Summary
Despite its high prevalence and burden, insomnia is often trivialized, under-diagnosed, and under-treated in practice. Little information is available on the subjective experience and perceived consequences of insomnia, help-seeking behaviors, and treatment preferences. The use of qualitative approaches (e.g., ethnography, phenomenology, grounded theory) may help gain a better understanding of this sleep disorder. The present paper summarizes the evidence derived from insomnia studies using a qualitative research methodology (e.g., focus group, semi-structured interviews). A systematic review of the literature was conducted using PsycINFO and Medline databases. The review yielded 22 studies and the quality of the methodology of each of them was evaluated systematically using the CASP appraisal tool. Selected articles possess at least a very good methodological rigor and they were categorized according to their main focus: “Experience of insomnia”, “Management of insomnia” and “Medicalization of insomnia”. The main findings indicate that: 1) insomnia is often experienced as a 24-hour problem and is perceived to affect several domains of life, 2) a sense of frustration and misunderstanding is very common among insomnia patients, which is possibly due to a mismatch between patients’ and health care professionals’ perspectives on insomnia and its treatment, 3) health care professionals pay more attention to sleep hygiene education and medication therapies and less to the patient’s subjective experience of insomnia, and 4) health care professionals are often unaware of non-pharmacological interventions other than sleep hygiene education. An important implication of these findings is the need to develop new clinical measures with a broader scope on insomnia and more targeted treatments that take into account the patient’s experience of insomnia. Greater use of qualitative approaches in future research may produce novel and more contextualized information leading to a more comprehensive understanding of insomnia.
Keywords: Insomnia, qualitative research, systematic review
Introduction
Insomnia is a widespread and debilitating condition that can affect anyone, including children [1], adults, and the elderly [2]. It is characterized by difficulties initiating and/or maintaining sleep, and is associated with significant distress or daytime impairments, despite adequate sleep opportunity. Clinical diagnosis is based on the presence of these subjective symptoms during at least three nights per week, for at least three months [3]. About one-third of adults in the general population report occasional sleep problems and 6% to 10% report symptoms that meet diagnostic criteria for insomnia disorder [4, 5]. Insomnia is more prevalent among women, middle-aged and older adults, and individuals with poor self-rated physical or psychological mental health [2]. In primary care settings, approximately 10% to 20% of individuals complain of significant insomnia symptoms with greater functional impairments and reduction in productivity, as well as increased health care utilization [6–8].
The burden of insomnia is high, producing significant adverse effects on the individual and on society [6, 9, 10]. Its consequences lie predominantly in the negative impact it has on daytime functioning with significant distress and/or impairments in the personal (e.g., fatigue), social (e.g., isolation), occupational (e.g., reduced attention), economic (e.g., absenteeism) and health (e.g., co-morbidity, depression, anxiety) domains [11], as well as on the quality of life [6, 8].
Despite its high prevalence, negative impact, and substantial direct and indirect costs [6, 9, 10], insomnia remains an under-recognized, under-diagnosed, and under-treated condition [12]. Differing perceptions of insomnia and its treatments between patients and clinicians may contribute to this paradox. Indeed, patients typically describe their insomnia in terms of its daytime impairments in everyday life, extending the experience beyond nighttime sleep difficulties. They usually perceive available insomnia treatments as ineffective or unattractive, they are prone to self-medicate, and tend to believe that insomnia will resolve spontaneously [4, 13–15]. Conversely, clinicians have a tendency to focus on standard diagnostic criteria rather than on the patient’s subjective experience of insomnia [16, 17] and usually perceive this problem as less of a priority and less urgent than other medical symptoms seen in their practice. They often report a lack of adequate knowledge and training in sleep interventions, and as a result, they manage insomnia mainly through basic sleep hygiene recommendations and hypnotic medication [16, 18].
The discrepancy between patients’ and clinicians’ perspectives concerning the significance and the emphasis given to the experience, assessment, and treatment of insomnia could be explained partially by the fact that several studies in this domain focus on the quantitative features of insomnia. Generally, the quantitative descriptors of the sleep disorder (e.g., severity and duration of insomnia) are favored while the qualitative descriptions of the nature or experience of insomnia and its interventions, as well as of the meaning of the patient-clinician relationship, are frequently put aside. Indeed, epidemiological, cross-sectional, and meta-analytic studies traditionally rely on diagnostic assessment of insomnia based on clinical interviews, validated surveys, or more objective measures, such as polysomnography [19]. Conversely, qualitative studies take into account the context and the experiences of the patient and the clinician, as well as the patient-clinician relationship and its variations over time from a more nuanced perspective.
To date, the majority of existing meta-analyses or literature reviews of insomnia have adopted a quantitative approach and have traditionally focused on randomized clinical trials of pharmacological or non-pharmacological interventions for insomnia [e.g., 20–22] and observational studies of clinical symptoms [e.g., 23] and impairments in daily life [e.g., 11]. To the best of our knowledge, there is only one narrative review that has focused on the insomnia patient’s perspective [18], yet 70% of the studies included in that review used a quantitative methodology.
Insufficient attention has been paid to the subjective experience of insomnia, and this accounts for a significant gap between patients and clinicians’ definitions, expectations, and beliefs about this sleep disorder. There is much less research exploring how patients experience insomnia in their daily lives and how clinicians manage insomnia in their clinical practice. There is even less research exploring how the multiple contexts related to insomnia (e.g., economic, physical, spiritual, emotional, social) contribute to shape patients’ and clinicians’ subjective experiences and their interactions. A more thorough understanding of the subjective experience of insomnia is therefore needed to narrow the gap between patients and clinicians.
Qualitative approaches may play a significant role in moving the field forward, as these approaches offer a more detailed and nuanced perspectives on human experience, and particularly on insomnia and its complexities, by generating novel, individualized, and more in-depth data. Qualitative research comprises different approaches (see Table 1) and has gained increasing recognition in various disciplines (e.g., anthropology, sociology, education, marketing, psychology, clinical medicine, and health services) since the early 1900s with a burgeoning of interest since the early 2000s [24–27].
Table 1.
Summary of the main qualitative research approaches
| Qualitative approaches | Aim(s) | Often applied in… |
|---|---|---|
| Ethnography | To describe and interpret a group with a shared culture | Anthropology and Sociology |
| Phenomenology | To describe how individuals experience a specific phenomenon | Philosophy and Psychology |
| Case study | To investigate a specific or multiple bounded system(s) | Social sciences |
| Grounded theory | To generate theory or an analytical schema grounded in data gathered in the field | Sociology |
| Participatory action research | To inquire equally all partners of a specific setting or environment for achieving social change | Health research |
Qualitative research is a form of scientific inquiry that, in contrast to quantitative research, focuses primarily on generating hypotheses. It is concerned with meaning rather than generalized statements. Open-ended discussions and observations (e.g., words, ideas, images) are used to explore individuals’ experiences and perspectives on complex phenomena or processes [26]. Data collection involves semi-structured interviews (i.e., in-depth discussion between researcher and participant, driven by participant), focus groups (i.e., guided discussions within a group of people who share a common characteristic or interest), audio-diaries (i.e., recording of personal perceptions of a given phenomenon in participants’ environments), participation (i.e., learning through exposure to or involvement in the day-to-day or routine activities of participants in natural settings), or observation (i.e., examination of people in natural settings) [24, 26]. The sample size varies according to the complexity of the phenomenon and is generally small, specific, and studied intensively in natural settings. Most of the time, adequacy of sample sizes in qualitative research is determined by achieving saturation, a point at which no new or relevant information or concepts can emerge from the data collection. [28]. Qualitative researchers are immersed in the study and use an inductive process to create patterns, categories, taxonomies, themes and theories to reduce and analyze detailed data [25]. Researchers’ biases and personal stances are identified (e.g., reflexive) and participants’ meanings of the phenomena are explicitly mentioned in the presentation of the results (e.g., verbatim) [27].
Qualitative research has contributed to the advancement of knowledge in different fields and topics by producing new types of data (e.g., verbatim recordings collected from social interactions), extracting detailed descriptions of individual perceptions and experiences, generating hypotheses concerning potential causal mechanisms, developing sound quantitative measurement processes or instruments, and improving methods for recruitment, retention and measurement of underrepresented populations in research [25]. Within the sleep research community, there is also increasing interest in and recognition of the capacity of qualitative approaches to improve our understanding of sleep disorders such as insomnia [18, 29]. However, to date, little is known about the experiences and perceptions of insomnia and its impacts on daytime functioning, help-seeking behaviors, and treatment preferences. Synthesizing the evidence derived from qualitative studies on insomnia may further our knowledge by helping to identify gaps and by generating new hypotheses grounded in the patients’ and clinicians’ subjective experiences. Therefore, the first aim of the present paper was to conduct a systematic review and synthesis of qualitative studies of insomnia, exploring and contrasting clinicians’ and patients’ perspectives. A secondary aim was to critically assess the utilisation of qualitative approaches in insomnia research, and to make recommendations for future studies.
Method
Search and identification of eligible articles
A systematic literature search was conducted by the first author (TA) between December 2013 and November 2015. Articles were retrieved in PsycINFO and Medline databases and imported into the EndNote® X6 citation management software. Duplicates were deleted. As it was expected that most of the relevant studies would have been conducted since the early 1990’s, the search was restricted to the period from January 1990 to November 2015. Key words used for this search included insomnia, chronic insomnia, sleep initiation, maintenance disorders, qualitative study, and qualitative research. To identify additional qualitative studies of insomnia, we also reviewed reference lists of relevant papers citing studies on insomnia patients/clinicians perspectives, insomnia patients’ help-seeking experiences or insomnia treatment experiences/preferences.
Selection of studies
The main inclusion criteria in this systematic review were: 1) the main focus of the study was insomnia, 2) the sample was composed of adults (≥ 18 years), 3) the methodology involved qualitative data collection (e.g., semi-structured interviews) and analysis (e.g., thematic analysis), and 4) the study was published in either English or French. Mixed methods studies (i.e., qualitative and quantitative data are collected, analyzed and combined to gather a more comprehensive understanding of complex phenomena), as well as reviews and commentaries were excluded.
Data extraction and organization of results
Information extracted from the studies as part of the systematic coding/rating included investigators and country where the study was conducted, descriptor of the main theme of the study, objectives, sample size and demographic attributes (age and gender), qualitative research methodology including data collection methods and data analysis techniques, main findings, and ratings of the quality of the research methodology (see Table 2).
Table 2.
Summary of qualitative studies on insomnia from the systematic review
| 1. EXPERIENCE OF INSOMNIA (n = 15) | |||||
|---|---|---|---|---|---|
| Author(s), Year, Ref. Number & Country | Study Objective(s) | Sample N, age (years), gender | Qualitative Research Methodology (data collection/data analysis) | CASP*/12 | Main Findings |
| Carey TJ et al 200548 USA |
Document patients’ experience of insomnia and develop scale that assesses changes in daytime and nocturnal experience | N = 16 Pa (Mage = 47.1; 50% female) | Focus groups Content analysis |
8 | Insomnia viewed as hidden disorder with daytime experiences emphasized more than nocturnal phenomena Impact of insomnia was pervasive and misunderstood by others (e.g., family members, friends, practitioners) |
| Cheung JMY et al 201341 Australia |
Document behavioral patterns and help-seeking experiences in patients with insomnia | N = 26 Pa (Mage = 42.6;range: 20–74; 61.5% female) | Semi-structured interviews Framework analysis |
8 | Three themes: patients’ sleep beliefs, treatment beliefs, and access to specialized care Daytime symptoms serve as cues for patients to seek medical help, few seek immediate medical help in early stages |
| Collier E et al 200349 UK |
Examine the experience of insomnia for psychiatric inpatients and provide practitioners data on interventions | N = 7 Pa (Mage = 33.5; range: 28–47; 42.85% female) | Semi-structured interviews Content analysis |
9 | Ten themes: control, holistic wants or desires, conflict, assessment, beliefs, sleep signatures communication, resignation, and individualism Sleep viewed as an isolated and silent problem |
| Davidson JR et al 200739 Canada |
Determine how to make non-pharmacologic insomnia treatments available to people with cancer | N = 26 Pa (Mage = 57.7, SD = 11.2; range: 44–79; 57.7% female) | Focus groups Semi-structured interviews Content analysis |
12 | Themes included: recognition and experience of sleep problem, need for information, importance of sleep, inclusion of insomnia assessment, reluctance to report, receiving help from others, no desire to use drugs |
| Dyas JV et al 201016 UK |
Explore patients’ and clinicians’ experiences of sleep difficulties | N = 30 Pa (range: 25–70; 63.3% female) N = 11 GP + 4 NP (53.3% female) |
Focus groups Constant comparative analysis |
9 | Patients describe insomnia in terms of impact on life; clinicians focus on underlying causes Clinicians need to elicit patients’ beliefs and expectations, and offer tailored treatments |
| Fleming L et al 201045 UK |
Conduct qualitative analysis of onset and impact of insomnia in cancer survivors | N = 21 Pa (Mage = 62; ≥18y; 66.7% female) | Focus groups Content analysis |
11 | Insomnia usually follows cancer diagnosis and is exacerbated by cancer treatment Early identification of insomnia in cancer care settings should be a priority |
| Green A et al 200817 UK |
Explore patients’ experience of insomnia Investigate what information patients want from health professionals |
N = 6 Pa (Mage = 50; range: 20–30; 100% female) | Focus groups Open questions/vignettes Content analysis |
9 | Participants reported major disruption in daytime activities, felt misunderstood by others, wanted evidence of efficacy on insomnia treatment, responsibility in managing problem within collaborative relationship with practitioner |
| Henry D et al 200842 USA |
Explore patients’ sociocultural aspects of insomnia in work place | N = 24 Pa (Mage = 53; range: 22–74; 79% female) | Semi-structured interviews Content analysis |
8 | Patients cite work as main catalyst in onset of insomnia, for needing “good” sleep, for seeking medical attention, and behavioral compliance with medication use |
| Henry D et al 201343 USA |
Explore patients’ beliefs about insomnia, course, symptom evaluation, response, and treatment expectation | N = 24 Pa (Mage = 55; range: 22–72; 79.2% female) | Semi-structured interviews Content analysis |
8 | Themes discussed include first response: delay seeking medical attention, help-seeking behavior, self-treatment Patient’s lack of awareness of treatment options was a major reason for medical consultation |
| Hsu HC et al 200946 Taiwan |
Generate descriptive theory framework on subjective experiences of sleep problems among perimenopausal women | N = 21 Pa (Mage = 51; range: 46–57; 100% female | Semi-structured interviews Constant comparative analysis |
10 | Key theme: “getting back a good night’s sleep”; process to recover quality sleep to reduce physical, psychological and social, health changes due to sleep problems |
| Kleinman L et al 201350 USA |
Explore patients’ experience of insomnia Generate a conceptual framework and endpoint model on insomnia and daytime consequences |
N = 28 Pa (Mage = 54.1; 57.1% female) | Focus groups Questionnaires (complementary data) Content analysis |
9 | Content analysis generated conceptual model (sleep and daytime impairments) and created an endpoint model for potential use in a clinical trial of a new or existing insomnia medication. Insomnia patients understand how amount and quality of sleep can affect activities and functions performed next day |
| Kyle SD et al 201040 UK |
Document patients’ daytime experience of insomnia and impact on quality of life | Focus group: N = 11 Pa (Mage = 38; range: 20–64; 81.9% female) Audio-diary: N = 8 Pa (sub-sample of 11; Mage = 36; range: 20–64; 75% female) |
Focus groups Audio-diaries Interpretative phenomenological analysis |
8 | Impact found for cognitive, emotional, and physical functioning, social life, work performance, and life aspirations Sleep disturbances limits overall quality of life |
| Moloney 200936 USA |
Explore patients’ experience with insomnia, interactions with practitioners, patient attitude toward insomnia treatment | N = 27 Pa (Mage = 50; range: 31–78; 62.9% female) | Semi-structured interviews Content analysis |
7 | Patients “normalize” insomnia by linking it to aging or hormonal changes, report positive practitioner interactions, and prefer pharmacological interventions Practitioner-patient interaction were based on consultation time, practitioners’ attitude toward treatment, consumerism, pre-existing prescription |
| Vigeta SMG et al 201251 Brazil |
Identify factors that influence perception of sleep quality in postmenopausal women | N = 22 Pa (Mage = 54.5; range: 46–60; 100% female) | Semi-structured interviews Discourse analysis |
9 | Sleep loss and being in menopause expressed as mood shifts and irritability Onset of sleep disorders may have occurred in childhood/stressful situations (not essentially linked with menopause) |
| Yung KP et al 201544 China |
Explore patients’ experience of chronic insomnia in a Chinese population | N = 43 Pa (Mage = 50.7; range: 26–66; 72% female) | Focus groups Insomnia experience diaries Constant comparative analysis |
11 | Four main themes and 16 subthemes show that patients’ sleep-related beliefs, behaviors, arousal, and emotions are in general compatible with qualitative studies results in the West. However, some areas related to insomnia are largely influenced by Chinese cultural beliefs and values (e.g., being modest in sleep expectation) Cultural adaptation should be incorporated in the assessment and treatment of insomnia, particularly in non-Western societies |
| 2. MANAGEMENT OF INSOMNIA (n = 5) | |||||
| Cheung JMY et al 201433 Australia |
Explore primary care health practitioners’ perspectives on the management of insomnia | N = 8 GP (50% female) N = 14 PH (36% female) (No information on age) |
Semi-structured interviews Framework analysis |
10 | Health practitioners initially addressed sleep complaint non-pharmacologically, but limited to sleep-hygiene advice Health practitioners exhibited a distinct pattern of zolpidem prescriptions since the media coverage on the adverse effects of zolpidem |
| Davy Z et al 201337 UK |
Explore primary care patients’ and health practitioners’ perceptions on the management of insomnia | N = 28 Pa (range: 20–70; 57.1% female) N = 23 HcP (9GP, 2NP, 5 PH, 7MHP). (65.2% female) (No information on age) |
Focus groups Semi-structured interviews Thematic analysis |
9 | Practitioners focus on sleep hygiene, treat cause rather than insomnia itself, and are ambivalent about hypnotics Patients and practitioners want more options and training for insomnia |
| Hislop J et al 200334 UK |
Explore medicalization and “healthicization” concepts for understanding the management of women’s sleep disruption (see note) | N = 82 Pa (> 40y; 100% female) N = 5 GP* (No information on age and gender) |
Focus groups Semi-structured interviews* Thematic analysis |
6 | Themes: restoration of balanced sleep patterns maintained through on-going use of personalized strategies and interaction between medicalization and personalization Provide an alternative model for the management of women’s sleep |
| Hubbling A et al 201447 USA |
Explore how mindfulness training is experienced by patients with chronic insomnia | N = 9 Pa (Mage = 47; range: 25–66; 89% female) | Focus groups Content analysis |
11 | Four themes: the impact of mindfulness on sleep and motivation to adopt a healthy sleep lifestyle, benefits of mindfulness on aspects of life beyond sleep, challenges and successes in adopting mindfulness-based practices and the importance of group sharing and support Practicing mindfulness and following sleep hygiene guidelines are useful in optimizing sleep benefits |
| Middlemass J et al 201235 UK |
Explore patients’ and practitioners’ perspective on role of social networking to develop a Computerized CBT-I program to increase access | N = 28 Pa N = 23 HcP (No information on age and gender) |
Focus groups Semi-structured interviews Thematic analysis |
9 | Themes: (1) trust (program, practitioner advocacy, patient-practitioner relation) and (2) functionality (accessibility, format, timing of program) Patient/practitioner views differed whether useful from less useful or potentially incorrect information could be distinguished |
| 3. MEDICALIZATION OF INSOMNIA (n = 2) | |||||
| Barter G et al 199638 UK |
Explore patients’ experiences and cognitions concerning long-term use of benzodiazepines | N = 11 Pa (range: 60–89; 90% female) N = 20 Co (range: 60–79; 60% female) |
Semi-structured interviews (Qualitative data analysis technique not specified) | 6 | Long-term users are highly heterogeneous group in patterns of use, in perceived efficacy of their tablets and in appraisal of doctor behavior in relation to their benzodiazepine use |
| Moloney 200936 USA |
Explore medicalization of insomnia and factors in patient-practitioner dyad that may fuel medicalization process | N = 8 PHY (Mage = 45; range: 32–63; 25% female) | Semi-structured interviews Content analysis |
7 | Patients’ individual/cultural norms influence perceptions of sleep and ideas of what is abnormal and treatable Patient-practitioner interactions influenced by: consumerism, physician compliance, insurance companies, authority, knowledge |
Quality appraisal of research methodology for qualitative studies: CASP score between 10 and 12 = “excellent”; between 7 and 9 = “very good”; between 4 and 6 = “good”; 3 and less = “poor”.
Pa: patients; Co: controls; Pr: practitioners; GP: general practitioners; PHY: Physicians; NP: Nurse prescribers; HcP: Health-care professionals; MHP: Mental Health professionals; PH: pharmacists
Note. “Healthicization” concept, according to the authors, is the link between personalization (personalized strategies) and medicalization in the patient help-seeking journey.
Information from the selected studies was summarized and conceptually organized by themes based on a thematic analysis process. The main findings were critically synthesized and interpreted in order to describe the diversity of experiences from the patients’ and the clinicians’ perspectives.
Assessment of the research methodology
The quality of the methodology of each article included in this review was evaluated with the qualitative research checklist of the Critical Appraisal Skills Programme (CASP – www.casp-uk.net). This appraisal tool was developed by the Public Health Resource Unit and designed to check research trustworthiness, results, and relevance, with scores ranging between “0” and “12”. A modified version, developed and previously used in qualitative systematic reviews [30–32] was used in the present review. The questionnaire included two screening questions (aims of the research and appropriateness of qualitative study methodology) and 10 specific questions that appraised the quality of the qualitative methodology (e.g., member check, reaching saturation, procedure for identification of research themes). Indeed, this modified version is deemed effective in appraising qualitative studies [33–35]. For the purposes of the present review, studies with a score between “10” and “12” are considered as presenting an “excellent” methodological quality rigor; a score between “7” and “9” as “very good”; a score between “4” and “6” as “good”; and a score of “3” and less as “poor”. Two of the authors (TA & DCJ) independently evaluated the quality of each article selected for this review. When discrepancies occurred between assessors, a discussion was initiated until a consensus was achieved.
Results
Flow of included studies
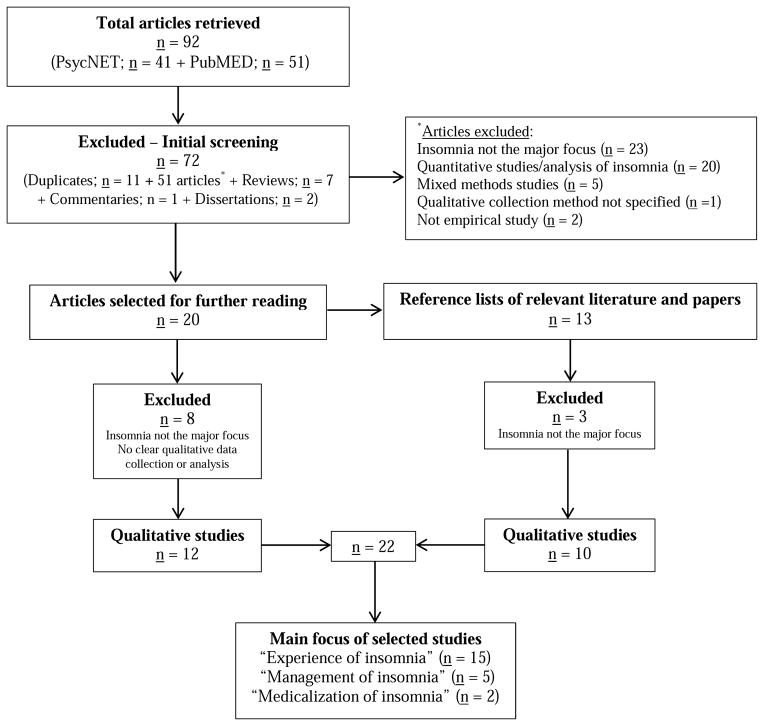
The flow chart of study selection for this systematic review is presented in Figure 1. A total of 92 articles were selected and duplicates (n = 11) were deleted. Initial screening based on the selection criteria and the content of the abstracts led to the exclusion of 51 articles, seven reviews, one commentary, and two dissertations for which insomnia was not the main focus of the study. The remaining 20 qualitative studies were read and a further eight articles were excluded. From the 12 studies retained, a dissertation with insomnia as main topic was included [36] and its two chapters were considered as two independent empirical studies. Thirteen additional qualitative studies were identified manually by reviewing reference lists of selected papers and other relevant literature. Ten articles met the selection criteria and were retained. The final sample was composed of 22 studies. To verify the accuracy of these selections, one of the co-authors (DCJ) reviewed five (22.73%) of the identified articles.
Fig. 1.
Flow chart of study selection
Quality of studies
Of the 22 studies retained in this review, four articles provided no or incomplete information on participants’ sociodemographic characteristics (age and gender) [33–35, 37] and one provided no information on data analyses [38]. Twenty studies focused on patients only, two studies focused on health care professionals1 only [33, 36], four studies included both patients and health care professionals [16, 34, 35, 37], and one study included healthy controls [38]. Data were collected mainly through semi-structured interviews (n = 14) and focus groups (n = 12). Four studies used both individual interviews and focus groups [34, 35, 37, 39]. Audio-diaries were used in one study [40]. Content analysis was the most commonly used technique for data analysis (see Table 3). Of the total sample of 22 articles, 11 studies [16, 33–37, 41–44] used qualitative research software for coding and analysis: QSR NVivo (n = 8), ATLAS.ti (n = 2) and MAXqda (n = 1).
Table 3.
Summary of qualitative research techniques used to analyse data
| Qualitative data analysis techniques | Description | N ( /22) |
|---|---|---|
| Content analysis | Analysis of manifest and latent content of subjective experiences, images, documents | 11 |
| Thematic analysis | Narrative analysis of a story or an experience | 3 |
| Constant comparative analysis | Comparative and contrasting analysis of incidents or subjective experiences | 3 |
| Framework analysis | Analysis of a specific questions and a priori issues in a defined group | 2 |
| Discourse analysis | Linguistic analysis of ongoing flow of communication | 1 |
| Interpretative phenomenological analysis | Analysis of detailed and in-depth understanding of personal lived experiences | 1 |
| Studies without qualitative data analysis techniques specified | 1 |
Of the 22 studies, six were rated as “excellent” for their methodological quality according to the CASP criteria [33, 39, 44–47], 14 studies were rated as “very good” [16, 17, 35–37, 40–43, 48–51], two were rated as “good” [34, 38], and none was ranked as “poor”. In general, studies retained for this review presented several strengths according to qualitative methodology standards. First, all the articles clearly stated their research objectives, used recognized qualitative methodology, included information on predefined questions that were part of the interviews, indicated that the data were audio-taped and transcribed verbatim, and presented samples of the original data (e.g., quotations). Second, all articles but one [38] included clear information on how the research themes were identified, and all articles but one [34] reported that ethical review or ethical waivers were obtained. Third, 17 of the 22 articles reported that the data were coded/analyzed by more than one assessor [16, 17, 33, 35, 37, 39, 40, 42–51].
Studies selected also presented some limitations in their methodology and presentation of findings. For instance, several studies did not report if saturation was achieved when analyzing the data [17, 34, 36, 38, 40, 42, 43, 48–50], if participants’ answers were reviewed for clarification (i.e., member check) [16, 34–36, 38, 41–44, 48, 50,51], if the facilitator received training or had experience in leading individual interviews or focus groups [16, 17, 33–38, 40–43, 46, 48, 49, 51], and if piloting for individual interviews, focus groups, audio-diaries, or other pretests was conducted [16, 17, 33–38, 40–43, 45–51].
Description of selected qualitative studies
The majority of qualitative studies selected for this review were conducted since the early 2000s and most were done in the United Kingdom (n = 9), followed by the United States of America (n = 7), Australia (n = 2), and one investigation each was conducted in Brazil, Canada, China and Taiwan. Data also show that these four studies were published in English but originally conducted in another language. None of selected studies were published in French. Six studies were published in Behavioral Sleep Medicine, a journal specifically devoted to sleep, whereas other studies were published in journals with a focus on primary health care (n = 5), health care and health policy (n = 3), sociology of health, illness and health care (n = 3), nursing (n = 2), university press (n = 2), and occupational therapy (n =1).
Main themes
Three themes emerged from the analysis of the selected papers: “Experience of insomnia”, “Management of insomnia”, and “Medicalization of insomnia”. Fifteen studies focused on patients’ experiences of insomnia symptoms, daytime consequences and available insomnia treatments, five focused on how patients and health care professionals manage insomnia symptoms, and two explored how patients experienced the medicalization of insomnia.
Experience of insomnia
This first theme explored the patients’ subjective experience of insomnia in a wide range of contexts, such as insomnia and daytime consequences, quality of life, help-seeking behaviors, patients’ beliefs about sleep, insomnia treatment, patient and health care professional interactions, insomnia and cancer, insomnia and menopause. One study [16] also considered the perspective of health care professionals on the experience of sleep difficulties.
Most studies found that the experience of insomnia is heterogeneous and has a pervasive impact on quality of life that is perceived to extend well beyond nighttime difficulties, encompassing many domains of daytime functioning. For example, Henry and colleagues [42] interviewed 24 participants about the sociocultural aspects of insomnia in the work place. Using content analysis of data derived from semi-structured interviews, they found that insomnia was viewed as “an impediment to occupational success” (p. 724). Similarly, in another study [40] using focus groups and audio-diaries, Kyle and colleagues found that insomnia was perceived as a barrier to the desired self. Insomnia was also viewed as a stigmatized, silent and hidden problem [40, 46, 48, 49], despite causing significant personal and social deficits in daily life [40, 44]. Different studies [16, 17, 40, 44, 48] revealed that patients usually felt misunderstood by others (e.g., family, friends, and practitioners), which produced feelings of frustration and views of being an “outsider” with respect to “normal” society [40, 43].
Studies exploring patients’ beliefs about insomnia and help-seeking experiences demonstrated that social stigma related to experiencing sleep problems could lead to a significant delay in patients’ self-diagnosis and help-seeking behaviors [41, 43, 44]. People suffering from insomnia may experience a sense of resignation and hopelessness about insomnia and its treatment (e.g., can never be successfully treated) [40, 44]. Conversely, some may tend to “normalize” insomnia (e.g., attribute it to the aging process, hormonal changes or mood disorders, cultural beliefs and values) [36, 44] which, in turn, may prevent help-seeking behaviors in early stages of the sleep disorder. Using focus groups and insomnia experience diaries, Yung and colleagues [44] interviewed 43 participants in a Chinese population and demonstrated that cultural and social values (e.g. modesty in Chinese society) can influence participants’ sleep expectations and behaviors (e.g., being realistic and humble regarding sleep outcomes and adopting a letting-go attitude).
Another issue pertaining to the experience of insomnia concerns the patients’ perception that health care professionals have inadequate training in recognizing and treating sleep disorders, as well as the divergent perceptions of insomnia and its management between patients and clinicians [16, 41]. The latter issue refers to the fact that the presentation, beliefs, expectations, and management of insomnia have been shown to be quite different between patients and clinicians [16]. Patients tend to focus on daytime impairments and self-medication, while clinicians tend to focus on descriptors of the insomnia, which may contribute to a feeling of being misunderstood and a decreased motivation to seek treatment. However, both patients and health care professionals emphasize that these differing points of view on insomnia should be seen as complementary and taken into account in a holistic way to improve recognition of insomnia and treatment tailoring. Some authors [16, 41, 49] also emphasized the need for educational support for the dyad patient-health care professional (e.g., better assessments of sleep disorders, patient information, treatment choices) to improve individualized management of insomnia. Only one study [44] emphasized the need for cultural adaptation in the assessment and treatment of insomnia (e.g., adoption of culture-specific therapies), particularly in non-Western societies.
Most studies in this first theme were rated as presenting at least a “very good” methodological rigor, which ensured their validity. However, given that these studies did not report achieving saturation and/or member check, other new findings may still emerge from this theme and contribute to a broader understanding of how patients and health care professionals experience insomnia.
Management of insomnia
The second theme identified in this review was concerned with insomnia management, and explored two sub-domains including strategies used to manage insomnia and patients’ and/or health care professionals’ perceptions (e.g., attitudes, expectations, beliefs) of current therapies. In the first sub-domain, Hislop and colleagues [34] described medicalization and “healthicization” (see note on Table 2) concepts to better understand the management of women’s insomnia. The findings showed that the application of a medicalization-healthicization framework did not lead to a complete understanding of how women manage sleep disruption within the social context of their lives (e.g., role of working woman, partner, mother, etc.). Those authors proposed an alternative model for the management of women’s sleep incorporating personalized strategies embedded in women’s daily routines (e.g., taking hot baths, relocating to other rooms or beds). Hubbling and colleagues [47], using focus groups, explored how an 8-week mindfulness-based stress reduction program was experienced by patients with chronic insomnia. They showed that mindfulness training in a group format, combined with sleep hygiene guidelines, is useful in optimizing sleep benefits (e.g., sleeping better, waking more refreshed) and is effective in insomnia treatment.
The second sub-domain involved patients’ and/or practitioners’ perceptions of insomnia management. Studies found divergent perspectives on insomnia treatments between patients and health care professionals. Davy and colleagues [37] showed that health care professionals often took patients’ socio-economic status into consideration to guide their intervention, and focused on treating the underlying cause of insomnia (e.g., physical, psychological) rather than insomnia per se. The fact that the sleep disorder was not prioritized in office visits generated a feeling of frustration among patients, even though they understood that their insomnia could have multiple causes. Those same authors also indicated that patients perceived health care professionals’ stepped care approach (i.e., assessment, sleep hygiene advice and drug prescription) to be too simplistic and even dismissive given the complexity of their insomnia. This difference of perspectives concerning insomnia treatments tended to create a tension in the health care professional-patient relationship. Furthermore, Cheung and colleagues [33] suggest that insomnia is usually perceived as a less urgent matter by health care professionals. Indeed, they reported that these professionals rarely referred patients with insomnia to sleep clinics (e.g., “I haven’t referred unless again there is something suspicious…” – p. G) and instead managed insomnia with a predominant focus on sleep hygiene or, more frequently, by pharmacotherapy [33]. The issue of prescribing medication was related to the fact that health care professionals perceived sleep hygiene as ineffective or insufficient for managing insomnia, despite their advocating or advising this to their patients [33, 37]. Also, health care professionals were ambivalent about hypnotic drugs (i.e., they prescribe it to avoid confrontation or to show empathy with patients) and reported a lack of knowledge, confidence, or adequate support in providing psychological therapies, such as Cognitive Behavioral Therapy for Insomnia (CBT-I) [33, 37]. Lastly, professionals perceived their patients as over-using medications and being reluctant to engage in non-pharmacological treatments [33].
Several inconsistencies emerged between practitioners and patients. For instance, health care professionals often perceive patients to be reluctant to engage in non-pharmacological therapies, whereas other findings suggest that patients prefer non-pharmacological therapies over drug treatment. Health care professionals also perceived some pressure from their patients to obtain a prescription drug during the office visits [33]. Surprisingly, Davy and colleagues [37] showed that insomnia patients seeking help at a pharmacy were often satisfied to receive sleep hygiene advice, rather than an over-the-counter remedy. However, health care professionals perceived their patients to use drugs incorrectly when they self-medicate (e.g., combine prescribed hypnotics with over-the-counter medication). Despite over-reliance on hypnotic prescriptions in the management of insomnia, health care professionals were aware of their potential risks (e.g., dependence, tolerance) and reported preferences for short-term treatments whenever possible [33, 37]. Relatedly, patients were sometimes, but not always, concerned about addiction and withdrawal [37].
Additionally in this second sub-domain, patients’ and health care professionals’ perspectives on previous experiences with online health care programs were investigated [35]. Middlemass and colleagues found that “trust” and “functionality” were perceived as important factors to improve uptake and adherence to Computerized CBT-I. “Trust”, for both patients and health care professionals, was related to accreditation of online health care programs (e.g., evidence of effectiveness, patient-practitioner relationship, professional and online peer support). “Functionality” referred to the functions that may improve program’s usability and usefulness for patients (e.g., mobile applications, self-assessment, interactive/personalized information on sleep). The authors further posited that better patient control and interaction with other users and professionals, as well as more online access and computer literacy, may enable greater and more positive experiences of online therapy in insomnia management.
Most studies in this second theme were rated as presenting at least a “very good” methodological rigor and only a few limits concerning conducting pretests, training of facilitators and member check. Four out of five studies achieved saturation [33, 35, 37, 47], ensuring they reliably explored issues related to this second theme. Additionally, they highlight the need for a better understanding of the advantages and limitations of current approaches in the management of insomnia, in particular non-pharmacological therapies, and the need to disseminate up-to-date information about insomnia therapies and educational resources both to patients and health care professionals.
Medicalization of insomnia
The third theme identified by this review concerned patients’ (mainly older adults) and/or health care professionals’ experiences (e.g., behaviors, cognitions) with respect to the medicalization of insomnia. Two studies examined this issue. Moloney [36] found that health care professionals (e.g. clinicians) use sociological language to describe insomnia (e.g., “medicalize”, “disease”) and are cognizant and critical of medicalization. Health care professionals were highly aware of factors that promote the medicalization of insomnia [i.e., “the expansion of a disease category”, “the influence of advertisements” (p.89)], yet they routinely prescribed sleep medications despite their expressed preferences for non-pharmacological solutions when feasible. Moloney [36] also identified sociocultural factors such as consumerism (e.g., patients’ request of specific drugs), time constraints (e.g., limited-time in office visit) and pre-existing prescription (e.g., patients’ expectation of refill) that influenced the patient-clinician relationship and fueled the medicalization of insomnia. Specifically, it is suggested that these sociocultural factors impact a physician’s receptivity to a patient’s input concerning their insomnia diagnosis and treatment plan.
The other study on this theme explored patients’ and health care professionals’ perceptions of on the use of prescribed sleep medications [38]. According to this study, patients’ perceptions are often influenced by the degree of interactions they have with their prescribing health care professional. Automatic prescription renewals without direct interaction between patients and professionals is perceived to limit opportunities to improve patients’ knowledge about medication. Conversely, some patients are very compliant with physicians’ prescriptions and do not question their practices (e.g., “I don’t stop unless the doctor says”, “[The doctor]… only allows me 30 of them at a time…” – p. 495). This study [38] also found that most of the elderly patients interviewed use prescribed sleep medications (especially benzodiazepine hypnotic) for protracted lengths of time (e.g., ≥ 10 years), and that withdrawal symptoms (e.g., rebound insomnia) usually fueled the patients’ continual use. Additionally, authors reported that long-term hypnotic users are a heterogeneous group based on their: (1) patterns of use (e.g., reasons for first use), (2) perceived risks and benefits (e.g., worries of long-term use of benzodiazepine), and (3) beliefs about withdrawal (e.g., advantages and disadvantages of stopping sleep aids). These findings highlight the need for clearer information about sleep medication in the patient-health care professional dyad, particularly concerning the (dis)continuation process.
Studies in this third theme were rated as presenting at least a “good” methodological rigor. Achieving saturation and/or member check were not reported by authors, which suggests that further investigation in insomnia management could lead to new findings in the patient-health care professional dyad.
Discussion
The aim of the present systematic review was to summarize the current evidence on insomnia, as experienced by patients and clinicians, based on qualitative studies, and to show how qualitative approaches are used in insomnia research. Following stringent criteria, 22 studies were identified, most of them were rated as having at least a “very good” rigorous methodology. Three themes emerged as primary foci of these studies (“Experience of insomnia”, “Management of insomnia”, and “Medicalization of insomnia”). The complexity of relevant issues, such as experience of insomnia or the use of non-drug interventions was addressed with a predominant focus on the patient’s perspective. When researchers were interested in insomnia management or medicalization of insomnia, health care professionals’ views were also examined.
Contexts of publication
This systematic review highlights an increasing interest over the last decade in qualitative investigations of insomnia, particularly in exploring the subjective experience of insomnia and its treatment options. Along with this increasing interest in qualitative studies of insomnia, qualitative research has also been gaining increasing recognition in various disciplines. The keyword “qualitative research” appeared for the first time in Medline database in 2003, the same year that publication of qualitative studies on insomnia started to be more present in sleep medicine field. However, the total number of studies using a qualitative approach in insomnia is still low compared to other health care research topics, such as depression or patient-physician communication.
Although definitions of qualitative and quantitative research are widely present in the literature, this has not ensured a standardized database classification of studies. The present systematic review found several articles identified by the authors as “qualitative research”, yet they used quantitative research methods. For example, despite the presence of descriptive or interpretative data in the identified “qualitative studies”, the qualitative content was not analyzed in detail in order to take into account the multiple contexts that constitute the studied phenomenon. Likewise no specification of clear qualitative data collection or analysis, and methodological references were stated. Instead, statistical analyses (i.e., chi-square, McNemar test, f) were carried out, and a quantification of qualitative data was performed.
A majority of the research was published in health journals or in specialized qualitative journals. Studies performed in other languages suggest that qualitative studies might be published in other languages than English as well. Overall, the context of publication might be interpreted as the result of a dominant biomedical positivist paradigm in insomnia research and more broadly in sleep research [52]. This dominance might imply that sleep researchers may not be aware of the recent development, rigor, relevancy and advantages of qualitative approaches.
Contexts of methodology
The majority of the studies retained in the present review were rated as having at least a “very good” scientific rigor. Semi-structured interviews and focus groups were the most common tools used to gather data, being used in a range of different types of qualitative approaches, but particularly in ethnographical and phenomenological studies. These methodologies provided a variety of data with their own particularities. For example, interviews gathered individual responses and more introspective data, whereas focus groups were used to gather collective responses and to elicit a range of diverse feelings and experiences regarding a specific topic. These two methods have been shown to be complementary [43] and have proved effective for producing novel and contextualized data by individualized, detailed and in-depth interviewee’s descriptions of insomnia [37, 40, 48]. While audio-diaries also have the strength of capturing rich qualitative data in the participant’s own environment, they were used in only one study [40]. In terms of data coding and analysis, content analysis was the technique most often used. This technique provides insights into the meaning and patterns of human thoughts, language and behaviors, and both qualitative (i.e., taxonomies, themes and theories) and quantitative data can emerge from its text analysis process. Content analysis is valued by researchers especially for its closeness to the data, yet it is a time-consuming technique. While qualitative data analysis software are recognize for coding and analyzing data more properly and faster, they were used only in half of studies. QRS NVivo was the preferred one.
Most of the information essential to evaluate the methodological rigor of a qualitative study was reported in the studies selected for this review. Information most commonly missing was about methodological features such as saturation of data, reviewing participants’ answers for clarification, conducting pretests, or training of facilitators. The CASP used in this systematic review is an exhaustive tool in appraising qualitative studies. However, all the criteria assessed by this appraisal tool do not necessarily have to be systematically used in each qualitative study, since they need to be balanced according to the theoretical framework of a specific research. Therefore, a qualitative study could be methodologically valid without presenting all the CAPS criteria. In the present review, the missing information suggests that new data may emerge from further qualitative investigations of insomnia and its complexities.
Contexts of emerging themes
The review underlines the seriousness of insomnia, which is perceived and experienced as a debilitating condition with detrimental consequences for the patients’ everyday life [40, 42, 44, 48]. The findings clearly illustrate subtleties in the perceived daily consequences of insomnia. The review also highlights the mismatch between patients’ and health care professionals’ point of views on the experience of insomnia, as well as the complexity and extent of the phenomenon. Studies reviewed here made it clear that the mismatch led to a sense of frustration, conflict, and misunderstanding in patients. From the patient’s point of view, insomnia is a 24-hour burden that affects every part of their lives. Patients tend to focus on the symptoms and consequences of insomnia and want help in relieving the symptoms, often expressing their interest in treatment options other than drugs. They also tend to feel stigmatized and guilty not to be able to fill their socially productive role completely. Conversely, for health care professionals, greater importance is placed on examining the root cause of insomnia. Less attention is placed on the subjective experience of insomnia and more emphasis is focused on medicating the patient. As such, providing support, education, and information about behavioral strategies is vital for improving patient-health care professional interaction [33, 37]. There is an increasing emphasis placed on decision-sharing in the management of various medical conditions, and insomnia is certainly a health problem that could be managed more efficiently by using a patient/health care professional decision sharing process. This issue is closely related to the fact that health care professionals often lack adequate training to manage sleep problems [16]. There is also a general misunderstanding of non-pharmacological interventions with knowledge often limited to a few basic sleep hygiene education principles; and many do not necessarily understand the specificities of psychological therapies such as CBT-I. More systematic training in recognition and management of insomnia (both CBT and medication) would likely make health care professionals more attentive to insomnia complaints and more confident in their own skills to initiate treatment other than sleep medications [16, 17, 41].
Limitations
This review had a number of methodological limitations. The first and the most important, is that only a few studies presented information about the specific steps involved in the methodological analysis [e.g., 41, 42] and procedures concerning theoretical saturation: this information is necessary for ensuring the rigor and the validity of findings [e.g., 17, 18, 33]. The second limitation pertains to the fact that some studies failed to report sociodemographic information [e.g., 33, 35, 37], which may prevent accurate description of the entire sample of this systematic review and precludes adequate transferability of the findings to other contexts.
Implications for research and practice
This review has important implications for research and practice. Openness to qualitative studies in insomnia may offer unique opportunities to contribute to the empirical literature on key aspects of insomnia outcomes, such as effectiveness, efficiency, timeliness, and patient-centeredness. It has been shown that qualitative research can “broaden the scope of evidence based medicine” (p. 1230) [53]. Studies, such as the ones we selected for this review, need to be rigorous, grounded with clear objectives and a well-defined qualitative approach. Several key procedures also need to be conducted and named in the publication; this might imply more space than usual for a paper (5000 words or more). The concept of saturation, the use of inter-rater reliability, or the use of any other assessment technics needs to be identified in the publication. All these recommendations and others on how to publish qualitative research (in medical journals) have been extensively presented in a diversity of publications, including method handbooks, in the last decades [e.g., 54]. However, qualitative research is still underrepresented in such journals [55]. This is unfortunate, as qualitative methods may help move the sleep research field forward.
Much more diverse and creative methods could be used in insomnia research to investigate perceptions and actions that will contribute to understanding insomnia in a more holistic way. Individual and focus group interviews, which we found to be almost the only methods used, allow the exploration of perceptions. However, these standard qualitative research methods fail to adequately assess actions. Therefore, new themes that can more globally assess the patient’s context, such as the trajectory of care and the human environment, need to be investigated through more diversified qualitative approaches. For instance, observations of insomnia consultations could be planned to capture the structure and the presence (or absence) of a co-construction of meaning between the health care professional and the patient; family or couple interviews would allow understanding of the meaning of insomnia for all family members, as was done by Araújo [56]. Further studies could explore how insomnia is experienced by the patient’s partner, family or colleagues in their own environment, and as such take into account the sociocultural context, as in the Yung and colleagues study [44]. Such creative methods could be helpful to: 1) gain a more comprehensive understanding of a wide range of relevant issues including, but not limited to the subjective experience of insomnia, help-seeking behaviors, diagnosis, and treatment options from the patients’, health care professionals’ views and/or the patient’s related (e.g. translation of evidence-based practices in primary care), 2) develop new assessment instruments grounded in the interviewee’s descriptions of the phenomena (e.g., patient reported outcomes and community programs of intervention), 3) design more effective non-pharmacological interventions (e.g., CBT-I) that take into account the contextual experience of insomnia, and 4) refine treatment modalities according to patients’ needs and practical health care professionals experiences (e.g., implementation of guidelines for improving timeliness of insomnia assessment in primary care).
Clinical practice may benefit from these issues by relevant dissemination of qualitative research outcomes and of updated insomnia information to the public. Additionally, insights from qualitative studies could be incorporated and gathered into educational resources for both patients and health care professionals. This could improve management of insomnia in the primary care system, an entry point for at least 10% to 20% of patients who complain of important insomnia symptoms [7].
In summary, this review highlights the importance of qualitative approaches in the behavioral sleep medicine field and more specifically for insomnia disorder. Indeed, there has been a surge of insomnia studies since the 2000s using qualitative methodologies. Giving more attention to qualitative approaches in future studies might offer a more comprehensive understanding of insomnia and its complexities.
Practice Points.
Clinical evaluation of insomnia should incorporate qualitative assessment of issues relevant to the patient’s subjective experience of insomnia, help-seeking behaviors, and perceptions of treatment options.
Treatment planning should take into account these patient’s perceptions and prior experiences and tailor insomnia interventions accordingly.
In order to improve communication between patient and health care professionals and, possibly, treatment outcome, training of health care professionals should include information about the patients’ perception of insomnia and their treatment expectations as these may differ significantly from their own perceptions and expectations.
Research Agenda.
Incorporate additional qualitative methods (e.g., family or couple interviews) to those currently employed (i.e., individual and focus group interviews) in future studies of insomnia. The use of more diversified approaches that respect accepted standards of qualitative methodology (e.g., saturation, in-depth description of results, inter-rater reliability) are needed to achieve a more comprehensive understanding of insomnia.
Develop new assessment instruments grounded in the patient’s subjective and cultural experience of insomnia in order to improve individualized management of insomnia.
Explore the patient-health care professional interactions in different clinical settings and sociocultural contexts through more diverse and creative qualitative research (e.g., observations of patients-health care professionals interactions during insomnia consultations).
Acknowledgments
This study was supported by National Institute of Mental Health (Grant #MH091053), and the Canadian Institutes of Health Research (Grant #MOP42504) to Charles Morin, and by the Canadian Institutes of Health Research Fellowship (Grant #BO512201) awarded to Denise C. Jarrin.
Abbreviations
- CBT-I
cognitive behavioral therapy for insomnia
- CASP
critical appraisal skills programme
Footnotes
In the present review, health care professionals will encompass practitioners, general practitioners, physicians, nurse prescribers, mental health professionals and pharmacists. In Table 2, this information is detailed according to selected studies.
Disclosure: C. Morin has served on advisory boards for Merck, Novartis, and Valeant. The other authors report no conflict of interest associated with the material presented in this review.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Sheldon SH. Insomnia in Children. Curr Treat Options Neurol. 2001;3:37–50. doi: 10.1007/s11940-001-0022-9. [DOI] [PubMed] [Google Scholar]
- 2.Morin CM, LeBlanc M, Belanger L, Ivers H, Merette C, Savard J. Prevalence of insomnia and its treatment in Canada. Can J Psychiatry. 2011;56:540–8. doi: 10.1177/070674371105600905. [DOI] [PubMed] [Google Scholar]
- 3.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5) 5. Washington, DC: American Psychiatric Publishing; 2013. [Google Scholar]
- 4.Morin CM, LeBlanc M, Daley M, Gregoire JP, Merette C. Epidemiology of insomnia: prevalence, self-help treatments, consultations, and determinants of help-seeking behaviors. Sleep Med. 2006;7:123–30. doi: 10.1016/j.sleep.2005.08.008. [DOI] [PubMed] [Google Scholar]
- 5.Roth T, Jaeger S, Jin R, Kalsekar A, Stang PE, Kessler RC. Sleep problems, comorbid mental disorders, and role functioning in the national comorbidity survey replication. Biol Psychiatry. 2006;60:1364–71. doi: 10.1016/j.biopsych.2006.05.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rosekind MR, Gregory KB. Insomnia risks and costs: health, safety, and quality of life. Am J Manag Care. 2010;16:617–26. [PubMed] [Google Scholar]
- 7.Aikens JE, Rouse ME. Help-seeking for insomnia among adult patients in primary care. J Am Board Fam Pract. 2005;18:257–61. doi: 10.3122/jabfm.18.4.257. [DOI] [PubMed] [Google Scholar]
- 8.Simon GE, VonKorff M. Prevalence, burden, and treatment of insomnia in primary care. Am J Psychiatry. 1997;154:1417–23. doi: 10.1176/ajp.154.10.1417. [DOI] [PubMed] [Google Scholar]
- 9.Daley M, Morin CM, LeBlanc M, Gregoire JP, Savard J. The economic burden of insomnia: direct and indirect costs for individuals with insomnia syndrome, insomnia symptoms, and good sleepers. Sleep. 2009;32:55–64. [PMC free article] [PubMed] [Google Scholar]
- 10.Ozminkowski RJ, Wang S, Walsh JK. The direct and indirect costs of untreated insomnia in adults in the United States. Sleep. 2007;30:263–73. doi: 10.1093/sleep/30.3.263. [DOI] [PubMed] [Google Scholar]
- 11.Fortier-Brochu E, Beaulieu-Bonneau S, Ivers H, Morin CM. Insomnia and daytime cognitive performance: a meta-analysis. Sleep Med Rev. 2012;16:83–94. doi: 10.1016/j.smrv.2011.03.008. [DOI] [PubMed] [Google Scholar]
- 12.Leger D, Poursain B. An international survey of insomnia: under-recognition and under-treatment of a polysymptomatic condition. Curr Med Res Opin. 2005;21:1785–92. doi: 10.1185/030079905X65637. [DOI] [PubMed] [Google Scholar]
- 13.Bartlett DJ, Marshall NS, Williams A, Grunstein RR. Predictors of primary medical care consultation for sleep disorders. Sleep Med. 2008;9:857–64. doi: 10.1016/j.sleep.2007.09.002. [DOI] [PubMed] [Google Scholar]
- 14.Harvey AG, Stinson K, Whitaker KL, Moskovitz D, Virk H. The subjective meaning of sleep quality: a comparison of individuals with and without insomnia. Sleep. 2008;31:383–93. doi: 10.1093/sleep/31.3.383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stinson K, Tang NK, Harvey AG. Barriers to treatment seeking in primary insomnia in the United Kingdom: a cross-sectional perspective. Sleep. 2006;9:1643–6. doi: 10.1093/sleep/29.12.1643. [DOI] [PubMed] [Google Scholar]
- *16.Dyas JV, Apekey TA, Tilling M, Orner R, Middleton H, Siriwardena AN. Patients’ and clinicians’ experiences of consultations in primary care for sleep problems and insomnia: a focus group study. Br J Gen Pract. 2010;60:e180–200. doi: 10.3399/bjgp10X484183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *17.Green A, Hicks J, Wilson S. The experience of poor sleep and its consequences: A qualitative study involving people referred for cognitive-behavioural management of chronic insomnia. Brit J Occup Ther. 2008;71:196–204. [Google Scholar]
- *18.Cheung JM, Bartlett DJ, Armour CL, Saini B. The insomnia patient perspective, a narrative review. Behav Sleep Med. 2013;11:369–89. doi: 10.1080/15402002.2012.694382. [DOI] [PubMed] [Google Scholar]
- 19.Smith MT, Wegener ST. Measures of sleep: The Insomnia Severity Index, Medical Outcomes Study (MOS) Sleep Scale, Pittsburgh Sleep Diary (PSD), and Pittsburgh Sleep Quality Index (PSQI) Arthritis Care Res. 2003;49:S184–S196. [Google Scholar]
- 20.Morin CM, Culbert JP, Schwartz SM. Nonpharmacological interventions for insomnia: a meta-analysis of treatment efficacy. Am J Psychiatry. 1994;151:1172–80. doi: 10.1176/ajp.151.8.1172. [DOI] [PubMed] [Google Scholar]
- 21.Holbrook AM, Crowther R, Lotter A, Cheng C, King D. Meta-analysis of benzodiazepine use in the treatment of insomnia. CMAJ. 2000;162:225–33. [PMC free article] [PubMed] [Google Scholar]
- 22.Sok SR, Erlen JA, Kim KB. Effects of acupuncture therapy on insomnia. J Adv Nurs. 2003;44:375–84. doi: 10.1046/j.0309-2402.2003.02816.x. [DOI] [PubMed] [Google Scholar]
- 23.Vernon MK, Dugar A, Revicki D, Treglia M, Buysse D. Measurement of non-restorative sleep in insomnia: A review of the literature. Sleep Med Rev. 2010;14:205–12. doi: 10.1016/j.smrv.2009.10.002. [DOI] [PubMed] [Google Scholar]
- 24.Denzin NK, Lincoln YS. Handbook of Qualitative Research. Thousand Oaks, California: SAGE Publications; 2011. [Google Scholar]
- 25.Curry LA, Nembhard IM, Bradley EH. Qualitative and mixed methods provide unique contributions to outcomes research. Circulation. 2009;119:1442–52. doi: 10.1161/CIRCULATIONAHA.107.742775. [DOI] [PubMed] [Google Scholar]
- 26.Creswell JW, Clark VLP. Designing and Conducting Mixed Methods Research. SAGE Publications; 2007. [Google Scholar]
- 27.Creswell JW. Research Design: Qualitative, Quantitative, and Mixed Methods Approaches. 4. SAGE Publications; 2014. [Google Scholar]
- 28.Morse JM, Field P-A. Nursing research: The application of qualitative approaches. Nelson Thornes; 1995. [Google Scholar]
- 29.Arber S, Meadows R, Veen S. Sleep and Society. In: Morin CM, Espie CA, editors. The Oxford Handbook of Sleep and Sleep Disorders. New York: Oxford University Press; 2012. pp. 223–247. [Google Scholar]
- 30.Mills E, Jadad AR, Ross C, Wilson K. Systematic review of qualitative studies exploring parental beliefs and attitudes toward childhood vaccination identifies common barriers to vaccination. J Clin Epidemiol. 2005;58:1081–8. doi: 10.1016/j.jclinepi.2005.09.002. [DOI] [PubMed] [Google Scholar]
- 31.Mills EJ, Nachega JB, Bangsberg DR, Singh S, Rachlis B, Wu P, et al. Adherence to HAART: a systematic review of developed and developing nation patient-reported barriers and facilitators. PLoS Med. 2006;3:e438. doi: 10.1371/journal.pmed.0030438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Strech D, Synofzik M, Marckmann G. How physicians allocate scarce resources at the bedside: a systematic review of qualitative studies. J Med Philos. 2008;33:80–99. doi: 10.1093/jmp/jhm007. [DOI] [PubMed] [Google Scholar]
- *33.Cheung JM, Atternas K, Melchior M, Marshall NS, Fois RA, Saini B. Primary health care practitioner perspectives on the management of insomnia: a pilot study. Aust J Prim Health. 2014;20:103–12. doi: 10.1071/PY12021. [DOI] [PubMed] [Google Scholar]
- 34.Hislop J, Arber S. Understanding women’s sleep management: beyond medicalization-healthicization? Sociol Health Illn. 2003;25:815–37. doi: 10.1046/j.1467-9566.2003.00371.x. [DOI] [PubMed] [Google Scholar]
- 35.Middlemass J, Davy Z, Cavanagh K, Linehan C, Morgan K, Lawson S, et al. Integrating online communities and social networks with computerised treatment for insomnia: a qualitative study. Br J Gen Pract. 2012;62:e840–50. doi: 10.3399/bjgp12X659321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Moloney ME. Up all night: The medicalization of sleeplessness. Chap. 4, 5. The University of North Carolina; Chapel Hill: 2009. [Google Scholar]
- *37.Davy Z, Middlemass J, Siriwardena AN. Patients’ and clinicians’ experiences and perceptions of the primary care management of insomnia: qualitative study. Health Expect. 2013:1–13. doi: 10.1111/hex.12119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Barter G, Cormack M. The long-term use of benzodiazepines: patients’ views, accounts and experiences. Fam Pract. 1996;13:491–7. doi: 10.1093/fampra/13.6.491. [DOI] [PubMed] [Google Scholar]
- *39.Davidson JR, Feldman-Stewart D, Brennenstuhl S, Ram S. How to provide insomnia interventions to people with cancer: insights from patients. Psychooncol. 2007;16:1028–38. doi: 10.1002/pon.1183. [DOI] [PubMed] [Google Scholar]
- *40.Kyle SD, Espie CA, Morgan K. “…Not just a minor thing, it is something major, which stops you from functioning daily”: quality of life and daytime functioning in insomnia. Behav Sleep Med. 2010;8:123–40. doi: 10.1080/15402002.2010.487450. [DOI] [PubMed] [Google Scholar]
- 41.Cheung JM, Bartlett DJ, Armour CL, Glozier N, Saini B. Insomnia patients’ help-seeking experiences. Behav Sleep Med. 2014;12:106–22. doi: 10.1080/15402002.2013.764529. [DOI] [PubMed] [Google Scholar]
- 42.Henry D, McClellen D, Rosenthal L, Dedrick D, Gosdin M. Is sleep really for sissies? Understanding the role of work in insomnia in the US. Soc Sci Med. 2008;66:715–26. doi: 10.1016/j.socscimed.2007.10.007. [DOI] [PubMed] [Google Scholar]
- *43.Henry D, Rosenthal L, Dedrick D, Taylor D. Understanding patient responses to insomnia. Behav Sleep Med. 2013;11:40–55. doi: 10.1080/15402002.2011.620671. [DOI] [PubMed] [Google Scholar]
- *44.Yung KP, Chung KF, Ho FY, Yeung WF, Ng TH. The experience of chronic insomnia in chinese adults: a study using focus groups and insomnia experience diaries. Behav Sleep Med. 2015;00:1–23. doi: 10.1080/15402002.2015.1017097. [DOI] [PubMed] [Google Scholar]
- 45.Fleming L, Gillespie S, Espie CA. The development and impact of insomnia on cancer survivors: a qualitative analysis. Psychooncol. 2010;19:991–6. doi: 10.1002/pon.1652. [DOI] [PubMed] [Google Scholar]
- 46.Hsu HC, Chen NH, Jou HJ, An C, Tsao LI. Sleep disturbance experiences among perimenopausal women in Taiwan. J Clin Nurs. 2009;18:2116–24. doi: 10.1111/j.1365-2702.2008.02665.x. [DOI] [PubMed] [Google Scholar]
- 47.Hubbling A, Reilly-Spong M, Kreitzer MJ, Gross CR. How mindfulness changed my sleep: focus groups with chronic insomnia patients. BMC Complem Altern Med. 2014;14:50. doi: 10.1186/1472-6882-14-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *48.Carey TJ, Moul DE, Pilkonis P, Germain A, Buysse DJ. Focusing on the experience of insomnia. Behav Sleep Med. 2005;3:73–86. doi: 10.1207/s15402010bsm0302_2. [DOI] [PubMed] [Google Scholar]
- 49.Collier E, Skitt G, Cutts H. A study on the experience of insomnia in a psychiatric inpatient population. J Psychiatr Ment Health Nurs. 2003;10:697–704. doi: 10.1046/j.1365-2850.2003.00654.x. [DOI] [PubMed] [Google Scholar]
- 50.Kleinman L, Buysse DJ, Harding G, Lichstein K, Kalsekar A, Roth T. Patient-reported outcomes in insomnia: development of a conceptual framework and endpoint model. Behav Sleep Med. 2013;11:23–36. doi: 10.1080/15402002.2011.607199. [DOI] [PubMed] [Google Scholar]
- 51.Vigeta SMG, Hachul H, Tufik S, de Oliveira EM. Sleep in postmenopausal women. Qual Health Res. 2012;22:466–75. doi: 10.1177/1049732311422050. [DOI] [PubMed] [Google Scholar]
- 52.Williams S, Meadows R, Arber S. The Sociology of Sleep. In: Cappuccio F, Miller M, Lockley S, editors. Sleep, Health and Society: From Aetiology to Public Health. Northamptonshire, Great Britain: Oxford University Press; 2010. pp. 275–299. [Google Scholar]
- 53.Green J, Britten N. Qualitative research and evidence based medicine. BMJ. 1998;316(7139):1230–2. doi: 10.1136/bmj.316.7139.1230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Anderson C. Presenting and evaluating qualitative research. Am J Pharm Educ. 2010;74:1–7. doi: 10.5688/aj7408141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Gagliardi AR, Dobrow MJ. Paucity of qualitative research in general medical and health services and policy research journals: analysis of publication rates. BMC Health Serv Res. 2011;11:268. doi: 10.1186/1472-6963-11-268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Araújo T. L’expérience vécue des difficultés de sommeil dans la relation de couple au Canada et au Brésil: une étude interculturelle comparative entre les villes de Québec et de Fortaleza. Université Laval; Québec: 2013. [Google Scholar]