Abstract
Health-related quality of life (HRQoL) is an important outcome to assess among persons living with HIV/AIDS, but few studies have been conducted in sub-Saharan Africa. We examined HRQoL among 1180 ART-initiating adults from six clinics in Ethiopia in 2012–2013, and compared the correlates of two subscale scores between women and men. Women scored significantly higher than men on both overall function (8.4 points higher) and life satisfaction (6.3 points higher). In multivariable models, psychological distress, low CD4+ count, unemployment, and food insecurity were associated with lower quality of life scores among women and men. Men whose last sexual encounter occurred 3 months to 1 year from the interview date had lower overall function and life satisfaction scores. Men between the ages of 30–39 had lower overall function scores. Protestant women and women in the low-middle social support category had lower life satisfaction scores. Assessment of HRQoL over time will help inform HIV care and treatment practices to ensure favorable patient outcomes.
Keywords: Quality of life, Gender differences, ART initiation, Psychosocial factors or variables, Ethiopia
Introduction
Health-related quality of life (HRQoL) scales have been utilized to measure the effect of both HIV and its treatment on the functional capacity and well-being of persons living with HIV/AIDS (PLWHA) [1, 2]. In the era of antiretroviral therapy (ART), achieving high HRQoL is a priority in the long-term management of PLWHA in the United States and other higher-income countries [3–5]. The construct of HRQoL is based on the World Health Organization’s definition of health as “a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity” [6] and has been used as a health measure of populations [7]. As life expectancy of PLWHA has increased with the use of ART, and HIV has become a chronic illness [8], HRQoL is of increasing importance. HRQoL has been shown to be a more sensitive marker of symptomatic changes than immunologic/virologic markers [9, 10]. In addition, several studies have reported that HRQoL plays a significant role in retention in care, treatment adherence and survival [11–14]. These studies have shown how patients with the same clinical criteria often have dramatically different responses to treatment. Second, by providing a measure of patient-perceived burden, ART programs can use HRQoL to monitor patient needs and improve retention and engagement in care. Finally, in 2010, Boer-van der Kolk et al. found that patient-reported HRQoL predicted survival among PLWHA independent of clinical and treatment status [13]. It has become increasingly clear that monitoring HRQoL is important for the sustainability of ART programs and the assessment of disease burden.
Prior studies have shown socio-demographic, psychosocial and immunologic factors to be predictive of HRQoL scores [11, 15]. However, few studies have examined these associations in sub-Saharan Africa (SSA)[16, 17]. Because the burden of HIV is greatest in SSA, a better understanding of HRQoL and its determinants among PLWHA is needed in this region [18].
Further, it is important to examine HRQoL scores by gender as men and women tend to experience the social and psychological impact of HIV/AIDS differently [9, 19– 21]. We explored gender differences in HRQoL among PLWHA initiating ART in Ethiopia, where the national prevalence of HIV is 1.5 % (~793,700) and HIV prevalence is almost twice as high among women (1.9 %) than in men (1.0 %) [22]. We also generated additional baseline HRQoL data among ART initiators and focused on the psychosocial correlates of HRQoL.
Data and Methods
Study Population
Participants included in these analyses were recruited in the Multi-level Determinants of Late ART Initiation (LSTART) study, a cross-sectional study conducted from June 2012 through April 2013 to examine the correlates of late ART initiation at six secondary-level urban hospitals in the Oromia State of Ethiopia. Participating health facilities were public sector HIV care and treatment clinics supported by ICAP at Columbia University through funding from the United States President’s Emergency Plan for AIDS Relief (PEPFAR). Participant eligibility criteria included the following: at least 18 years of age, had initiated ART within 2 weeks of study enrollment, and consented to structured interviews.
Data Collection
Data collection consisted of patient interviews and use of clinical information routinely collected by clinicians at patient visits. For the interviews, providers referred interested patients to research staff to learn about the study. Research staff screened the patients for eligibility and solicited written informed consent. Consenting individuals completed an interview in Amharic or Oromiffa that lasted approximately 45 min and the questionnaire collected information on sociodemographics, behavior, socio-medical and psychosocial characteristics. Patient data routinely collected at enrollment in HIV care and during each clinic visit was documented by clinicians on national forms. Trained data clerks routinely abstracted relevant clinical data from patients’ medical charts and entered them into electronic databases. Data quality assessments were performed every 3 months to assess completeness and accuracy. Interview data were linked with clinic medical records for the period of HIV care enrollment through 12 months after ART initiation and de-identified prior to analysis. The study was approved by the institutional review boards at Columbia University, the City University of New York, and the Oromia Regional Bureau of Health in Ethiopia.
Quality of Life Measurement
Instruments to measure HRQoL have been documented in use since 1973 [23]. The majority of efforts to use such instruments to measure HRQoL in the context of HIV postdate 2000, however [24]. For this reason many measures of HRQoL among PLWHA used instruments adapted from other conditions [25]. To date, no “gold standard” of measurement nor established definition exists for HRQoL in PLWHA [24]. The HIV/AIDS-Targeted Quality of Life (HAT-QoL) instrument, used here, was the first HRQoL measurement tool developed directly from the concerns of PLWHA [25]. The HAT-QoL has been in use since 1996 and has been shown to provide both a reliable and valid measure of HRQoL among symptomatic and asymptomatic HIV-infected persons [25, 26]. While the majority of studies that have used HAT-QoL focused on U.S. populations, it has also been proven to be a reliable measure in resource-limited settings, such as SSA [27, 28].
The HAT-QoL instrument measures the following nine subscales of HRQoL: overall function, life satisfaction, health worries, financial worries, medication worries, HIV mastery, disclosure worries, provider trust, and sexual function [25]. In this study, two of the nine subscales—comprising a total of ten items—were examined: overall function and life satisfaction. All HAT-QoL items addressed the 4 weeks before the date of interview. All questions had the same five-point Likert rated options from 1 (none of the time) to 5 (all of the time). Scores for each subscale were then transformed linearly to a possible range of 0–100, according to a prescribed algorithm [29], with higher values indicating better functioning and higher life satisfaction. The Cronbach’s alpha reliability coefficient was 0.96 for the 6-item overall function scale and 0.85 for the 4-item life satisfaction subscale.
Covariates
Hypothesized correlates were chosen a priori based on associations found in the HRQoL literature. Correlates examined included age, marital status, number of children, education, religion, food insecurity, type of residence, electricity, work status, social support, HIV disclosure status, time from last sexual encounter, psychological distress, time since enrollment in HIV care (in days) and early versus late ART initiation with late ART initiation defined as CD4 < 150 cells/µL or WHO IV.
Social support was assessed using a scale developed by Wortman, et al. for the Coping and Change Study, a psychosocial supplement to the Chicago site of the Multicenter AIDS Cohort Study [30, 31]. Response options for each item of the scale were ranked from 1 to 5, where 1 = none and 5 = all of the time. Higher scores represented higher levels of social support, and total scores were divided into categories by quartiles of the distribution among all respondents. Both food insecurity and electricity were assessed as dichotomous variables. Psychological distress was measured using the Kessler-10 Psychological Distress Scale where raw scores were divided based on cut-off levels [32].
Data Analysis
Categorical socio-demographic, psychosocial, and clinical variable distributions were compared between men and women using χ2 tests. Wilcoxon rank-sum non-parametric tests were used to compare gender differences in median time from enrollment in HIV care and age. Univariate tests were used to examine measures of central tendency and dispersion for all variables.
Gender-stratified bivariate and multivariable linear regression analyses were performed to determine factors associated with HAT-QoL score. All factors associated at p < 0.10 in bivariate models were included in multivariable models. Multivariable models controlled for the following factors: age, marital status, number of children, religion, food insecurity, work status, social support, time from last sexual encounter, psychological distress, and early versus late ART initiation. All analyses were conducted using SAS version 9.3 (SAS Institute Inc., Cary, NC, USA).
Results
Participant Characteristics
Characteristics of all 1180 participants (458 males and 722 females) are shown by gender in Table 1. The majority of participants were women (61 %) and resided in urban settings (78 %) with a median age of 34 years (IQR 28–40). Most participants reported less than secondary education levels (72 %). The median time from enrollment in care to ART initiation was 88 days (IQR 16–940).
Table 1.
Participant characteristics by gender, 2012–2013, Oromia, Ethiopia
| (N = 1180) | P value | ||||
|---|---|---|---|---|---|
| Male | Female | ||||
| N | % or median/IQR | N | % or median/IQR | ||
| Number | 458 | 38.8 % | 722 | 61.2 % | |
| Age (in years) | |||||
| <29 | 78 | 17.0 | 296 | 41.0 | |
| 30–39 | 205 | 44.8 | 277 | 38.4 | |
| ≥40 | 175 | 38.2 | 149 | 20.6 | <0.0001 |
| Relationship status | |||||
| Married | 297 | 64.8 | 335 | 46.4 | |
| Not married/single | 160 | 34.9 | 382 | 52.9 | |
| Missing | 1 | 0.2 | 5 | 0.7 | <0.0001 |
| Children | |||||
| None | 112 | 24.4 | 141 | 19.5 | |
| 1–2 | 172 | 37.5 | 338 | 46.8 | |
| 3–4 | 120 | 26.2 | 144 | 19.9 | |
| ≥5 | 53 | 11.6 | 99 | 13.7 | |
| Missing | 1 | 0.2 | 0 | – | <0.05 |
| Education | |||||
| None | 92 | 20.1 | 282 | 39.0 | |
| Any primary | 200 | 43.7 | 273 | 37.8 | |
| Any secondary | 111 | 24.2 | 126 | 17.4 | |
| Any tertiary | 48 | 10.5 | 34 | 4.7 | |
| Vocational or other | 6 | 1.3 | 5 | 0.7 | |
| Missing | 1 | 0.2 | 2 | 0.3 | <0.0001 |
| Religion | |||||
| Ethiopian orthodox | 323 | 70.5 | 501 | 69.4 | |
| Protestant | 85 | 18.5 | 154 | 21.3 | |
| Musim | 47 | 10.3 | 61 | 8.4 | |
| No religion/othera | 3 | 0.6 | 5 | 0.7 | |
| Missing | 0 | – | 1 | 0.1 | 0.54 |
| Food insecurity | |||||
| Never | 172 | 37.5 | 250 | 34.6 | |
| Ever | 284 | 62.0 | 470 | 65.1 | |
| Missing | 2 | 0.4 | 2 | 0.3 | 0.11 |
| Type of residence | |||||
| Rural | 122 | 26.6 | 137 | 18.9 | |
| Urban | 335 | 73.1 | 585 | 81.0 | |
| Missing | 1 | 0.2 | 0 | – | <0.05 |
| Electricity | |||||
| Yes | 344 | 75.1 | 581 | 80.5 | |
| No | 114 | 24.9 | 140 | 19.4 | |
| Missing | 0 | – | 1 | 0.1 | 0.06 |
| Work status | |||||
| Cash or in-kind | 419 | 91.5 | 485 | 67.1 | |
| Not working for payment | 39 | 8.5 | 235 | 32.6 | |
| Don’t know/refused | 0 | – | 2 | 0.3 | <0.0001 |
| Social support | |||||
| Bottom 25 % | 110 | 24.0 | 188 | 26.0 | |
| Low-middle 25 % | 139 | 30.3 | 166 | 23.0 | |
| Middle-high 25 % | 128 | 27.9 | 164 | 22.7 | |
| Top 25 % | 81 | 17.7 | 204 | 28.2 | <0.0001 |
| Disclosed (number) | |||||
| No one | 86 | 18.8 | 81 | 11.2 | |
| 1 person | 160 | 34.9 | 262 | 36.3 | |
| 2–5 people | 145 | 31.7 | 251 | 34.8 | |
| >5 people | 67 | 14.6 | 128 | 17.7 | <0.05 |
| Time since last sexual intercourse | |||||
| Within last 30 days | 158 | 34.4 | 213 | 29.5 | |
| >30 days–3 months | 75 | 16.3 | 71 | 9.8 | |
| 3 months–1 year | 95 | 20.7 | 123 | 17.0 | |
| >1 year/never | 130 | 28.5 | 315 | 43.7 | <0.0001 |
| Kessler distress categoryb | |||||
| None or low | 175 | 38.3 | 305 | 42.2 | |
| Mild or moderate | 140 | 30.5 | 208 | 28.9 | |
| High | 142 | 30.9 | 205 | 28.4 | |
| Missing | 1 | 0.2 | 4 | 0.6 | 0.36 |
| ART WHO stage | |||||
| Stage 1 | 68 | 15.0 | 188 | 26.0 | |
| Stage 2 | 128 | 27.9 | 205 | 28.5 | |
| Stage 3 | 240 | 52.3 | 299 | 41.4 | |
| Stage 4 | 18 | 3.9 | 27 | 3.7 | |
| Missing | 4 | 0.9 | 3 | 0.4 | <0.0001 |
| Enroll WHO stage | |||||
| Stage 1 | 99 | 21.8 | 279 | 38.6 | |
| Stage 2 | 134 | 29.2 | 174 | 24.2 | |
| Stage 3 | 193 | 42.0 | 222 | 30.7 | |
| Stage 4 | 15 | 3.3 | 16 | 2.2 | |
| Missing | 17 | 3.7 | 31 | 4.3 | <0.0001 |
| ART CD4 category | |||||
| <100 cells/µL | 109 | 23.7 | 108 | 14.9 | |
| 100–250 cells/µL | 208 | 45.5 | 252 | 35.0 | |
| ≥250 cells/µL | 109 | 23.7 | 285 | 39.4 | |
| Missing | 32 | 7.0 | 77 | 10.7 | <0.0001 |
| ART initiation status | |||||
| Early | 257 | 56.6 | 551 | 76.4 | |
| Late | 198 | 43.4 | 170 | 23.6 | <0.0001 |
| Days from enrollment in HIV care | 455/458 | 33.0 (14.0, 523.0) | 721/722 | 160.0 (19.0, 1142.0) | <0.0001 |
IQR interquartile range
Other religion category = Catholic, Traditional, Other, and Other Christian
Defined as the Kessler Psychological Distress Scale (K10) where <20 = well, 20–29 = mild/moderate, ≥30 = severe
By gender, a higher proportion of men (43 %) than women (24 %) initiated ART late (p < 0.0001). A higher proportion of men reported being married (65 vs. 46 %; p < 0.0001) and employed for payment (92 vs. 67 %; p < 0.0001). Women tended to be younger (median age 30 vs. 37 years for men; p < 0.0001) and a greater proportion of women reported food insecurity (24 vs. 18 %; p = 0.11).
HAT-QoL Scores
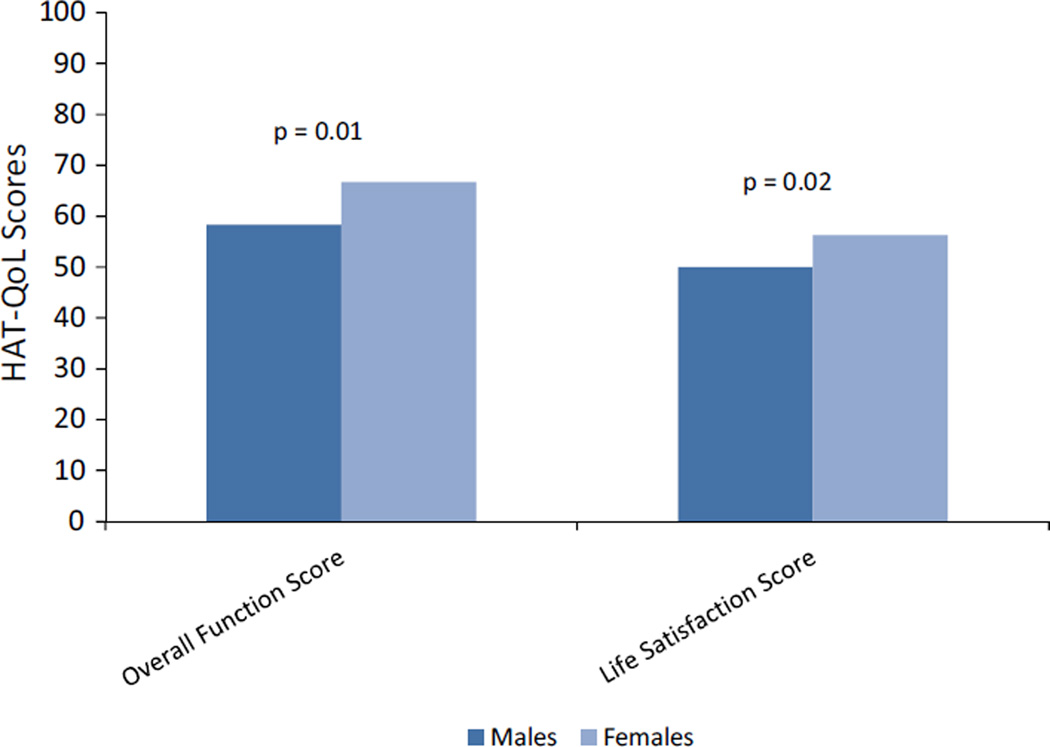
All participants, regardless of gender, scored lower on the life satisfaction subscale (mean score = 51, SD = 26.2) compared to the overall function subscale (mean score = 62, SD = 29.4). Women scored significantly higher than men on both of the subscales: 8.4 points higher on overall function (median score = 66.7 vs. 58.3; p = 0.01) and 6.3 points higher on life satisfaction (median score = 56.3 vs. 50; p = 0.02), Fig. 1.
Fig. 1.
Median *HAT-QoL scores by gender, 2012–2013, Oromia, Ethiopia. *Defined as HIV/AIDS-targeted quality of life instrument where scale = 0 to 100. Higher scores = higher quality of life
Correlates of HAT-QoL Scores
In bivariate analyses, the following variables were associated with lower HAT-QoL scores at the p < 0.10 level for both subscales, among men and women: being single (ref: married), food insecurity, longer time from last sexual encounter, higher levels of psychological distress, and late ART initiation. Greater social support was significantly associated with HAT-QoL scores among both men and women. Among women, Muslims and Protestants reported lower HAT-QoL scores compared to those of other religions. Men who were between the ages of 30–39, unemployed, had fewer than three children, and disclosed HIV status to two or more people reported lower HAT-QoL scores.
In the multivariable model for overall function, mild psychological distress (reference (ref): low distress; β = −21.1, 95 % CI −25.8 to −16.5, p < 0.0001 for men; β = −19.6, 95 % CI −23.6 to −15.7, p < 0.0001 for women) and high psychological distress (ref: low distress; β = −48.4, 95 % CI −53.1 to −43.7, p < 0.0001 for men; β = −45.0, 95 % CI −49.1 to −40.9, p < 0.0001 for women), unemployment (ref: working for cash or in-kind); β = −12.7, 95 % CI −19.5 to −5.8, p = 0.0003 for men; β = −4.1, 95 % CI −7.6 to −0.5, p = 0.0233 for women) and late ART initiation (ref: early initiation; β = −6.7, 95 % CI −10.7 to −2.7, p = 0.0010 for men; β = −9.8, 95 % CI −13.7 to −5.8, p < 0.0001 for women) were independently associated with lower HAT-QoL scores, Table 2. Men between the ages of 30–39 (ref: ≥40 years; β = −5.3, 95 % CI −10.8 to 0.1, p = 0.05) also had lower scores. Men who reported their last sexual encounter occurring 3 months to 1 year from the interview date had lower overall function scores (ref: past 30 days; β = −8.2, 95 % CI −13.7 to −2.7, p = 0.0035).
Table 2.
Parameter estimates from a multivariable linear regression model of overall function by gender, 2012–2013, Oromia, Ethiopia
| Parameter | Men (n = 451) | Women (n = 708) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Estimates | SE | 95 % CI | p-value | Estimates | SE | 95 % CI | p-value | |||
| Lower cl | Upper cl | Lower cl | Upper cl | |||||||
| Age category in years (ref: ≥40) | ||||||||||
| ≤29 | −5.09 | 3.08 | −11.15 | 0.98 | 0.10 | −2.98 | 2.65 | −8.17 | 2.22 | 0.26 |
| 30–39 | −5.35 | 2.78 | −10.80 | 0.11 | 0.05 | −1.25 | 1.89 | −4.97 | 2.46 | 0.51 |
| Marital status (ref: married) | ||||||||||
| Single/not married | −0.50 | 2.70 | −5.81 | 4.80 | 0.85 | −3.12 | 2.23 | −7.49 | 1.25 | 0.16 |
| Children (ref: ≥5) | ||||||||||
| None | 0.94 | 4.10 | −7.12 | 9.01 | 0.82 | −1.97 | 3.17 | −8.20 | 4.25 | 0.53 |
| 1–2 | −0.12 | 3.47 | −6.95 | 6.71 | 0.97 | −1.08 | 2.85 | −6.68 | 4.52 | 0.70 |
| 3–4 | 2.60 | 3.39 | −4.05 | 9.26 | 0.44 | −3.48 | 2.98 | −9.32 | 2.37 | 0.24 |
| Religion (ref: Ethiopian Orthodox) | ||||||||||
| No religion/other | −2.28 | 11.58 | −25.04 | 20.47 | 0.84 | 12.53 | 9.52 | −6.16 | 31.22 | 0.19 |
| Muslim | 1.26 | 3.27 | −5.16 | 7.68 | 0.70 | −2.98 | 3.05 | −8.97 | 3.01 | 0.33 |
| Protestant | −4.42 | 2.50 | −9.32 | 0.49 | 0.08 | −3.53 | 2.00 | −7.47 | 0.40 | 0.08 |
| Food insecurity (ref: never) | ||||||||||
| Ever | −0.11 | 2.84 | −5.69 | 5.47 | 0.97 | −2.63 | 2.37 | −7.29 | 2.04 | 0.27 |
| Work status (ref: cash or in-kind) | ||||||||||
| Not working | −12.68 | 3.48 | −19.53 | −5.84 | <0.05 | −4.10 | 1.80 | −7.63 | −0.56 | <0.05 |
| Social support (ref: top 25 %) | ||||||||||
| Bottom 25 % | 0.20 | 3.27 | −6.23 | 6.64 | 0.95 | 0.28 | 2.38 | −4.40 | 4.96 | 0.91 |
| Low-middle 25 % | 3.85 | 2.94 | −1.93 | 9.63 | 0.19 | −2.09 | 2.37 | −6.74 | 2.57 | 0.38 |
| Middle-high 25 % | 3.83 | 2.93 | −1.92 | 9.58 | 0.19 | 0.35 | 2.29 | −4.14 | 4.83 | 0.88 |
| Last sexual encounter (ref: past 30 days) |
||||||||||
| >1 year/never | −4.33 | 2.78 | −9.79 | 1.12 | 0.12 | −1.45 | 2.61 | −6.57 | 3.67 | 0.58 |
| 3 months–1 year | −8.20 | 2.79 | −13.68 | −2.71 | <0.05 | −1.52 | 2.63 | −6.67 | 3.64 | 0.56 |
| >30 days–3 months | −3.36 | 2.89 | −9.03 | 2.32 | 0.25 | 4.50 | 2.99 | −1.37 | 10.36 | 0.13 |
| Psychological distress (ref: none or low) |
||||||||||
| High | −48.43 | 2.39 | −53.13 | −43.73 | <0.0001 | −44.98 | 2.09 | −49.08 | −40.88 | <0.0001 |
| Mild or moderate | −21.14 | 2.36 | −25.78 | −16.49 | <0.0001 | −19.65 | 2.02 | −23.61 | −15.69 | <0.0001 |
| Late ART status (ref: early initiation) | ||||||||||
| Late initiation | −6.69 | 2.03 | −10.68 | −2.71 | <0.05 | −9.77 | 2.01 | −13.73 | −5.82 | <0.0001 |
Correlates examined at the bivariate level included age, marital status, number of children, education, religion, food insecurity, type of residence, electricity work status, social support, HIV disclosure status, time from last sexual encounter, psychological distress, time since enrollment in HIV care (in days) and early versus late ART initiation with late ART initiation defined as CD4 < 150 cells/µL or WHO IV. All variables associated at p < 0.10 in bivariate models were included above
Estimates greater than 1 are better
CI confidence interval, SE standard error
With regards to life satisfaction, mild psychological distress (ref: low distress; β = −19.5, 95 % CI −23.5 to −15.5, p < 0.0001 for men; β = −17.2, 95 % CI −20.7 to −13.6, p < 0.0001 for women) and high psychological distress (ref: low distress; β = −41.7, 95 % CI −45.8 to −37.6, p < 0.0001 for men; β = −37.0, 95 % CI −40.7 to −33.3, p < 0.0001 for women), food insecurity (ref: never; β = −7.6, 95 % CI −12.4 to −2.7, p = 0.0022 for men; β = −11.1, 95 % CI −15.3 to −6.9, p < 0.0001 for women), and late ART initiation (ref: early initiation; β = −5.6, 95 % CI −9.1 to −2.2, p = 0.0014 for men; β = −5.9, 95 % CI −9.5 to −2.4, p = 0.0010 for women) remained strong correlates, Table 3. Unemployed men (β = −6.0, 95 %CI−12.0 to−0.09, p = 0.0465) and those who reported their last sexual encounter occurring 3 months to 1 year from the interview date (β = −5.9, 95 %CI−10.6 to −1.1, p = 0.0155) had lower life satisfaction scores. Protestant women (ref: Ethiopian Orthodox; β = −3.9, 95 % CI −7.5 to −0.4, p = 0.0279) and those in the low-middle social support category (ref: high social support; β = −4.8, 95 % CI −9.0 to −0.6, p = 0.0234) also scored lower on the life satisfaction subscales.
Table 3.
Parameter estimates from a multivariable linear regression model of life satisfaction by gender, 2012–2013, Oromia, Ethiopia
| Parameter | Males (n = 451) | Females (n = 708) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Estimates | SE | 95 % CI | p-value | Estimates | SE | 95 % CI | p-value | |||
| Lower cl | Upper cl | Lower cl | Upper cl | |||||||
| Age category in years (ref: ≥40) | ||||||||||
| ≤29 | 0.27 | 2.68 | −5.00 | 5.53 | 0.92 | 0.28 | 2.37 | −4.37 | 4.93 | 0.91 |
| 30–39 | −2.11 | 2.41 | −6.84 | 2.63 | 0.38 | −1.96 | 1.69 | −5.29 | 1.37 | 0.25 |
| Marital status (ref: married) | ||||||||||
| Single/not married | 0.38 | 2.34 | −4.22 | 4.98 | 0.87 | −1.14 | 1.99 | −5.06 | 2.77 | 0.57 |
| Children (ref: ≥5) | ||||||||||
| None | −4.20 | 3.56 | −11.21 | 2.80 | 0.24 | −4.13 | 2.84 | −9.71 | 1.44 | 0.15 |
| 1–2 | −4.65 | 3.02 | −10.58 | 1.28 | 0.12 | −1.14 | 2.55 | −6.15 | 3.88 | 0.66 |
| 3–4 | 1.21 | 2.94 | −4.57 | 6.99 | 0.68 | −2.05 | 2.67 | −7.29 | 3.19 | 0.44 |
| Religion (ref: Ethiopian Orthodox) | ||||||||||
| No religion/other | −12.25 | 10.05 | −32.00 | 7.51 | 0.22 | 9.54 | 8.53 | −7.20 | 26.28 | 0.26 |
| Muslim | −0.13 | 2.84 | −5.71 | 5.45 | 0.96 | −2.70 | 2.73 | −8.06 | 2.66 | 0.32 |
| Protestant | −3.10 | 2.17 | −7.36 | 1.16 | 0.15 | −3.95 | 1.79 | −7.48 | −0.43 | <0.05 |
| Food insecurity (ref: never) | ||||||||||
| Ever | −7.59 | 2.46 | −12.43 | −2.75 | <0.05 | −11.13 | 2.13 | −15.30 | −6.95 | <0.0001 |
| Work status (ref: cash or in-kind) | ||||||||||
| Not working | −6.04 | 3.02 | −11.98 | −0.09 | 0.05 | −2.11 | 1.61 | −5.28 | 1.06 | 0.19 |
| Social support (ref: top 25 %) | ||||||||||
| Bottom 25 % | −1.57 | 2.84 | −7.16 | 4.02 | 0.58 | −0.76 | 2.14 | −4.95 | 3.43 | 0.72 |
| Low-middle 25 % | 1.67 | 2.55 | −3.35 | 6.69 | 0.51 | −4.82 | 2.12 | −8.99 | −0.65 | < 0.05 |
| Middle-high 25 % | 1.77 | 2.54 | −3.22 | 6.76 | 0.49 | −0.96 | 2.05 | −4.98 | 3.06 | 0.64 |
| Last sexual encounter (ref: past 30 days) | ||||||||||
| >1 year/never | −2.99 | 2.41 | −7.73 | 1.75 | 0.22 | −0.09 | 2.33 | −4.68 | 4.49 | 0.97 |
| 3 months–1 year | −5.89 | 2.42 | −10.65 | −1.13 | < 0.05 | −2.79 | 2.35 | −7.41 | 1.82 | 0.24 |
| >30 days–3 months | 0.69 | 2.51 | −4.24 | 5.62 | 0.78 | 2.23 | 2.67 | −3.02 | 7.48 | 0.40 |
| Psychological distress (ref: none or low) | ||||||||||
| High | −41.69 | 2.08 | −45.77 | −37.61 | < 0.0001 | −37.00 | 1.87 | −40.67 | −33.32 | < 0.0001 |
| Mild or moderate | −19.52 | 2.05 | −23.55 | −15.49 | < 0.0001 | −17.16 | 1.81 | −20.71 | −13.61 | < 0.0001 |
| Late ART status (ref: early initiation) | ||||||||||
| Late initiation | −5.66 | 1.76 | −9.12 | −2.20 | < 0.05 | −5.94 | 1.80 | −9.48 | −2.40 | < 0.05 |
Correlates examined at the bivariate level included age, marital status, number of children, education, religion, food insecurity, type of residence, electricity work status, social support, HIV disclosure status, time from last sexual encounter, psychological distress, time since enrollment in HIV care (in days) and early versus late ART initiation with late ART initiation defined as CD4 < 150 cells/µL or WHO IV. All variables associated at p < 0.10 in bivariate models were included above
Estimates greater than 1 are better
CI confidence interval, SE standard error
Discussion
The rapid scale-up of ART in SSA over the past decade has both increased life expectancy and reduced HIV-related morbidity in this region [33]. Barriers to care and treatment still exist [34, 35], however, including those in the realms of the psychosocial and socio-medical aspects of living with HIV/AIDS. Although psychosocial barriers to accessing care and treatment, such as stigma and HIV knowledge, have been well described in this region [36–38] less attention has been paid to socio-medical aspects such as HRQoL [16]. The assessment of HRQoL is central to understanding how people are affected by HIV infection and how this may, in turn, affect utilization of care across the HIV care continuum.
Our study results showed that elevated levels of psychological distress and late ART initiation were significantly associated with lower overall function and life satisfaction scores among men and women. The observed association between psychological distress and HRQoL is consistent with prior research from the region [39]. Although the cause of psychological distress is beyond the scope of this study, the availability of ongoing counseling services to PLWHA has been shown to help mitigate the trauma or other psychological effects that may result from receiving an HIV diagnosis, navigating complex drug regimens, or isolation caused by stigma [40, 41]. Our findings that persons who initiated treatment late (CD4+ count <150 cells/µL or WHO stage 4) had lower HAT-QoL scores than those with less advanced disease were also consistent with studies performed in other resource-limited settings that showed a strong correlation between clinical indicators and HRQoL [2, 12]. Both unemployed men and women reported lower overall function scores but the effect of unemployment on HAT-QoL scores was larger in men. Unemployment may reflect both poorer function and mental well-being directly influencing reported HRQoL [15]. In addition, unemployment may be more strongly associated with HRQoL among men as compared to women due to the higher labor participation rates of men in our study population. Lastly, food insecurity was associated with lower life satisfaction scores for both genders. In women, the effect of food insecurity on HRQoL was larger than for men. Food insecurity affects millions of households in SSA [42] and women tend to play a larger role in domestic responsibilities in this region [43].
Other factors associated with HRQoL varied by gender. Among women, Protestants reported lower life satisfaction scores than Ethiopian Orthodox, but the latter represented the majority of participants (>60 %). Women in the low-middle social support category also reported lower life satisfaction scores than women in the top social support category. Studies have shown that women may be more vulnerable to HIV-related stigma and social support may be a protective resource for mental health and quality of life among HIV-infected women [44]. For men, longer time from last sexual encounter and lack of employment were associated with both lower overall function and life satisfaction scores. Time from last sexual encounter and employment status may serve as indicators of functional status and, hence, may directly affect measures of overall function, in particular [3].
The study has several strengths as it represents one of the first studies to utilize HAT-QoL in Ethiopia and in an HIV-infected population at ART initiation. Measures of HRQoL in SSA have mainly focused on medication-related physical effects experienced by ART users [45]. However, social and psychological issues experienced by ART users can also play a pivotal role in HRQoL and influence health outcomes [18, 46]. By examining baseline HRQoL among ART initiators, our study focused on psychosocial correlates of HRQoL beyond the anticipated effects of ART. The study included a large and diverse sample of participants and stratified by gender. It also utilized both clinical data as well as systematically assessing HRQoL through use of an established survey instrument.
Our study has some limitations worth noting. First, due to its cross-sectional design, we were unable to establish temporal associations between the covariates examined and HAT-QoL scores. However, our parameters were chosen a priori based on established literature of HRQoL predictors both in SSA and resource-rich regions, and our results were consistent with previous findings from both cross-sectional and prospective studies [3, 15, 41, 42]. Other limitations of our study included that we did not use the full HAT-QoL questionnaire. Due to the length of the study questionnaire, our study was limited to subscales exploring overall function and life satisfaction.
In Ethiopia, where an estimated 793,700 people are living with HIV [22], gender disparities exist not only in the prevalence of HIV/AIDS, but in the social, economic, and psychological impact of HIV/AIDS [47]. Additional information on HIV/AIDS-related outcomes, such as HRQoL, stratified by gender, should be identified for interventions specifically targeted to ART initiating patients to improve long-term health outcomes. Further research is needed to assess change in HRQoL over time to help inform HIV care and treatment and ensure favorable outcomes for all patients.
Acknowledgments
We would like to thank all patients at the health facilities included in this study. We want to acknowledge the efforts of the ICAP staff in-country and health facility staff for their commitment to confronting the HIV epidemic. We would also like to thank Dr. David G. Ostrow for his consultative contributions to this study. This work was supported by a research grant from the National Institute of Mental Health (Grant No. R01MH089831). All the clinics included in this analysis received support from ICAP at Columbia University through funding from the President’s Emergency Plan for AIDS Relief.
References
- 1.Guyatt GH, Feeny DH, Patrick DL. Measuring health-related quality of life. Ann Intern Med. 1993;118(8):622–629. doi: 10.7326/0003-4819-118-8-199304150-00009. [DOI] [PubMed] [Google Scholar]
- 2.Safren SA, Hendriksen ES, Smeaton L, et al. Quality of life among individuals with HIV starting antiretroviral therapy in diverse resource-limited areas of the world. AIDS Behav. 2012;16(2):266–277. doi: 10.1007/s10461-011-9947-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Liu C, Johnson L, Ostrow D, Silvestre A, Visscher B, Jacobson LP. Predictors for lower quality of life in the HAART era among HIV-infected men. J Acquir Immune Defic Syndr. 2006;42(4):470–477. doi: 10.1097/01.qai.0000225730.79610.61. [DOI] [PubMed] [Google Scholar]
- 4.Mandorfer M, Payer BA, Scheiner B, et al. Health-related quality of life and severity of fatigue in HIV/HCV co-infected patients before, during, and after antiviral therapy with pegylated interferon plus ribavirin. Liver Int. 2014;34(1):69–77. doi: 10.1111/liv.12253. [DOI] [PubMed] [Google Scholar]
- 5.Merlins JS, Tucker RO, Saag MS, Selwyn PA. The role of palliative care in the current HIV treatment era in developed countries. Top Antivir Med. 2013;21(1):20–26. [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization. Geneva: WHO; 1948. WHO Constitution. [Google Scholar]
- 7.Romero M, Vivas-Consuelo D, Alvis-Guzman N. Is Health Related Quality of Life (HRQoL) a valid indicator for health systems evaluation? Springer Plus. 2013;2:664. doi: 10.1186/2193-1801-2-664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Deeks SG, Lewin SR, Havlir DV. The end of AIDS: HIV infection as a chronic disease. Lancet. 2013;382(9903):1525–1533. doi: 10.1016/S0140-6736(13)61809-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vigneshwaran E, Padmanabhareddy Y, Devanna N, Alvarez-Uria G. gender differences in health related quality of life of people living with HIV/AIDS in the era of highly active antiretroviral therapy. N Am J Med Sci. 2013;5(2):102–107. doi: 10.4103/1947-2714.107526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.MacArthur RD, DuPont HL. Etiology and pharmacologic management of noninfectious diarrhea in HIV-infected individuals in the highly active antiretroviral therapy era. Clin Infect Dis. 2012;55(6):860–867. doi: 10.1093/cid/cis544. [DOI] [PubMed] [Google Scholar]
- 11.Jia H, Uphold CR, Wu S, Chen GJ, Duncan PW. Predictors of changes in health-related quality of life among men with HIV infection in the HAART era. AIDS Patient Care STDS. 2005;19(6):395–405. doi: 10.1089/apc.2005.19.395. [DOI] [PubMed] [Google Scholar]
- 12.Tomita A, Garrett N, Werner L, et al. Health-related quality of life dynamics of HIV-positive South African Women up to ART initiation: evidence from the CAPRISA 002 acute infection cohort study. AIDS Behav. 2014;18(6):1114–1123. doi: 10.1007/s10461-013-0682-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.de Boer-van der Kolk IM, Sprangers MA, Prins JM, Smit C, de Wolf F, Nieuwkerk PT. Health-related quality of life and survival among HIV-infected patients receiving highly active antiretroviral therapy: a study of patients in the AIDS Therapy Evaluation in the Netherlands (ATHENA) Cohort. Clin Infect Dis. 2010;50(2):255–263. doi: 10.1086/649216. [DOI] [PubMed] [Google Scholar]
- 14.Mannheimer SB, Matts J, Telzak E, et al. Quality of life in HIV-infected individuals receiving antiretroviral therapy is related to adherence. AIDS Care. 2005;17(1):10–22. doi: 10.1080/09540120412331305098. [DOI] [PubMed] [Google Scholar]
- 15.Rueda S, Raboud J, Plankey M, et al. Labor force participation and health-related quality of life in HIV-positive men who have sex with men: the Multicenter AIDS Cohort Study. AIDS Behav. 2012;16(8):2350–2360. doi: 10.1007/s10461-012-0257-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Greeff M, Chepuka LM, Chilemba W, et al. Using an innovative mixed method methodology to investigate the appropriateness of a quantitative instrument in an African context: Antiretroviral treatment and quality of life. AIDS Care. 2013 doi: 10.1080/09540121.2013.859651. [DOI] [PubMed] [Google Scholar]
- 17.Igumbor J, Stewart A, Holzemer W. Comparison of the health-related quality of life, CD4 count and viral load of AIDS patients and people with HIV who have been on treatment for 12 months in rural South Africa. SAHARA J. 2013;10(1):25–31. doi: 10.1080/17290376.2013.807070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Odek WO. Social networks and mental health among people living with human immunodeficiency virus (HIV) in Johannesburg, South Africa. AIDS Care. 2014;26(8):1042–1049. doi: 10.1080/09540121.2014.902421. [DOI] [PubMed] [Google Scholar]
- 19.Geary C, Parker W, Rogers S, et al. Gender differences in HIV disclosure, stigma, and perceptions of health. AIDS Care. 2014;26(11):1419–1425. doi: 10.1080/09540121.2014.921278. [DOI] [PubMed] [Google Scholar]
- 20.Richardson ET, Collins SE, Kung T, et al. Gender inequality and HIV transmission: a global analysis. J Int AIDS Soc. 2014;17:19035. doi: 10.7448/IAS.17.1.19035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hare AQ, Ordonez CE, Johnson BA, et al. Gender-specific risk factors for virologic failure in KwaZulu-Natal: automobile ownership and financial insecurity. AIDS Behav. 2014;18(11):2219–2229. doi: 10.1007/s10461-014-0849-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ethiopia FDRo. Country progress report on the HIV Response, 2014. Addis Ababa. 2014 [Google Scholar]
- 23.Wood-Dauphinee S. Assessing quality of life in clinical research: from where have we come and where are we going? J Clin Epidemiol. 1999;52(4):355–363. doi: 10.1016/s0895-4356(98)00179-6. [DOI] [PubMed] [Google Scholar]
- 24.Drewes J, Gusy B, Ruden U. More than 20 years of research into the quality of life of people with HIV and AIDS—a descriptive review of study characteristics and methodological approaches of published empirical studies. J Int Assoc Provid AIDS Care. 2013;12(1):18–22. doi: 10.1177/1545109712456429. [DOI] [PubMed] [Google Scholar]
- 25.Holmes WC, Shea JA. Performance of a new, HIV/AIDS-targeted quality of life (HAT-QoL) instrument in asymptomatic seropositive individuals. Qual Life Res. 1997;6(6):561–571. doi: 10.1023/a:1018464200708. [DOI] [PubMed] [Google Scholar]
- 26.Holmes WC, Bilker WB, Wang H, Chapman J, Gross R. HIV/AIDS-specific quality of life and adherence to antiretroviral therapy over time. J Acquir Immune Defic Syndr. 2007;46(3):323–327. doi: 10.1097/QAI.0b013e31815724fe. [DOI] [PubMed] [Google Scholar]
- 27.Taylor TN, Dolezal C, Tross S, Holmes WC. Reliability and validity of two HIV/AIDS-specific quality of life instruments adapted for use in HIV-positive Zimbabweans. AIDS Care. 2009;21(5):598–607. doi: 10.1080/09540120802302574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Phaladze NA, Human S, Dlamini SB, et al. Quality of life and the concept of “living well” with HIV/AIDS in sub-Saharan Africa. J Nurs Scholarsh. 2005;37(2):120–126. doi: 10.1111/j.1547-5069.2005.00023.x. [DOI] [PubMed] [Google Scholar]
- 29.Holmes WC, Shea JA. A new HIV/AIDS-targeted quality of life (HAT-QoL) instrument: development, reliability, and validity. Med Care. 1998;36(2):138–154. doi: 10.1097/00005650-199802000-00004. [DOI] [PubMed] [Google Scholar]
- 30.Kessler RC, Price RH, Wortman CB. Social factors in psychopathology: stress, social support, and coping processes. Annu Rev Psychol. 1985;36:531–572. doi: 10.1146/annurev.ps.36.020185.002531. [DOI] [PubMed] [Google Scholar]
- 31.Drummond MF. The economic impact of AIDS. AIDS Care. 1989;1(2):216–218. doi: 10.1080/09540128908260265. [DOI] [PubMed] [Google Scholar]
- 32.Kessler RC, Andrews G, Colpe LJ, et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med. 2002;32(6):959–976. doi: 10.1017/s0033291702006074. [DOI] [PubMed] [Google Scholar]
- 33.El-Sadr WM, Holmes CB, Mugyenyi P, et al. Scale-up of HIV treatment through PEPFAR: a historic public health achievement. J Acquir Immune Defic Syndr. 2012;60(Suppl 3):S96–S104. doi: 10.1097/QAI.0b013e31825eb27b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lahuerta M, Ue F, Hoffman S, et al. The problem of late ART initiation in Sub-Saharan Africa: a transient aspect of scale-up or a long-term phenomenon? J Health Care Poor Underserved. 2013;24(1):359–383. doi: 10.1353/hpu.2013.0014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lahuerta M, Wu Y, Hoffman S, et al. Advanced HIV disease at entry into HIV care and initiation of antiretroviral therapy during 2006–2011: findings from four sub-saharan African countries. Clin Infect Dis. 2014;58(3):432–441. doi: 10.1093/cid/cit724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tomori C, Kennedy CE, Brahmbhatt H, et al. Barriers and facilitators of retention in HIV care and treatment services in Iringa, Tanzania: the importance of socioeconomic and sociocultural factors. AIDS Care. 2013 doi: 10.1080/09540121.2013.861574. [DOI] [PubMed] [Google Scholar]
- 37.Risher K, Adams D, Sithole B, et al. Sexual stigma and discrimination as barriers to seeking appropriate healthcare among men who have sex with men in Swaziland. J Int AIDS Soc. 2013;16(3 Suppl 2):18715. doi: 10.7448/IAS.16.3.18715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ayiga N, Nambooze H, Nalugo S, Kaye D, Katamba A. The impact of HIV/AIDS stigma on HIV counseling and testing in a high HIV prevalence population in Uganda. Afr Health Sci. 2013;13(2):278–286. doi: 10.4314/ahs.v13i2.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kagee A. Psychological distress among persons living with HIV, hypertension, and diabetes. AIDS Care. 2010;22(12):1517–1521. doi: 10.1080/09540121.2010.484458. [DOI] [PubMed] [Google Scholar]
- 40.Selman L, Simms V, Penfold S, et al. ‘My dreams are shuttered down and it hurts lots’—a qualitative study of palliative care needs and their management by HIV outpatient services in Kenya and Uganda. BMC Palliat Care. 2013;12(1):35. doi: 10.1186/1472-684X-12-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Fleishman JA, Sherbourne CD, Cleary PD, Wu AW, Crystal S, Hays RD. Patterns of coping among persons with HIV infection: configurations, correlates, and change. Am J Commun Psychol. 2003;32(1–2):187–204. doi: 10.1023/a:1025667512009. [DOI] [PubMed] [Google Scholar]
- 42.Garcia J, Hromi-Fiedler A, Mazur RE, et al. Persistent household food insecurity, HIV, and maternal stress in peri-urban Ghana. BMC Public Health. 2013;13:215. doi: 10.1186/1471-2458-13-215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Studies ESoP. Gender inequality and women’s empowerment, Addis Ababa: United Nations Population Fund (UNFPA) 2008 [Google Scholar]
- 44.Casale M, Wild L, Cluver L, Kuo C. Social support as a protective factor for depression among women caring for children in HIV-endemic South Africa. J Behav Med. 2015;38(1):17–27. doi: 10.1007/s10865-014-9556-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Breet E, Kagee A, Seedat S. HIV-related stigma and symptoms of post-traumatic stress disorder and depression in HIV-infected individuals: does social support play a mediating or moderating role? AIDS Care. 2014;26(8):947–951. doi: 10.1080/09540121.2014.901486. [DOI] [PubMed] [Google Scholar]
- 46.Palermo T, Rawat R, Weiser SD, Kadiyala S. Food access and diet quality are associated with quality of life outcomes among HIV-infected individuals in Uganda. PLoS One. 2013;8(4):e62353. doi: 10.1371/journal.pone.0062353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sori AT. Poverty, sexual experience and HIV vulnerability risks: evidence from Addis Ababa, Ethiopia. J Biosoc Sci. 2012;44(6):677–701. doi: 10.1017/S0021932012000193. [DOI] [PubMed] [Google Scholar]