell DL, Lucas JW, Clarke TC. Summary health statistics for U.S. adults: National Health Interview Survey, 2012. Vital and health statistics Series 10, Data from the National Health Survey. 2014;(260):1–171. [PubMed] [Google Scholar]
- Bliese PD, Wright KM, Adler AB, Cabrera O, Castro CA, Hoge CW. Validating the primary care posttraumatic stress disorder screen and the posttraumatic stress disorder checklist with soldiers returning from combat. Journal of consulting and clinical psychology. 2008;76(2):272–281. doi: 10.1037/0022-006X.76.2.272. [DOI] [PubMed] [Google Scholar]
- Boals A, Hayskip B, Banks J. Age Differences in Autobiographical Memories of Negative Events. Int’l J Aging and Human Development. 2014;78(1):47–65. doi: 10.2190/AG.78.1.d. [DOI] [PubMed] [Google Scholar]
- Boyko EJ, Jacobson IG, Smith B, Ryan MA, Hooper TI, Amoroso PJ, Smith TC. Risk of diabetes in US military service members in relation to combat deployment and mental health. Diabetes care. 2010;33(8):1771–1777. doi: 10.2337/dc10-0296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boscarino JA, Chang J. Electrocardiogram abnormalities among men with stress-related psychiatric disorders: implications for coronary heart disease and clinical research. Ann Behav Med. 1999;21:227–234. doi: 10.1007/BF02884839. [DOI] [PubMed] [Google Scholar]
- Brakemeier EL, Frase L. Interpersonal psychotherapy (IPT) in major depressive disorder. European Archives of Psychiatry and Clinical Neuroscience. 2012;262:117–121. doi: 10.1007/s00406-012-0357-0. [DOI] [PubMed] [Google Scholar]
- Brave Heart MYH. Oyate Ptayela: Rebuilding the Lakota Nation through addressing historical trauma among Lakota parents. Journal of Human Behavior in the Social Environment. 1999;2(1–2):109–126. [Google Scholar]
- Brave Heart MYH. The historical trauma response among Natives and its relationship with substance abuse: A Lakota illustration. Journal of psychoactive drugs. 2003;35(1):7–13. doi: 10.1080/02791072.2003.10399988. [DOI] [PubMed] [Google Scholar]
- Brave Heart MYH, DeBruyn LM. The American Indian Holocaust: Healing historical unresolved grief. American Indian and Alaska Native Mental Health Research. 1998;8:56–78. [PubMed] [Google Scholar]
- Brunner R, Stefanick ML, Aragaki AK, Beresford SAA, Hubbell FA. Self-rated Health and Medical Outcomes in the Women’s Health Initiative: The Aging Continuum, Health, Morbidity, Mortality. J Gerontol Geriat Res. 2013;3(139) doi: 10.4172/2167-7182.1000139. [DOI] [Google Scholar]
- Campbell DG, Felker BL, Liu CF, Yano EM, Kirchner JE, Chan D, Chaney EF. Prevalence of depression–PTSD comorbidity: Implications for clinical practice guidelines and primary care-based interventions. Journal of General Internal Medicine. 2007;22(6):711–718. doi: 10.1007/s11606-006-0101-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) National diabetes fact sheet: national estimates and general information on diabetes and prediabetes in the United States, 2011. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2011. [Google Scholar]
- Ciechanowski PS, Katon WJ, Russo JE. Depression and diabetes: impact of depressive symptoms on adherence, function, and costs. Archives of internal medicine. 2000;160(21):3278–3285. doi: 10.1001/archinte.160.21.3278. [DOI] [PubMed] [Google Scholar]
- Cox DJ, Gonder-Frederick L, Pohl S, Pennebaker JW. Reliability of symptom-blood glucose relationships among insulin-dependent adult diabetics. Psychosomatic medicine. 1983;45(4):357–360. doi: 10.1097/00006842-198308000-00009. [DOI] [PubMed] [Google Scholar]
- De Groot M, Anderson R, Freedland KE, Clouse RE, Lustman PJ. Association of depression and diabetes complications: a meta-analysis. Psychosomatic medicine. 2001;63(4):619–630. doi: 10.1097/00006842-200107000-00015. [DOI] [PubMed] [Google Scholar]
- Ditlevsen DN, Elklit A. The combined effect of gender and age on post traumatic stress disorder: do men and women show differences in the lifespan distribution of the disorder. Ann Gen Psychiatry. 2010;9:32. doi: 10.1186/1744-859X-9-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dirkzwager AJE, Van Der Velden PG, Grievink L, Yzermans CJ. Disaster-Related Posttraumatic Stress Disorder and Physical Health. Psychosomatic Medicine. 2007;69:435–440. doi: 10.1097/PSY.0b013e318052e20a. [DOI] [PubMed] [Google Scholar]
- Dirmaier J, Steinmann M, Krattenmacher T, Watzke B, Barghaan D, Koch U, Schulz H. Non-pharmacological treatment of depressive disorders: A review of evidence-based treatment options. Reviews on recent clinical trials. 2012;7(2):141–149. doi: 10.2174/157488712800100233. [DOI] [PubMed] [Google Scholar]
- Egede LE. Major depression in individuals with chronic medical disorders: prevalence, correlates and association with health resource utilization, lost productivity and functional disability. General hospital psychiatry. 2007;29(5):409–416. doi: 10.1016/j.genhosppsych.2007.06.002. [DOI] [PubMed] [Google Scholar]
- Egede LE. Diabetes, major depression, and functional disability among US adults. Diabetes care. 2004;27(2):421–428. doi: 10.2337/diacare.27.2.421. [DOI] [PubMed] [Google Scholar]
- Egede LE, Nietert PJ, Zheng D. Depression and all-cause and coronary heart disease mortality among adults with and without diabetes. Diabetes Care. 2005;28(6):1339–1345. doi: 10.2337/diacare.28.6.1339. [DOI] [PubMed] [Google Scholar]
- Egede LE, Zheng D, Simpson K. Comorbid depression is associated with increased health care use and expenditures in individuals with diabetes. Diabetes care. 2002;25(3):464–470. doi: 10.2337/diacare.25.3.464. [DOI] [PubMed] [Google Scholar]
- Ehlers CL, Gizer IR, Gilder DA, Yehuda R. Lifetime history of traumatic events in an American Indian community sample: Heritability and relation to substance dependence, affective disorder, conduct disorder and PTSD. Journal of psychiatric research. 2013a;47(2):155–161. doi: 10.1016/j.jpsychires.2012.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehlers CL, Gizer IR, Gilder DA, Ellingson JM, Yehuda R. Measuring historical trauma in an American Indian community sample: contributions of substance dependence, affective disorder, conduct disorder and PTSD. Drug Alcohol Depend. 2013b;133(1):180–7. doi: 10.1016/j.drugalcdep.2013.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans-Campbell T. Historical trauma in American Indian/Native Alaska communities: A multilevel framework for exploring impacts on individuals, families, and communitites. Journal of Interpersonal Violence. 2008;23:316–338. doi: 10.1177/0886260507312290. [DOI] [PubMed] [Google Scholar]
- Evans-Campbell T, Lindhorst T, Huang B, Walters KL. Interpersonal violence in the lives of urban American Indian and Alaska Native women: Implications for health, mental health, and help-seeking. American Journal of Public Health. 2006;96(8):1416–1422. doi: 10.2105/AJPH.2004.054213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flett RA, Kazantzis N, Long NR, MacDonald C, Millar M. Gender and ethnicity differences in the prevalence of traumatic events: Evidence from a New Zealand community sample. Stress and health. 2004;20(3):149–157. [Google Scholar]
- Freedy JR, Steenkamp MM, Magruder KM, Yeager DE, Zoller JS, Hueston WJ, Carek PJ. Post-traumatic stress disorder screening test performance in civilian primary care. Family practice. 2010;27(6):615–624. doi: 10.1093/fampra/cmq049. [DOI] [PubMed] [Google Scholar]
- Ghafoori B, Barragan B, Palinkas L. Mental Health Service Use Among Trauma-Exposed Adults: A Mixed-Methods Study. J Nerv Ment Dis. 2014;202(3):239–46. doi: 10.1097/NMD.0000000000000108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbody S, Richards D, Barkham M. Diagnosing depression in primary care using self-completed instruments: UK validation of PHQ–9 and CORE–OM. British Journal of General Practice. 2007;57(541):650–652. [PMC free article] [PubMed] [Google Scholar]
- Goddijn PPM, Bilo HJG, Feskens EJM, Groenier KH, Van der Zee KI, De Jong BM. Longitudinal study on glycaemic control and quality of life in patients with Type 2 diabetes mellitus referred for intensified control. Diabetic Medicine. 1999;16(1):23–30. doi: 10.1046/j.1464-5491.1999.00002.x. [DOI] [PubMed] [Google Scholar]
- Gone JP. Redressing First Nations historical trauma: theorizing mechanisms for indigenous culture as mental health treatment. Transcultural psychiatry. 2013;50(5):683–706. doi: 10.1177/1363461513487669. [DOI] [PubMed] [Google Scholar]
- Hegel MT, Moore CP, Collins ED, Kearing S, Gillock KL, Riggs RL, Ahles TA. Distress, psychiatric syndromes, and impairment of function in women with newly diagnosed breast cancer. Cancer. 2006;107(12):2924–2931. doi: 10.1002/cncr.22335. [DOI] [PubMed] [Google Scholar]
- Idler EL, Benyamini Y. Self-rated health and mortality: a review of twenty-seven community studies. Journal of health and social behavior. 1997;38(1):21–37. [PubMed] [Google Scholar]
- Idler EL, Russell LB, Davis D. Survival, functional limitations, and self-rated health in the NHANES I Epidemiologic Follow-up Study, 1992. American journal of epidemiology. 2000;152(9):874–883. doi: 10.1093/aje/152.9.874. [DOI] [PubMed] [Google Scholar]
- Iversen AC, van Staden L, Hughes JH, Browne T, Hull L, Hall J, Fear NT. The prevalence of common mental disorders and PTSD in the UK military: using data from a clinical interview-based study. BMC psychiatry. 2009;9(1):68. doi: 10.1186/1471-244X-9-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacob MM, Gonzales KL, Calhoun D, Beals J, Jacobsen Muller C, Goldberg J, Howard BV. Psychological trauma symptoms and type 2 diabetes prevalence, glucose control, and treatment modality among American Indians in the Strong Heart Family Study. Journal of Diabetes and Its Complications. 2013;27:553–557. doi: 10.1016/j.jdiacomp.2013.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johansen VA, Wahl AK, Eilertsen DE, Weisaeth L, Hanestad BR. The predictive value of posttraumatic stress disorder symptoms for quality of life: a longitudinal study of physically injured victims of non-domestic violence. Health Qual Life Outcomes. 2007;5:26. doi: 10.1186/1477-7525-5-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karmali S, Laupland K, Harrop AR, Findlay C, Kirkpatrick AW, Winston B, Hameed M. Epidemiology of severe trauma among status Aboriginal Canadians: a population-based study. Canadian Medical Association Journal. 2005;172(8):1007–1011. doi: 10.1503/cmaj.1040432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaufman CE, Beals J, Croy C, Jiang L, Novins DK, AI-SUPERPFP Team Multilevel context of depressions in two American Indian Tribes. Journal of consulting and clinical psychology. 2013;81(6):1040–1051. doi: 10.1037/a0034342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Archives of general psychiatry. 1995;52(12):1048. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Kirmayer L, Simpson C, Cargo M. Healing Traditions: culture, community and mental health promotion with Canadian Aboriginal peoples. Australiasian Psychiatry. 2003;11(S1):S15–S23. [Google Scholar]
- Kleefstra N, Ubink-Veltmaat LJ, Houweling ST, Groenier KH, Meyboom-de Jong B, Bilo HJ. Cross-sectional relationship between glycaemic control, hyperglycaemic symptoms and quality of life in type 2 diabetes (ZODIAC-2) Neth J Med. 2005;63(6):215–221. [PubMed] [Google Scholar]
- Klest B, Freyd JJ, Foynes MM. Trauma exposure and posttraumatic symptoms in Hawaii: Gender, ethnicity, and social context. Psychological Trauma: Theory, Research, Practice, and Policy. 2013;5(5):409–416. doi: 10.1037/a0029336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knaster ES, Fretts AM, Phillips LE. The association of depression with diabetes management among urban American Indians/Alaska Natives in the United States, 2011. Ethnicity & Disease. 2015;25(1):83–89. [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB. The Phq-9. Journal of general internal medicine. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kubany ES, Hill EE, Owens JA, Iannce-Spencer C, McCaig MA, Tremayne KJ, Williams PL. Cognitive trauma therapy for battered women with PTSD (CTT-BW) Journal of Consulting and clinical Psychology. 2004;72(1):3–18. doi: 10.1037/0022-006X.72.1.3. [DOI] [PubMed] [Google Scholar]
- Kubany ES, Hill EE, Owens JA. Cognitive trauma therapy for battered women with PTSD: Preliminary findings. Journal of Traumatic Stress. 2003;16(1):81–91. doi: 10.1023/A:1022019629803. [DOI] [PubMed] [Google Scholar]
- Lauterbach D, Vora R, Rakow M. The Relationship Between Posttraumatic Stress Disorder and Self-Reported Health Problems. Psychosomatic Medicine. 2005;67:939–947. doi: 10.1097/01.psy.0000188572.91553.a5. [DOI] [PubMed] [Google Scholar]
- Lukaschek K, Baumert J, Kruse J, Emeny RT, Lacruz ME, Huth C, Ladwig KH. Relationship between posttraumatic stress disorder and Type 2 Diabetes in a population-based cross-sectional study with 2970 participants. Journal of psychosomatic research. 2013;74(4):340–345. doi: 10.1016/j.jpsychores.2012.12.011. [DOI] [PubMed] [Google Scholar]
- Manea L, Gilbody S, McMillan D. Optimal cut-off score for diagnosing depression with the Patient Health Questionnaire (PHQ-9): a meta-analysis. Canadian Medical Association Journal. 2012;184(3):E191–E196. doi: 10.1503/cmaj.110829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maguen S, Lucenko BA, Reger MA, Gahm GA, Litz BT, Seal KH, Marmar CR. The impact of reported direct and indirect killing on mental health symptoms in Iraq war veterans. Journal of Traumatic Stress. 2010;23(1):86–90. doi: 10.1002/jts.20434. [DOI] [PubMed] [Google Scholar]
- Manson SM, Beals J, Klein SA, Croy CD, AI-SUPERPFP team Social epidemiology of trauma among 2 American Indian reservation populations. American journal of public health. 2005;95(5):851–859. doi: 10.2105/AJPH.2004.054171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maxwell SE, Delaney HD. Bivariate median splits and spurious statistical significance. Psychological bulletin. 1993;113(1):181–190. [Google Scholar]
- McGee DL, Liao Y, Cao G, Cooper RS. Self-reported health status and mortality in a multiethnic US cohort. American journal of epidemiology. 1999;149(1):41–46. doi: 10.1093/oxfordjournals.aje.a009725. [DOI] [PubMed] [Google Scholar]
- Miilunpalo S, Vuori I, Oja P, Pasanen M, Urponen H. Self-rated health status as a health measure: the predictive value of self-reported health status on the use of physician services and on mortality in the working-age population. Journal of clinical epidemiology. 1997;50(5):517–528. doi: 10.1016/s0895-4356(97)00045-0. [DOI] [PubMed] [Google Scholar]
- Miller SA, Mancuso CA, Boutin-Foster C, Michelen W, McLean-Long C, Foote B, Charlson ME. Associations between posttraumatic stress disorder and hemoglobin A1C in low-income minority patients with diabetes. General hospital psychiatry. 2011;33(2):116–122. doi: 10.1016/j.genhosppsych.2010.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nadew GT. Exposure to traumatic events, prevalence of posttraumatic stress disorder and alcohol abuse in Aboriginal communities. Rural and remote health. 2012;12(4):1667. [PubMed] [Google Scholar]
- Ouimette P, Cronkite R, Henson BR, Prins A, Gima K, Moos RH. Posttraumatic stress disorder and health status among female and male medical patients. Journal of Traumatic Stress. 2004;17(1):1–9. doi: 10.1023/B:JOTS.0000014670.68240.38. [DOI] [PubMed] [Google Scholar]
- Pacella ML, Hruska B, Delahanty DL. The physical health consequences of PTSD and PTSD symptoms: a meta-analytic review. Journal of anxiety disorders. 2013;27(1):33–46. doi: 10.1016/j.janxdis.2012.08.004. [DOI] [PubMed] [Google Scholar]
- Pietrzak RH, Goldstein RB, Southwick SM, Grant BF. Medical Comorbidity of Full and Partial Posttraumatic Stress Disorder in US Adults: Results From Wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. Psychosomatic Medicine. 2011;73(8):697–707. doi: 10.1097/PSY.0b013e3182303775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prins A, Ouimette P, Kimerling R, Camerond RP, Hugelshofer DS, Shaw-Hegwer J, Sheikh JI. The primary care PTSD screen (PC-PTSD): development and operating characteristics. International Journal of Psychiatry in Clinical Practice. 2003;9(1):9–14. [Google Scholar]
- Prisciandaro JJ, Gebregziabher M, Grubaugh AL, Gilbert GE, Echols C, Egede LE. Impact of psychiatric comorbidity on mortality in veterans with type 2 diabetes. Diabetes Technology & Therapeutics. 2011;13(1):73–78. doi: 10.1089/dia.2010.0092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robin RW, Chester B, Rasmussen JK, Jaranson JM, Goldman D. Prevalence and characteristics of trauma and posttraumatic stress disorder in a southwestern American Indian community. American Journal of Psychiatry. 1997;154(11):1582–1588. doi: 10.1176/ajp.154.11.1582. [DOI] [PubMed] [Google Scholar]
- Sahota PK, Knowler WC, Looker HC. Depression, diabetes, and glycemic control in an American Indian community. The Journal of clinical psychiatry. 2008;69(5):800–809. doi: 10.4088/jcp.v69n0513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sareen J, Cox BJ, Stein MB, Afifi TO, Fleet C, Asmundson GJ. Physical and mental comorbidity, disability, and suicidal behavior associated with posttraumatic stress disorder in a large community sample. Psychosomatic Medicine. 2007;69(3):242–248. doi: 10.1097/PSY.0b013e31803146d8. [DOI] [PubMed] [Google Scholar]
- Schnurr PP, Spiro A, Paris AH. Physician-diagnosed medical disorders in relation to PTSD symptoms in older military veterans. Health Psychol. 2000;19(1):91–97. doi: 10.1037//0278-6133.19.1.91. [DOI] [PubMed] [Google Scholar]
- Singh PK, Looker HC, Hanson RL, Krakoff J, Bennett PH, Knowler WC. Depression, diabetes, and glycemic control in Pima Indians. Diabetes Care. 2004;27(2):618–619. doi: 10.2337/diacare.27.2.618-a. [DOI] [PubMed] [Google Scholar]
- Spitzer C, Barnow S, Volzke H, Ulrich J, Freyberger HJ, Grabe HJ. Trauma, Posttraumatic Stress Disorder, and Physical Illness: Findings from the General Population. Psychosomatic Medicine. 2009;71(9):1012–1017. doi: 10.1097/PSY.0b013e3181bc76b5. [DOI] [PubMed] [Google Scholar]
- Sugarman JR, Grossman DC. Trauma among American Indians in an urban county. Public Health Reports. 1996;111(4):321. [PMC free article] [PubMed] [Google Scholar]
- Trief PM, Ouimette P, Wade M, Shanahan P, Weinstock RS. Post-traumatic stress disorder and diabetes: co-morbidity and outcomes in a male veterans sample. Journal of behavioral medicine. 2006;29(5):411–418. doi: 10.1007/s10865-006-9067-2. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. Mental Health: Culture, Race, and Ethnicity—A Supplement to Mental Health: A Report of the Surgeon General. Rockville, MD: U.S Department of Health and Human Services, Substance Abuse and Mental Health Services Administration Center for Mental Health Services; 2001. [Google Scholar]
- Walls ML, Whitbeck LB. Distress among Indigenous North Americans: Generalized and Culturally Relevant Stressors. Soc Mental Health. 2011;1(2):124–136. doi: 10.1177/2156869311414919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walls ML, Aronson BD, Soper GV, Johnson-Jennings MD. The Prevalence and Correlates of Mental and Emotional Health Among American Indian Adults With Type 2 Diabetes. The Diabetes Educator. 2014;40(3):319–328. doi: 10.1177/0145721714524282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warner CH, Warner CM, Appenzeller GN, Hoge CW. Identifying and managing posttraumatic stress disorder. American family physician. 2013;88(12):827–834. [PubMed] [Google Scholar]
- Weisberg RB, Bruce SE, Machan JT, Kessler RC, Culpepper L, Keller MB. Nonpsychiatric illness among primary care patients with trauma histories and posttraumatic stress disorder. Psychiatric Services. 2002;53(7):848–854. doi: 10.1176/appi.ps.53.7.848. [DOI] [PubMed] [Google Scholar]
- Whitbeck LB, Adams GW, Hoyt DR, Chen X. Conceptualizing and measuring historical trauma among American Indian people. Am J Community Psychol. 2004;33(3–4):119–130. doi: 10.1023/b:ajcp.0000027000.77357.31. [DOI] [PubMed] [Google Scholar]
- Whitbeck LB, Walls ML, Johnson KD, Morrisseau AD, McDougall CM. Depressed affect and historical loss among North American indigenous adolescents. American Indian and Alaska native mental health research. 2009;16(3):16–41. doi: 10.5820/aian.1603.2009.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolfe J, Schnurr PP, Brown PJ, Furey J. Posttraumatic stress disorder and war-zone exposure as correlates of perceived health in female Vietnam war veterans. J Consult Clin Psychol. 1994;62(6):1235–40. doi: 10.1037//0022-006x.62.6.1235. [DOI] [PubMed] [Google Scholar]
- Wu S, Wang R, Zhao Y, Ma X, Wu M, Yan X, He J. The relationship between self-rated health and objective health status: a population-based study. BMC public health. 2013;13(1):320. doi: 10.1186/1471-2458-13-320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zatzick DF, Marmar CR, Weiss DS, Browner WS, Metzler TJ, Golding JM, Wells KB. Posttraumatic Stress Disorder and Functioning and Quality of Life Outcomes in a Nationally Representative Sample of Male Vietnam Veterans. Am J Psychiatry. 1997;154:1690–1695. doi: 10.1176/ajp.154.12.1690. [DOI] [PubMed] [Google Scholar]


