Abstract
Objective
The design of health insurance, and the role out‐of‐pocket (OOP) payments play in it, is a key policy issue as rising health costs have encouraged greater cost‐sharing measures. This paper compares the percentage of Americans spending large amounts OOP to meet their health needs with percentages in eight other developed countries. By disaggregating by age and income, the paper focuses on the poor and elderly populations within each.
Data Source
The study uses nationally representative household survey data made available through the Luxembourg Income Study. It includes nations with high, medium, and low levels of OOP spending.
Study Design
Households have high medical spending when their OOP expenditures exceed a threshold share of income. I calculate the share of each nation's population, as well as subpopulations within it, with high OOP expenditures.
Principal Findings
The United States is not alone in exposing large numbers of citizens to high OOP expenses. In six of the other eight countries, one‐quarter or more of low‐income citizens devoted at least 5 percent of their income to OOP expenses, and in all but two countries, more than 1 in 10 elderly citizens had high medical expenses.
Conclusions
For some populations in the sample nations, health insurance does not provide adequate financial protection and likely contributes to inequities in health care delivery and outcomes.
Keywords: Out‐of‐pocket, insurance design, financing equity, access, international comparison
The design of health insurance coverage, and the role out‐of‐pocket (OOP) payments play in it, has become a key policy concern as rising health care costs encourage the expansion of greater cost‐sharing measures (Tambor et al. 2011; Balabanova et al. 2012; Law et al. 2013; Zare and Anderson 2013; Collins et al. 2014; OECD 2014). The percentage of Americans covered by employer‐offered health insurance with deductibles of at least $1,000 grew from 10 to 41 percent over the period 2006 and 2014, and deductibles for one‐in‐five are now $2,000–$4,500 (Kaiser Family Foundation 2014). While a shift toward higher OOP expenditures—defined as the costs associated with using health care–may be justified because they make insurance more affordable and reduce the overconsumption of health services and products, this shift also has the potential to increase inequities in health care delivery and outcomes.
This paper estimates the percentage of citizens in the United States with large OOP expenditures and compares this percentage with the proportion in eight other developed countries. It focuses on high spending rates among nations' vulnerable poor and elderly populations, as these are the ones for whom concern over OOP's consequences are greatest. While OOP expenditures generally make up only a small fraction of overall health spending, and all countries rely to one degree or another on them, this manner of financing health expenses is the most regressive (Wagstaff et al. 1999; Waters, Anderson, and Mays 2004). Moreover, unlike third‐party insurance payments, which are largely paid for through taxes and payroll deductions, OOP expenses are usually discretionary, occurring at the point of health care delivery. High levels of it can discourage health care usage, especially among the poor and elderly.
Background
Among members of the Organization for Economic Cooperation and Development (OECD), OOP payments account for an average of 19 percent of total health care expenditures, while in the United States they account for 12 percent (Column 1 in Table 1). As Table 1 also shows (column 2), the average per‐capita dollar amount of OOP spending among OECD countries ranges from around $200 to around $1,200.
Table 1.
Out‐of‐Pocket Expenses by Country (2010)a
| OOP % Healtha | OECD Per‐Capita | LIS Per‐Capita | LIS/OECD Per‐Capita | |
|---|---|---|---|---|
| OOPa | OOPb | OOP | ||
| Australia | 19.3 | $730 | $498 | 68% |
| France | 7.5 | $300 | $235 | 78% |
| Israel | 18.2 | $501 | $372 | 74% |
| Japan | 14.4 | $436 | $419 | 96% |
| Poland | 22.1 | $317 | $285 | 90% |
| Slovenia | 12.2 | $300 | $255 | 85% |
| Russia | 36.4 | $472 | $387 | 82% |
| Switzerland | 25.1 | $1,253 | $958 | 76% |
| United States | 12.0 | $988 | $739 | 75% |
| Belgium | 20.8 | $836 | ||
| Canada | 14.4 | $637 | ||
| Czech Republic | 14.9 | $286 | ||
| Denmark | 13.2 | $598 | ||
| Estonia | 18.6 | $242 | ||
| Finland | 19.6 | $645 | ||
| Germany | 13.1 | $581 | ||
| Hungary | 26.3 | $447 | ||
| Iceland | 18.2 | $619 | ||
| Ireland | 18.2 | $690 | ||
| Italy | 17.5 | $553 | ||
| Korea | 34.0 | $704 | ||
| Luxembourg | 9.6 | $448 | ||
| New Zealand | 10.5 | $318 | ||
| Portugal | 25.8 | $721 | ||
| Slovak Rep | 21.7 | $442 | ||
| Spain | 19.8 | $597 | ||
| Sweden | 16.3 | $613 | ||
| United Kingdom | 8.8 | $282 | ||
| OECD AVG | 19.0 |
All calculations from LIS data based on person‐weighted observations.
OECD Health Statistics 2014, available at http://stats.oecd.org/Index.aspx?DataSetCode=SHA. Per‐capita expressed in 2010 purchasing power parity dollars (PPP$). Data for Switzerland from 2004, expressed in 2004 PPP$; data for Japan from 2008, and expressed in 2008 PPP$. Russia data from World Bank available at http://data.worldbank.org/indicator/SH.XPD.OOPC.ZS.
Author calculation from LIS data, available from www.lisdatacenter.org. All amounts expressed in PPP$ for 2010, except for Switzerland (2004) and Japan (2008). PPP$ conversion based on OECD figures available at http://stats.oecd.org/Index.aspx?datasetcode=SNA_TABLE4.
Relying on the direct users of health care to pay some (or occasionally all) of their medical expenses can help reduce the moral hazard associated with insurance, and in many instances paying OOP can be fair as some expenses reflect individual preferences and income instead of medical necessity. Some forms of cost‐sharing can also improve efficiency if they reduce the administrative costs necessitated by third‐party payers.
Yet OOP requirements can also create inequitable burdens and unintended consequences. If large, they can require forgoing essential household spending, or incurring debt that could lead to bankruptcy (Himmelstein et al. 2009). Most troubling is when OOP requirements lead people needing medical care, pharmaceutical products, or other essential medical goods to delay, skip, or economize on them (Karaca‐Mandic et al. 2010; Wang et al. 2011; Balabanova et al. 2012; Eaddy et al. 2012), a consequence of cost‐sharing most common among the poor (Tamblyn et al. 2001; Chernew et al. 2008; Schoen et al. 2010; Lesen et al. 2013); elderly (Tamblyn et al. 2001), and those with chronic health problems (Rector and Venus 2004). Not only have OOP spending requirements been linked to the reduced use of medical services and poorer adherence to medication therapies, but they have also been shown to be associated with poorer health outcomes (Soumerai et al. 1991; Tamblyn et al. 2001; Heisler et al. 2010; Eaddy et al. 2012).
Theoretically, striking the right balance between efficiency and equity concerns suggests that OOP spending is more appropriate for the smaller and more certain expenses that can be anticipated, and for health expenses that might be considered more discretionary (Swartz 2010). Yet in practice such distinctions are often not obvious, and individuals infrequently have the right information to respond to cost‐sharing measures by weighing health benefits against their costs (Baiker and Goldman 2011). As a result, no consensus exists on how to ascertain when OOP spending requirements are too high; the most common practice (employed here) is to judge their collective effect based on the financial burden created (Cunningham 2009; Law et al. 2013; Collins et al. 2014; Schoen et al. 2014). This measure offers a straightforward gauge of citizens' protection from the risk of large medical bills, and the inequities in health care financing, access, and outcomes that can result when they are not. Among the poor and elderly, this measure is probably most appropriate as these groups are at greater risk for underutilizing health care when faced with cost‐sharing measures.
A common indicator of a household's exposure to high OOP expenses, sometimes referred to in the literature (and here as well) as underinsurance, is when these exceed a particular share of household income—most commonly 10 percent, and often less if the household is poor (Cunningham 2009; Schoen et al. 2010, 2014; Collins et al. 2014). This measure provides an indicator of the degree to which health care policy exposes citizens to a substantial financial risk associated with needing health care. By this or a similar measure, research shows that large numbers of Americans have such exposure; some estimate that 63 percent of America's poor households have high medical expenses relative to income (Schoen et al. 2014), while others find that 40 percent of nonelderly, poor adults with health insurance do (Collins et al. 2014). High OOP spending has been found to be especially common among poor Americans, those in poor health (Cunningham 2009), and the elderly (Marshall, McGarry, and Skinner 2010). Studies of the financial burden of OOP spending in other countries find that it is often high, and also that it varies significantly by country (Xu et al. 2007; Schoen et al. 2010; Tambor et al. 2011; Luczak and García‐Gómez 2012; Law et al. 2013).
The OECD and World Bank provide country‐level estimates of per‐capita OOP spending, a sample of which is presented in Table 1. However, these figures are based on nations' responses to health‐financing questionnaires, and the OECD's data sources do not permit disaggregating expenditures to the household level so that the incidence of high OOP spending within countries can be compiled and compared with one another. These sources thus do not allow comparing the size of OOP expenditures among vulnerable groups such as the elderly and poor.1
Such lack of comparable data hinders cross‐national research on the incidence of high OOP expenses. As a rare exception, Schoen et al. (2010) inquired into households' OOP spending in 11 countries, finding that high spending (above $1,000/year) was most common in the United States, with Switzerland a close second. Another international comparison used OOP spending data from a large international sample of hemodialysis patients, finding that among 11 countries, the average American patient paid twice the amount OOP for prescription medications than did the average patient in the other 10 countries (Hirth et al. 2008). Such limited examples suggest that the United States is an outlier when it comes to the financial burden citizens can face when meeting their health needs.
As pressure on private and social insurance schemes mount, it is increasingly important that assessments of national health care systems' performance include measures of high OOP spending. The purpose of this paper is to offer robust cross‐national comparison of high OOP expenses using nationally representative data from nine countries. Such comparative data can provide insight into the effect country‐level insurance policies have on the amount of financial protection provided citizens.
Methods
Data Source
To compare the frequency with which households in different countries encounter high OOP expenses, I draw on household survey (HS) data from the United States and eight other countries made available through the Luxembourg Income Study (LIS). LIS produces harmonized versions of national HSs by aligning their variables with international standards to facilitate cross‐national research. Numerous LIS datasets include households' OOP expenses; this paper excluded all those where LIS estimates were significantly different from OECD figures (Hungary and Italy), where countries used a definition of OOP spending that deviated significantly from LIS's (Taiwan and Canada), where the most recent HS was over a decade old (Estonia and Romania), and where the country's income was low relative to the United States (China, Guatemala, India, Mexico, Peru, Serbia, and South Africa). This left nine countries remaining: France, Australia, Israel, Japan, Poland, Russia, the United States, Slovenia, and Switzerland. For all countries except Japan (2008) and Switzerland (2004), the HS data are from 2010. As can be seen in Table 1, the sample of countries used in this study are somewhat representative of the range and distribution of OOP spending found in different countries. In this study, the United States and Switzerland are at the high end of OOP expenditures, with spending levels similar to those in Greece, Korea, Portugal, and Belgium. Japan and Australia fall in the mid‐range of OOP requirements, with levels similar to those in Canada, Denmark, Finland, Italy, and Germany. France and Slovenia represent the low end in this study; their OOP spending levels are similar to those in Luxembourg, New Zealand, and the United Kingdom.
Data Description
LIS's data for the United States originate with the Current Population Survey's Annual Social and Economic Supplement (CPS). CPS's household health spending data have been found to be comparable in quality to that contained in the Medical Expenditure Panel Survey (MEPS) (Caswell and O'Hara 2010). In addition, the CPS data are superior to MEPS in two regards: its sample size is five times larger, and it contains much more detailed and accurate information on household income (Caswell and O'Hara 2010). Other nations' HS data come from nationally representative surveys designed to provide official estimates of household income and (for some) consumption patterns. The number of individuals in each survey ranges from 7,938 in Switzerland to 203,799 in the United States, and all results reported here are based on person‐level weights assigned for making national‐level estimations. Table 2 presents detail on each country's dataset and variables.
Table 2.
Sources of National Data, Notes, and Percent of Population by Income Category
| Country | Data Source | Year | Number Observations Used/Total | Universe | Percent of Population | ||
|---|---|---|---|---|---|---|---|
| Extreme Poverty | Poverty | NearPoor | |||||
| Australia | Australian Bureau of Statistics Household Expenditure Survey and Survey of Income and Housing | 2010 | 22,087/42,595 | Residents of private dwellings, excluding households with members of non‐Australian defense forces, and households with diplomatic personnel. | 6% | 21% | 29% |
| France | Institut National de la Statistique et des Etudes Economiques Enquête “Budget de Famille” | 2010 | 40,854/41,285 | Excludes collective households (such as hospices, religious communities, university campuses, workers dormitories, prisons, etc.) and persons without a residence. | 5% | 16% | 34% |
| Israel | Central Bureau of Statistics Household Expenditure Survey | 2010 | 20,203/20,225 | Excludes residents for kibbutzim, collective moshavim and Bedouins living outside of localities. | 12% | 28% | 22% |
| Japan | Keio University Joint Research Center for Panel Studies Japan Household Panel Survey | 2008 | 10,852/14,575 | Excludes households in which the oldest member is under the age of 20. | 7% | 18% | 32% |
| Poland | Central Statistical Office Household Budget Survey | 2010 | 107,147/107,967 | Excludes collective households (e.g., students' hostels, social welfare homes) and household of foreigners | 5% | 16% | 34% |
| Russia | National Research University Higher School of Economics Russia Longitudinal Monitoring Survey‐Higher School of Economics | 2010 | 15,081/16,867 | Excludes military, penal, and other institutionalized populations. | 6% | 16% | 34% |
| Slovenia | Statistical Office of the Republic of Slovenia Household Budget Survey | 2010 | 11,514/11,515 | Excludes collective households such as boarding schools, nursing homes for children, old people's homes, hospitals, homes for pupils, student hostels, etc. | 10% | 21% | 29% |
| Switzerland | Federal Statistical Office Income and Expenditure Survey | 2004 | 7,938/7,993 | Excludes border residents, foreign tourists, and collective households (e.g., prisons). | 4% | 15% | 35% |
| United States | United States Census Bureau Current Population Survey Annual Social and Economic Supplement | 2010 | 203,799/204,983 | Civilian noninstitutional population in the United States. | 11% | 24% | 26% |
Calculations are based on weighted values using LIS's ppopwgt variable. Out‐of‐pocket spending is LIS variable hmcmed or hcmed. All negative values for disposable income (dhi) or out‐of‐pocket spending (hcmed or hmcmed) bottom‐coded to zero.
Definitions
Out‐of‐Pocket Spending
Out‐of‐pocket medical spending is most frequently measured by the costs to individuals of purchasing medical goods and services through copays, coinsurance, and deductibles; the expenses of those without health insurance; and the cost of goods and services not covered by insurance. The LIS OOP variable “consumption of health” used here measures total household expenditures on medical products, appliances, and equipment, outpatient services and hospital services, and excludes payments for health insurance; its definition is consistent with that in the United Nation's Classification of Individual Consumption According to Purpose. Where possible, LIS verifies or modifies national datasets so that each complies with this definition.2
Because of potential inconsistencies or inaccuracies in households' estimate of their OOP spending (Heijink et al. 2010), LIS estimates of per‐capita OOP spending (Table 1, Column 3) are compared with those reported by the OECD (or in the case of Russia, the World Bank) (Column 2). Column 4 shows LIS's estimates relative to the OECD's. As shown, LIS's estimates fall between 68 and 96 percent of the OECD's. These discrepancies are likely explained by two important differences between the two sources: HSs such as those provided by LIS generally exclude the institutionalized population (e.g., those in long‐term care facilities) and individuals who died earlier in the year. These two populations commonly have large OOP expenses (Marshall, McGarry, and Skinner 2010; Cubanski et al. 2014). For this reason, the paper's estimates likely underestimate the incidence of high OOP spending, particularly among the elderly populations. However, it is also true that OECD's estimates of OOP spending have their own shortcomings as Calcoen et al. (2015) discuss.
Income
To measure household resources available to pay OOP medical expenses, I use income defined as disposable income, meaning income after accounting for both government taxes and cash and near‐cash social transfers. This adjustment is especially important for the elderly and poor, as many of them are heavily dependent on cash and near‐cash transfers (rather than earned income) for their income. As with OOP spending, disposable income is measured at the household level.
A second use of income is for partitioning each nation's population into distinct income categories to examine differences in the burden medical spending places on each. To this end, I classify each country's population into four income categories, and place individuals into them based on their equivalized household disposable income (disposable income divided by the square root of household size), an adjustment that accounts for economies of scale in household size. As all members of the same household have identical values of equivalized household disposable income, each is placed in the same income category. The four categories are “extreme poverty” (equivalized disposable income below 40 percent of the nation's median value); “poverty” (income below 60 percent of the median, and thus including those in extreme poverty)3; the “near poor” (those with income falling within 60–100 percent of median income); and “above‐median income” (the top 50 percent of the population). Table 2 columns 5–7 show the percentage of citizens in each country falling within each income category.
High Medical Expenses
High OOP spending (also referred to as underinsurance) is measured by calculating each household's health expenses as a share of its disposable income. If this ratio exceeds 10 percent, or 5 percent if the household is in poverty as defined above—then all individuals in the household are regarded as having high medical expenses (i.e., being underinsured). This way of measuring high OOP spending is conservative because it employs an ex‐post definition rather than citizens' ex‐ante risk of having high medical expenses. It also entails an arbitrary division between the “poor” and the “nonpoor”: someone with 59 percent of median income is poor, whereas another with 61 percent is not. The measure also does not capture those who register low OOP spending because they defer or forgo medical treatment rather than pay the cost. This is an important omission, as Abraham, DeLeire, and Royalty (2010) estimate that many individuals in the United States with less generous insurance benefits register low OOP spending only because they forgo health care rather than pay for it out‐of‐pocket. Finally, as discussed above, LIS estimates of OOP spending are below the OECD's, and therefore likely underestimate the phenomenon of high OOP medical spending, particularly among the elderly.
The measurement of high spending used could also overestimate its incidence for several reasons. One, I do not consider household wealth, and especially among the elderly, wealth can make otherwise high levels of OOP expenses affordable. Two, I only measure OOP spending for a single year, and many households may be capable of smoothing out 1 year of high medical expenses. High OOP spending is most problematic when it is either very high, or persists over time, and the estimates here take no account of such distinctions (Cohen and Yu 2012). Finally, I do not distinguish between unpredictable and unknown levels of OOP spending that may soar significantly above the income threshold, and those that are predictable in type (e.g., a high deductible), and that could involve some degree of discretion in amount. In some countries, OOP requirements predominantly fall into the latter category, with OOP spending primarily taking the form of expenditures on eyewear, hearing products, and dental care. However, in most OECD countries, OOP medical expenses are most commonly spent on prescription drugs and rehabilitative services (OECD 2013).
Age
The paper investigates high spending among the elderly (65 years and over) and nonelderly population (below 65 years ); among the elderly, it further distinguishes between 65‐ to 74‐year olds and those 75 years and over.
Results
National
Figure 1 presents country‐level estimates of the frequency of high OOP medical expenses in each of the nine countries. As shown, in five nations, more than 10 percent of individuals lived in households with high medical spending (United States, Poland, Israel, Switzerland, and Russia), and only in France (2.9 percent) did less than 5 percent of the population incur high OOP expenses.
Figure 1.
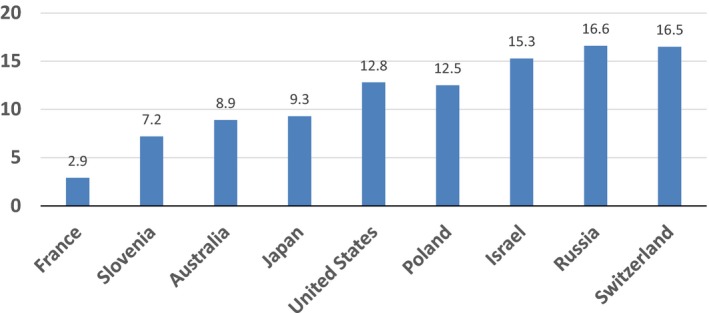
Percent of Citizens with High Out‐of‐Pocket Health Expenditures, by Country and Select Year
Source: Author calculation from LIS data (www.lisdatacenter.org). Based on weighted observations. Year is 2010 except for Japan (2008) and Switzerland (2004).
Notes: High OOP defined as above 10% of household income, or 5% if poor. Poverty, income, and OOP defined in text.
By Income
To investigate the burden OOP requirements place on vulnerable populations, I first examine its incidence by income, and then among the elderly versus nonelderly populations. These two populations are especially vulnerable in part because OOP requirements can compound other challenges they face in gaining adequate access to health care.
To distinguish by income, I calculate high spending rates for those in each of the four income groups previously defined. Table 3 presents these rates for each of the nine countries. As shown, the frequency with which high OOP spending occurs increases as household income falls. The significantly lower rates among the near poor compared with the poor is partially due to measurement choice (spending exceeding 10 percent of income among the former but only 5 percent among the latter). However, in all countries underinsurance rates (the percentage spending above a threshold level of income) are lower among those with above‐median income compared with the near poor, and only in Israel are rates among those in extreme poverty slightly below the rate of those in poverty—although this may reflect underutilization of services rather than superior insurance coverage.
Table 3.
Percent of Population with High OOP Spending, Overall and by Age and Incomea
| United States | France | Australia | Japan | Poland | Switzerland | Israel | Russia | Slovenia | |
|---|---|---|---|---|---|---|---|---|---|
| % High spendingb | 12.8 | 2.9 | 8.9 | 9.3 | 12.5 | 16.5 | 15.3 | 16.6 | 7.2 |
| Age (years) | |||||||||
| Below 65 | 10.9 | 2.7 | 6.8 | 8.1 | 9.9 | 13.3 | 13.7 | 15.0 | 5.9 |
| 65–74 | 18.2 | 2.7 | 21.4 | 15.8 | 29.3 | 30.3 | 27.7 | 26.0 | 15.0 |
| Above 75 | 23.2 | 5.4 | 25.5 | 12.1 | 33.8 | 43.2 | 33.2 | 25.6 | 13.1 |
| Incomec | |||||||||
| Extreme poverty | 32.3 | 17.4 | 38.0 | 40.0 | 34.0 | 34.5 | 32.4 | 36.8 | 31.4 |
| Poverty | 28.7 | 11.5 | 26.7 | 29.6 | 31.9 | 33.5 | 34.0 | 35.3 | 22.4 |
| Near poverty | 11.1 | 1.9 | 5.3 | 5.7 | 12.1 | 17.5 | 12.0 | 15.4 | 6.7 |
| Above median | 4.8 | 1.0 | 3.5 | 4.4 | 6.8 | 11.0 | 6.2 | 8.6 | 2.9 |
All data for 2010 except Japan (2008) and Switzerland (2004).
High spending is spending in excess of 10% of disposable income, or 5% if household income is below the poverty threshold.
Income is defined as household disposable income. Extreme poverty is equivalized disposable income equalling 40% or less of equivalized median disposable income. Poverty is 60% or less. Near poverty is 60%–100% of median disposable income.
Source: Author calculations from LIS data (www.lisdatacenter.org). Health expenses is the LIS variable hcmed or hcmmed.
Table 3 shows that pronounced income‐based differences in high spending rates exist in every country. The difference in rates among those in extreme poverty and those with above‐median income is lowest in France (16 percentage points larger) and largest in Japan and Australia (36 and 35 percentage point difference, respectively); the United States (28 percentage point difference between the two income groups) is just above the average in the nine countries. In absolute terms, the poor in France were the least likely to have high medical expenses (11.5 percent), while the poor in Russia were the most (35.3 percent).
In sum, paying at the point of consumption for medical goods and services places a very large financial burden on poor Americans, as 29 percent of those in poverty had high medical expenses in 2010. But the United States is not alone. The frequency of high spending among America's poor is equal to its frequency in Japan and Australia, but high spending among the poor is even more common in Israel, Poland, and Switzerland. Only in France (11.5 percent) and to a much lesser extent Slovenia (22.4 percent) were significantly fewer poor citizens exposed to high medical expenses at the point of consumption than were America's poor.
By Age
Table 3 presents a comparison of high spending rates among the nonelderly (below 65), the young‐elderly (between 65 and 74), and the old‐elderly (75 and above). With two minor exceptions (Slovenia and Japan), high spending rates increase with age, with the difference between the nonelderly and those 75 years and older most pronounced in Switzerland (30 percentage point difference) and Poland (24 percentage points). Unlike with income, however, age‐related differences in the incidence of high medical expenses are not large in some countries: in France, Slovenia, and Japan, the high spending rates among the elderly are less than 10 percentage points above those of the nonelderly. And while 18 percent of Americans aged 65‐ to 74‐year olds were underinsured, this rate is similar to what I find in Japan and Australia, while rates in Poland, Russia, Israel, and Switzerland are even higher. France (3 percent) had the fewest high spenders among this age group, followed by Slovenia (15 percent).
Discussion
This study provides some of the best comparative evidence to date of variation within and between countries of the percentage of citizens exposed to high OOP medical expenses. The results foremost underscore the very high financial burden that using health care places on many Americans.
But unlike other studies, I also find that high spending among poor and elderly Americans is equally common among their counterparts in many other countries. In seven of the nine countries (United States, Japan, Australia, Poland, Israel, Russia, and Switzerland), one‐quarter or more of poor citizens devoted at least 5 percent of their income to OOP expenses; and in all nine countries, at least one‐in‐ten poor citizens did. Underinsurance rates among the elderly were somewhat lower than among the poor, yet the results show that one‐in‐four elderly citizen had high OOP expenditures in Switzerland, Russia, Poland, and Israel, while more than 15 percent did in Australia, Slovenia, Japan, and the United States.
Prior cross‐national research indicates Americans are more exposed to high OOP spending than those in other nations (Hirth et al. 2008; Schoen et al. 2010), a finding perhaps consistent with America's uniquely large number of uninsured citizens. But this study shows that high OOP expenses are usual in many countries. The common magnitude of these expenses is especially concerning given that my estimates likely underestimate, perhaps by a considerable degree, citizens' true exposure to the financial risk associated with meeting one's health care needs. While the results indicate that France and to a lesser extent Slovenia provide their citizens with significant financial protection from this risk, the findings here suggest this may be an exception rather than a typical feature of countries' health insurance design. Clearly, the results of this study cannot be generalized to more than the sample of countries in it; however, as shown earlier in Table 1, the countries included in this study are fairly representative of the range and diversity of OOP spending in developed countries.
That high OOP spending in the United States is on par with its scale in about half of the study's countries could nonetheless overlook the extreme levels of spending to which Americans are uniquely exposed, or the especially unpredictable nature of OOP spending in the United States. Regarding the first point, Table 4 displays OOP spending by income and age, measured at the 50th, 75th, and 90th percentiles. Even when compared at the high end of the spending spectrum, France stands out for requiring much lower OOP health care expenses than do the other eight countries. And the amount spent by poor and elderly citizens in the United States at the 75th and even 90th percentile of spending is similar to amounts spent by their counterparts in many of the other sample countries. In short, examining the tail ends of the distribution does not suggest the findings here should obviously be viewed with caution. The only qualification is that it is possible that America's extreme tail of the OOP spending distribution lies significantly beyond those in other countries (see Marshall, McGarry, and Skinner 2010; Cohen and Yu 2012). It is hence possible that the comparison here based primarily on the extent of high OOP spending could overlook differences in the intensity of the phenomenon, despite the evidence in Table 4 suggesting otherwise.
Table 4.
OOP Spending as a Percent of Income at Different Spending Percentiles, by Income, Age, and Country
| United States | France | Australia | Japan | Poland | Switzerland | Israel | Russia | Slovenia | |
|---|---|---|---|---|---|---|---|---|---|
| 50 percentile | |||||||||
| Age (years) | |||||||||
| Below 65 | 1.5 | 0.8 | 1.2 | 1.4 | 1.9 | 0.7 | 1.5 | 1.5 | 0.7 |
| 65–74 | 1.5 | 0.8 | 2.8 | 2.2 | 5.3 | 2.3 | 3.2 | 3.6 | 1.2 |
| Above 75 | 2.7 | 0.9 | 2.8 | 1.9 | 6.2 | 5.0 | 3.6 | 3.6 | 0.9 |
| Income | |||||||||
| Extreme poverty | 2.1 | 0.7 | 2.9 | 3.7 | 1.9 | 1.8 | 2.2 | 1.7 | 0.0 |
| Poverty | 1.9 | 0.7 | 1.7 | 2.9 | 2.1 | 1.4 | 2.4 | 2.0 | 0.0 |
| Near poverty | 1.9 | 0.9 | 1.4 | 1.8 | 2.4 | 0.9 | 1.7 | 2.1 | 0.6 |
| Above median | 1.4 | 0.7 | 1.2 | 1.3 | 2.1 | 0.8 | 1.3 | 1.5 | 0.8 |
| 75 percentile | |||||||||
| Age (years) | |||||||||
| Below 65 | 3.9 | 1.7 | 2.9 | 2.8 | 4.5 | 4.0 | 4.2 | 4.8 | 2.5 |
| 65–74 | 6.1 | 1.6 | 5.6 | 4.9 | 10.3 | 11.6 | 8.7 | 8.7 | 4.6 |
| Above 75 | 7.3 | 2.4 | 6.3 | 4.2 | 11.8 | 20.8 | 9.9 | 8.8 | 4.2 |
| Income | |||||||||
| Extreme poverty | 7.5 | 3.1 | 9.0 | 8.9 | 7.9 | 11.1 | 7.2 | 10.0 | 8.3 |
| Poverty | 6.0 | 2.4 | 5.3 | 5.9 | 6.6 | 9.2 | 7.3 | 8.6 | 3.7 |
| Near poverty | 5.0 | 2.1 | 3.4 | 3.3 | 5.9 | 6.0 | 5.0 | 6.5 | 3.1 |
| Above median | 3.3 | 1.5 | 2.7 | 2.3 | 4.5 | 4.0 | 3.4 | 4.2 | 2.3 |
| 90 percentile | |||||||||
| Age (years) | |||||||||
| Below 65 | 8.7 | 3.6 | 6.3 | 6.0 | 8.5 | 12.1 | 9.5 | 11.4 | 5.9 |
| 65–74 | 13.3 | 4.0 | 11.6 | 10.4 | 16.5 | 36.1 | 18.2 | 17.2 | 11.4 |
| Above 75 | 15.6 | 5.1 | 11.7 | 8.7 | 18.7 | 58.0 | 21.4 | 17.7 | 10.2 |
| Income | |||||||||
| Extreme poverty | 25.9 | 8.5 | 29.4 | 27.1 | 20.8 | 46.1 | 18.1 | 33.3 | 30.5 |
| Poverty | 17.3 | 5.7 | 11.9 | 13.8 | 14.4 | 31.7 | 17.3 | 21.4 | 12.3 |
| Near poverty | 10.7 | 4.1 | 6.6 | 6.4 | 11.0 | 18.6 | 12.0 | 16.0 | 7.1 |
| Above median | 6.7 | 3.0 | 5.2 | 4.6 | 8.2 | 11.3 | 7.2 | 9.1 | 5.2 |
See Table 3.
A separate reason why this paper may not adequately capture the particularly large burden health care financing in the United States places on individuals is that the country‐level comparisons are based on nonpremium OOP spending, which sidesteps Americans' large expenditures on private health insurance premiums. Indeed, private insurance pays 35 percent of America's health expenses, while it pays less than 10 percent of total costs in five of the other eight countries in this study. It could be, then, that a more accurate cross‐national comparison of health care's financial burden should include Americans' distinctly high expenditures on insurance premiums. However, this issue raises the more general one of how health care is financed and the distributional implications of different financing mechanisms, a topic addressed elsewhere (Wagstaff et al. 1999; Waters, Anderson, and Mays 2004) and beyond this paper's scope. Rather, the paper's focus has been strictly on the costs associated with using health care services and purchasing medical products, costs that bear directly on health care access.
A final possible shortcoming in this cross‐national comparison is that the “high spending” measure used in this paper is a crude one. It is common in the literature in large part because it is straightforward to measure. But it misses the possibly large number of citizens forgoing health care because of its cost, as Abraham, DeLeire, and Royalty (2010) clearly show. Moreover, it does not distinguish among possible differences among countries in how citizens incur OOP expenses: OOP spending requirements for optional medical products are quite different in effect than are required payments for life‐saving and life‐lengthening drug therapies, for instance. A better understanding of how countries compare on these two issues would improve comparative assessments of nations' cost‐sharing practices, and this deserves prioritization.
Conclusions
Evidence consistently shows that cost‐sharing requirements can cause individuals to forgo health care and skip or economize on recommended drug therapies, and cost‐related nonadherence has been shown to have important medical consequences. For this reason, the magnitude of high medical spending uncovered—estimates that likely underestimate its true size—implicates OOP requirements not just in financing inequities but also in countries' inequitable access to health care and the uneven medical outcomes documented elsewhere (van Doorslaer, Masseria, and Koolman 2006; Mackenbach et al. 2008; OECD 2013). As pressure on private and social insurance schemes mount, assessments of national health care systems' performance should include measures of high OOP spending. Advancing the goals of financing equity as well as equality in access and outcomes depends on ensuring that the pressure for high OOP spending does not undermine these essential features of nations' health care systems. This indicates a need, at least for some populations, to expand insurance protection, especially as evidence indicates that the deterrence effect of OOP requirements is stronger where the cumulative burden of OOP spending is higher (Karaca‐Mandic et al. 2010).
The widespread feature of the findings also underscores a clear need to better monitor and prioritize the dissemination of information on the prevalence of high medical spending, a conclusion that holds true for a large number of countries. Such monitoring, though, requires grappling with defining when high OOP becomes excessive. To do this requires collecting much more detailed data than is currently available. Developing improved measures and data sources allowing cross‐national comparisons of how OOP requirements influence access would better ensure that the tension between the policy objectives of affordability and reduced consumer demand, are appropriately balanced with the goals of financing equity and equal access. It would also permit countries, even those with very different health care systems, to gain insights into how best to structure insurance policies and coverage, especially for vulnerable groups.
The finding that the United States is not an outlier when it comes to the financial burden resulting from health care consumption in the sample of countries here highlights the fact that health insurance in many countries is commonly porous: high levels of OOP spending frequently occur in many countries despite universal insurance and the existence of policies that supposedly limit citizens' financial exposure (Paris, Devaux, and Wei 2010; Zare and Anderson 2013; Commonwealth Fund 2013). The complicated nature of health care and health insurance benefits; the complex ways in which consumers respond to insurance benefits and their limits; and finally the often significant health risks not covered by insurance policies: all of these combine to leave large numbers of people across many countries devoting considerable resources to meeting their health care needs (see Domenighetti et al. 2010; Law et al. 2013; and Rosenthal 2015). Considering this evidence, then, solving the problem of the uninsured in the United States will most likely leave standing the separate one of underinsurance, unless policy explicitly seeks to tackle them both.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: The University of Washington Tacoma's School of Interdisciplinary Arts and Sciences provided financial support, and the Luxembourg Income Study (LIS) provided training and technical support with the data. Teresa Munzi of LIS deserves special thanks for her interest in the project and unending assistance explaining complications in the datasets.
Disclosures: None.
Disclaimers: None.
Notes
Personal email communication, Michael Mueller, Health Policy Analyst, OECD's Health Division, February 4, 2015.
Personal email communication, Teresa Munzi, Data Team Manager and Research Associate, Luxembourg Income Study, February 27, 2015.
In the United States, this threshold equals about 162 percent of the 2010 federal poverty level.
References
- Abraham, J. M. , DeLeire T., and Royalty A. B.. 2010. “Moral Hazard Matters: Measuring Relative Rates of Underinsurance Using Threshold Measures.” Health Services Research 45 (3): 806–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baiker, K. , and Goldman D.. 2011. “Patient Cost‐Sharing and Healthcare Spending Growth.” Journal of Economic Perspectives 25 (2): 47–68. [DOI] [PubMed] [Google Scholar]
- Balabanova, D. , Roberts B., Richardson E., Haerpfer C., and McKee M.. 2012. “Health Care Reform in the Former Soviet Union: Beyond the Transition.” Health Services Research 47 (2): 840–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calcoen, P. , Moens D., Verlinden P., van de Ven W. P. M. M., and Pocolet J.. 2015. “Improved Estimates of Belgian Private Health Expenditure Can Give Important Lessons to Other OECD Countries.” Health Policy 119: 341–55. [DOI] [PubMed] [Google Scholar]
- Caswell, K. J. , and O'Hara B.. 2010. Medical Out‐of‐pocket Expenses, Poverty, and the Uninsured. Washington, DC: US Bureau of the Census. [Google Scholar]
- Chernew, M. , Gibson T. B., Yu‐Isenberg K., Sokol M. C., Rosen A. B., and Fendrick A. M.. 2008. “Effects of Increased Patient Cost Sharing on Socioeconomic Disparities in Health Care.” Journal of General Internal Medicine 23 (8): 1131–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen, S. , and Yu W.. 2012. The Concentration and Persistence in the Level of Health Expenditures over Time. Rockville, MD: Agency for Healthcare Research and Quality; [accessed on October 25, 2014]. Available at http://www.meps.ahrq.gov/mepsweb/data_files/publications/st354/stat354.pdf [Google Scholar]
- Collins, S. R. , Rasmussen P. W., Doty M. M., and Beutel S.. 2014. Too High a Price: Out‐of‐Pocket Health Care Costs in the United States. New York: Commonwealth Fund; November 2014. [accessed on January 27, 2015]. Available at http://www.commonwealthfund.org/publications/issue-briefs/2014/nov/out-of-pocket-health-care-costs [PubMed] [Google Scholar]
- Commonwealth Fund . 2013. International Profiles of Health Care Systems. New York: Commonwealth Fund; [accessed on November 4, 2015]. Available at http://www.commonwealthfund.org/~/media/Files/Publications/Fund%20Report/2013/Nov/1717_Thomson_intl_profiles_hlt_care_sys_2013_v2.pdf [Google Scholar]
- Cubanski, J. , Swoope C., Damico A., and Neuman T.. 2014. How Much Is Enough? Out‐of‐Pocket Spending among Medicare Beneficiaries. Washington, DC: Kaiser Family Foundation; [accessed on January 20, 2015]. Available at http://kff.org/health-costs/report/how-much-is-enough-out-of-pocket-spending-among-medicare-beneficiaries-a-chartbook/ [Google Scholar]
- Cunningham, P. J. 2009. Chronic Burdens: The Persistently High OOP Health Care Expenses Faced by Many Americans with Chronic Conditions. New York: Commonwealth Fund; [accessed on March 9, 2015]. Available at http://www.commonwealthfund.org/publications/issue-briefs/2009/jul/chronic-burdens-the-persistently-high-out-of-pocket-health-care-expenses-faced-by-many-americans [PubMed] [Google Scholar]
- Domenighetti, G. , Vineis P., De Pietro C., and Tomada A.. 2010. “Ability to Pay and Equity in Access to Italian and British National Health Services.” European Journal of Public Health 20 (5): 500–3. [DOI] [PubMed] [Google Scholar]
- van Doorslaer, E. , Masseria C., and Koolman X.. 2006. “Inequalities in Access to Medical Care by Income in Developed Countries.” Canadian Medical Association Journal 174 (2): 177–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaddy, M. T. , Cook C. L., O'Day K., Burch K. P., and Cantrell C. R.. 2012. “How Patient Cost‐sharing Trends Affect Adherence and Outcomes.” P T 37 (1): 45–55. [PMC free article] [PubMed] [Google Scholar]
- Heijink, R. , Xu K., Saksena P., and Evans D.. 2010. Validity and Comparability of Out‐of‐Pocket Health Expenditure from Household Surveys. WHO Discussion Paper. New York: World Health Organization. [Google Scholar]
- Heisler, M. , Choi H., Rosen A. B., Vijan S., Kabeto M., Langa K. M., and Piette J. D.. 2010. “Hospitalizations and Deaths among Adults with Cardiovascular Disease Who Underuse Medications Because of Cost: A Longitudinal Analysis.” Medical Care 48 (2): 87–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Himmelstein, D. , Thorne D., Warren E., and Woolhandler S.. 2009. “Medical Bankruptcy in the United States, 2007: Results of a National Study.” American Journal of Medicine 122 (8): 741–6. [DOI] [PubMed] [Google Scholar]
- Hirth, R. A. , Greer S., Albert J. M., Young E. W., and Piette J. D.. 2008. “OOP Spending and Medication Adherence among Dialysis Patients in Twelve Countries.” Health Affairs 27 (1): 89–102. [DOI] [PubMed] [Google Scholar]
- Kaiser Family Foundation . 2014. Employer Health Benefits, 2014 Annual Survey. Washington, DC: Kaiser Family Foundation; [accessed on March 12, 2015]. Available at http://kff.org/health-costs/report/2014-employer-health-benefits-survey/ [Google Scholar]
- Karaca‐Mandic, P. , Joyce G. F., Goldman D. P., and Laouri M.. 2010. “Cost Sharing, Family Health Care Burden, and the Use of Specialty Drugs for Rheumatoid Arthritis.” Health Services Research 45 (5 Pt 1): 1227–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Law, M. R. , Daw J. R., Cheng L., and Morgan S. G.. 2013. “Growth in Private Payments for Health Care by Canadian Households.” Health Policy 110: 141–6. [DOI] [PubMed] [Google Scholar]
- Lesen, E. , Sundell K. A., Carlsten A., Mardby A. C., and Jonsson A. K.. 2013. “Is the Level of Patient Co‐Payment for Medicines Associated with Refill Adherence in Sweden?” European Journal of Public Health 24 (1): 85–90. [DOI] [PubMed] [Google Scholar]
- Luczak, J. , and García‐Gómez P.. 2012. “Financial Burden of Drug Expenditures in Poland.” Health Policy 105: 256–64. [DOI] [PubMed] [Google Scholar]
- Mackenbach, J. P. , Stirbu I., Roskam A. J., Schaap M. M., Menvielle G., Leinsalu M., and Kunst A. E., 2008. “Socioeconomic Inequalities in Health in 22 European Countries.” New England Journal of Medicine 358: 2468–81. [DOI] [PubMed] [Google Scholar]
- Marshall, S. , McGarry K. M., and Skinner J. S.. 2010. The Risk of OOP Health Care Expenditure at End of Life. Cambridge: NBER. [Google Scholar]
- OECD . 2013. Health at a Glance 2013: OECD Indicators. Paris: OECD; [accessed on January 12, 2015]. Available at http://dx.doi.org/10.1787/health_glance-2013-en [Google Scholar]
- OECD . 2014. Out‐of‐Pocket Expenditure on Health Per Capita, In Health: Key Tables from OECD, No. 6. Paris: OECD; [accessed on June 22, 2015]. Available at http://dx.doi.org/10.1787/oopexphtlca-table-2014-1-en [Google Scholar]
- Paris, V. M. , Devaux M., and Wei L.. 2010. Health Systems Institutional Characteristics: A Survey of 29 OECD Countries. Paris: OECD; [accessed on August 3, 2014]. Available at http://dx.doi.org/10.1787/5kmfxfq9qbnr-en [Google Scholar]
- Rector, T. S. , and Venus P. J.. 2004. “Do Drug Benefits Help Medicare Beneficiaries Afford Prescribed Drugs?” Health Affairs 23 (4): 213–22. [DOI] [PubMed] [Google Scholar]
- Rosenthal, E. February 7, 2015. “Insured But Not Covered.” New York Times [accessed on March 27, 2015]. Available at http://www.nytimes.com/2015/02/08/Sunday-review/insured-but-not-covered.html?_r=0 [Google Scholar]
- Schoen, C. , Osborn R., Squires D., Doty M., Pierson R., and Applebaum S.. 2010. “How Health Insurance Design Affects Access to Care and Costs, by Income, in Eleven Countries.” Health Affairs 29 (12): 2323–34. [DOI] [PubMed] [Google Scholar]
- Schoen, C. , Hayes S. L., Collins S. R., Lippa J. A., and Radley D. C.. 2014. America's Underinsured. New York: Commonwealth Fund. [Google Scholar]
- Soumerai, S. B. , Ross‐Degnan D., Avorn J., McLaughlin T. J., and Choodnovskiy I.. 1991. “Effect of Medicaid Drug‐Payment Limits on Admission to Hospitals and Nursing Homes.” New England Journal of Medicine 325: 1072–7. [DOI] [PubMed] [Google Scholar]
- Swartz, K. 2010. Cost‐Sharing: Effects on Spending and Outcomes. The Synthesis Project, Issue 20. Princeton, NJ: Robert Wood Johnson Foundation. [PubMed] [Google Scholar]
- Tamblyn, R. , Laprise R., Hanley J. A., et al. 2001. “Adverse Events Associated with Prescription Drug Cost Sharing among Poor and Elderly Persons.” Journal of the American Medical Association 285: 421–9. [DOI] [PubMed] [Google Scholar]
- Tambor, M. , Pavolova M., Woch P., and Groot W.. 2011. “Diversity and Dynamics of Patient Cost Sharing.” European Journal of Public Health 21 (5): 585–90. [DOI] [PubMed] [Google Scholar]
- Wagstaff, A. , van Doorslaer E., van der Burg H., et al. 1999. “Equity in the Finance of Health Care: Some Further International Comparisons.” Journal of Health Economics 18: 263–90. [DOI] [PubMed] [Google Scholar]
- Wang, V. , Liu C. F., Bryson C. L., Sharp N. D., and Maciejewski M. L.. 2011. “Does Medication Adherence Following a Copayment Increase Differ by Disease Burden?” Health Services Research 46 (6 Pt 1): 1963–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waters, H. R. , Anderson G. F., and Mays J.. 2004. “Measuring Financial Protection in Health in the United States.” Health Policy 69: 339–49. [DOI] [PubMed] [Google Scholar]
- Xu, K. , Evans D. B., Carrin G., Aquilar‐Rivera A. M., Musgrove P., and Evans T.. 2007. “Protecting Households from Catastrophic Health Spending.” Health Affairs 26 (4): 972–83. [DOI] [PubMed] [Google Scholar]
- Zare, H. , and Anderson G.. 2013. “Trends in Cost Sharing Among Select High Income Countries—2000‐2010.” Health Policy 112: 35–44. [DOI] [PubMed] [Google Scholar]


