The double-blind, randomized, placebo-controlled study was done to determine if a single administration of laninamivir octanoate was superior to a placebo in preventing influenza, from the standpoint of the proportion of participants with clinical influenza within 10 days after exposure.
Keywords: laninamivir, neuraminidase inhibitor, influenza, prophylaxis, post-exposure
Abstract
Background. A single administration of laninamivir octanoate, a long-acting neuraminidase inhibitor, has been proven to be effective in the treatment of influenza but not for post-exposure prophylaxis.
Methods. We conducted a double-blind, multicenter, randomized, placebo-controlled study to determine if a single administration of laninamivir octanoate 40 mg was superior to placebo for post-exposure prophylaxis. Eligible participants who had cohabited with an influenza patient within 48 hours of symptom onset were randomly assigned (1:1:1) to 1 of 3 groups: 40 mg of laninamivir octanoate single administration (LO-40SD), 20 mg of laninamivir octanoate once daily for 2 days (LO-20TD), or placebo. The primary efficacy endpoint was the proportion of participants who developed clinical influenza (defined as influenza virus positive, an axillary temperature >37.5°C, and at least 2 symptoms) over a 10-day period.
Results. A total of 803 participants were enrolled, with 801 included in the primary analysis. The proportions of participants with clinical influenza were 4.5% (12/267), 4.5% (13/269), and 12.1% (32/265) in the LO-40SD, LO-20TD, and placebo groups, respectively. A single administration of laninamivir octanoate 40 mg significantly reduced the development of influenza compared with placebo (P = .001). The relative risk reductions compared with the placebo group were 62.8% and 63.1% for the LO-40SD and LO-20TD groups, respectively. The incidence of adverse events in the LO-40SD group was similar to that of the LO-20TD and placebo groups.
Conclusions. A single administration of laninamivir octanoate was effective and well tolerated as post-exposure prophylaxis to prevent the development of influenza.
Clinical Trials Registration. JapicCTI-142679.
Close contact with an influenza patient increases the risk of subsequent infection. In such cases, antiviral chemoprophylaxis should be considered for persons at high risk from serious illness or death related to influenza (the elderly, those with chronic respiratory illness or metabolic disorders including diabetes mellitus, chronic heart disease, and immunodeficiency) [1, 2].
A single administration of laninamivir octanoate, a long-acting neuraminidase inhibitor, has been demonstrated to be an effective treatment for influenza [3–5], while oseltamivir and zanamivir need repeated administration, twice daily for 5 days. In Japan, laninamivir octanoate has been used widely not only because of its high level of efficacy and safety but also because of its convenience [6–8].
For the post-exposure prophylaxis of influenza, the inhalation of 20 mg of laninamivir octanoate once daily for 2 or 3 days effectively prevented the development of influenza through household contacts in a study conducted during the 2011–2012 influenza season [9]. However, it was not demonstrated that a single inhalation of laninamivir octanoate was effective for post-exposure prophylaxis. In a study conducted during the 2009 influenza pandemic season, the inhalation of 20 or 40 mg of laninamivir octanoate once a week reduced the proportion of patients who developed influenza (relative risk reduction [RRR] compared with placebo, 45.8% and 43.2%, respectively), but the differences with placebo were not significant [10]. A pharmacokinetics finding that a relatively high laninamivir concentration persisted in the lungs for 10 days after a single inhalation [11] suggested that a single inhalation of laninamivir octanoate may be effective for post-exposure prophylaxis. This study was conducted to evaluate the efficacy of a single inhalation of 40 mg of laninamivir octanoate as post-exposure prophylaxis for household contacts.
PATIENTS AND METHODS
Study Design and Oversight
This study was a multicenter, double-blind, randomized, placebo-controlled study. It was conducted at 50 primary care clinics in Japan between November 2014 and March 2015. The protocol and accompanying documents are available with the full text of this article at http://cid.oxfordjournals.org. The protocol was reviewed and approved by all applicable ethics and regulatory committees and formulated in accordance with the Declaration of Helsinki and Good Clinical Practice guidelines [12]. All index patients and participants provided written informed consent.
Study Population
Eligible participants were family members who had cohabited with the index patient within 48 hours of symptom onset. Participants were enrolled in the study if they were found not to have influenza, had an axillary temperature ≤36.9°C, had no influenza-like symptoms, and were aged ≥10 years at the time of enrollment. The main exclusion criteria were as follows: other family members in addition to the index patient infected before completing the enrollment process; history of hypersensitivity to neuraminidase inhibitors; treatment with a corticosteroid or other immunosuppressant; or treatment with a neuraminidase inhibitor within the previous 4 weeks. Pregnant women, lactating women, and women who wished to become pregnant during the study period were also excluded. The index patient was the first household member infected with influenza A or B virus in the 2014–2015 influenza season. The infection of the index patient was diagnosed using a rapid influenza antigen detection test. The protocol for the treatment of the index patients was standardized to exclude any possible influence on the efficacy evaluation of the study drug. The index patients, except for teenagers, were treated with oseltamivir; teenagers were treated with zanamivir because a regulatory advisory had been issued in Japan to restrict oseltamivir use in children aged 10–19 years because of safety concerns in relation to abnormal behavior.
Randomization and Blinding
Participants were randomly assigned to 1 of 3 treatments in a 1:1:1 ratio on an individual basis. The treatment groups were as follows: 40 mg of laninamivir octanoate, single administration (40SD); 20 mg of laninamivir octanoate, once daily for 2 days (20TD); and placebo. The 40SD group was treated with 40 mg of laninamivir octanoate on day 1 and with placebo on day 2. The 20SD group was treated with 20 mg of laninamivir octanoate on days 1 and 2, with placebo given as the second administration on both days. The placebo group was likewise treated with placebo administered twice on days 1 and 2. Laninamivir octanoate or an identically packaged placebo, both containing lactose as the base excipient, was administrated by self-activated inhalation. A computer-generated block random allocation sequence was provided by Bell Medical Solutions Inc. (Tokyo, Japan) and was stratified according to virus type, determined by a rapid influenza antigen detection test, of the index patient and the participant′s influenza vaccination status in the 2014–2015 influenza season. If the eligibility of the participant was confirmed, the investigator accessed the interactive web response system and was notified of the allocation number of the test drug, which was individually packaged and numbered. The participants, index patients, investigators, and study personnel were blinded to the group assignment throughout the study.
Study Procedures
For all index patients, nasopharyngeal swabs were taken on day 1 for the detection of influenza virus. For all participants, nasopharyngeal swabs were taken on days 1, 3, and 11. When a participant developed a temperature of at least 37.5°C or another symptom (headache, myalgia/arthralgia, fatigue, chills/sweats, nasal symptoms, sore throat, and cough) between day 1 and day 10, they were requested to visit the study site as soon as possible, where swabs were obtained for the detection of influenza virus. Participants who were diagnosed with influenza virus infection at this visit were provided with appropriate treatment and did not receive any subsequent doses of the test drugs. Participants recorded their axillary temperature and the severity of their symptoms (headache, myalgia/arthralgia, fatigue, chills/sweats, nasal symptoms, sore throat, and cough) twice daily from day 1 to day 11. The severity of each symptom was graded into 4 categories (0, absent; 1, mild; 2, moderate; 3, severe). For the efficacy outcomes, the severity categories 2 and 3 were defined as the presence of the symptom. Hematology, blood chemistry, and urinalysis were performed on days 1 and 11 for the safety assessment.
Laboratory Virological Testing
Each swab was placed in a sample tube containing viral transport medium and transferred to a test laboratory. Influenza virus was confirmed by determining the influenza type and subtype by reverse transcriptase-polymerase chain reaction with specific primers designed from the hemagglutinin sequences of the influenza seasonal influenza A(H1N1), influenza A(H3N2), and influenza B viruses in accordance with the manual published by the National Institute of Infectious Diseases of Japan [13]. The specific primers for influenza A(H1N1)pdm09 were designed by making a minor modification to the method described in the manual published by the Centers for Disease Control and Prevention [14]. Laboratory virological tests were performed at LSI Medience Corporation (Tokyo, Japan).
Efficacy Outcomes
The primary endpoint was the proportion of participants who developed clinical influenza between day 1 and day 11. Clinical influenza was defined as influenza virus positive, an axillary temperature >37.5°C, and at least 2 symptoms with a score 2 or 3. The secondary endpoints were symptomatic influenza, asymptomatic influenza, and influenza infection. Symptomatic influenza was defined as influenza virus positive and an accompanying axillary temperature >37.5°C or at least 1 symptom with a score 2 or 3. Asymptomatic influenza was defined as influenza virus positive, but without an axillary temperature >37.5°C or any symptoms with a score 2 or 3. Influenza infection was defined as laboratory-confirmed influenza, regardless of axillary temperature or symptom status.
Statistical Analyses
The sample size was calculated on the basis of the assumption that the proportion of participants with clinical influenza would be 3% for the laninamivir octanoate groups and 10% for the placebo group, based on previous prophylaxis studies of laninamivir octanoate and oseltamivir [9, 10, 15]. On this basis, 250 participants in each group were required to achieve an 80% power to detect the superiority of laninamivir octanoate over the placebo.
In the efficacy analysis, the full analysis set (FAS) based on the intention-to-treat principle was defined as the primary analysis set. Additional analyses were conducted for FAS index-infected (FASII) participants and FAS index-infected virus-negative at baseline (FASIINAB) participants. FASII was defined as participants in the FAS whose related index patient was confirmed to be positive for influenza virus at baseline on day 1. FASIINAB was defined as participants in the FAS who were negative for the influenza virus at baseline on day 1 and whose related index patient was confirmed to be positive for influenza virus at baseline on day 1. The safety analysis included all participants who received at least 1 dose of the study drug and who underwent at least 1 safety assessment. All analyses were performed using SAS System Release 9.2 (SAS Institute). All reported P values were 2-sided with a level of significance of P < .05.
The primary analysis was to compare the LO-40SD group and placebo group using the Fisher exact test with respect to the proportion of participants who developed clinical influenza. The LO-20TD group was also compared with the placebo group using the same method as the secondary analysis. We also calculated the RRR compared with the placebo and the corresponding 95% confidence interval (CI). Symptomatic influenza, asymptomatic influenza, and laboratory-confirmed influenza infection were analyzed as the secondary endpoints in the same manner as for the primary endpoint. Additionally, we explored the consistency of the treatment effect on the primary endpoint in the prespecified subgroups.
This study is registered with JapicCTI (study number JapicCTI- 142679).
RESULTS
Study Population
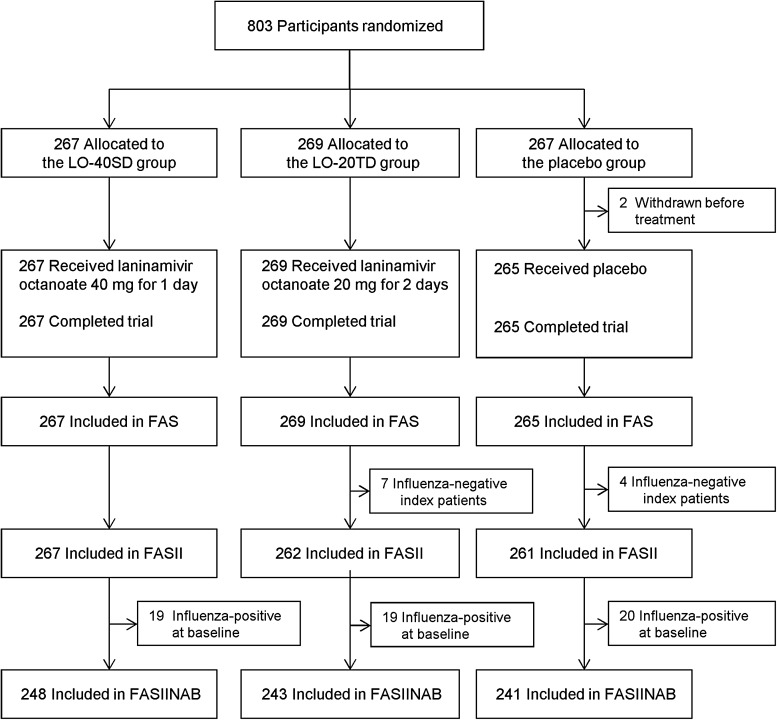
A total of 803 participants were enrolled in the study (Figure 1). Of these, 2 who discontinued before receiving treatment were excluded from all analyses. A total of 801 participants were included in the FAS (267, LO-40SD; 269, LO-20TD; 265, placebo). Of these, the FASII and FASIINAB consisted of 790 and 732 participants, respectively. The baseline characteristics of participants and index patients were well balanced among the 3 FAS groups. Most of the participants were aged 30–49 years and a parent of the index patient. Among the participants, 37.5%–38.1% were vaccinated in the 2014–2015 influenza season (Table 1). More than 1 participant could be enrolled for each index patient. Of the 687 index patients, 584 were associated with 1 participant, 92 with 2 participants, and 11 with 3 participants in the FAS. Among all index patients, 670 were infected with the influenza A(H3N2) virus, 6 with influenza B, and 2 with influenza A(H1N1)pdm09.
Figure 1.
Participant flow chart. A total of 801 participants were included in the safety analysis set (267 participants in the LO-40SD group, 269 in the LO-20TD group, and 265 in the placebo group). More than 1 participant could be enrolled for each index patient. In this case, the index patient was counted once for each household contact who was enrolled. In fact, 687 index patients (the full analysis set [FAS]) were enrolled. Abbreviations: FASII, the full analysis set, index-infected; FASIINAB, the full analysis set, index-infected virus-negative at baseline; LO-20TD, 20 mg of laninamivir octanoate administered once daily for 2 days; LO-40SD, 40 mg of laninamivir octanoate, single administration.
Table 1.
Demographic and Baseline Characteristics—the Full Analysis Set
| Characteristic | LO-40SD (N = 267) | LO-20TD (N = 269) | Placebo (N = 265) |
|---|---|---|---|
| Participants (household contacts) | |||
| Age | |||
| Mean ± SD, y | 36.2 ± 11.9 | 34.5 ± 10.5 | 35.3 ± 11.1 |
| Group, no. (%) | |||
| 10–14 | 29 (10.9) | 33 (12.3) | 29 (10.9) |
| 15–19 | 6 (2.2) | 7 (2.6) | 4 (1.5) |
| 20–29 | 14 (5.2) | 10 (3.7) | 18 (6.8) |
| 30–39 | 101 (37.8) | 124 (46.1) | 118 (44.5) |
| 40–49 | 100 (37.5) | 91 (33.8) | 88 (33.2) |
| 50–59 | 11 (4.1) | 4 (1.5) | 6 (2.3) |
| ≥ 60 | 6 (2.2) | 0 (0.0) | 2 (0.8) |
| Sex, no. (%) | |||
| Female | 237 (88.8) | 241 (89.6) | 235 (88.7) |
| Male | 30 (11.2) | 28 (10.4) | 30 (11.3) |
| Time to first dose after onset of symptoms in the index patient | |||
| Mean ± SD, hours | 20.6 ± 10.6 | 22.6 ± 12.0 | 21.9 ± 11.5 |
| Group, no. (%) | |||
| < 24 | 180 (67.4) | 159 (59.1) | 152 (57.4) |
| ≥ 24 | 87 (32.6) | 110 (40.9) | 113 (42.6) |
| Vaccinated in current season, no. (%) | |||
| No | 166 (62.2) | 168 (62.5) | 164 (61.9) |
| Yes | 101 (37.8) | 101 (37.5) | 101 (38.1) |
| Relationship to the index patient, no. (%) | |||
| Parent | 223 (83.5) | 227 (84.4) | 231 (87.2) |
| Sibling | 32 (12.0) | 37 (13.8) | 33 (12.5) |
| Index patientsa | |||
| Age | |||
| Mean ± SD, y | 8.3 ± 6.8 | 8.2 ± 6.4 | 8.2 ± 6.3 |
| Group, no. (%) | |||
| 0–4 | 59 (22.1) | 58 (21.6) | 54 (20.4) |
| 5–9 | 124 (46.4) | 124 (46.1) | 122 (46.0) |
| 10–14 | 69 (25.8) | 78 (29.0) | 79 (29.8) |
| 15–19 | 7 (2.6) | 3 (1.1) | 6 (2.3) |
| 20–29 | 3 (1.1) | 1 (0.4) | 1 (0.4) |
| 30–39 | 1 (0.4) | 2 (0.7) | 0 (0.0) |
| 40–49 | 3 (1.1) | 2 (0.7) | 0 (0.0) |
| 50–59 | 0 (0.0) | 0 (0.0) | 2 (0.8) |
| ≥ 60 | 1 (0.4) | 1 (0.4) | 1 (0.4) |
| Sex, no. (%) | |||
| Female | 113 (42.3) | 131(48.7) | 123 (46.4) |
| Male | 154 (57.7) | 138(51.3) | 142 (53.6) |
| Rapid diagnostic test, no. (%) | |||
| Positive | 267 (100.0) | 269 (100.0) | 265 (100.0) |
| Laboratory-confirmed influenza infection, no. (%) | |||
| Virus type and subtype, no. (%) | |||
| A/H1N1pdm09 | 0 (0.0) | 1 (0.4) | 1 (0.4) |
| A/H1N1 | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| A/H3N2 | 265 (99.3) | 258 (95.9) | 258 (97.4) |
| B | 2 (0.7) | 3 (1.1) | 2 (0.8) |
| Negative | 0 (0.0) | 7 (2.6) | 4 (1.5) |
Abbreviations: FAS, the full analysis set; LO-20TD, 20 mg of laninamivir octanoate administered once daily for 2 days; LO-40SD, 40 mg of laninamivir octanoate, single administration; SD, standard deviation.
a More than 1 participant could be enrolled for each index patient. In this case, the index patient was counted once for each household member who was enrolled. Of the 687 index patients (FAS) enrolled, 584 were associated with 1 participant, 92 with 2 participants, and 11 with 3 participants. In this table, the number “N” of household members and index patients in each treatment group is identical.
Efficacy
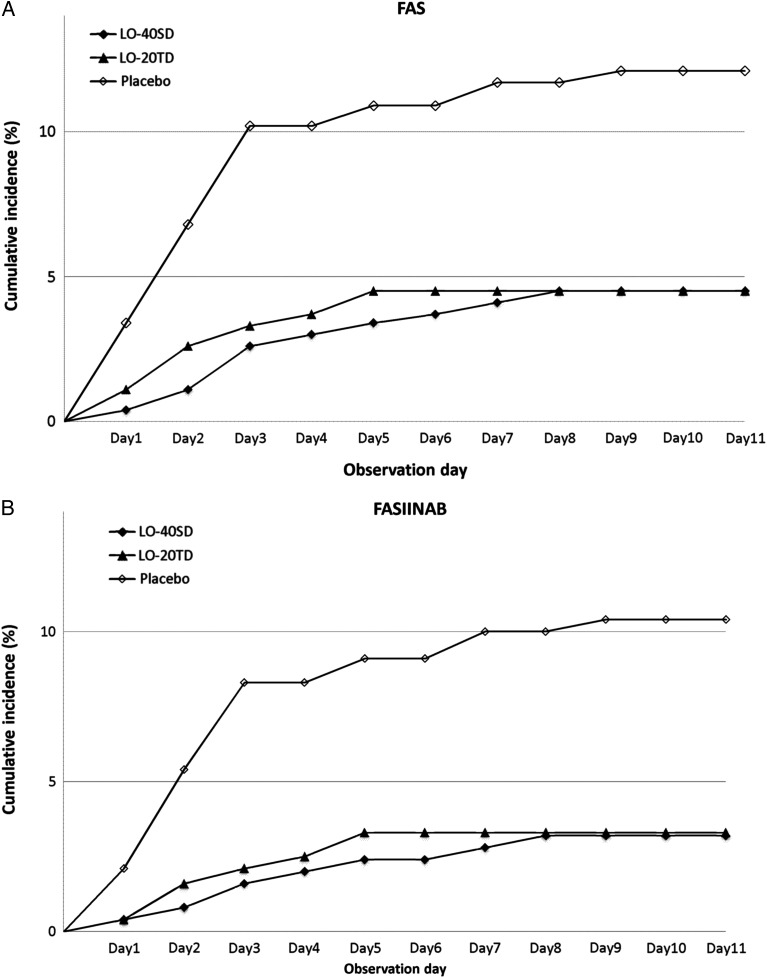
In the FAS, the proportions of participants who contracted clinical influenza (defined as influenza virus positive, an axillary temperature >37.5°C, and at least 2 symptoms with a severity of grade 2 or 3), the primary endpoint, were 4.5% (12/267), 4.5% (12/269), and 12.1% (32/265) in the LO-40SD, LO-20TD, and placebo groups, respectively (Table 2 and Figure 2A). Laninamivir octanoate significantly reduced the proportion of participants with clinical influenza compared with placebo (P = .001, P = .001, respectively). The protective efficacy of LO-40SD was comparable to that of LO-20TD, with RRRs compared with placebo of 62.8% (95% CI, 29.3 to 80.4) and 63.1% (95% CI, 29.8 to 80.5), respectively. Similar results were obtained in the FASII and FASIINAB (Table 2 and Figure 2B). The proportions of participants with symptomatic influenza were 8.6% (23/267), 9.3% (25/269), and 18.9% (50/265) in the LO-40SD, LO-20TD, and placebo groups, respectively, and the proportions of participants with laboratory-confirmed influenza infection were 11.7% (29/248), 13.0% (32/247), and 25.3% (62/245), respectively, showing a significant reduction compared with placebo (Table 2).
Table 2.
Protective Effect of Laninamivir Against Influenza Infection
| LO-40SD |
LO-20TD |
Placebo | |||||
|---|---|---|---|---|---|---|---|
| Outcome | No./Total (%) | P Valuea | RRRb (95% CI) | No./Total (%) | P Valuea | RRRb (95% CI) | No./Total (%) |
| Primary endpoint (FAS) | |||||||
| Clinical influenza | 12/267 (4.5) | .001 | 62.8 (29.3 to 80.4) | 12/269 (4.5) | .001 | 63.1 (29.8 to 80.5) | 32/265 (12.1) |
| Secondary endpoints (FAS) | |||||||
| Symptomatic influenza | 23/267 (8.6) | <.001 | 54.3 (27.4 to 71.3) | 25/269 (9.3) | .001 | 50.7 (22.8 to 68.6) | 50/265 (18.9) |
| Asymptomatic influenza | 25/267 (9.4) | .32 | 22.5 (–27.2 to 52.7) | 29/269 (10.8) | .68 | 10.7 (−43.3 to 44.4) | 32/265 (12.1) |
| Laboratory-confirmed influenza infectionc | 29/248 (11.7) | <.001 | 53.8 (30.8 to 69.2) | 32/247 (13.0) | <.001 | 48.8 (24.5 to 65.3) | 62/245 (25.3) |
| Other endpoints | |||||||
| Clinical influenza in FASII | 12/267 (4.5) | .001 | 63.3 (30.4 to 80.7) | 12/262 (4.6) | .001 | 62.6 (29.1 to 80.3) | 32/261 (12.3) |
| Clinical influenza in FASIINAB | 8/248 (3.2) | .001 | 68.9 (32.4 to 85.7) | 8/243 (3.3) | .002 | 68.3 (31.0 to 85.4) | 25/241 (10.4) |
Abbreviations: CI, confidence interval; FAS, the full analysis set; FASII, the full analysis set, index-infected; FASIINAB, the full analysis set, index-infected virus-negative at baseline; LO-20TD, 20 mg of laninamivir octanoate administered once daily for 2 days; LO-40SD, 40 mg of laninamivir octanoate, single administration; RRR, relative risk reduction.
a Analyzed using Fisher exact test.
b 100 × (1 − laninamivir/placebo).
c Participants confirmed to be infected with the influenza virus at baseline were excluded.
Figure 2.
Cumulative number of participants with clinical influenza, the primary endpoint, according to observation day. A, The cumulative number of participants with clinical influenza, the primary endpoint, by observation day in the full analysis set (FAS). B, The cumulative number of participants with clinical influenza, the primary endpoint, by observation day in the FAS index-infected virus-negative at baseline set (FASIINAB). Abbreviations: LO-20TD, 20 mg of laninamivir octanoate administered once daily for 2 days; LO-40SD, 40 mg of laninamivir octanoate, single administration.
In the subgroup of participants whose related index patient was infected with the influenza A(H3N2) virus, laninamivir octanoate significantly reduced the proportion of participants infected with clinical influenza compared with placebo (Table 3). In both the vaccinated and unvaccinated subgroups in the 2014–2015 influenza season, laninamivir octanoate reduced the proportion of participants who developed clinical influenza compared with placebo. A similar trend for protective efficacy was generally seen in the other subgroup categories examined in the prespecified subgroup analyses (Table 3).
Table 3.
Subgroup Analyses for Clinical Influenza—the Full Analysis Set
| Subgroup | LO-40SD |
LO-20TD |
Placebo | ||||
|---|---|---|---|---|---|---|---|
| No./Total (%) | P Valuea | RRRb (95% CI) | No./Total (%) | P Valuea | RRRb (95% CI) | No./Total (%) | |
| Age | |||||||
| <16 y | 1/33 (3.0) | .60 | 54.5 (–376.1 to 95.7) | 1/35 (2.9) | .59 | 57.1 (–349.6 to 95.9) | 2/30 (6.7) |
| ≥16 y | 11/234 (4.7) | .002 | 63.2 (28.3 to 81.1) | 11/234 (4.7) | .002 | 63.2 (28.3 to 81.1) | 30/235 (12.8) |
| Sex | |||||||
| Female | 11/237 (4.6) | .001 | 63.6 (29.2 to 81.3) | 11/241 (4.6) | .001 | 64.2 (30.3 to 81.7) | 30/235 (12.8) |
| Male | 1/30 (3.3) | 1.00 | 50.0 (–422.4 to 95.2) | 1/28 (3.6) | 1.00 | 46.4 (–458.7 to 94.9) | 2/30 (6.7) |
| Time from onset of influenza symptoms in the index patient to completion of the first study treatment | |||||||
| < 24 hours | 10/180 (5.6) | .10 | 47.2 (−12.9 to 75.3) | 4/159 (2.5) | .004 | 76.1 (30.1 to 91.8) | 16/152 (10.5) |
| ≥ 24 hours | 2/87 (2.3) | .004 | 83.8 (31.3 to 96.2) | 8/110 (7.3) | .13 | 48.6 (–15.1 to 77.1) | 16/113 (14.2) |
| Vaccinated in current season | |||||||
| No | 7/166 (4.2) | .01 | 63.6 (15.7 to 84.3) | 3/168 (1.8) | <.001 | 84.6 (48.9 to 95.4) | 19/164 (11.6) |
| Yes | 5/101 (5.0) | .08 | 61.5 (–3.9 to 85.8) | 9/101 (8.9) | .49 | 30.8 (–54.7 to 69.0) | 13/101 (12.9) |
| Relationship to the index patient | |||||||
| Parent | 11/223 (4.9) | .003 | 62.0 (26.1 to 80.5) | 11/227 (4.8) | .002 | 62.7 (27.4 to 80.8) | 30/231 (13.0) |
| Sibling | 1/32 (3.1) | 1.00 | 48.4 (–441.0 to 95.1) | 1/37 (2.7) | .59 | 55.4 (–369.5 to 95.8) | 2/33 (6.1) |
| Virus type and subtype | |||||||
| A/H1N1pdm09 | 0/0 | – | – | 0/1 (0.0) | – | – | 0/1 (0.0) |
| A/H3N2 | 12/265 (4.5) | .001 | 63.5 (30.7 to 80.8) | 12/258 (4.7) | .002 | 62.5 (28.8 to 80.2) | 32/258 (12.4) |
| B | 0/2 (0.0) | – | – | 0/3 (0.0) | – | – | 0/2 (0.0) |
| Negative | 0/0 | – | – | 0/7 (0.0) | – | – | 0/4 (0.0) |
Abbreviations: CI, confidence interval; LO-20TD, 20 mg of laninamivir octanoate administered once daily for 2 days; LO-40SD, 40 mg of laninamivir octanoate, single administration; RRR, relative risk reduction.
a Analyzed using Fisher exact test.
b 100 × (1 − laninamivir/placebo).
Safety
The incidence of adverse events was similar for the LO-40SD, LO-20TD, and placebo groups at 11.6% (31/267), 11.2% (30/269), and 12.1% (32/265), respectively. The most common adverse events were nasopharyngitis (3.4%, 3.0%, and 4.2%, respectively) and upper respiratory tract inflammation (1.1%, 1.5%, and 1.1%, respectively). The incidences of adverse events considered by the investigators to be drug related were 1.9% (5/267), 1.9% (5/269), and 1.5% (4/265), respectively. All of the adverse events were regarded as being mild or moderate in severity. No deaths, bronchospasm, or other serious adverse events were reported.
DISCUSSION
The proportion of participants with clinical influenza (defined as laboratory-confirmed influenza with a temperature of at least 37.5°C accompanied by at least 2 symptoms), the primary endpoint, in the LO-40SD group was significantly lower than that in the placebo group. The RRR compared with placebo in the LO-40SD group was 62.8%, which was similar to the 63.1% in the LO-20TD group. This suggests that a single administration of laninamivir octanoate 40 mg as post-exposure prophylaxis is effective for preventing the development of influenza through household contacts. The RRR compared with the placebo was comparable to that of laninamivir octanoate 20 mg for 2 days, which was proven to be effective for post-exposure prophylaxis in a previous study [9].
The proportion of participants infected with influenza virus, the secondary endpoint, in the LO-40SD and LO-20TD groups was significantly lower than that in the placebo group, which shows that a single administration of laninamivir octanoate is effective in preventing the transmission of the influenza virus.
There are differences in the protective efficacies of laninamivir octanoate reported in other post-exposure prophylaxis studies. In a study of the 2009 influenza pandemic season, the proportions of participants with clinical influenza were 3.6% (7/197), 3.7% (7/188), and 6.6% (12/183) for the 20-mg weekly, 40-mg weekly, and placebo groups, respectively, with protective efficacies of 45.8% and 43.2% in the 20-mg weekly and 40-mg weekly groups, respectively [10]. In contrast, in a study of the 2011–2012 influenza season, the proportions of participants with clinical influenza were 3.9% (19/487), 3.7% (18/486), and 16.9% (81/478) for the 20-mg 2-day, 20-mg 3-day, and placebo groups, respectively, with protective efficacies of 77.0% and 78.1% for the 20-mg 2-day and 20-mg 3-day groups, respectively [9]. One reason for this is that the epidemic virus strains vary from season to season, with incidence rates differing by age. Notably, the number of patients infected with the influenza A(H1N1)pdm09 virus in the 2009 influenza pandemic season was very low in persons aged ≥30 years, and it was persons in this age group who comprised most of the study participants, and the study did not have sufficient statistical power to detect significance.
In both the vaccinated and unvaccinated subgroups in the 2014–2015 influenza season, laninamivir octanoate reduced the incidence of clinical influenza compared with placebo. Regardless of the vaccination status, laninamivir octanoate was shown to be effective as post-exposure prophylaxis. In the subgroup of participants who were first administered laninamivir octanoate less than 24 hours after the onset of symptoms in the index patient, the protective efficacy for participants in the LO-20TD group was higher than that for participants in the LO-40SD group. In the subgroup of participants administered the drug at least 24 hours after, the reverse was true. The reasons for this finding are unclear and further research is necessary.
Our study had several limitations. First, the vast majority of the index patients were infected with influenza A(H3N2) and the number of participants whose index patient was infected with influenza A(H1N1)pdm09, seasonal influenza A(H1N1), or influenza B virus was small. Although nonclinical study results have shown that laninamivir octanoate is effective against the influenza A(H1N1)pdm09, seasonal influenza A(H1N1), and influenza B viruses [16, 17], the efficacy against these virus types will need to undergo further evaluation. Second, the study design was different from the household influenza prophylaxis trial design recommended in the Food and Drug Administration guidance [18]. The randomization and analysis of this study were all done on an individual basis, not for the whole family. Our purpose was to evaluate the efficacy of laninamivir octanoate for those in close contact with an influenza patient in a household setting. Third, in this study we did not assess viral resistance to laninamivir octanoate. However, no decrease of neuraminidase inhibitory activity was found for laninamivir octanoate administration in investigations done in the 2010–2011 to 2013–2014 influenza seasons [19–22]. Finally, we excluded children aged <10 years because their recommended dose regimen is different from that for patients aged ≥10 years. However, a parallel study of children aged <10 years in the 2014–2015 influenza season confirmed the efficacy of a single inhalation of 20 mg of laninamivir as post-exposure prophylaxis (manuscript in preparation).
Our findings indicate that prophylaxis with laninamivir octanoate is an effective option for post-exposure prophylaxis in terms of its convenience and high compliance rate. A single inhalation of laninamivir octanoate may have great advantages over drugs that require daily administration, such as oseltamivir and zanamivir, particularly for healthcare workers in a pandemic setting. Further studies of prophylaxis are required for laninamivir octanoate use with persons at high risk of acquiring influenza, such as residents of nursing homes.
In conclusion, a single administration of 40 mg of laninamivir octanoate was effective as post-exposure prophylaxis to prevent the development of influenza through household contacts, as was the inhalation of 20 mg of laninamivir octanoate once daily for 2 days. Furthermore, both regimens were well tolerated.
Supplementary Material
Notes
Financial support. Daiichi Sankyo Co., Ltd. (Tokyo, Japan).
Manuscript preparation. Daiichi Sankyo Co., Ltd., was involved in the study design, data collection and statistical analyses. Assistance in the editing of the manuscript was provided by Corbet Vernon Sullivan (Fukuoka, Japan), funded by Daiichi Sankyo Co., Ltd.
Potential conflicts of interests. S. K., A. W., and H. I. have received consultancies for this study from Daiichi Sankyo Co., Ltd. All other authors were from Daiichi Sankyo Co., Ltd. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
APPENDIX
The following are members of Laninamivir Prophylaxis Study Group Project steering committee: Seizaburo Kashiwagi (Japan Physicians Association, Tokyo, Japan); Akira Watanabe (Research Division for Development of Anti-Infective Agents, Institute of Development, Aging and Cancer, Tohoku University, Sendai, Japan); Hideyuki Ikematsu (Japan Physicians Association, Tokyo, Japan); and Katsuyasu Ishida, Shinichiro Awamura, Satoshi Nishioka, Koji Isobe, Tokuhito Sumitani, and Mitsutoshi Uemori (Daiichi Sankyo, Tokyo, Japan).
Clinical investigators who enrolled at least 1 patient include the following: Toshiko Yamaguchi, Yutaka Igarashi, Hideki Sato, Kouta Saito, Tomoyuki Shibuya, Shinya Enomoto, Eiki Oshika, Yasuko Murakawa, Haruo Kuroki, Koji Maehara, Yuko Miyazono, Yoshihiro Umezawa, Ryuta Ono, Kenji Saito, Jiro Takei, Mikiko Takano, Hideki Amemiya, Kazuo Arakawa, Shigenori Matsubara, Kazumasa Sugimoto, Hiroshi Kikumori, Toshihiko Sunami, Ryota Yoshimura, Toshikazu Takahashi, Yutaka Nakamura Keiichi Tsuboi, Hidehisa Shinohara, Shigeru Onari, Michiko Tanabe, Hiroshi Taniguchi, Mikio Kihara, Tatsuo Yoshimitsu, Takato Yokoyama, Yoshio Takasaki, Yuji Yamashita, Hiroshi Harada, Katsumaro Aida, Shizuo Shindo, Kunihisa Shimomura, Yumi Kiyomatsu, Toru Umezu, Motohisa Ikeda, Minako Iwaya, Masaki Higashikawa, Takeshi Inamitsu, Yasuyuki Tokunaga, Satoru Okazaki, Yoichi Tokunaga, Tetsunari Maeda, and Hirofumi Tahara.
Contributor Information
Collaborators: for the Laninamivir Prophylaxis Study Group, Seizaburo Kashiwagi, Akira Watanabe, Hideyuki Ikematsu, Katsuyasu Ishida, Shinichiro Awamura, Satoshi Nishioka, Koji Isobe, Tokuhito Sumitani, Mitsutoshi Uemori, Toshiko Yamaguchi, Yutaka Igarashi, Hideki Sato, Kouta Saito, Tomoyuki Shibuya, Shinya Enomoto, Eiki Oshika, Yasuko Murakawa, Haruo Kuroki, Koji Maehara, Yuko Miyazono, Yoshihiro Umezawa, Ryuta Ono, Kenji Saito, Jiro Takei, Mikiko Takano, Hideki Amemiya, Kazuo Arakawa, Shigenori Matsubara, Kazumasa Sugimoto, Hiroshi Kikumori, Toshihiko Sunami, Ryota Yoshimura, Toshikazu Takahashi, Yutaka Nakamura, Keiichi Tsuboi, Hidehisa Shinohara, Shigeru Onari, Michiko Tanabe, Hiroshi Taniguchi, Mikio Kihara, Tatsuo Yoshimitsu, Takato Yokoyama, Yoshio Takasaki, Yuji Yamashita, Hiroshi Harada, Katsumaro Aida, Shizuo Shindo, Kunihisa Shimomura, Yumi Kiyomatsu, Toru Umezu, Motohisa Ikeda, Minako Iwaya, Masaki Higashikawa, Takeshi Inamitsu, Yasuyuki Tokunaga, Satoru Okazaki, Yoichi Tokunaga, Tetsunari Maeda, and Hirofumi Tahara
References
- 1.Harper SA, Bradley JS, Englund JA et al. Seasonal influenza in adults and children—diagnosis, treatment, chemoprophylaxis, and institutional outbreak management: clinical practice guidelines of the Infectious Diseases Society of America. Clin Infect Dis 2009; 48:1003–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fiore AE, Fry A, Shay D, Gubareva L, Bresee JS, Uyeki TM. Antiviral agents for the treatment and chemoprophylaxis of influenza—recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 2011; 60:1–24. [PubMed] [Google Scholar]
- 3.Watanabe A, Chang SC, Kim MJ, Chu DW, Ohashi Y. Long-acting neuraminidase inhibitor laninamivir octanoate versus oseltamivir for treatment of influenza: a double-blind, randomized, noninferiority clinical trial. Clin Infect Dis 2010; 51:1167–75. [DOI] [PubMed] [Google Scholar]
- 4.Sugaya N, Ohashi Y. Long-acting neuraminidase inhibitor laninamivir octanoate (CS-8958) versus oseltamivir as treatment for children with influenza virus infection. Antimicrob Agents Chemother 2010; 54:2575–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Watanabe A. A randomized double-blind controlled study of laninamivir compared with oseltamivir for the treatment of influenza in patients with chronic respiratory diseases. J Infect Chemother 2013; 19:89–97. [DOI] [PubMed] [Google Scholar]
- 6.Ikematsu H, Kawai N, Iwaki N, Kashiwagi S. The duration of fever and other symptoms after the initiation of laninamivir octanoate hydrate in the Japanese 2011–2012 influenza season. J Infect Chemother 2014; 20:81–5. [DOI] [PubMed] [Google Scholar]
- 7.Ikematsu H, Kawai N, Iwaki N, Kashiwagi S. Continued effectiveness of laninamivir octanate hydrate for influenza treatment in Japan: comparison between the 2011–2012 and 2012–2013 influenza seasons. J Infect Chemother 2014; 20:799–803. [DOI] [PubMed] [Google Scholar]
- 8.Ikematsu H, Kawai N, Iwaki N, Kashiwagi S. Clinical outcome of laninamivir octanoate hydrate for influenza in the 2013–2014 Japanese season. J Infect Chemother 2015; 21:802–7. [DOI] [PubMed] [Google Scholar]
- 9.Kashiwagi S, Watanabe A, Ikematsu H et al. Laninamivir octanoate for post-exposure prophylaxis of influenza in household contacts: a randomized double blind placebo controlled trial. J Infect Chemother 2013; 19:740–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kashiwagi S. Review of laninamivir octanoate for the postexposure prophylaxis against influenza. Jpn J Chemother 2013; 61:492–503. [Google Scholar]
- 11.Ishizuka H, Toyama K, Yoshiba S, Okabe H, Furuie H. Intrapulmonary distribution and pharmacokinetics of laninamivir, a neuraminidase inhibitor, after a single inhaled administration of its prodrug, laninamivir octanoate, in healthy volunteers. Antimicrob Agents Chemother 2012; 56:3873–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.International Conference on Harmonization of Technical Requirements for Registration of Pharmaceuticals for Human Use. ICH Harmonized Tripartite Guideline: Guideline for Good Clinical Practice, June 1996 Available at: http://www.ich.org/fileadmin/Public_Web_Site/ICH_Products/Guidelines/Efficacy/E6/E6_R1_Guideline.pdf. Accessed 23 January 2016. [PubMed] [Google Scholar]
- 13.National Institute of Infectious Diseases. Byogenkin kensyutsu manyual, 2003. Available at: http://www0.nih.go.jp/niid/reference/pathogen-manual-60.pdf Accessed 7 September 2015. Japanese.
- 14.World Health Organization. CDC protocol of real-time RTPCR for influenza A (H1N1). 30 April 2009 Available at: http://www.who.int/csr/resources/publications/swineflu/realtimeptpcr/en/index.html Accessed 10 September 2015.
- 15.Welliver R, Monto AS, Carewicz O et al. Effectiveness of oseltamivir in preventing influenza in household contacts: a randomized controlled trial. JAMA 2001; 285:748–54. [DOI] [PubMed] [Google Scholar]
- 16.Yamashita M, Tomozawa T, Kakuta M, Tokumitsu A, Nasu H, Kubo S. CS-8958, a prodrug of the new neuraminidase inhibitor R-125489, shows long-acting anti-influenza virus activity. Antimicrob Agents Chemother 2009; 53:186–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Itoh Y, Shinya K, Kiso M et al. In vitro and in vivo characterization of new swine-origin H1N1 influenza viruses. Nature 2009; 460:1021–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Food and Drug Administration. Guidance for Industry Influenza: Developing Drugs for Treatment and/or Prophylaxis, 2011 Available at: http://www.fda.gov/downloads/drugs/guidancecomplianceregulatoryinformation/guidances/ucm091219.pdf Accessed 24 January 2016.
- 19.Ikematsu H, Kawai N, Iwaki N, Kashiwagi S. In vitro neuraminidase inhibitory activities of four neuraminidase inhibitors against influenza viruses isolated in the 2010–2011 season in Japan. J Infect Chemother 2012; 18:529–33. [DOI] [PubMed] [Google Scholar]
- 20.Ikematsu H, Kawai N, Iwaki N, Kashiwagi S. In vitro neuraminidase inhibitory activity of four neuraminidase inhibitors against influenza virus isolates in the 2011–2012 season in Japan. J Infect Chemother 2014; 20:77–80. [DOI] [PubMed] [Google Scholar]
- 21.Ikematsu H, Kawai N, Iwaki N, Kashiwagi S. In vitro neuraminidase inhibitory activity of four neuraminidase inhibitors against clinical isolates of influenza virus in the Japanese 2012–2013 season. J Infect Chemother 2015; 21:39–42. [DOI] [PubMed] [Google Scholar]
- 22.Ikematsu H, Kawai N, Iwaki N, Kashiwagi S. In vitro neuraminidase inhibitory activity of four neuraminidase inhibitors against clinical isolates of influenza virus circulating in the Japanese 2013–2014 season. J Infect Chemother 2015; 21:634–8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.