Abstract
Objective
This study is designed to assess the cost of services provided to Medicare beneficiaries by nurse practitioners (NPs) billing under their own National Provider Identification number as compared to primary care physicians (PCMDs).
Data Source
Medicare Part A (inpatient) and Part B (office visit) claims for 2009–2010.
Study Design
Retrospective cohort design using propensity score weighted regression.
Data Extraction Methods
Beneficiaries cared for by a random sample of NPs and primary care physicians.
Principal Findings
After adjusting for demographic characteristics, geography, comorbidities, and the propensity to see an NP, Medicare evaluation and management payments for beneficiaries assigned to an NP were $207, or 29 percent, less than PCMD assigned beneficiaries. The same pattern was observed for inpatient and total office visit paid amounts, with 11 and 18 percent less for NP assigned beneficiaries, respectively. Results are similar for the work component of relative value units as well.
Conclusions
This study provides new evidence of the lower cost of care for beneficiaries managed by NPs, as compared to those managed by PCMDs across inpatient and office‐based settings. Results suggest that increasing access to NP primary care will not increase costs for the Medicare program and may be cost saving.
Keywords: Nurse practitioner, cost, primary care
In their role as primary care clinicians, nurse practitioners (NPs) work both autonomously and in collaboration with primary care and specialist physicians, physician assistants, and other clinicians. The preponderance of findings from research extending over several decades, including randomized control trials, indicate that NPs achieve clinical outcomes and patient satisfaction comparable to primary care physicians across a variety of settings and diagnoses (Mundinger et al. 2000; Venning et al. 2000; Brooten et al. 2002; Sakr et al. 2003; Lenz et al. 2004; Naylor et al. 2004; Wilson et al. 2005; Sears et al. 2007b; Ohman‐Strickland et al. 2008).
In recent years, policy makers have focused increasing attention on the potential of NPs to expand the capacity of the primary care workforce. Health insurance expansions under the Affordable Care Act (ACA), combined with the aging of the baby boom generation, are expected to increase the demand for primary care services and exacerbate current and projected problems in primary care physician supply and geographic distribution (Hofer, Abraham, and Moscovice 2011). Additionally, the ACA encourages the development of new models of primary care delivery that emphasize greater collaboration and teamwork between physicians and other clinicians, including NPs (Bodenheimer and Smith 2013). Finally, reports from the Institute of Medicine (2010) and National Governor's Association (2012) recommended the removal of state scope of practice regulations that restrict NPs from practicing to the full extent of their education and licensure.
A central tenet of the argument for expanding the numbers and roles of primary care NPs is that it takes less time to educate an NP compared to their physician counterpart, and that these clinicians provide equivalent quality on many dimensions of primary care. Although a few studies have examined the costs of NP provided care compared to primary care physicians (Roblin et al. 2004; Laurant et al. 2009), these studies focused on a specific disease or care setting and analyzed costs over a limited period of time. To our knowledge, no study has used national‐level data to systematically examine the cost of primary care services provided by NPs and primary care physicians over an extended time frame.
In this study we use Medicare administrative data to assess the cost of services provided over a 12‐month period to Medicare beneficiaries treated by NPs billing under their own National Provider Identification (NPI) number. We apply standard methods for assigning Medicare beneficiaries to NPs and to primary care physicians, control for patient severity and other differences that may affect the cost of care, and examine the cost of services provided by both clinicians.
Methods
We use a retrospective cohort design to compare Medicare allowed payment amounts for inpatient and ambulatory services provided by NPs and primary care physicians and use propensity score weighted regression to adjust for differences between beneficiaries.
Sample
We developed our sample in two stages. First, we selected a random sample of NPs and primary care physicians with NPIs and, second, gathered all claims for the beneficiaries treated by these clinicians during 2009 and 2010. As very little is known about the panel sizes of Medicare beneficiaries for NPs, we purposefully weighted our sample to include approximately two‐thirds NP associated beneficiaries and one‐third primary care physicians beneficiaries to help capture an adequate number of NPs. On average, NPs see about half as many Medicare beneficiaries as primary care physicians (see Table 1).
Table 1.
Number of Clinicians by Type in the Random and Full Sample, 2009–2010
| Number of Clinicians in Medicare (Population)a | Number of Clinicians in Random Sampleb | Mean Beneficiaries per Clinicianb | Range of Beneficiaries per Clinicianb | Number of Clinicians Observed in Full Sampleb | |
|---|---|---|---|---|---|
| NP (specialty code = 50) | 57,597 | 4,363 | 183 | 1–10,503 | 9,422 |
| MD (specialty code = 11 or 8) | 266,724 | 541 | 367 | 1–13,937 | 68,069 |
Derived from the 100% sample of all Medicare Part B claims maintained by Buccaneer.
Medicare, Part B paid claims for our sample.
Because each of the selected beneficiaries was treated by a number of clinicians, including specialists and others over the 12‐month period, gathering all claims for each beneficiary of our selected NPs and primary care physicians resulted in additional clinicians captured in the sample. The two‐step process resulted in 128,006 beneficiaries with one or more claims with specialty code “50” = NP and 9,422 unique NPs (Table 1). For primary care physicians we used Part B specialty codes “08” = family medicine and “11” = internal medicine to capture 474,243 beneficiaries and 68,069 unique physicians.
Attribution
We assigned beneficiaries to NPs and primary care physicians based on the distribution of the beneficiaries' total evaluation and management (E&M) expenditures. Specifically, we used the new (M1A: 99201‐99205) and established office visit (M1B: 99211‐99215), home visit (M4A: 99340‐99345; 99347‐99350), or nursing home visit (M4B: 99304‐99306; 99307‐99310) from the Berenson‐Eggers Type of Service Codes (BETOS) to constitute primary care E&M. These codes eliminate inpatient, emergency department, and specialist services from our definition of E&M.
Because each beneficiary in the sample had claims from an average of eight unique clinicians in 2009, we used the following attribution procedure to help ensure that a relatively strong clinical relationship existed between the beneficiary and the NP or primary care physician. First, we calculated the proportion of primary care E&M paid amounts provided to a given beneficiary by each clinician submitting a claim for that beneficiary in 2009 (range 0–1). Second, the beneficiary was then assigned to the clinician who provided the highest proportion of E&M paid amounts to that beneficiary. Third, we imposed a 30 percent minimum threshold for assignment; that is, for a given beneficiary to be assigned to a primary care clinician, that clinician had to provide the highest proportion of E&M services and this proportion had to represent at least 30 percent of the beneficiary's total E&M claims (Mehrotra et al. 2010). In the case of ties (two or more providers with the same percent of E&M paid amounts), one primary care clinician was randomly selected.
As a sensitivity test, we reproduced our results using 20 percent, 30 percent, 40 percent, and 50 percent minimum attribution thresholds (see Appendix SA2). Above 50 percent, the sample size begins to decrease, raising concerns about bias; however, the core results remain the same regardless of the attribution threshold used.
Dependent Variables
Cost was defined as the Medicare paid amount on paid claims. The influence of the primary care provider on costs likely increases as the setting of care for a given beneficiary shifts from inpatient to office based. To capture this influence, we used the total Part A, or inpatient paid amount, total Part B, or clinician paid amount, and E&M amount (as defined by the BETOS procedure code groupings on the Part B claim).
Under Medicare rules, NPs are permitted to bill their services at 85 percent of physician fees. This, by definition makes physicians more expensive, and therefore cost cannot be used as a proxy for resource use. To adjust for this payment differential, we included the work component of the resource value unit (RVU) as an additional dependent variable. An RVU consists of three components: work, practice, and malpractice expenses. The work component uses the Current Procedural Terminology code on the claim to determine the level of intensity and skill required to perform a given service. It provides a measure of resource use that is not affected by the payment differential. We multiplied the work RVU by the mean Medicare payment for primary care services in 2010 ($40) (Health Care Cost Institute 2012), to create our new dependent variable, dollar adjusted RVUs.
Independent Variables
To control for the effects of geographic variation in health care spending and regional practice differences on our measures of the costs of care (Newhouse and Graham 2013), we used the beneficiary zip code from the Medicare enrollment file to identify the CMS region in which a given beneficiary resided in 2010. Regions 8 and 9 were combined because of small sample size, leaving seven regions in the model and CMS Region 4 (AL, FL, GA, KY, MS, NC, SC, TN) as the reference group. A rural flag was also added from the Area Resource File based on beneficiary's place of residence. We included age in years, female sex, and white race as demographic controls derived from the enrollment file. Dual Medicaid‐Medicare eligibility status was defined as one or more months of state buy‐in, meaning the state subsidized the beneficiary's Medicare premium for at least 1 month during the calendar year. This variable serves as a proxy for poverty and identifies approximately 75 percent of dually eligible beneficiaries (Research Data Assistance Center 2012).
Clinical severity for each beneficiary was captured by the Elixhauser comorbid conditions (Elixhauser et al. 1998). The 30 comorbidities were identified through the diagnostic codes on all of a beneficiary's ambulatory and institutional paid claims in 2010.
Analysis
We used propensity score weighting to adjust for observable differences between the beneficiaries assigned to NPs and to primary care physicians. Propensity score weighted regression involves the estimation of a logistic regression model predicting the probability that a given beneficiary will see an NP (Hirano and Imbens 2001; Weintraub et al. 2012). For this model, we included all available demographics (age, sex, race, dual eligible, and original reason for entitlement), CMS region, and Elixhauser comorbidities. The predicted probability was then used as a weight in the paid amount and dollar adjusted RVU ordinary least squares regression models. In these models, each NP beneficiary was weighted 1 and each physician beneficiary was weighted p/(1‐p), where p is the probability of seeing an NP. The models controlled for the independent variables identified above.
Results
Our sample consisted of 928,440 beneficiaries continuously enrolled in Medicare Part A and Part B in 2010, with 558,199 assigned to an NP or a primary care physician. The remaining 370,241 beneficiaries were either assigned to a specialist physician, a facility (e.g., dialysis center), or were unassigned because no single provider accounted for 30 percent of the beneficiaries' E&M services and were excluded from the analytic sample. Of the beneficiaries in the analytic sample, 81 percent (N = 450,880) were assigned to primary care physicians and 19 percent (N = 107,219) assigned to NPs.
Beneficiaries assigned to NPs were significantly more likely to be non‐white, younger, female, dually eligible for Medicare and Medicaid, and living in a rural area (Table 2). They were also more likely than beneficiaries assigned to primary care physicians to have originally qualified for Medicare due to a disability, and were significantly less likely to have each of the Elixhauser comorbid conditions, with the exception of paralysis, neurological disorder, AIDS, weight loss, alcohol abuse, drug abuse, and psychoses.
Table 2.
Weighted and Unweighted Covariates for Nurse Practitioners and Primary Care Physician Assigned Beneficiaries
| Characteristic of Beneficiaries | Unweighted | Weighted | ||||
|---|---|---|---|---|---|---|
| Primary Care Physician (%) | NP (%) | p‐value | Primary Care Physician (%) | NP (%) | p‐value | |
| Demographic characteristics | ||||||
| Female | 62.3 | 66.2 | <.0001 | 66.4 | 66.2 | .29 |
| White | 86.6 | 83.5 | <.0001 | 83.4 | 83.5 | .78 |
| Mean age (years) | 73.6 | 72.0 | <.0001 | 71.8 | 71.9 | .03 |
| Dually eligible for Medicare and Medicaid | 26.4 | 40.4 | <.0001 | 40.7 | 40.4 | .09 |
| Rural | 2.6 | 16.0 | <.0001 | 4.3 | 4.2 | .08 |
| CMS region | ||||||
| Region 1 | 7.5 | 6.6 | <.0001 | 6.7 | 6.6 | .70 |
| Region 2 | 5.9 | 5.7 | .13 | 5.7 | 5.7 | .73 |
| Region 3 | 13.3 | 6.9 | <.0001 | 6.9 | 6.9 | .95 |
| Region 4 | 26.0 | 29.7 | <.0001 | 29.5 | 29.6 | .32 |
| Region 5 | 20.1 | 18.0 | <.0001 | 17.9 | 18.0 | .72 |
| Region 6 | 7.9 | 11.3 | <.0001 | 11.5 | 11.4 | .37 |
| Region 7 | 6.1 | 7.3 | <.0001 | 7.3 | 7.3 | .76 |
| Region 8 | 6.6 | 9.7 | <.0001 | 9.8 | 9.7 | .37 |
| Region 9 | 6.4 | 4.5 | <.0001 | 4.5 | 4.5 | .83 |
| Elixhauser comorbidity | ||||||
| Congestive heart failure | 21.0 | 19.0 | <.0001 | 18.8 | 18.8 | .81 |
| Valve disorders | 17.3 | 10.7 | <.0001 | 10.7 | 10.7 | .93 |
| Pulmonary circulation disease | 6.3 | 3.9 | <.0001 | 3.9 | 3.9 | .79 |
| Peripheral vascular disease | 24.1 | 23.1 | <.0001 | 23.0 | 23.0 | .49 |
| Hypertension | 77.5 | 70.1 | <.0001 | 69.9 | 70.1 | .31 |
| Complex hypertension | 4.6 | 3.7 | <.0001 | 3.7 | 3.7 | .91 |
| Paralysis | 4.3 | 5.1 | <.0001 | 5.1 | 5.1 | .48 |
| Neurological disorders | 23.5 | 27.3 | <.0001 | 27.5 | 27.3 | .41 |
| Chronic pulmonary disease | 30.0 | 26.1 | <.0001 | 26.1 | 26.1 | .71 |
| Diabetes w/o complications | 36.8 | 32.6 | <.0001 | 32.6 | 32.6 | .95 |
| Diabetes w/complications | 14.8 | 12.7 | <.0001 | 12.7 | 12.7 | .86 |
| Hypothyroidism | 23.5 | 21.5 | <.0001 | 21.5 | 21.5 | .98 |
| Renal failure | 15.6 | 13.1 | <.0001 | 13.1 | 13.1 | .94 |
| Liver disease | 3.3 | 2.8 | <.0001 | 2.9 | 2.9 | .85 |
| Bleeding ulcer | 0.24 | 0.15 | <.0001 | 0.15 | 0.15 | .96 |
| AIDS | 0.32 | 1.10 | <.0001 | 1.1 | 1.1 | .63 |
| Lymphoma | 1.15 | 0.74 | <.0001 | 0.75 | 0.75 | .85 |
| Metastatic cancer | 2.1 | 1.5 | <.0001 | 1.5 | 1.5 | .95 |
| Solid tumor w/o metastasis | 11.8 | 7.7 | <.0001 | 7.7 | 7.7 | .74 |
| Rheumatoid arthritis | 6.2 | 4.6 | <.0001 | 4.6 | 4.6 | .93 |
| Coagulopathy | 6.5 | 4.9 | <.0001 | 4.9 | 4.9 | .82 |
| Obesity | 8.3 | 7.6 | <.0001 | 7.7 | 7.6 | .41 |
| Weight loss | 9.9 | 10.8 | <.0001 | 10.7 | 10.7 | .92 |
| Fluid disorders | 23.7 | 20.3 | <.0001 | 20.3 | 20.2 | .86 |
| Anemia | 2.6 | 1.8 | <.0001 | 1.8 | 1.8 | .94 |
| Deficiency anemia | 30.4 | 27.9 | <.0001 | 27.8 | 27.9 | .63 |
| Alcohol abuse | 2.0 | 2.0 | .19 | 2.0 | 2.0 | .81 |
| Drug abuse | 2.5 | 2.6 | .49 | 2.6 | 2.6 | .52 |
| Psychoses | 16.6 | 19.3 | <.0001 | 19.5 | 19.3 | .13 |
| Depression | 18.9 | 20.8 | <.0001 | 21.0 | 20.8 | .13 |
Sidak adjusted p‐value = 0.0012205.
Bonferroni adjusted p‐value = 0.0011905.
Applying the propensity score weights balanced the two groups of beneficiaries on all demographic and diagnostic characteristics (Table 2).
Cost of Care Provided by Nurse Practitioners and Primary Care Physicians
Table 3 presents the unadjusted estimates of the mean paid amounts and dollar adjusted RVUs per assigned beneficiary. The difference in costs between NP and primary care physician assigned beneficiaries is smallest (7 percent) in the inpatient setting. For the unadjusted total Part B paid amounts, beneficiaries assigned to an NP cost approximately 26 percent less than beneficiaries assigned to a primary care physician. Similarly, for unadjusted E&M paid amounts, NP assigned beneficiaries were 15 percent less costly than primary care physician assigned beneficiaries.
Table 3.
Unadjusted Paid Amounts and Relative Value Units for Nurse Practitioner and Physician Attributed Beneficiariesa
| Unadjusted Paid Amount/RVU | Number of Beneficiaries | Mean Total Paid Amount ($) | Nurse Practitioner Attributed Beneficiaries | Primary Care Physician Attributed Beneficiaries | Difference between Mean Paid Amounts | Percent Differenceb | ||
|---|---|---|---|---|---|---|---|---|
| Number | Mean Paid Amount | Number | Mean Paid Amount | |||||
| Total inpatient paid amount | 183,598 | $21,061 | 27,305 | $18,574 | 156,293 | $21,495 | $1,445 | 7 |
| Total part B paid amount | 522,726 | $3,769 | 96,241 | $2,924 | 426,485 | $3,960 | $1,036 | 26 |
| Total E&M paid amount | 519,495 | $1,585 | 95,241 | $1,266 | 424,254 | $1,657 | $112 | 15 |
| Cost of total dollar adjusted work RVUc | 522,715 | $2,403 | 96,238 | $1,905 | 426,477 | $2,515 | $611 | 24 |
| Cost of dollar adjusted E&M RVUc | 519,557 | $1,553 | 95,234 | $1,309 | 424,323 | $1,583 | $274 | 17 |
Results based on an attribution threshold of 30%.
PCMD‐PCNP difference as a percent of PCMD total.
The work RVU was multiplied by $40 to calculate a dollar value.
Dollar Adjusted RVUs
We next examined dollar adjusted RVUs. Findings from these analyses suggest that all Part B services provided to NP assigned beneficiaries over a 12‐month period were $611 less than services provided to beneficiaries assigned to primary care physicians or a 24 percent difference (Table 3). This difference between beneficiary groups decreases to $274 when RVUs for E&M services only are assessed. This is about 17 percent less than the dollar adjusted RVU E&M amount for beneficiaries assigned to primary physicians.
Propensity Score Weighted Analyses
Figure 1 shows the distribution of propensity scores for NP and MD assigned beneficiaries. The range for NP assigned beneficiaries is 0.02–0.67 compared to 0.02–0.65 for primary care physician assigned beneficiaries. There is a high degree of overlap between the two ranges with the scores of primary care physician assigned beneficiaries falling almost completely within the range of NP assigned beneficiaries, which indicates that propensity weighted regression is appropriate for our analytic purpose (Sears et al. 2007a; Caliendo and Kopeining 2008; Garrido et al. 2014). However, as a sensitivity test, we also ran the final models with cases outside the region of common support removed (N = 17,173 primary care physician assigned and N = 3,245 NP assigned beneficiaries), and our results did not change.
Figure 1.
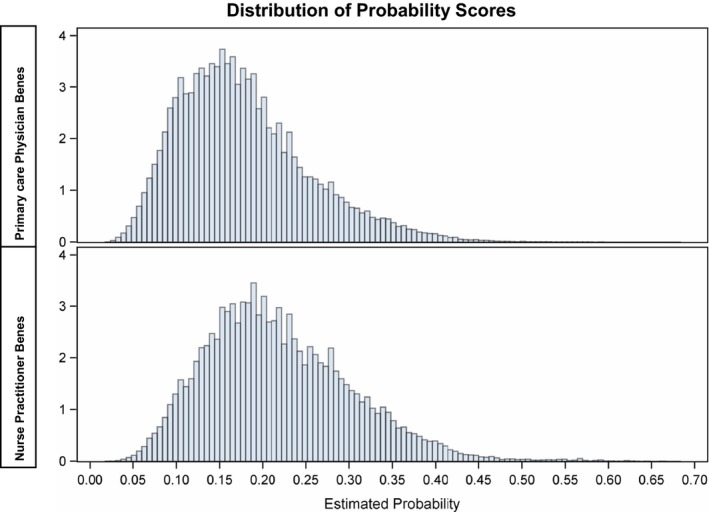
- Note: Results based on 30 percent attribution threshold.
Table 4 reports the propensity score weighted multivariable analysis, which adjusts for observable differences between beneficiaries assigned to NPs and primary care physicians. In these regression models, the intercept equals the average adjusted primary care physician paid amount, and the NP coefficient reflects the reduction in paid amounts for care provided by NPs. The total adjusted mean paid amount for Part A inpatient admissions is $22,898. Controlling for demographic and diagnostic characteristics, and the propensity to see an NP, beneficiaries assigned to an NP cost, on average, $2,474 less than those assigned to primary care physicians. This difference is approximately 11 percent less than the average, adjusted payment for physician assigned beneficiaries.
Table 4.
Propensity Score Weighted Regression Results of Medicare Paid Amounts and Dollar Adjusted RVUsa
| Inpatient Paid Amountb | Part B Paid Amountb | Evaluation and Management Paid Amountc | Total Dollar Adjusted Work RVUb | Total Dollar Adjusted E&M RVUc | |
|---|---|---|---|---|---|
| Intercept | 22,898 | 2,955 | 705 | $1,911 | 713 |
| Female | −1,877 | −22 | −12 | −10 | −11 |
| White | −1,970 | 67 | −11 | 63 | −1 |
| Age (years) | −288 | −34 | −10 | −22 | −10 |
| Duals | −2,082 | −511 | −133 | −320 | −94 |
| Rural | 606 | −140 | −144 | −132 | −154 |
| NP | −2,474 | −522 | −207 | −282 | −128 |
| Adjusted R 2 | 0.22 | 0.32 | 0.44 | 0.45 | 0.46 |
| Average percent difference NP to MD | 11 | 18 | 29 | 15 | 18 |
Parameter estimates in dollars adjusted for beneficiaries' sex, race, age, dual eligibility status, provider type, CMS regions, rural region, and 30 Elixhauser comorbidities (parameter estimates are not shown for geographic measures and Elixhauser comorbidities).
Results based on an attribution threshold of 30%.
All parameter estimates are significant at the <.0001 level.
All parameter estimates except for female and white are significant at the <.0001 level.
E&M, evaluation and management; NP, nurse practitioner; RVU, relative value unit.
Regression results for Part B office‐based expenditures indicate the average for primary care physician assigned beneficiaries was $2,955 while the average for NP assigned beneficiaries was $2,433. This is approximately 18 percent less or $522 (Table 4). By way of comparison, the unadjusted difference between NP and primary care physician assigned patients is $1,036 (Table 3). The adjusted results are nearly half of the unadjusted results.
For E&M services only, primary care physician assigned beneficiaries cost $705 compared to $498 for NP assigned beneficiaries. The adjusted difference is $207 or 29 percent.
The multivariate results for dollar adjusted RVUs are also shown in Table 4. After adjusting for demographic characteristics, geography, comorbidities, and the propensity to see an NP, the dollar adjusted RVU payments for beneficiaries assigned to an NP were $1,629 or approximately 15 percent less than primary care physician assigned beneficiaries ($1,911). Similarly, when E&M RVUs were examined, NP assigned beneficiaries cost $585, or approximately 18 percent less than primary care physician assigned beneficiaries ($173).
Discussion
The aim of this study was to determine the difference in paid claims for services provided to Medicare beneficiaries who were assigned to either an NP or to a primary care physician. To help ensure a meaningful clinical relationship existed between beneficiary and clinician, we imposed a high threshold for attribution, requiring the clinician to account for at least 30 percent of E&M services. Such a relationship is particularly important when examining Medicare beneficiaries who are often seen by many different clinicians during a year. Propensity score weighted regression was also used to help adjust for clinical and socio‐economic differences between beneficiaries assigned to an NP versus a primary care physician. We examined beneficiary level paid amounts for primary care services extending from inpatient to outpatient E&M care over a 12‐month period.
Findings indicate that Medicare paid amounts are consistently lower for NP assigned beneficiaries compared to primary care physician assigned beneficiaries in both inpatient and office‐based settings. When considering the size of the differences relative to their average cost, the largest difference is for E&M services. Here, the Medicare allowed payment amounts for NP assigned beneficiaries were approximately 29 percent less than primary care physician beneficiaries. This difference is at least partly explained by the payment differential between NPs and physicians.
Modeling dollar adjusted RVUs narrowed the E&M payment differences from 29 percent to 18 percent, suggesting that reimbursement rates are a major driver of observed cost differences. The unexplained cost difference of 18 percent may be due to differences in practice patterns between NPs and primary care physicians, uncontrolled differences in beneficiary case mix, or to other unobserved factors (such as beneficiaries' preferences or requests) that affect the costs of providing primary care services.
We believe that our examination of beneficiary claims over a 12‐month period offers a more comprehensive assessment of the costs of NP provided care. Prior studies that focused on much smaller units of time (Laurant et al. 2009) found similar or no differences in the costs of NP and physician provided care. However, by assessing claims over a year, findings from our analysis suggest the possibility of different practice styles between the two groups of clinicians which may result in lower average 12‐month expenditures for similar patients. Not only does such an approach illuminate possible differences between NPs and primary care physicians, but it also implies that analysts developing physician value based purchasing payment models consider that the full benefit of primary care services accrue over weeks or months of time rather than just days (Berenson and Kaye 2013; Chien and Rosenthal 2013).
Adjusting for potential differences in beneficiary characteristics is one of the major challenges in comparing provider performance. We considered using instrumental variables to address this selection problem. In this approach, the instrument serves as a proxy for the unobserved sorting mechanism that leads to the observed assignment (NP or primary care physician). However, there were no viable instruments available in the claims data, such as distance to clinician or beneficiary preference. Propensity score weighted regression offers an alternative to adjust for observable differences between the two groups. However, it is possible that some unobservable differences remain, such as waiting time or beneficiary preference for type of clinician. It is not possible to capture these preferences using claims data.
The study is limited by the fact that some NPs bill Medicare for their services “incident to” a physician. Under incident to billing the care provided by an NP is billed under a physician's NPI when certain conditions are met, including an initial encounter between the physician and patient and the presence of a physician in the office when the service is performed. Because services billed in this manner cannot be identified in the claims data, some services billed by physicians may have actually been provided by NPs. Incident to billing may be more common in states with restrictive scope of practice laws, but there may be financial and other reasons for a practice to select this approach. Therefore, our results should be interpreted with awareness that it is unclear whether incident to billing under‐ or overstates the differences between these two groups of clinicians. This uncertainty, as well as the unknown frequency of incident to billing, could be addressed by the Medicare program adjusting its claims coding practices to identify incident to billing.
In addition to incident to billing, there are other reasons why services provided to beneficiaries by NPs may not be visible in Medicare administrative data. For example, NPs may not bill all or some of the services they provide under their own NPI number either due to supervision requirements within their organizations, employment arrangements, or state scope of practice requirements for diagnosing and prescribing. We are limited in our capacity to see the impact of state regulations given the distribution of beneficiaries by state. Finally, because NPs who bill Medicare under their own NPI may differ from those who do not, our results cannot be generalized to all NPs providing care to Medicare beneficiaries.
To our knowledge, this is the first national‐level analysis of the cost of NPs providing primary care to Medicare beneficiaries. Because Medicare enrollments will expand rapidly as the baby boom generation ages, total spending on the program is likely to increase substantially. Further, as policy makers attempt to increase the capacity of the primary care workforce, in part by increasing the numbers of NPs, our results suggest that having more NPs providing primary care services to Medicare beneficiaries is unlikely to cost Medicare more than if the program relied solely on primary care physicians, and it may actually reduce costs. The $207 per beneficiary annual difference between primary care physicians and NPs on E&M services suggests that the Medicare program could obtain significant cost savings if more NPs were providing primary care services to beneficiaries. Indeed, our results are consistent with a recent estimate from the CMS Office of the Actuary that Medicare could save $60 million over 10 years by allowing CMS to assign beneficiaries to accountable care organizations based on services provided by NPs, physician assistants, and clinical nurse specialists (HHS FY2016). While the Office of the Actuary's study is not directly comparable to ours due to differences in methods, both studies suggest that expanding the role of NPs as primary care clinicians could result in savings to the Medicare program.
Supporting information
Appendix SA1: Author Matrix.
Appendix SA2: Sensitivity of Results to Attribution Threshold.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: This work was generously supported by a grant jointly provided by the Robert Wood Johnson Foundation, the Gordon and Betty Moore Foundation, and Johnson and Johnson's Campaign for Nursing's Future. We also acknowledge the tremendous statistical and programming contributions of Galina Zolotusky. The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; or the preparation, review, or approval of the manuscript. Dr. Perloff had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Disclosures: None.
Disclaimers: None.
References
- Berenson, R. A. , and Kaye D. R.. 2013. “Grading a Physician's Value — The Misapplication of Performance Measurement.” New England Journal of Medicine 369 (22): 2079–81. [DOI] [PubMed] [Google Scholar]
- Bodenheimer, T. S. , and Smith M. D.. 2013. “Primary Care: Proposed Solutions to the Physician Shortage without Training More Physicians.” Health Affairs 32 (11): 1881–6. [DOI] [PubMed] [Google Scholar]
- Brooten, D. , Naylor M. D., York R., Brown L. P., Munro B. H., Hollingsworth A. O., Cohen S. M., Finkler S., Deatrick J., and Youngblut J. M.. 2002. “Lessons Learned from Testing the Quality Cost Model of Advanced Practice Nursing (APN) Transitional Care.” Journal of Nursing Scholarship 34 (4): 369–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caliendo, M. , and Kopeining S.. 2008. “Some Practical Guidance for the Implementation of Propensity Score Matching.” Journal of Economic Surveys 22 (1): 31–72. [Google Scholar]
- Chien, A. T. , and Rosenthal M. B.. 2013. “Medicare's Physician Value‐Based Payment Modifier — Will the Tectonic Shift Create Waves?” New England Journal of Medicine 369 (22): 2076–8. [DOI] [PubMed] [Google Scholar]
- Elixhauser, A. , Steiner C., Harris D. R., and Coffey R. M.. 1998. “Comorbidity Measures for Use with Administrative Data.” Medical Care 36 (1): 8–27. [DOI] [PubMed] [Google Scholar]
- Garrido, M. M. , Kelley A. S., Paris J., Roza K., Meier D. E., Morrison R. S., and Aldridge M. D.. 2014. “Methods for Constructing and Assessing Propensity Scores.” Health Services Research 49 (5): 1701–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health Care Cost Institute . 2012. Health Care Cost and Utilization Report. Washington, DC: HCCI. [Google Scholar]
- Health and Human Services . 2015. “Fiscal Year 2016 Budget in Brief Strengthening Health and Opportunity for All Americans,” pp. 65–6. United States Department of Health; [accessed on August 15, 2015]. Available at http://www.hhs.gov/sites/default/files/budget/fy2016/fy-2016-budget-in-brief.pdf [Google Scholar]
- Hirano, K. , and Imbens G.. 2001. “Estimation of Causal Effects Using Propensity Score Weighting: An Application to Data on Right Heart Catheterization.” Health Services and Outcomes Research Methodology 2 (3–4): 259–78. [Google Scholar]
- Hofer, A. N. , Abraham J. M., and Moscovice I. R. A.. 2011. “Expansion of Coverage under the Patient Protection and Affordable Care Act and Primary Care Utilization.” Milbank Quarterly 89 (1): 69–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine . 2010. The Future of Nursing. Washington, DC: The National Academies Press; [accessed on August 15, 2015]. Available at http://www.thefutureofnursing.org/IOM-Report [Google Scholar]
- Laurant, M. , Harmsen M., Wollersheim H., Grol R., Faber M., and Sibbald B.. 2009. “The Impact of Nonphysician Clinicians: Do They Improve the Quality and Cost‐Effectiveness of Health Care Services?” Medical Care Research and Review 66 (6 suppl): 36S–89S. [DOI] [PubMed] [Google Scholar]
- Lenz, M. , Kane R., Hopkins S., and Lin S.. 2004. “Primary Care Outcomes in Patients Treated by Nurse Practitioners or Physicians: Two‐year Follow‐up.” Medical Care Research and Review 61: 332–51. [DOI] [PubMed] [Google Scholar]
- Mehrotra, A. , Adams J. L., Thomas J. W., and McGlynn E. A.. 2010. “The Effect of Different Attribution Rules on Individual Physician Cost Profiles.” Annals of Internal Medicine 152 (10): 649–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mundinger, M. O. , Kane R. L., Lenz E. R., Totten A. M., Tsai W. Y., Cleary P. D., Friedewald W. T., Siu A. L., and Shelanski M. L.. 2000. “Primary Care Outcomes in Patients Treated by Nurse Practitioners or Physicians: A Randomized Trial.” The Journal of the American Medical Association 283 (1): 59–68. [DOI] [PubMed] [Google Scholar]
- National Governor's Association . 2012. The Role of Nurse Practitioners in Meeting Increasing Demand for Primary Care. Washington, DC: National Governors Association Center for Best Practices. [Google Scholar]
- Naylor, M. B. , Brooten D. A., Campbell R. L., Maislin G., McCauley K. M., and Schwartz J. S.. 2004. “Transitional Care of Older Adults Hospitalized with Heart Failure: A Randomized, Controlled Trial.” Journal of the American Geriatrics Society 52 (5): 675–84. [DOI] [PubMed] [Google Scholar]
- Newhouse, J. P. , and Graham R. P.. 2013. Variation in Health Care Spending: Target Decision Making, Not Geography. Washington, DC: Institute of Medicine of the National Academies. [PubMed] [Google Scholar]
- Ohman‐Strickland, P. A. , Orzano A. J., Hudson S. V., Solberg L. I., DiCiccio‐Bloom B., O'Malley D., Tallia A. F., Balasubramanian B. A., and Crabtree B. F.. 2008. “Quality of Diabetes Care in Family Medicine Practices: Influence of Nurse‐Practitioners and Physician's Assistants.” Annals of Family Medicine 6 (1): 14–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Research Data Assistance Center . 2012. “Identifying Dual Eligible Medicare Beneficiaries in the Medicare Beneficiary Enrollment Files” [accessed on October 4, 2014]. Available at http://www.resdac.org/resconnect/articles/149
- Roblin, D. W. , Howard D. H., Becker E. R., Adams E., and Roberts M. H.. 2004. “Use of Midlevel Practitioners to Achieve Labor Cost Savings in the Primary Care Practice of an MCO.” Health Services Research 39 (3): 607–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sakr, M. K. , Kendall R., Angus J., Sanders A., Nicholl J., and Wardrope J.. 2003. “Emergency Nurse Practitioners: A Three Part Study in Clinical and Cost Effectiveness.” Emergency Medicine Journal 20 (2): 158–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sears, J. M. , Wickizer T. M., Franklin G. M., Cheadle A. D., and Berkowitz B.. 2007a. “Nurse Practitioners as Attending Providers for Injured Workers: Evaluating the Effect or Role Expansion on Disability and Cost.” Medical Care 45 (12): 1154–61. [DOI] [PubMed] [Google Scholar]
- Sears, J. W. , Wickizer T. M., Franklin G. M., Cheadle A. D., and Berkowitz B.. 2007b. “Nurse Practitioners as Attending Providers for Workers with Uncomplicated Back Injuries: Using Administrative Data to Evaluate Quality and Process of Care.” Journal of Occupational and Environmental Medicine 49 (8): 900–8. [DOI] [PubMed] [Google Scholar]
- Venning, P. D. , Durie A., Roland M., Roberts C., and Leese B.. 2000. “Randomized Controlled Trial Comparing Cost Effectiveness of General Practitioners and Nurse Practitioners in Primary Care.” British Medical Journal 320: 1048–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weintraub, W. S. , Grau‐Sepulveda M. V., Weiss J. M., O'Brien S. M., Peterson E. D., Kolm P., Zhang Z., Klein L. W., Shaw R. E., McKay C., Ritzenthaler L. L., Popma J. J., Messenger J. C., Shahian D. M., Grover F. L., Mayer J. E., Shewan C. M., Garratt K. N., Moussa I. D., Dangas G. D., and Edwards F. H.. 2012. “Comparative Effectiveness of Revascularization Strategies.” New England Journal of Medicine 366 (16): 1467–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson, I. B. , Landon B. E., Hirschhorn L. R., McInnes K., Ding L., Marsden P. V., and Cleary P. D.. 2005. “Quality of HIV Care Provided by Nurse Practitioners, Physician Assistants, and Physicians.” Annals of Internal Medicine 143 (10): 729–36. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix SA1: Author Matrix.
Appendix SA2: Sensitivity of Results to Attribution Threshold.


