Abstract
Objective To determine whether parent health behavior changes and feeding practices were associated with child changes in body mass index z-score and related health behaviors over the course of 1 year. Methods Anthropometric data from 590 child–parent dyads of ethnic/racial minority groups were collected at baseline, 14 weeks (postintervention), and 1-year follow-up. Additionally, parent screen time and feeding practices and child dietary consumption, diet quality, physical activity, and screen time were collected. Results Random effects growth models revealed that changes in child screen time moved in tandem with parent screen time from baseline to 14-week postintervention and from postintervention to 1-year follow-up. Greater parental monitoring predicted greater reduction in child calorie consumption at 1 year. Conclusions Future studies should include innovative ways to explicitly involve parents in prevention efforts.
Keywords: childhood obesity, minority, parent, preschool, prevention
Introduction
Although some recent improvements have been noted, the rates of obesity among preschool children remain alarmingly high (Ogden, Carroll, Kit, & Flegal, 2014). Without intervention, obese children are more likely to remain obese into adulthood, increasing the risk of poor health outcomes (Cunningham, Kramer, & Narayan, 2014; Fahlman, McCaugtry, Martin, & Shen, 2010; Olshansky et al., 2005). Results from the 2011–2012 National Health and Nutrition Examination Survey found that among 2- to 5-year-olds, 3.5% of Non-Hispanic Caucasians, 11.3% of Non-Hispanic African-Americans, and 16.7% of Hispanics are obese, and the prevalence of obesity is even higher among 6–11-year-olds (13.1% of Non-Hispanic Caucasians, 23.8% of Non-Hispanic African-Americans, and 26.1% of Hispanics; Ogden et al., 2014). Thus, the preschool years represent a critical period to address weight-related health behaviors among at-risk children (Estabrooks, Dzewaltowski, Glasgow, & Klesges, 2003; Fitzgibbon et al., 2005; Hesketh & Campbell, 2010). Identifying variables associated with child health behavior change related to weight among at-risk preschool children can inform future prevention efforts.
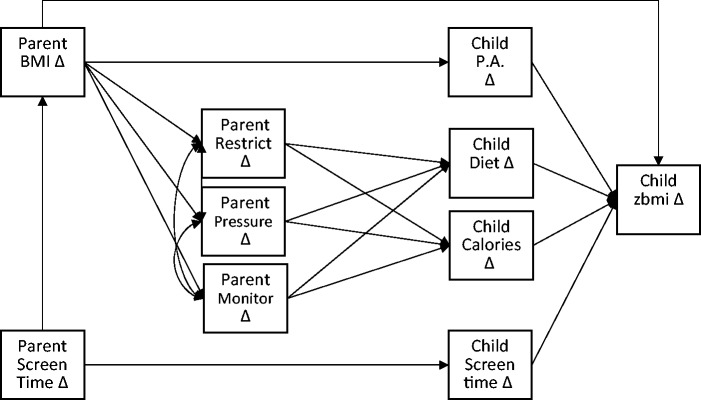
Previous reviews of the childhood obesity prevention literature suggest that parental involvement and parent behavior change are paramount in the initiation and maintenance of child changes (Bluford, Sherry, & Scanlon, 2007; Campbell & Hesketh, 2007; Golley, Hendrie, Slater, & Corsini, 2011; Skouteris et al., 2011). In a 2011 review, Skouteris and colleagues (2011) proposed a conceptual model illustrating the relation between preschool child weight and child and parent beliefs and behaviors (See Figure 1; Bluford et al., 2007; Faith & Kerns, 2005; Harvey-Berino & Rourke, 2003; Lobstein, Baur, & Uauy, 2004; Trost et al., 2003). Results across studies have reported an association between parent and child health behaviors (e.g., eating behaviors, physical activity, sedentary behaviors), such that behaviors change in tandem. More specifically, as depicted in Figure 1, parent modeling and reinforcement of child eating predicts child behaviors, and these behaviors predict child weight. Additionally, research suggests a link between child eating behaviors and parent feeding practices. Faith and colleagues (2004) found that parental pressure to eat and parental monitoring were associated with lower child body mass index (BMI), and restriction was associated with higher child BMI. The relations between parent behaviors and child behaviors can be conceptualized through the broad principles of Social Cognitive Theory (SCT; Bandura, 1986), which suggests that personal change occurs as a result of the dynamic interaction between behavior change, cognition, and the environment (e.g., social support). From a SCT perspective, parental modeling of health behaviors and reinforcement of child behaviors serve as mechanisms for change as depicted in the conceptual model.
Figure 1.
Associations between parent health behaviors, child health behaviors, and child weight. Adapted with permission from Skouteris and colleagues (2011) and John Wiley & Sons, Inc.
Although relations between parent and child health behaviors and obesity have been studied extensively in Caucasian children, research on the relations between parent and child health behavior changes ethnic and racial minority preschool children is sparse. Harvey-Berino and Rourke (2003) investigated the impact of parent education regarding child feeding practices on child weight outcomes in a sample of 43 Native American mothers of preschool children. They found that reduction in parental food restriction was associated with improved weight gain prevention. To our knowledge, no studies to date have examined relationships in the long-term changes in child and parent health behaviors in a predominately African-American sample.
The current study contributes to the literature by exploring relations between child and adult weight status and behavior changes over the course of a year in a predominantly African-American sample of preschoolers. The Hip-Hop to Health Jr. Obesity Prevention Effectiveness Trial (HH Effectiveness) was a 14-week teacher-delivered intervention targeting preschool children. We hypothesized that across the three time points of the HH Effectiveness trial (baseline, 14-week postintervention, and 1-year follow-up), parent BMI changes and screen time would predict changes in child body mass index z-score (z-BMI) and screen time, respectively. We also hypothesized that maladaptive parent feeding practices would predict calorie overconsumption and poor diet quality, leading to increased weight gain. Although HH Effectiveness was primarily school-based, establishing relations between parent and preschool child weight and health behavior changes over time within this at-risk group may help to inform the development of more focused strategies to address childhood obesity.
Method
Study Design, Participants, Setting
HH Effectiveness was a randomized controlled trial designed to compare BMI and z-BMI changes in intervention and comparison groups at 14 weeks postintervention and 1-year follow-up. Eighteen schools were randomized to one of two conditions: (1) a teacher-delivered weight control intervention curriculum or (2) a teacher-delivered general health curriculum. Participants were 590 preschool children participating in Head Start programs administered through Chicago Public Schools. Each school served predominantly African-American students, and two preschool classrooms from each school participated in the study. Child age ranged from 3 to 5 years (M = 4.3; SD = 0.5). Children were primarily African-American (94% of the sample). Only 3% of participants were Hispanic or Latino, 0.5% were Asian, and 2.5% were multiracial. Parents were also primarily African-American (95%). About 3% reported that they were Hispanic or Latino, and about 2% were multiracial or other. About 80% of parents reported an annual household income that was <$30,000. Mean child z-BMI was 0.64 (SD = 1.03) and mean parent BMI was 32 (SD = 8.34). All children in the intervention and control classrooms received the classroom curriculum. However, data were only collected from children whose parent/guardian provided informed consent. There were 729 children enrolled in the participating classrooms (Fitzgibbon et al., 2011; Kong et al., 2015). We were unable to obtain parental consent for 60 of these children (8%, 30 from intervention classrooms, 30 from control classrooms). In many of these cases, the parent did not actively refuse consent; instead, we were unable to contact the parent during the recruitment period. The institutional review boards at the University of Illinois at Chicago and the Chicago Public Schools approved this study.
Intervention Components
Intervention Curriculum
Full descriptions of the Hip-Hop to Health Jr. intervention and general health curriculum including theoretical framework, were described previously (Fitzgibbon et al., 2002). Briefly, the intervention included both a classroom and minimal parent component and was delivered twice weekly for 14 weeks. The intervention curriculum sought to improve diet quality (e.g., decrease fat intake, increase fruits and vegetables) and physical activity, and decrease television viewing. Each week’s sessions focused on a theme and included (1) a 20-min lesson on healthy eating or physical activity and (2) a 20-min interactive physical activity component. Teachers were provided colorful puppets representing food groups, and a CD with songs about healthy eating and exercise and two fully scripted exercise routines. Cultural practices and beliefs in key areas such as food, family, music, community, social roles, and relationships were all considered in the development of these materials (Fitzgibbon et al., 2002).
Parent Component
Parents received the same CD used in the classroom in addition to a weekly newsletter that highlighted the weekly theme along with an optional homework assignment reinforcing concepts. Examples of newsletter topic areas included education around portion sizes, healthy snacks, encouraging consumption of five or more fruits and vegetables per day, and limiting television watching. The corresponding homework assignments were designed to check for comprehension, and to encourage parents to help their children make changes around eating and active lifestyle. Parents received $5 per completed homework assignment returned. On average, the 307 parents in the intervention group completed 5.0 (SD = 4.5) of the 13 homework assignments. Twenty (7%) of the parents completed all 13 assignments. One hundred fifteen parents (37%) completed more than half of the homework assignments, and 238 (78%) completed at least one assignment (Fitzgibbon et al., 2011).
General Health Curriculum
The control classrooms received the “general health” curriculum, which was offered once weekly over the course of 14 weeks. Teachers covered a variety of health and safety topics such as car safety (e.g., seat belts, car seats), immunizations, dental hygiene, and emergency procedures (e.g., calling 911). Parents received a weekly newsletter based on that week’s topic, but were not asked to complete homework.
Procedure
At baseline, postintervention (14 weeks), and 1-year follow-up, parents and children completed anthropometric measures. Child physical activity data were collected at baseline and postintervention. Parents completed measures regarding child dietary consumption, child and parent screen time, and child feeding practices.
Measures
Anthropometric Variables
Child and parent height and weight were measured at baseline, 14 weeks (postintervention), and 1-year follow-up. Height was measured using a portable stadiometer, and weight was measured with a digital scale. Participants were weighed without shoes and in light clothing. Height (nearest 0.1 cm) and weight (nearest 0.1 kg) were measured twice and averaged for analyses. For children, BMI percentiles for age and sex and z-BMIs, based on the 2000 Centers for Disease Control (CDC) Growth Charts, were calculated using a SAS program developed by the CDC (Kuczmarski et al., 2002).
Dietary Intake
Children’s dietary intake was estimated from a 24-hr dietary recall collected at baseline, postintervention, and 1-year follow-up, using a combination of in-preschool meal observations and a 24-hr dietary recall obtained by parent interview, as recommended by McPherson, Hoelscher, Alexander, Scanlon, and Serdule (2002). Details of the meal observation protocol have been published previously (Fitzgibbon et al., 2011). Average daily caloric intake was estimated from the in-preschool observations and out of school recalls. Parent dietary intake was not collected.
Diet Quality
The in-school meal observation and recall were used to estimate children’s overall diet quality. All diet data were entered and processed using the Nutrition Data System for Research, 2007 (Nutrition Coordinating Center, University of Minnesota). The Healthy Eating Index (HEI)-2005 was used to estimate diet quality specifically (Guenther, Reedy, & Krebs-Smith, 2008; Miller et al., 2010). HEI-2005 measures diet quality based on compliance with the Dietary Guidelines for Americans (U.S. Department of Health and Human Services and U.S. Department of Agriculture, 2005) and considers the following food groups and nutrients: total fruit, total vegetables, dark green and orange vegetables and legumes, whole grains, total grains, milk, meat and beans, oils, saturated fat, sodium, and calories from solid fats, alcoholic beverages, and added sugars. The total HEI score is the sum of component scores with a maximum value of 100. Higher scores suggest better adherence to dietary guidelines (U.S. Department of Health and Human Services and U.S. Department of Agriculture, 2005).
Screen Time
At baseline, postintervention, and at 1-year follow-up, parents were asked to estimate the amount of time their child engaged in various forms of screen time on a typical weekday and weekend day, respectively (Borzekowski & Robinson, 2005). Screen time activities included watching television, DVDs, and videotapes, playing video games, or using a computer. Total screen time in minutes per day was calculated using a weighted average of time spent on school days (i.e., weekdays) and weekends. Parents were also asked to respond to the same questions regarding their own personal daily screen time. This measure has been previously examined for test–retest reliability on older school-age children (r = .94) (Borzekowski & Robinson, 2005; Robinson & Killen, 1995) but not in preschool-age samples. In our sample, the Cronbach’s alpha was .70 for both parents and children at baseline.
Physical Activity
The Actigraph GT1M activity monitor (ActiGraph, Pensacola, FL) was used to measure the children’s physical activity at baseline and postintervention. The ActiGraph is a small, lightweight uniaxial accelerometer designed to detect normal body motion and filter out motion from other sources. The acceleration signal is sampled 30 times per second, and signals are summed at the end of 15 s and stored in nonvolatile flash memory. Children were asked to wear the ActiGraph on a belt around the waist during waking hours for 7 days. Activity counts were downloaded from the accelerometers using ActiLife GT1M software (ActiGraph), and the resulting text files were read and analyzed using SAS for Windows v9.1 (SAS Institute Inc., Cary, NC). For each day in the record, the amount of time the accelerometer was worn was estimated. Time not worn was defined as at least 60 min with 0 activity counts, allowing for interruptions of up to two consecutive minutes with counts ≥100. Only days with 8 hr of wear were included in the main analyses, and participants with fewer than four valid days were excluded. Time spent in moderate-to-vigorous physical activity was calculated using count thresholds from a calibration study conducted with preschool children (Pate, Almeida, McIver, Pfeiffer, & Dowda, 2006); the threshold for moderate activity was 420 counts/15 s, and the threshold for vigorous was 842 counts/15 s. Minutes of moderate to vigorous physical activity (MVPA) were calculated for each day, and then averaged across all of the child’s valid days.
Child Feeding Questionnaire
The Child Feeding Questionnaire (CFQ) is a self- report measure that assesses parental beliefs, attitudes, and practices regarding child feeding. The CFQ has been widely used and validated for use with parents of children ages 2–11 years (Birch et al., 2001). We included only the three subscales related to parent feeding practices in the current study: restriction, monitoring, and pressure to eat. The internal consistencies for these subscales in our sample were 0.79 (monitoring), 0.64 (restriction), and 0.55 (pressure to eat).
Analytic Plan
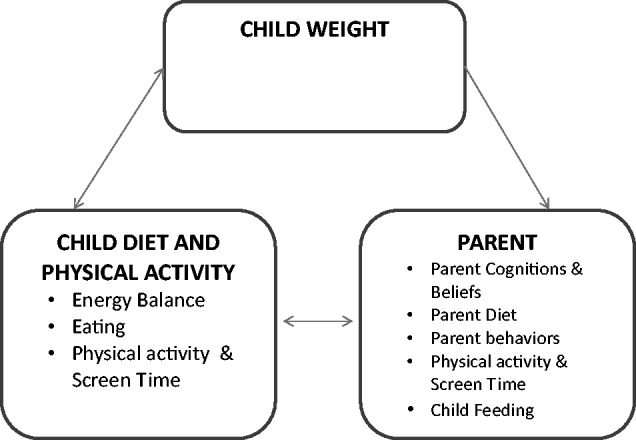
To examine the relations among changes in children’s z-BMI, diet quality, caloric intake, physical activity, screen time, and caregiver BMI, screen time, feeding practices (pressure, monitoring, and restriction), Pearson correlations, and random effects growth modeling with individually varying times of observation and path analysis were conducted for two periods (baseline to postintervention and postintervention to 1 year). This approach coupled with full information robust maximum likelihood estimation allowed for the modeling of multiple change process with missing, nested, and nonnormally distributed data. Robust estimation of standard errors takes into account both nonnormality of outcomes and nonindependence of observations owing to the nesting of study participants across classrooms. The random effects capture individual differences, in terms of random slopes (i.e., individual differences in the rates of change) and intercepts (initial values). As a necessary first step, unconditional quadratic and piecewise growth models (with residual variances fixed to zero to ensure identification) were evaluated separately for each variable of interest to characterize the nature of change. The exception to this was children’s physical activity, which was modeled as linear change because it was only assessed twice. Pending significant variability in the rates of change and initial values, factor scores from these models were exported and used with path analysis to decrease model complexity, help to maintain an appropriate classroom (cluster) to parameter ratio, and facilitate model convergence. Given the significant variability in the rates of change and baseline values across both groups, all individuals from the intervention and the comparison groups were included in the original path models tested. To rule out any potential confounding effects of group status in terms of differential prediction, exploratory follow-up and multigroup moderation analyses were conducted. They hypothesized model is presented in Figure 2.
Figure 2.
Hypothesized path model. Based on Social Cognitive Theory, and the conceptual model adapted from Skouteris and colleagues (2011), we developed the hypotheses depicted in this path model to test relations between parent and child variables. Overall, we hypothesized that parent BMI would predict child BMI, and that maladaptive parent feeding practices would predict higher child calorie intake, and, subsequently, higher child BMI. We also hypothesized that parent screen time would predict child screen time. In our analyses, we also tested paths from initial values of each variable to the change in each variable.
The goodness of fit for the path model was evaluated using the Robust Chi-Square statistic (χ2); however, because the chi-square statistic is sensitive to sample size (Hu & Bentler, 1999), the Comparative Fit Index (CFI) was also included. CFI values range from 0 to 1. Values of ≥0.90 and ≥0.95 represent an adequate and good model fit, respectively (Bollen, 1989; Hoyle & Panter, 1995). The Root Mean Square Error of Approximation (RMSEA; MacCallum, Browne, & Sugawara, 1996) statistic was also supplied as an indication of the population error variance (Browne & Cudeck, 1993). Interpretation of RMSEA values in terms of fit are as follows: good (<0.05), acceptable (0.05–0.08), marginal (0.08–0.10), and poor (>0.10). All analyses were conducted in Mplus 7.20 (Muthén & Muthén, 1998–2012).
Results
Correlations
Pearson correlations were conducted examining data collected from 587 of the 590 children participating in the HH Effectiveness Trial; three participants were missing data on at least one variable and were excluded. The average proportion of values present for each variable included in the model was 92% (SD = 8%; ranged 100–68%), with the Physical Activity variable having the lowest proportion. Greater initial child z-BMIs were associated with greater initial parent BMIs (r = .245, p < .01), and lower initial pressure to eat from parents (r = −.122, p < .01). Decreases in child’s screen time were associated with greater decreases in parent’s screen time behavior from baseline to postintervention (r = .267, p < .01).
Random Effects Growth Model Results—Baseline to 14-Weeks Postintervention
All 590 participants were included in the growth curve model analyses. Given that significant variability in all growth estimates was found (suggesting that some individuals increased, whereas others decreased), the hypothesized path model was estimated using changes from baseline to postintervention, while controlling for initial status. This model had adequate fit (χ2 = 177.041, df = 115, p < .0001; RMSEA = 0.030; CFI = 0.941); full results are presented in Table I. Regarding parent and child behavior change, changes in child screen time moved in tandem with parent screen time. Follow-up multigroup path analyses were conducted to determine whether group status moderated any of the predictive paths within the model. There were no between-group differences in relations between child and parent variables.
Table I.
Predictors of Rates of Change From Baseline to 14 Weeks After Intervention
| Predictors of rates of change | Estimate | SE | Est./SE | p |
|---|---|---|---|---|
| DV: zBMI change slope | ||||
| Caloric intake slope | 0.003 | 0.002 | 1.413 | .158 |
| Physical activity slope | 0.150 | 0.071 | 2.100 | .036 |
| Diet quality slope | 0.114 | 0.063 | 1.798 | .072 |
| Screen time slope | 0.009 | 0.006 | 1.532 | .126 |
| Parent BMI slope | −0.002 | 0.015 | −0.116 | .908 |
| Initial zBMI | −0.115 | 0.040 | −2.873 | .004 |
| DV: Caloric intake slope | ||||
| Parent restriction slope | 0.278 | 0.469 | 0.592 | .554 |
| Parent Pressure to eat slope | 0.142 | 0.274 | 0.517 | .605 |
| Parent monitoring slope | −0.456 | 0.388 | −1.174 | .240 |
| Initial caloric intake | −0.526 | 0.085 | −6.167 | .000 |
| DV: Physical activity slope | ||||
| Parent BMI slope | 0.007 | 0.013 | 0.505 | .614 |
| Initial physical activity | −0.451 | 0.086 | −5.222 | .000 |
| DV: Diet quality slope | ||||
| Parent restriction slope | −0.011 | 0.015 | −0.769 | .442 |
| Parent pressure to eat slope | 0.007 | 0.009 | 0.752 | .452 |
| Parent monitoring slope | 0.017 | 0.011 | 1.506 | .132 |
| Initial diet quality | −0.762 | 0.105 | −7.255 | .000 |
| DV: Screen time slope | ||||
| Parent screen time behavior slope | 0.125 | 0.036 | 3.475 | .001 |
| Initial screen time | −0.557 | 0.095 | −5.885 | .000 |
| DV: Parent restriction slope | ||||
| Parent BMI slope | −0.005 | 0.028 | −0.164 | .870 |
| Initial restriction | −0.577 | 0.054 | −10.724 | .000 |
| DV: Parent pressure to eat slope | ||||
| Parent BMI slope | 0.013 | 0.036 | 0.359 | .719 |
| Initial pressure to eat slope | −0.456 | 0.064 | −7.140 | .000 |
| DV: Parent monitoring slope | ||||
| Parent BMI slope | 0.024 | 0.028 | 0.847 | .397 |
| Initial parent monitoring | −0.587 | 0.108 | −5.438 | .000 |
| DV: Parent BMI slope | ||||
| Parent sedentary behavior slope | 0.005 | 0.016 | 0.328 | .743 |
| Initial parent BMI | −0.006 | 0.015 | −0.428 | .669 |
| Parent screen time with | ||||
| Initial parent sedentary behavior | −0.623 | 0.069 | −9.037 | .000 |
| Parent restriction slope with | ||||
| Parent pressure to eat slope | 0.289 | 0.059 | 4.894 | .000 |
| Parent monitoring slope | 0.283 | 0.110 | 2.567 | .010 |
| Parent pressure to eat slope with | ||||
| Monitoring slope | −0.022 | 0.093 | −0.241 | .810 |
| Initial parent BMI with | ||||
| Initial zBMI | 2.260 | 0.421 | 5.369 | .000 |
Note. BMI = body mass index; zBMI = body mass index z-score; DV = dependent variable.
Random Effects Growth Model Results—14-Weeks Postintervention to 1-Year Follow-Up
The 14-weeks postintervention to 1-year follow-up model had a marginally acceptable model fit: (χ2 = 112.429, df = 90, p = .055; RMSEA = 0.021; CFI = 0.902); full results are presented in Table II. Similar to the active treatment model, changes in child screen time continued to move in tandem with parent screen time. In terms of caloric intake, higher parental monitoring was associated with greater decreases in caloric intake over time. Follow-up multigroup path analyses were conducted to determine whether group status moderated any of the predictive paths within the postintervention to follow-up model. There were no between-group differences in relations between child and parent variables.
Table II.
Predictors of Rates of Change From 14 Weeks After Intervention to 1-Year Follow-Up
| Predictors of rate of change | Estimate | SE | Est./SE | p |
|---|---|---|---|---|
| DV: z-BMI slope 2 | ||||
| Caloric intake slope 2 | 0.000 | 0.002 | 0.106 | .916 |
| Diet quality slope 2 | 0.020 | 0.076 | 0.263 | .792 |
| Screen time slope 2 | 0.006 | 0.011 | 0.507 | .612 |
| Parent’s BMI slope 2 | 0.016 | 0.015 | 1.017 | .309 |
| Initial z-BMI | −0.051 | 0.022 | −2.261 | .024 |
| DV: Caloric intake slope 2 | ||||
| Parent restriction slope 2 | −0.530 | 0.539 | −0.983 | .326 |
| Parent pressure to eat slope 2 | −0.289 | 0.510 | −0.567 | .571 |
| Parent monitoring slope 2 | −1.114 | 0.473 | −2.352 | .019 |
| Initial caloric intake slope 2 | −0.127 | 0.055 | −2.309 | .021 |
| DV: Diet quality | ||||
| Parent restriction slope 2 | −0.012 | 0.018 | −0.653 | .514 |
| Parent pressure to eat slope 2 | 0.021 | 0.015 | 1.395 | .163 |
| Parent monitoring slope 2 | 0.000 | 0.014 | −0.028 | .978 |
| Initial diet quality | 0.116 | 0.071 | 1.641 | .101 |
| DV: Screen time | ||||
| Parent sedentary behavior slope 2 | 0.216 | 0.038 | 5.623 | .000 |
| Initial screen time | 0.010 | 0.052 | 0.200 | .842 |
| DV: Parent restriction slope 2 | ||||
| Parent BMI slope 2 | −0.010 | 0.023 | −0.428 | .669 |
| Initial restriction | 0.010 | 0.038 | 0.261 | .794 |
| DV: Parent pressure to eat slope 2 | ||||
| Parent BMI slope 2 | 0.005 | 0.038 | 0.137 | .891 |
| Initial parent pressure to eat | 0.027 | 0.030 | 0.897 | .370 |
| DV: Parent monitoring slope 2 | ||||
| Parent BMI slope 2 | 0.019 | 0.028 | 0.672 | .502 |
| Initial parent monitoring | 0.070 | 0.072 | 0.962 | .336 |
| DV: Parent BMI slope 2 | ||||
| Parent screen time slope 2 | −0.012 | 0.028 | −0.440 | .660 |
| Initial parent BMI | −0.014 | 0.008 | −1.794 | .073 |
| DV: Parent screen time slope 2 | ||||
| Initial parent sedentary behavior | 0.044 | 0.039 | 1.149 | .251 |
| Parent restriction slope 2 with | ||||
| Parent pressure to eat slope 2 | 0.092 | 0.030 | 3.049 | .002 |
| Parent monitoring to eat slope 2 | 0.051 | 0.047 | 1.100 | .271 |
| Parent pressure to eat slope 2 with | ||||
| Parent monitoring slope 2 | 0.056 | 0.050 | 1.134 | .257 |
Note. BMI = body mass index; zBMI = body mass index z-score; DV = dependent variable.
Discussion
The purpose of this study was to identify relations between parent and child variables related to weight, screen time, and feeding practices within the context of a large, school-based prevention intervention for preschool children of ethnic and racial minority groups. Although baseline parent BMI and child z-BMI were correlated, our final path model did not reveal any significant relations between change in parent BMI and child z-BMI from baseline to postintervention or from postintervention to 1-year follow-up. However, from baseline to postintervention and from postintervention to follow-up, parent and child changes in sedentary screen time moved in tandem across groups; as parent screen time decreased, so did child screen time (and vice versa). This finding is consistent with recently published cross-sectional data among young children (Carson & Janseen, 2012; Jago et al., 2014). A recent review of effective intervention strategies for reducing screen time among young children noted that more studies are needed to determine effective means to reduce screen time among preschool-aged and minority children (Schmidt et al., 2012). Our results suggest that parent and child changes in screen time are interrelated, and therefore, parent involvement may be integral in obesity- prevention programs.
In addition to the relation found between changes in child and parent screen time, higher levels of baseline child food monitoring predicted a greater calorie reduction from postintervention to 1-year follow-up. This finding is consistent with available literature (Clark, Goyder, Bissel, Blank, & Peters, 2007). Overall, young children tend to make healthier food choices when they know that their parents are monitoring their selections. However, this review of the literature noted that a limitation of this literature is a lack of studies with African-American and Latino samples. Our study adds to the literature on parental food monitoring and calorie intake among minority preschool children over the course of 1 year. Future interventions may benefit from parent education in child food monitoring (Clark et al., 2007).
Although the main purpose of this study was to explore relations between parent and child health behavior changes across treatment groups, it is of note that there were no between-group differences on any of the relations explored in the analyses. Given that children and parents in the intervention group received intervention components related to screen time and healthy eating and the comparison condition did not, this finding was somewhat surprising. However, overall, the parent component in the intervention group was limited. Parents received newsletters covering topics discussed in class, but did not receive any in-person contact. It is possible that the parent component in the intervention group was not involved enough to promote greater links between parent and child health behavior changes as compared with the control. Indeed, at 1-year postintervention, there were no significant differences in z-BMIs between groups. Kong and colleagues (2015) speculated increased parent involvement may have improved the impact of the overall intervention on child weight trajectories.
Our results should be interpreted within the context of several limitations. First, we were unable to assess relations between parent and child physical activity because we did not collect accelerometry data from the children at 1-year follow-up, and we did not collect parental physical activity at any time point. Although we could not investigate physical activity as a primary outcome, we were able to control for child physical activity in our baseline to 14-week analyses. In addition to parent physical activity, we also did not collect parent dietary intake. A second limitation is that the relations among variables may be affected by common method variance (parental and child screen time could be confounded because of a single-rater reporting on each, etc.). Additionally, HH Effectiveness was delivered in an urban environment and participants were predominantly low-income African-American children, so we cannot speculate how parent and child changes may be related in other settings with other racial/ethnic groups. Finally, the internal consistency of the pressure to eat subscale of the CFQ was in the questionable range (0.55). Future studies should consider using a multimethod approach to measuring parent feeding practices given this limitation.
Despite the limitations, this study adds to the literature by exploring relations between parent and child weight and behavior changes over the course of a preschool-based obesity prevention intervention for predominately African-American children. Our results suggest that future obesity-prevention studies consider developing innovative methods for engaging parents in treatment. The HH Effectiveness trial was primarily school-based. The effectiveness of the trial may have been further augmented with the implementation of a more intensive home-based component (Birch & Davison, 2001; Waters et al., 2011). There is evidence that parents have a significant impact on children’s eating (Birch & Fisher, 1998; Savage, Fisher, & Birch, 2007) and physical activity patterns (Golan, 2006; Irwin, He, Bouck, Tucker, & Pollett, 2005), suggesting that intervening in the home environment may also improve diet and behavior outcomes. A recent meta-analysis concluded that the most successful childhood obesity prevention interventions are school-based with home and community components (Wang et al., 2013). One challenge to home-based interventions is that the home environment is subject to various uncontrollable parental factors (e.g., work schedules, competing responsibilities). Phone coaching and/or text message interventions may provide a feasible avenue for involving parents in interventions without requiring burdensome in-person visits (Haines et al., 2013). Few studies have tested the efficacy of such interventions among parents of preschool children of racial and ethnic minority groups. Further formative research is necessary to determine the acceptability and feasibility of technology-delivered and other home-based interventions promoting parent involvement in obesity prevention programs.
Acknowledgments
We would like to thank Stephen Onufrak who wrote the SAS program we used to calculate the HEI. We would also like to thank the Chicago Public Schools Early Childhood Education Program, the families and teachers who participated in the project, the principals who supported the project, and all research staff for their time and dedication to this project.
Funding
This study was funded in part, by the National Heart, Lung and Blood Institute (R01HL081645) and the National Cancer Institute (R25CA057699).
Conflict of interest: None declared.
References
- Bandura A. (1986). Social foundations of thought and action. Englewood Cliffs, NJ: Prentice-Hall. [Google Scholar]
- Birch L. L., Davison K. K. (2001). Family environmental factors influencing the developing behavioral controls of food intake and childhood overweight. Pediatric Clinics of North America, 48, 893–907. [DOI] [PubMed] [Google Scholar]
- Birch L. L., Fisher J. O. (1998). Development of eating behaviors among children and adolescents. Pediatrics, 101, 539–549. [PubMed] [Google Scholar]
- Birch L. L., Fisher J. O., Grimm-Thomas K., Markey C. N., Sawyer R., Johnson S. L. (2001). Confirmatory factor analysis of the child feeding questionnaire: A measure of parental attitudes, beliefs, and practices about child feeding and obesity proneness. Appetite, 36, 201–210. [DOI] [PubMed] [Google Scholar]
- Bluford D., Sherry B., Scanlon K. (2007). Interventions to prevent or treat obesity in preschool aged children: A review of evaluated programs. Obesity, 15, 1356–1372. [DOI] [PubMed] [Google Scholar]
- Bollen K. A. (1989). Structural equations with latent variables. Oxford, England: John Wiley and Sons. [Google Scholar]
- Borzekowski D. L., Robinson T. N. (2005). The remote, the mouse, and the no. 2 pencil: The household media environment and academic achievement among third grade students. Archives of Pediatrics and Adolescent Medicine , 159, 607–613. [DOI] [PubMed] [Google Scholar]
- Browne M. W., Cudeck R. (1993). Alternative ways of assessing model fit. In Bollen K. A., Long J. S. (Eds.), Testing structural equation models (pp. 136–161). Newbury Park, CA: Sage. [Google Scholar]
- Campbell K., Hesketh K. (2007). Strategies which aim to positively impact on weight, physical activity, diet and sedentary behaviours in children from 0 to 5 years: A systematic review of the literature. Obesity Reviews, 8, 327–338. [DOI] [PubMed] [Google Scholar]
- Carson V., Janseen I. (2012). Associations between factors within the home setting and screen time among children 0-5 years: A cross-sectional study. BMC Public Health, 12, 539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark H. R., Goyder E., Bissel P., Blank L., Peters J. (2007). How do parents’ child-feeding behaviours influence child weight? Implications for childhood obesity policy. Journal of Public Health, 29, 132–141. [DOI] [PubMed] [Google Scholar]
- Cunningham S. A., Kramer M. R., Narayan K. M. (2014). Incidence of childhood obesity in the United States. New England Journal of Medicine, 370, 403–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Estabrooks P., Dzewaltowski. D. A., Glasgow R. E., Klesges L. M. (2003). Reporting of validity from school health promotion studies published in 12 leading journals, 1996-2000. Journal of School Health, 73, 21–28. [DOI] [PubMed] [Google Scholar]
- Fahlman M. M., McCaugtry N., Martin J., Shen B. (2010). Racial and socioeconomic disparities in nutrition behaviors: Targeted interventions needed. Journal of Nutrition Education and Behavior, 42, 10–16. [DOI] [PubMed] [Google Scholar]
- Faith M. S., Berkowitz R. I., Stallings V. A., Kerns J., Storey M., Stunkard A. J. (2004). Parental feeding attitudes and styles and child body mass index: Prospective analysis of gene-environment interaction. Pediatricks, 114, e429–e436. [DOI] [PubMed] [Google Scholar]
- Faith M. S., Kerns J. (2005). Infant and child feeding practices in childhood overweight: The role of restriction. Maternal and Child Nutrition, 1, 164–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzgibbon M. L., Stolley M. R., Dyer A. R., VanHorn L., KauferChristoffel K. (2002). A community-based obesity prevention program for minority children: Rationale and study design for Hip-Hop to Health Jr. Preventive Medicine, 34, 289–297. [DOI] [PubMed] [Google Scholar]
- Fitzgibbon M. L., Stolley M. R., Schiffer L. A., Braunschweig C. L., Gomez S. L., Dyer A. R. (2011). Hip-Hop to Health Jr. obesity prevention effectiveness trial: Postintervention results. Obesity, 19, 994–1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzgibbon M. L., Stolley M. R., Schiffer L., Van Horn L., KauferChristoffel K., Dyer A. (2005). Two-year follow-up results for Hip-Hop to Health Jr.: A randomized controlled trial for overweight prevention in preschool minority children. Journal of Pediatrics, 146, 618–625. [DOI] [PubMed] [Google Scholar]
- Golan M. (2006). Parents as agents of change in childhood obesity–from research to practice. International Journal of Pediatric Obesity, 1, 66–76. [DOI] [PubMed] [Google Scholar]
- Golley R. K., Hendrie G. A., Slater A., Corsini N. (2011). Interventions that involve parents to improve children’s weight-related nutrition intake and activity patterns- what nutrition and activity targets and behaviour change techniques are asssociated with intervention effectiveness? Obesity Reviews, 12, 114–130. [DOI] [PubMed] [Google Scholar]
- Guenther P. M., Reedy J., Krebs-Smith S. M. (2008). Development of the healthy eating index-2005. Journal of the American Dietetic Association , 108, 1896–1901. [DOI] [PubMed] [Google Scholar]
- Haines J., McDonald J., O’Brien A., Sherry B., Bottino C. J., Schmidt M. E., Taveras E. M. (2013). Health habits, happy homes: Randomized trial to improve household routines for obesity prevention among preschool-aged children. JAMA Pediatrics , 167, 1072–1079. [DOI] [PubMed] [Google Scholar]
- Harvey-Berino J., Rourke J. (2003). Obesity prevention in preschool Native-American Children: A pilot study usuing home visiting. Obesity Reviews, 11, 606–611. [DOI] [PubMed] [Google Scholar]
- Hesketh K. D., Campbell K. J. (2010). Interventions to prevent obesity in 0-5 year olds: An updated systematic review of the literature. Obesity, 18, S27–S35. [DOI] [PubMed] [Google Scholar]
- Hoyle R. H., Panter A. T. (1995). Writing about structural equation modeling. In Hoyle R. H. (Ed.), Structural equation modeling: Concepts, issues, and applications (pp. 158–176). Thousand Oaks, CA: Sage. [Google Scholar]
- Hu L., Bentler P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling, 6, 1–55. [Google Scholar]
- Irwin J. D., He M., Bouck L. M. S., Tucker P., Pollett G. L. (2005). Preschoolers' physical activity behaviours: Parents' perspectives. Canadian Journal of Public Health, 96, 299–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jago R., Thompson J. L., Sebire S. J., Wood L., Pool L., Zahra J., Lawlor D. (2014). Cross-sectional associations between screen time of parents and young children: Differences by parent and child gender and day of the week. International Journal of Behavioral Nutrition and Physical Activity, 11, 54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kong A., Buscemi J., Stolley M., Schiffer L. A., Kim Y., Braunschweig C. L., Gomez L. L., Blumstein L. B., Van Horn L., Dyer A. R., Fitzgibbon M. L. (2015). Hip Hop to Health Jr. obesity prevention effectiveness trial: 1-year post-intervention findings. American Journal of Preventive Medicine. [Google Scholar]
- Kuczmarski R. J., Ogden C. L., Guo S. S., Grummer-Strawn L. M., Flegal K. M., Mei Z., Wei R., Curtin L. R., Roche A. F., Johnson C. L. (2002). 2000 CDC growth charts for the United States: Methods and development. Vital Health Statistics, 246, 1–190. [PubMed] [Google Scholar]
- Lobstein T., Baur L., Uauy R. (2004). IASO international obesity task-force. Obesity in children and young people: A crisis in public health. Obesity Reviews, 5(Suppl 1), 4–85. [DOI] [PubMed] [Google Scholar]
- MacCallum R. C., Browne M. W., Sugawara M. (1996). Power analysis and determination of sample size for covariance structure modeling. Psychological Methods, 1, 130–149. [Google Scholar]
- McPherson S., Hoelscher D., Alexander M., Scanlon K., Serdule M. (2002). Validity and reliability of dietary assessment in school-age children. In C. Berdanier (Ed.), Handbook of nutrition and foods (pp. 495–522). New York, NY: CRC Press. [Google Scholar]
- Miller P. E., Mitchell D. C., Harala P. L., Pettit J. M., Smiciklas-Wright H., Hartman T. J. (2010). Development and evaluation of a method for calculating the Healthy Eating Index-2005 using the Nutrition Data System for Research. Public Health Nutrition,14, 306–13. [DOI] [PubMed] [Google Scholar]
- Muthén L. K., Muthén B. O. (1998–2012). Mplus user’s guide (7th ed.). Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Ogden C. L., Carroll M. D., Kit B. K., Flegal K. M. (2014). Prevalence of childhood and adult obesity in the United States, 2011-2012. Journal of the American Medical Association, 311, 806–814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olshansky S., Passaro D. J., Hershaw R. C., Layden J., Carnes B. A., Brody J., Hayflick L., Butler R. N., Allison D. B., Ludwig D. S. (2005). A potential decline in life expectancy in the United States in the 21st century. New England Journal of Medicine, 352, 1138–1145. [DOI] [PubMed] [Google Scholar]
- Pate R. R., Almeida M. J., McIver K. L., Pfeiffer K. A., Dowda M. (2006). Validation and calibration of an accelerometer in preschool children. Obesity (Silver Spring), 14, 2000–2006. [DOI] [PubMed] [Google Scholar]
- Robinson T. N., Killen J. D. (1995). Ethnic and gender differences in the relationships between television viewing and obesity, physical activity, and dietary fat intake. Journal of Health Education , 26(Suppl 2), S91–S98. [Google Scholar]
- Savage J. S., Fisher J. O., Birch L. L. (2007). Parental influence on eating behavior: Conception to adolescence. The Journal of Law, Medicine, and Ethics, 35, 22–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt M. E., Haines J., O’Brien A., McDonald J., Price S., Sherry B., Taveras E. M. (2012). Systematic review of effectiveness strategies for reducing screen time among young children. Obesity, 20, 1338–1354. [DOI] [PubMed] [Google Scholar]
- Skouteris H., McCabe M., Swinburn B., Newgreen V., Sacher P., Chadwick P. (2011). Parental influence and obesity prevention in pre-schoolers: A systematic review of interventions. Obesity Reviews, 12, 315–328. [DOI] [PubMed] [Google Scholar]
- Trost S., Sallis J., Pate R., Freedson P., Taylor W., Dowda M. (2003). Evaluating a model of parental influence on youth physical activity. American Journal of Preventive Medicine, 25, 277–282. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services and U.S. Department of Agriculture. (2005). Dietary guidelines for Americans, 2005 (6th ed.). Washington, DC: U.S. Government Printing Office. [Google Scholar]
- Wang Y., Wu Y., Wilson R. F., Bleich S., Cheskin L., Weston C., Showell N., Fawole O., Lau B., Segal J. (2013). Childhood obesity prevention programs: Comparative effectiveness review and meta-analysis. Comparative Effectiveness Review No. 115. (Prepared by the Johns Hopkins University Evidence-based Practice Center under Contract No. 290-2007-10061-I.) AHRQ Publication No. 13-EHC081-EF. Rockville, MD: Agency for Healthcare Research and Quality. Retrieved from www.effectivehealthcare.ahrq.gov/reports/final.cfm [PubMed] [Google Scholar]
- Waters E., de Silva-Sanigorski A., Hall B. J., Brown T., Campbell K. J., Gao Y., Armstrong R., Prosser L., Summerbell C. D. (2011). Interventions for preventing obesity in children. Cochrane Database of Systematic Reviews, 12, CD001871. [DOI] [PubMed] [Google Scholar]