Abstract
Background:
Despite documented age-related declines in self-reported functional status and measured physical capacity, it is unclear whether these functional indicators follow similar trajectories over time or whether the patterns of change differ by sex.
Methods:
We used longitudinal data from 687 initially nondisabled adults, aged 70 or older, from the Precipitating Events Project, who were evaluated every 18 months for nearly 14 years. Self-reported disability was assessed with a 12-item disability scale. Physical capacity was measured using grip strength and a modified version of Short Physical Performance Battery. Hierarchical linear models estimated the intra-individual trajectory of each functional indicator and differences in trajectories’ intercept and slope by sex.
Results:
Self-reported disability, grip strength, and Short Physical Performance Battery score declined over 13.5 years following nonlinear trajectories. Women experienced faster accumulation of self-reported disability, but slower declines in measured physical capacity, compared with men. Trajectory intercepts revealed that women had significantly weaker grip strength and reported higher levels of disability compared with men, with no differences in starting Short Physical Performance Battery scores. These findings were robust to adjustments for differences in sociodemographic characteristics, length-of-survival, health risk factors, and chronic-disease status.
Conclusions:
Despite the female disadvantage in self-reported disability, older women preserve measured physical capacity better than men over time. Self-reported and measured indicators should be viewed as complementary rather than interchangeable assessments of functional status for both clinical and research purposes, especially for sex-specific comparisons.
Keywords: Disability, Physical capacity, Sex differences, Trajectories
Functional status in older persons has generally been evaluated using self-reported indicators of ability to complete daily tasks, but there is increasing recognition that measured indicators of physical capacity may improve the evaluation (1). Previous studies have established the validity and predictive value of physical capacity indicators (2,3), and comparative studies have shown modest to moderate concordance between self-reported and measured indicators, without a consistent bias towards either under- or overreporting relative to measured indicators (4,5).
Because functional limitations develop over time, possibly nonmonotonically (6,7), long-term trajectories (i.e., initial level, rate, and magnitude of change) of self-reported and measured indicators can be useful outcomes in older adults. The paradoxical relationship between health and survival of women and men has been documented for a multitude of health outcomes, including self-reported disability and measured physical capacity (8). Despite surviving longer than men, women experience greater disability than men of the same age across a wide range of functional indicators, including basic activities of daily living (ADL), instrumental ADLs (IADLs), and mobility, and tend to perform worse on measured physical capacity (9). The higher burden of disability among older women is partially explained by higher incidence of disability, lower rates of recovery from disability, and lower mortality relative to men of the same age (10). However, sex differences in long-term trajectories of self-reported disability and measured physical capacity have been understudied; hence, it is still unclear (4) whether the observed sex differences in disability and physical capacity are due to higher levels of functional capacity in men (vs women), faster rates of decline in women (vs men), or a combination of both.
To address these gaps, the current study aims to evaluate sex differences in concomitant trajectories of self-reported disability and measured physical capacity over an extended period of time, while accounting for potential systematic bias due to sex differences in health status (8) and survival (6).
Methods
Study Population
We used data from the Precipitating Events Project, an ongoing panel of 754 initially nondisabled community-residing adults aged 70 or older, who were comprehensively evaluated for disability and physical capacity every 18 months for nearly 14 years (1998–2012). Study design, eligibility criteria, and response rates have been described previously (11).
Of the 754 Precipitating Events Project participants, 57 (7.6%) died and 7 (0.9%) dropped out prior to the first follow-up assessment and were excluded because longitudinal change could not be assessed. Three participants who were missing complete data on self-reported disability at baseline were also excluded, resulting in an analytic sample of 687 participants. Descriptive characteristics of excluded participants are provided in Appendix Table 1A. Over the follow-up period, 482 (70.2%) participants died over a median of 10.1 years (interquartile range 6.0–13.5); attrition among survivors was very low (11 participants; median follow-up = 4.5 years, interquartile range 1.5–9.0 years).
Data Collection
Comprehensive assessments were completed at baseline and repeated at 18-month intervals, with the exception of 126 months, for a total of 162 months (9 assessments).
Disability Assessment
Self-reported disability was assessed at each wave using the question “At the present time, do you need help from another person to (complete the task)?” Participants were evaluated for four ADLs (bathing, dressing, walking, and transferring), five IADLs (shopping, housework, meal preparation, taking medications, and managing finances), and three mobility tasks (walking one-quarter mile, walking up a flight of stairs, and lifting and carrying 10 pounds). For the main analyses, each of the 12 items was scored 0 for reported no need for (personal) help and 1 for reported need for (personal) help. A summary disability score was created (range 0–12) and then reverse-coded such that 12 = no disability and 0 = total disability.
Previous reports on assessment of self-reported functional status indicate that difficulty and dependence (i.e., need for help) represent related, but distinct concepts (12), and that pronounced sex differences exist in reporting several IADLs (13). Thus, we performed supplementary analyses using three additional scores: a difficulty score (range 0–12), assessing self-reported difficulty with performing the same 12 tasks (0 = no reported difficulty; 1= reported difficulty); a graded difficulty/dependence score (range 0–24), created by coding each of the 12 tasks as 0 for no reported difficulty or need for help, 1 for reported difficulty but not need for help, and 2 for need for help; and a score representing the sum of ADL and mobility tasks (range 0–7). The three scores were then reverse-coded such that higher scores reflect less difficulty and/or dependence.
Measurement of Upper- and Lower-extremity Capacity
Upper-extremity capacity was assessed at each wave using grip strength (14), calculated as the average of two maximal measurements out of three trials using a handheld dynamometer (Chatillon 100, Ametek Inc., Largo, FL). The raw grip strength score (in kilograms; range: 0–52) was re-scaled into a 0–12 score (higher scores denote stronger grip) for comparability with the disability and lower-extremity capacity scores.
Lower-extremity capacity was measured at each wave using a modified version of the Short Physical Performance Battery (SPPB) (3). The SPPB score is a highly reliable and responsive summary measure (15), which includes three hierarchical timed tests of repeated chair stands, short-distance walking speed, and balance. The modified version used three chair stands instead of five and a 20-foot walk with a turn instead of a 4-meter walk; for balance, the three standard maneuvers (side-by-side, semi-tandem, and tandem stands) and scoring were used. Per convention (3), a five-level summary scale ranging from 0 (unable to perform the task) to 4 (highest performance) was created separately for each test and an overall SPPB score (range: 0–12; higher scores indicate better performance) was calculated by summing the three scores. Concordance between the modified and standard SPPB was high: ICC = 0.88, 95%CI = 0.83–0.93.
Covariates
Sociodemographic characteristics included sex, age (years, at baseline), education (years completed), race (white/non-white), and living arrangement (with others/alone).
Health behaviors included smoking (non-smoker/current smoker) and alcohol use (non-drinker/drinker) recorded at baseline; body mass index calculated at each wave as [weight(kilograms)/(height)2(meters)]; and physical activity, assessed at each wave using a modified version of Physical Activity Score for the Elderly (M-PASE; range: 0–360) (16).
Health status indicators, assessed at each wave, were included because of associations with functional status (17) and to account for sex differences in morbidity (8). The sum of nine self-reported physician-diagnosed chronic diseases (hypertension, myocardial infarction, health failure, stroke, cancer, diabetes, arthritis, hip fracture, and lung disease) was calculated from individual-disease questions (absent/present). Depressive symptoms were evaluated using the short-form 11-item CES-D score (18) and a full CES-D equivalent-score (range: 0–60) was calculated according to previously described procedure (19). Cognitive functioning was assessed using the Mini-Mental State Examination score (range: 0–30) (20).
Length-of-survival was included to correct for potential mortality bias in trajectory estimation. This approach has been described in detail elsewhere (6). Briefly, for participants who died during follow-up, data were censored at the last assessment, and length-of-survival was calculated by subtracting the date-of-enrollment from the verified date-of-death. Participants alive for the 162-month evaluation were assigned a length-of-survival of 13.5 years. Length-of-survival (in years) was included as an individual-level (i.e., varying from participant to participant) covariate in the appropriate models.
Statistical Analysis
Hierarchical generalized linear models with maximum likelihood estimation (21) were used to calculate trajectories of disability, grip strength, and SPPB as a function of time. To estimate sex differences in trajectory intercept and slope, an unadjusted sex-only model (model M0 in Table 2) was tested first, followed by models incrementally adjusted for length-of-survival (model M1), and sociodemographic characteristics, health risk factors, and health status (model M2), for each of the three outcomes. Because the rate-of-change for various functional indicators may vary according to their initial level (22), slope equations adjusted for initial values were tested separately for each outcome (model M3). Finally, to test the effect of wave-to-wave changes in upper- and lower-extremity capacity on disability trajectory estimates, time-varying grip strength and SPPB score were added to the disability model (model M4).
Table 2.
Sex differences in Trajectories of Disability* and Physical Capacity† (1998–2012)
| Models‡ | M0 | M1 | M2 | M3 | M4 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| b | p Value | b | p Value | b | p Value | b | p Value | b | p Value | |
| Disability | ||||||||||
| Trajectory parameters§ | ||||||||||
| Intercept | 7.21 | <.001 | 6.66 | <.001 | 6.67 | <.001 | 7.07 | <.001 | 7.44 | <.001 |
| Female (vs male) | −0.90 | .015 | −1.41 | <.001 | −0.86 | .001 | −0.70 | .008 | −0.82 | .001 |
| Linear slope | −0.58 | <.001 | −1.06 | <.001 | −0.74 | <.001 | −0.77 | <.001 | −0.52 | <.001 |
| Female (vs male) | −0.05 | .443 | −0.09 | .115 | −0.10 | <.001 | −0.14 | .012 | −0.19 | <.001 |
| Quadratic slope | −0.03 | <.001 | −0.14 | <.001 | −0.10 | <.001 | −0.11 | <.001 | −0.09 | <.001 |
| Female (vs male) | 0.02 | .010 | 0.02 | .003 | 0.01 | .136 | 0.02 | .041 | 0.01 | .162 |
| Cubic slope | −0.004 | <.001 | −0.01 | <.001 | −0.01 | .005 | −0.01 | .001 | −0.01 | <.001 |
| Female (vs male) | 0.003 | .004 | 0.003 | .006 | 0.003 | .008 | 0.003 | .010 | 0.004 | .001 |
| Model fit | ||||||||||
| Deviance | 18806.26 | 18425.35 | 17845.20 | 17405.81 | 17810.66 | |||||
| # Parameters | 7 | 7 | 7 | 7 | 7 | |||||
| Grip strength | ||||||||||
| Trajectory parameters | ||||||||||
| Intercept | 5.71 | <.001 | 5.56 | <.001 | 6.28 | <.001 | 6.31 | <.001 | ||
| Female (vs male) | −2.24 | <.001 | −2.39 | <.001 | −2.25 | <.001 | −2.26 | <.001 | ||
| Linear slope | −0.29 | <.001 | −0.43 | <.001 | −0.30 | <.001 | −0.24 | <.001 | ||
| Female (vs male) | 0.15 | <.001 | 0.15 | <.001 | 0.16 | <.001 | 0.03 | .300 | ||
| Quadratic slope | −0.01 | .001 | −0.05 | <.001 | −0.03 | .001 | −0.07 | <.001 | ||
| Female (vs male) | −0.0001 | .960 | 0.001 | .864 | 0.001 | .765 | 0.03 | <.001 | ||
| Cubic slope | 0.001 | .372 | −0.002 | .016 | −0.001 | .609 | −0.001 | .526 | ||
| Female (vs male) | −0.001 | .018 | −0.001 | .014 | −0.002 | .003 | −0.002 | .006 | ||
| Model fit | ||||||||||
| Deviance | 13390.82 | 13207.79 | 13220.77 | 12303.14 | ||||||
| # Parameters | 7 | 7 | 7 | 7 | ||||||
| SPPB | ||||||||||
| Trajectory parameters | ||||||||||
| Intercept | 4.85 | <.001 | 4.36 | <.001 | 4.08 | <.001 | 4.04 | <.001 | ||
| Female (vs male) | −0.61 | .020 | −0.94 | <.001 | −0.41 | .066 | −0.37 | .080 | ||
| Linear slope | −0.66 | <.001 | −0.91 | <.001 | −0.67 | <.001 | −0.72 | <.001 | ||
| Female (vs male) | 0.21 | <.001 | 0.19 | <.001 | 0.16 | <.001 | 0.15 | .001 | ||
| Quadratic slope | −0.01 | .071 | −0.03 | .041 | −0.01 | .677 | −0.01 | .671 | ||
| Female (vs male) | 0.003 | .528 | 0.01 | .284 | 0.003 | .508 | 0.01 | .028 | ||
| Cubic slope | 0.003 | <.001 | 0.003 | .041 | 0.01 | <.001 | 0.01 | .002 | ||
| Female (vs male) | −0.001 | .066 | −0.001 | .102 | −0.001 | .206 | −0.002 | .064 | ||
| Model fit | ||||||||||
| Deviance | 18227.11 | 17953.60 | 17784.18 | 16828.22 | ||||||
| # Parameters | 7 | 7 | 7 | 7 | ||||||
Notes: CES-D = Center for Epidemiologic Studies Depression; MMSE = Mini-Mental State Examination; M-PASE = Modified Physical Activity Score for Elderly; SPPB = Short Physical Performance Battery.
*Disability assessed as “self-reported need for help.”
†Upper-extremity capacity assessed using grip strength and lower-extremity capacity assessed using SPPB score.
‡Models: M0, unadjusted sex-only; M1, added length-of-survival; M2, added age, race, education, living arrangements, smoking, alcohol, body mass index, M-PASE score, CES-D score, MMSE score, number of chronic diseases; M3, added baseline disability, grip strength, and SPPB scores respectively, in the corresponding equations for each slope coefficient; M4, model for disability trajectory only—added time-varying grip strength and SPPB scores at each wave.
§For each outcome, the intercept represents the estimated level of self-reported disability, SPPB, or grip strength, respectively, at mid-time point (6.75 years); the slope coefficients represent the estimated decline per year in each outcome; the gender coefficients represent the estimated difference in intercept and decline per year between women and men.
All models estimated the intercept, linear and nonlinear changes over time. Time was centered at its mean to minimize the possibility of multicollinearity when evaluating nonlinear time (t) functions. Consequently, the intercept for all the models should be interpreted as the outcome at the mid-time point (i.e., 6.75 years into the study).
Goodness-of-fit was assessed by comparing random effects (residual variance for each estimated parameter) and deviance statistics between nested models, and residuals inspection. Detailed model specification and additional statistical considerations are provided in the Supplementary Appendix. The statistical significance level was set at p < .05 (two-tailed). All analyses were performed using HLM 6.6 software (Scientific Software International, Lincolnwood, IL).
Results
Descriptive characteristics of the overall sample and according to sex are summarized in Table 1.
Table 1.
Sample Descriptive Characteristics According to Sex
| Full Sample (N = 687) | Women (N = 448) | Men (N = 239) | p Value* | |
|---|---|---|---|---|
| Mean (SD) or % | Mean (SD) or % | Mean (SD) or % | ||
| Baseline | ||||
| Disability score (0–12) | 10.8 (1.8) | 10.6 (1.9) | 11.3 (1.2) | <.001 |
| Grip strength (0–12) | 5.3 (2.0) | 4.4 (1.2) | 7.1 (1.9) | <.001 |
| SPPB score (0–12) | 6.9 (2.9) | 6.5 (2.9) | 7.7 (2.8) | <.001 |
| Age (y) | 78.2 (5.1) | 78.1 (5.2) | 78.4 (5.0) | .459 |
| White | 90.2% | 90.2% | 90.4% | .934 |
| Education (y) | 11.9 (2.9) | 11.8 (2.8) | 12.3 (3.0) | .029 |
| Lives alone | 39.7% | 48.4% | 23.0% | <.001 |
| BMI | 26.9 (5.1) | 27.2 (5.5) | 26.4 (4.2) | .049 |
| Smoker | 8.3% | 8.2% | 8.4% | .961 |
| Alcohol user | 22.2% | 15.7% | 34.3% | <.001 |
| M-PASE score (1–360) | 91.6 (57.1) | 81.7 (52.2) | 110.2 (61.2) | <.001 |
| Chronic conditions (1–9) | 1.7 (1.2) | 1.7 (1.2) | 1.7 (1.2) | .575 |
| MMSE score (0–30) | 26.8 (2.4) | 26.9 (2.4) | 26.6 (2.5) | .185 |
| CES-D (1–60) | 8.8 (8.5) | 9.8 (9.1) | 6.9 (6.8) | <.001 |
| Attrition | ||||
| Survival (years from baseline) | 8.9 (3.4) | 9.1 (3.3) | 8.4 (3.5) | .010 |
| Died | 70.2% | 68.1% | 74.1% | .103 |
Notes: BMI = body mass index; CES-D = Center for Epidemiologic Studies Depression; MMSE = Mini-Mental State Examination; M-PASE = Modified Physical Activity Score for Elderly; SPPB = Short Physical Performance Battery.
*p Values for differences between men and women.
Self-Reported Disability
The unconditional model (M0; Table 2) showed an average disability trajectory with a mid-point intercept of 7.21 (p < .001) and a declining nonlinear course, with a negative linear slope, negative quadratic slope, and negative cubic slope.
Compared with men, women started with more disability, but declined at a slightly slower rate. Adjustment for length-of-survival (M1) produced a more pronounced difference unfavorable to women in disability trajectory intercept and sex differences in rate-of-decline similar to those observed in the unconditional model. Subsequent adjustments (M2 and M3) for differences in relevant covariates and initial disability scores slightly attenuated the sex gradient in disability intercept but showed an even more accelerated decline in scores in women compared with men.
Finally, model M4 showed a modest attenuation of the rate-of-decline compared with M3, indicating that the decline in overall disability scores is only marginally explained by declines in upper- and lower-extremity capacity. Further, M4 (compared with M3) indicated a higher level of disability and faster decline in disability score among women compared with men after adjustment for grip strength and SPPB score.
Grip Strength
The unconditional model (M0) showed that, on average, grip strength declined following a quadratic trajectory with a mid-point intercept of 5.71 (p < .001), a negative linear slope and a negative quadratic slope. Additionally, this model showed a significantly lower intercept and slower rate-of-decline in women compared with men.
Intercept differences between women and men were robust to adjustments for differences in survival, socioeconomic characteristics, health risk factors, and health status. Control for initial level of grip strength in model M3 attenuated, but did not eliminate, the slower rate-of-decline (i.e., positive sex slope coefficients) in grip strength observed in women.
SPPB Score
The unconditional model (M0) showed an average SPPB trajectory with a mid-point intercept of 4.85 (p < .001) and a declining nonlinear course, with a negative linear slope, a nonsignificant quadratic slope and a small, positive cubic slope.
Women had a lower SPPB intercept but a slower rate-of-decline than men. These results were largely unchanged after adjusting for length-of-survival (M1). After adjustment for covariates (models M2 and M3), the sex difference in intercept became nonsignificant, whereas the sex difference in linear decline was preserved, denoting a slower decline in lower-extremity capacity in women compared with men.
Self-Reported Difficulty, Difficulty/Dependence, and ADL/Mobility Scores
Appendix Tables 2A and 3A provide the complete results from these supplementary models. For all the scores, the fully adjusted models showed declining nonlinear trajectories and sex differences similar to those revealed in the main analyses—women reported more difficulty and difficulty/dependence with completing tasks (i.e., lower trajectory intercepts) and declined at a faster rate compared with men.
Discussion
This study examined sex differences in long-term concomitant trajectories of self-reported disability and measured physical capacity in a cohort of community-dwelling older adults. Our results indicate that disability and physical capacity decline following distinct nonlinear trajectories and that women decline faster in their self-reported function, but preserve measured upper- and lower-extremity physical capacity better than men.
Prior studies have suggested that measured indicators may offer better assessments of functional status in older adults, and thus they should either replace or supplement self-reported information (1). However, an inconsistent association between self-reported and measured indicators of functioning has been found, ranging from weak (5) to moderate or strong (9,23,24), as well as large residual unexplained self-reported disability after accounting for matched standardized tests of measured function (4,24,25). In the current study, although all three indicators declined during nearly 14 years of observation following a nonlinear course, the trajectory of disability was only modestly altered by wave-to-wave changes in both grip strength and SPPB scores.
There are at least two potential explanations for this finding. First, disability and physical capacity may assess different functional domains, with disability reflecting a mismatch between the individuals’ needs or expectations for integration in their own living environment (26), whereas grip strength and SPPB reflect a combination of muscle strength and other physiological processes (i.e., balance, neurological, and vascular function) measured in quasi-laboratory settings. This explanation is supported by studies showing that individuals reporting optimal function (i.e., no disability) may score poorly on measured lower-extremity capacity (27) and conversely, individuals without measurable deficits in upper- or lower-extremity capacity may report substantial ADL/IADL disability (28). Second, other resources, such as activity accommodations, environmental modifications, or psychological coping, may differentially assist individuals in mitigating increases in disability, and thus may explain the dissociation between trajectories of disability and declines in physical capacity. Our results suggest that self-reported disability and measured physical capacity should be viewed as complementary, rather than interchangeable or superior/inferior (versus each other) means of assessing functional status.
Our study found that women start with more disability and report more rapid declines in function compared with men. This is consistent with findings from population-based and clinical studies (10,29) across different ages, races/ethnicities, or chronic health conditions, and when different self-report instruments were used. This gradient could be explained by a true surplus of disability in women (due to a higher incidence and prolonged duration of disability compared with men) (29), more transitions from trajectories of no/low disability to trajectories of high disability among women (10), incomplete adjustment for confounding factors (30), or reporting bias (9). Our results were robust to adjustments for many known and potential confounders, such as differences in survival and health status, and were even more pronounced when accounting for the starting level of disability.
The role of sex bias in disability reporting, in particular overreporting among women and/or underreporting among men, has been investigated, often by comparing self-reports of general or task-specific function with a matched measured indicator (9). The assumption underlying this type of accuracy assessment is that self-reported disability and physical capacity test the same functional phenomenon under similar conditions, and thus a mismatch between the two represents over- or underreporting of an objective state. Because mis-reporting is unlikely to change over time, the differences in rate-of-decline observed in the current study cannot be easily explained by sex bias in reporting. Instead, sex differences in trajectories of disability and physical capacity might be explained by the distinct functional demands faced by women and men in their daily life and reliance on different mechanisms to alleviate these demands or compensate for loss of functional/physiological abilities (4,31). Our results showing that the inclusion of time-varying grip strength and SPPB increased the sex gradient in self-reported disability suggest that changes in physical capacity have distinct associations with changes in disability in women versus men.
This study finds that despite faster declines in self-reported disability, women preserve both upper- and lower-extremity capacity better than men, suggesting that the sex-specific differences in physical capacity levels may diminish and eventually reverse among longer-surviving older adults. Other investigators have reported a slower rate-of-decline in isometric and isokinetic muscle strength, as well as in muscle mass among women compared with men (32). In our study, the annual declines were slower in women than men by 13% for grip strength (~0.03 units less decline per year compared with ~0.24 units per year decline in men) and by 21% for SPPB score (~0.15 SPPB units less decline per year compared with ~0.72 units per year decline in men). Although these differences are smaller than those reported in other studies (perhaps due to differences in participants’ age and health status), they are nevertheless substantial. Based on previously developed criteria (33), women may accumulate an “advantage” in lower-extremity capacity over men corresponding to a small meaningful loss (0.5 units difference in SPPB; equivalent to the loss of one flight of stairs in climbing ability or one block in walking ability) in the span of ~4 years and to substantial meaningful loss (1.0 unit difference in SPPB; equivalent to the loss of two flights of stairs in climbing ability or two blocks in walking ability) in the span of ~7 years (33). Our analyses accounted for multiple factors underlying sex differences in physical capacity (30) and for wave-to-wave changes in factors expected to show variability in old age (e.g., increase in number of chronic conditions or declines in mental status). However, the role of body composition/sarcopenia, inflammation, hormonal status, and various psychological resources remains to be investigated.
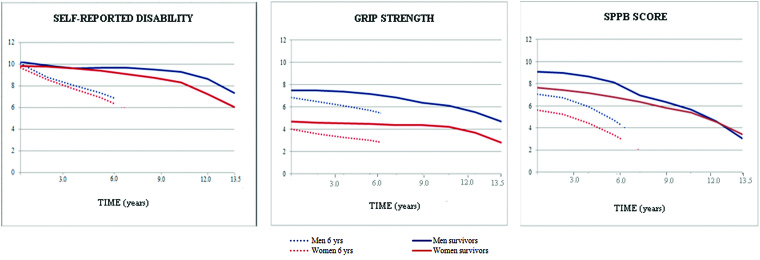
Our analytical strategy also adjusted for differences in length-of-survival. Failure to adjust for nonrandom missingness due to differential survival could result in biased trajectory estimates and/or sex difference coefficients (6). As shown in Figure 1, individuals who die sooner experience a more precipitous decline in function prior to death, whereas individuals who survive longer experience a slower decline in function and also accumulate a higher burden of disability (10,29). Additionally, because physically frail individuals were oversampled and high performers may decline faster than low performers (22), we controlled for initial values when estimating the rate-of-change in each outcome.
Figure 1.
Trajectories of disability* and physical capacity† by sex and length-of-survival (1998–2012). Dotted lines show estimated trajectories for participants who died after 6 years of follow-up. Continuous lines show estimated trajectories for participants who were alive at last assessment. *Disability assessed as “self-reported need for help.” †Upper-extremity capacity assessed using grip strength and lower-extremity capacity assessed using Short Physical Performance Battery (SPPB) score.
Several limitations deserve consideration. First, disability and lower-extremity capacity were assessed using composite scores, so we cannot exclude the possibility that individual functional score components evolve following trajectories that differ from those identified here or have distinct associations with sex. Second, because data were not suitable for age-based analyses (34), all trajectories were estimated as a function of time with control for age-at-baseline to minimize age-cohort confounding. Thus, the results do not represent the effect of age on self-reported disability and physical capacity, but rather the evolution of these measures over time in this specific age group. Lastly, the results may not be generalizable to the entire older population because our participants were selected from a single health plan in a small urban area. However, the demographic characteristics of our sample are similar to those of the entire U.S. population, with the exception of racial/ethnic representation (10).
In conclusion, this study provides new insights, by showing that self-reported functional status and measured physical capacity follow distinct declining courses over time, and that women report faster accumulating disability but preserve upper- and lower-extremity capacity better than men. These findings make a compelling argument for the use of self-reported and measured indicators as complementary rather than interchangeable assessments of functional status for both clinical and research purposes, especially for sex-specific comparisons.
Supplementary Material
Please visit the article online at http://gerontologist.oxfordjournals.org/ to view supplementary material.
Funding
This study was supported in part by the National Institute on Aging (T32 AG019134 and R37AG17560), the Claude D. Pepper Older Americans Independence Centers at University of Michigan (AG-024824) and Yale University School of Medicine (P30AG021342), and Michigan Institute for Clinical and Health Research (UL1TR000433). Dr. Gill is the recipient of an Academic Leadership Award (K07AG043587) from the National Institute on Aging.
Supplementary Material
Acknowledgments
We thank Denise Shepard, BSN, MBA, Andrea Benjamin, BSN, Barbara Foster, and Amy Shelton, MPH for assistance with data collection; Wanda Carr and Geraldine Hawthorne, BS, for assistance with data entry and management; Peter Charpentier, MPH, for design and development of the study database and participant tracking system; Joanne McGloin, MDiv, MBA, for leadership and advice as the Project Director; and our participants for sharing information about their health and function over the past 17 years.
References
- 1. Cesari M, Kritchevsky SB, Newman AB, et al. Added value of physical performance measures in predicting adverse health-related events: results from the Health, Aging and Body Composition Study. J Am Geriatr Soc.2009;57:251–259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. den Ouden ME, Schuurmans MJ, Arts IE, van der Schouw YT. Physical performance characteristics related to disability in older persons: a systematic review. Maturitas. 2011;69:208–219. [DOI] [PubMed] [Google Scholar]
- 3. Guralnik JM, Simonsick EM, Ferrucci L, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol A Biol Sci Med Sci.1994;49:85–94. [DOI] [PubMed] [Google Scholar]
- 4. Daltroy LH, Larson MG, Eaton HM, Phillips CB, Liang MH. Discrepancies between self-reported and observed physical function in the elderly: the influence of response shift and other factors. Soc Sci Med. 1999;48:1549–1561. [DOI] [PubMed] [Google Scholar]
- 5. Hoeymans N, Feskens EJ, van den Bos, Geertrudis AM, Kromhout D. Measuring functional status: cross-sectional and longitudinal associations between performance and self-report. J Clin Epidemiol. 1996;49:1103–1110. [DOI] [PubMed] [Google Scholar]
- 6. Botoseneanu A, Allore HG, Gahbauer EA, Gill TM. Long-term trajectories of lower extremity function in older adults: estimating gender differences while accounting for potential mortality bias. J Gerontol A Biol Sci Med Sci. 2013;68:861–868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Frederiksen H, Hjelmborg J, Mortensen J, McGue M, Vaupel JW, Christensen K. Age trajectories of grip strength: cross-sectional and longitudinal data among 8,342 Danes aged 46 to 102. Ann Epidemiol. 2006;16:554–562. [DOI] [PubMed] [Google Scholar]
- 8. Arber S, Cooper H. Gender differences in health in later life: the new paradox? Soc Sci Med. 1999;48:61–76. [DOI] [PubMed] [Google Scholar]
- 9. Merrill SS, Seeman TE, Kasl SV, Berkman LF. Gender differences in the comparison of self-reported disability and performance measures. J Gerontol A Biol Sci Med Sci. 1997;52:M19–M26. [DOI] [PubMed] [Google Scholar]
- 10. Gill TM, Gahbauer EA, Lin H, Han L, Allore HG. Comparisons between older men and women in the trajectory and burden of disability over the course of nearly 14 years. J Am Med Dir Assoc. 2013;14:280–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Gill TM, Desai MM, Gahbauer EA, Holford TR, Williams CS. Restricted activity among community-living older persons: incidence, precipitants, and health care utilization. Ann Intern Med. 2001;135:313–321. [DOI] [PubMed] [Google Scholar]
- 12. Gill TM, Robison JT, Tinetti ME. Difficulty and dependence: two components of the disability continuum among community-living older persons. Ann Intern Med. 1998;128:96–101. [DOI] [PubMed] [Google Scholar]
- 13. Murtagh KN, Hubert HB. Gender differences in physical disability among an elderly cohort. Am J Public Health. 2004;94:1406–1411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Rantanen T, Guralnik JM, Foley D, et al. Midlife hand grip strength as a predictor of old age disability. JAMA. 1999;281:558–560. [DOI] [PubMed] [Google Scholar]
- 15. Ostir GV, Volpato S, Fried LP, Chaves P, Guralnik JM. Reliability and sensitivity to change assessed for a summary measure of lower body function: results from the Women’s Health and Aging Study. J Clin Epidemiol. 2002;55:916–921. [DOI] [PubMed] [Google Scholar]
- 16. Washburn RA, McAuley E, Katula J, Mihalko SL, Boileau RA. The physical activity scale for the elderly (PASE): evidence for validity. J Clin Epidemiol. 1999;52:643–651. [DOI] [PubMed] [Google Scholar]
- 17. Tas U, Verhagen AP, Bierma-Zeinstra SM, Odding E, Koes BW. Prognostic factors of disability in older people: a systematic review. Br J Gen Pract. 2007;57:319–323. [PMC free article] [PubMed] [Google Scholar]
- 18. Kohout FJ, Berkman LF, Evans DA, Cornoni-Huntley J. Two shorter forms of the CES-D depression symptoms index. J Aging Health.1993;5:179–193. [DOI] [PubMed] [Google Scholar]
- 19. Penninx BW, Guralnik JM, Ferrucci L, Simonsick EM, Deeg DJ, Wallace RB. Depressive symptoms and physical decline in community-dwelling older persons. JAMA. 1998;279:1720–1726. [DOI] [PubMed] [Google Scholar]
- 20. Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. [DOI] [PubMed] [Google Scholar]
- 21. Raudenbush SW, Bryk AS. Hierarchical Linear Models: Applications and Data Analysis Methods. 2nd ed Thousand Oaks, CA: Sage Publications;2002. [Google Scholar]
- 22. Onder G, Penninx BWJH, Lapuerta P, et al. Change in physical performance over time in older women. J Gerontol A Biol Sci Med Sci.2002;57:289–293. [DOI] [PubMed] [Google Scholar]
- 23. Guralnik JM, Ferrucci L, Pieper CF, et al. Lower extremity function and subsequent disability. J Gerontol A Biol Sci Med Sci.2000;55:221–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Beauchamp MK, Jette AM, Ward RE, et al. Predictive validity and responsiveness of patient-reported and performance-based measures of function in the Boston RISE study. J Gerontol A Biol Sci Med Sci. 2015;70:616–622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Mendes de Leon CF, Guralnik JM, Bandeen-Roche K. Short-term change in physical function and disability: The Women’s Health and Aging Study. J Gerontol B Psychol Sci Soc Sci.2002;57:S355–65. [DOI] [PubMed] [Google Scholar]
- 26. Verbrugge LM, Jette AM. The disablement process. Soc Sci Med. 1994;38:1–14. [DOI] [PubMed] [Google Scholar]
- 27. Ferrucci L, Penninx BW, Leveille SG, et al. Characteristics of nondisabled older persons who perform poorly in objective tests of lower extremity function. J Am Geriatr Soc. 2000;48:1102–1110. [DOI] [PubMed] [Google Scholar]
- 28. Kivinen P, Sulkava R, Halonen P, Nissinen A. Self-reported and performance-based functional status and associated factors among elderly men. J Clin Epidemiol.1998;51:1243–1252. [DOI] [PubMed] [Google Scholar]
- 29. Hardy SE, Allore HG, Guo Z, Gill TM. Explaining the effect of gender on functional transitions in older persons. Gerontology. 2008;54:79–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Louie GH, Ward MM. Sex disparities in self-reported physical functioning: true differences, reporting bias, or incomplete adjustment for confounding? J Am Geriatr Soc. 2010;58:1117–1122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Leveille S, Resnick H, Balfour J. Gender differences in disability: evidence and underlying reasons. Aging Clin Exp Res.2000;12:106–112. [DOI] [PubMed] [Google Scholar]
- 32. Goodpaster BH, Park SW, Harris TB, et al. The loss of skeletal muscle strength, mass, and quality in older adults: the health, aging and body composition study. J Gerontol A Biol Sci Med Sci. 2006;61:1059–1064. [DOI] [PubMed] [Google Scholar]
- 33. Perera S, Mody SH, Woodman RC, Studenski SA. Meaningful change and responsiveness in common physical performance measures in older adults. J Am Geriatr Soc. 2006;54:743–749. [DOI] [PubMed] [Google Scholar]
- 34. Mendes de Leon CF. Aging and the elapse of time: a comment on the analysis of change. J Gerontol B Psychol Sci Soc Sci.2007;62:198–202. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.