Abstract
OBJECTIVE
To examine current levels, current correlates of, and changes in long-acting reversible contraceptive (LARC) use, including intrauterine devices and implants, among females aged 15–44 years using contraception between 2008–2010 and 2011–2013 with specific attention to associations between race, income, and age and their LARC use.
METHODS
We analyzed data from two rounds of the National Survey of Family Growth, nationally representative samples of females aged 15–44 years, consisting of 6,428 females in 2008–2010 and 5,601 females in 2011–2013. We conducted simple and multivariable logistic regression analyses with adjustments for the sampling design to identify demographic characteristics predictive of LARC use and changes in these patterns between the two time periods. In this cross-sectional, descriptive study, our primary outcome of interest was current prevalence of LARC use among all contraceptive users at the time of the interview.
RESULTS
The prevalence of LARC use among contracepting U.S. females increased from 8.5% in 2009 to 11.6% in 2012 (P<.01). The most significant increases occurred among Hispanic females (from 8.5% to 15.1%), those with private insurance (7.1–11.1%), those with fewer than two sexual partners in the previous year (9.2–12.4%), and those who were nulliparous (2.1–5.9%) (all P<.01). In multivariable analyses adjusting for key demographic characteristics, the strongest associations with LARC use in 2012 were parity (adjusted odds ratios [ORs] 4.3–5.5) and having a history of stopping non-LARC hormonal use (adjusted OR 1.9). Women aged 35–44 years (adjusted OR 0.3) were less likely to be LARC users than their counterparts (all P<.001). Poverty status was not associated with LARC use. There were no differences in discontinuation of LARC methods resulting from dissatisfaction between minority women and non-Hispanic white women.
CONCLUSION
During the most recent time period surveyed, use of LARC methods, particularly intrauterine devices, increased almost uniformly across the population of users.
Long-acting reversible contraceptive (LARC) methods, including intrauterine devices (IUDs) and subdermal hormonal implants, are some of the most effective contraceptive methods available.1 From 2002 to 2009, the percentage of U.S. females using contraception aged 15–44 years currently using LARC methods increased from 2.4% to 8.5%, including a sixfold increase among white females and a fourfold increase among black females.2
Given the efficacy, benefits, and acceptability of LARC methods among users, many in the women’s health field see the increase in use of these methods as promising for women who seek to avoid pregnancy.1,3 At the same time, many other voices have cautioned that promoting LARC methods to “at-risk” women may disproportionately target minority, poor, and young women, further devalue their childbearing, or disregard the root causes of health inequalities that drive disparities in unintended pregnancies.4–6 It is therefore important to gain a deeper understanding of which groups of women are using LARC methods. Moreover, as women’s childbearing shifts to later ages, it is important to understand which contraceptive methods women are using at various life stages, especially given the underrepresentation of LARC methods within the larger contraceptive method mix, the rapidly changing patterns of their use, and the historical and cultural context of contraceptive use.
This article uses the most recent nationally representative data available to examine current levels of, current correlates of, and changes in LARC use among females aged 15–44 years using contraception between 2009 and 2012 with a specific focus on associations between race, income level, and age (as indicators of relative disadvantage) and their LARC use.4–6 In addition, we examine associations between their characteristics and their discontinuation of LARC methods resulting from dissatisfaction by type of LARC method.
MATERIALS AND METHODS
Data for this cross-sectional, descriptive study come from the 2008–2010 and 2011–2013 rounds of the National Survey of Family Growth. These nationally representative samples of 6,428 (2008–2010) and 5,601 (2011–2013) females aged 15–44 years provide the most comprehensive sources of information on reproductive health topics such as contraceptive use, partnership, pregnancy history, and childbearing intentions in the United States. The National Survey of Family Growth uses a multistage probability sample design, oversamples women, teenagers, blacks, and Hispanics, and collects data through in-home, face-to-face interviews supplemented by computer-led surveys for more sensitive questions. Although men are also surveyed, the male sample was not included in this analysis. Data for this analysis are publicly available for download on the National Survey of Family Growth web site (http://www.cdc.gov/nchs/nsfg.htm). More detailed information on survey methodology, sampling design, response rates, estimation procedures, and variance estimation is published elsewhere.7 Given the deidentified nature of the public use data in the data set, our organization’s institutional review board (Department of Health and Human Services identifier IRB00002197) determined that this analysis was exempt from institutional review board approval. The funding donor had no role in the design, analysis, or reporting of this research, and the authors had complete access to and control of the data.
Our primary outcome of interest was current prevalence of LARC use among all contraceptive users at the time of the interview. We focus specifically on contraceptive users rather than all of those at risk for unintended pregnancy, because nonuse of methods (10%) and use of methods other than sterilization and LARC (50%) among females at risk for unintended pregnancy remained stable with only a small drop in females using sterilization (from 32% to 30%) occurring at the same time as the increase in LARC use (from 8% to 10%) during this time period (authors’ unpublished calculations). Current use of a LARC method is defined here as use of the contraceptive implant or the IUD, including both hormonal and nonhormonal devices, during the month of the interview. Respondents who indicated female or male sterilization as their contraceptive method were included as current contraceptive users; respondents who indicated that they were sterile by nonsurgical or noncontraceptive surgical means are not considered current contraceptive users in this analysis. Information regarding the type of IUD used (hormonal compared with nonhormonal) was collected in the 2011–2013 round of the National Survey of Family Growth, marking the first time this level of detail regarding LARC use has been captured at the national level. Geographic region of the country was also collected and is examined as an independent variable in the 2011–2013 round of data.
In addition to demographic characteristics, we included select sexual and reproductive health characteristics in our analyses that are theoretically related to LARC use. These included a woman’s number of male sexual partners in the previous year, whether she had ever experienced an unwanted pregnancy, her parity, the number of (additional) births she expects in her lifetime, and whether she had ever stopped using a non-LARC hormonal method as a result of dissatisfaction, because contraceptive users may be more motivated to initiate a LARC method if they disliked a shorter-acting method that they had previously used.
To examine change in use over time, we merged the 2008–2010 and 2011–2013 data sets and weighted each time period accordingly; they are presented here as reference years 2009 and 2012, respectively. We first tabulated the proportion of all contraceptive users using LARC methods by several demographic and reproductive health characteristics in 2009 and 2012 and then used simple logistic regression to test for significant differences in the proportions of LARC use by these characteristics between the reference years. We previously published estimates of the proportions of LARC use by select characteristics in the 2008–2010 National Survey of Family Growth (reference year 2009).2
We again used simple logistic regression to estimate unadjusted odds ratios for the relationship between demographic and sexual and reproductive health characteristics and current LARC use in 2012. All independent variables examined at the bivariate level that were significantly associated with LARC use at P<.1 as well as income resulting from its theoretical relevance to this analysis were subsequently entered into a multivariable logistic regression model to extricate correlated effects before identify characteristics predictive of current LARC use. After each iteration of a backward stepwise elimination regression process, we conducted Wald tests for each independent variable at P>.1 to determine if its inclusion affected the model. If the test was not significant at P<.05, the variable was omitted from the model. The final model included race, ethnicity, income, age, having been born outside of the United States, parity, having visited a family planning clinic in the previous year, ever having discontinued a non-LARC hormonal method as a result of dissatisfaction, and region.
Given the novelty of the data regarding type of IUD used, we calculated proportions of IUD users who fell into either the hormonal or nonhormonal categories. For key independent variables (race, income, and age), we used crosstabulation calculations to examine the proportion of females using each type of LARC method (hormonal IUD, nonhormonal IUD, and implant) by subgroup.
Our secondary outcome of interest was ever having discontinued a LARC method as a result of dissatisfaction (n=228), which was asked of all females who reported in the 2011–2013 data set that they had ever used a LARC method. We used simple logistic regression to estimate unadjusted odds ratios for the relationship between demographic and reproductive health characteristics and this outcome.
All analyses were conducted using the “svy” command prefix within Stata 13.1 to account for the National Survey of Family Growth’s use of a multistage probability sample.
In multivariable analyses adjusting for key demographic characteristics, the strongest associations with LARC use in 2012 were parity (adjusted odds ratios [ORs] 4.3–5.5) and having a history of stopping non-LARC hormonal use (adjusted OR 1.9). Women aged 35–44 years (adjusted OR 0.3) were less likely to be LARC users than their counterparts (all P<.001).
RESULTS
Between 2009 and 2012, there was a significant increase in the percent of females using contraception who used a LARC method, from 8.5% to 11.6% (P=.006; Table 1). Use of the IUD drove much of this observed trend, increasing from 7.7% to 10.3%; use of the implant remained low (1.3%) and did not change significantly between these two time periods.
Table 1.
Percentages of Current Long-Acting Reversible Contraceptive Users Among Current Contraception Users* by Selected Demographic Characteristics 2009 (n=6,428) and 2012 (n=5,601) and P Values and Percentage Point Change From Simple Logistic Regressions for the Difference in Long-Acting Reversible Contraception Use Between 2009 and 2012
| Demographic Characteristic | 2009 | 2012 | Percentage Point Change, 2009 Compared With 2012 |
|---|---|---|---|
| All | 8.5 | 11.6 | 3.2† |
| IUD | 7.7 | 10.3 | 2.6‡ |
| Implant | 0.8 | 1.3 | 0.5 |
| Race–ethnicity | |||
| White, non-Hispanic | 8.3 | 11.4 | 3.1‡ |
| Black, non-Hispanic | 9.2 | 8.6 | −0.6 |
| Other or multiple races, non-Hispanic | 9.2 | 10.6 | 1.3 |
| Hispanic | 8.5 | 15.1 | 6.6† |
| Income as a % of federal poverty level | |||
| Less than 100% | 8.1 | 13.0 | 4.9‡ |
| 100–199% | 9.6 | 13.0 | 3.4 |
| 200–299% | 7.7 | 10.1 | 2.3 |
| 300% or higher | 8.3 | 10.5 | 2.2 |
| Age (y) | |||
| 15–19 | 4.5 | 4.3 | 20.2 |
| 20–24 | 8.3 | 13.7 | 5.4‡ |
| 25–29 | 11.4 | 16.7 | 5.4‡ |
| 30–34 | 10.3 | 16.3 | 6.0 |
| 35–39 | 10.8 | 9.9 | −0.9 |
| 40–44 | 3.9 | 5.5 | 1.6 |
| Born outside the United States | |||
| No | 8.3 | 10.8 | 2.5 |
| Yes | 9.5 | 17.1 | 7.6‡ |
| Region | |||
| Northeast | NA | 10.1 | NA |
| South | NA | 9.3 | NA |
| Midwest | NA | 10.0 | NA |
| West | NA | 17.3 | NA |
| Relationship status | |||
| Not married or cohabitating | 5.7 | 9.4 | 3.7‡ |
| Married | 10.2 | 12.8 | 2.7 |
| Cohabitating | 10.1 | 13.5 | 3.4 |
| Education | |||
| No high school diploma | 7.3 | 11.0 | 3.7 |
| High school or high school equivalency certificate | 7.9 | 11.7 | 3.8‡ |
| Some college | 9.1 | 12.2 | 3.1 |
| College graduate | 9.2 | 11.2 | 2.0 |
| Employment | |||
| Not working full-time | 9.2 | 11.8 | 2.5 |
| Working full-time | 7.6 | 11.5 | 3.9‡ |
| Current insurance coverage | |||
| Private | 7.1 | 11.1 | 4.0† |
| Medicaid | 11.5 | 11.0 | −0.4 |
| Other§ | 8.0 | 14.0 | 5.9 |
| None | 10.6 | 13.1 | 2.4 |
| Religious affiliation | |||
| No religion | 9.4 | 10.4 | 1.0 |
| Catholic | 7.6 | 11.2 | 3.6 |
| Protestant | 7.6 | 11.7 | 4.1‡ |
| Other religions | 16.1 | 16.2 | 0.1 |
| No. of male sexual partners in previous year | |||
| Fewer than 2 | 9.2 | 12.4 | 3.3† |
| 2 or more | 5.5 | 8.2 | 2.8 |
| Ever experienced unwanted pregnancy | |||
| No | 8.6 | 11.1 | 2.5‡ |
| Yes | 8.0 | 13.4 | 5.4‡ |
| Total no. of live births | |||
| 0 | 2.1 | 5.9 | 3.8† |
| 1–2 | 15.0 | 16.8 | 1.8 |
| 3 or more | 6.3 | 10.9 | 4.6‡ |
| No. of additional births expected | |||
| 0 | 8.4 | 10.8 | 2.4 |
| 1–2 | 10.2 | 14.8 | 4.7‡ |
| 3 or more | 1.7 | 4.5 | 2.7 |
| Ever stopped using non-LARC hormonal method as a result of dissatisfaction? | |||
| No | 6.7 | 8.6 | 1.8 |
| Yes | 11.4 | 16.8 | 5.3‡ |
IUD, intrauterine device; NA, not available; LARC, long-acting reversible contraception.
Data are % unless otherwise specified.
Population includes all female respondents who reported current contraceptive method use, weighted to reflect the U.S. female civilian population of the United States.
Significant difference at P<.01.
Possible significant difference at P<.05, needs further study.
Other types of insurance include Medicare, military health care, or other forms of government health care (not including Indian Health Service).
Significant increases in LARC use between the two time periods were observed within many subgroups of females. The most significant increases occurred among Hispanic females (from 8.5% to 15.1%), those with private insurance (7.1–11.1%), those with fewer than two sexual partners in the previous year (9.2–12.4%), and those who were nulliparous (2.1–5.9%) (all P<.01). No significant decreases in LARC use were observed among any subgroups of females.
In 2012, LARC use was highest (greater than 16% of all females using contraception) among females aged 25–34 years, those who were born outside of the United States, those living in the western region of the country, those reporting an “other” religious affiliation, those who had had one or two births, and those who had ever stopped using a non-LARC hormonal method as a result of dissatisfaction. Long-acting reversible contraception use was lowest (less than 6% of all females using contraception) among females aged 15–19 years and 40–44 years, nulliparous females, and females who indicated expecting to have at least three (more) children.
In bivariate analyses, there were no significant differences in LARC use by race, ethnicity, poverty status, education level, employment status, insurance coverage, religious affiliation, experience of unwanted pregnancy, or intentions for a(nother) child (Table 2). In multivariable analyses adjusting for key demographic and sexual and reproductive health characteristics, the strongest predictor of LARC use in 2012 was having had a child (adjusted ORs 4.3–5.5, P<.001) (Table 2). On the other hand, women ages 35–44 years (adjusted OR 0.3, P<.001) had decreased odds of being LARC users as compared with females aged 15–24 years. Poverty status continued to not be associated with LARC use at the multivariable level.
Table 2.
Unadjusted and Adjusted Odds Ratios, P Values, and 95% Confidence Intervals From Simple and Multivariable Logistic Regression Analyses Assessing the Associations Between Selected Demographic and Reproductive Characteristics and U.S. Women’s Use of Long-Acting Reversible Contraception Methods,* 2012 (n=5,601)
| Demographic Characteristic | Unadjusted OR | 95% CI | Adjusted OR | 95% CI |
|---|---|---|---|---|
| Race–ethnicity | ||||
| White, non-Hispanic | — | — | ||
| Black, non-Hispanic | 0.7 | 0.5–1.0 | 0.6† | 0.4–0.9 |
| Other or multiple races, non-Hispanic | 0.9 | 0.5–1.7 | 0.6 | 0.3–1.2 |
| Hispanic | 1.4 | 0.9–2.0 | 0.7 | 0.5–1.2 |
| Income as a % of federal poverty level | ||||
| Less than 100% | — | — | ||
| 100–199% | 1.0 | 0.7–1.5 | 1.1 | 0.7–1.7 |
| 200–299% | 0.7 | 0.5–1.1 | 0.9 | 0.6–1.4 |
| 300% or higher | 0.8 | 0.5–1.1 | 1.3 | 0.8–2.3 |
| Age (y) | ||||
| 15–19 | — | — | ||
| 20–24 | 3.5‡ | 1.4–8.6 | ||
| 25–29 | 4.4‡ | 1.8–11.0 | 0.9 | 0.6–1.5 |
| 30–34 | 4.3‡ | 1.7–10.7 | ||
| 35–39 | 2.4 | 0.9–6.3 | 0.3§ | 0.2–0.6 |
| 40–44 | 1.3 | 0.5–3.6 | ||
| Born outside the United States | ||||
| No | — | — | ||
| Yes | 1.7† | 1.1–2.7 | 1.6 | 1.0–2.8 |
| Region | ||||
| Northeast | — | — | ||
| South | 0.9 | 0.6–1.3 | 1.1 | 0.7–1.6 |
| Midwest | 1.0 | 0.6–1.7 | 1.1 | 0.7–1.8 |
| West | 1.9‡ | 1.2–2.9 | 1.8* | 1.2–2.9 |
| Relationship status | ||||
| Not married or cohabitating | — | |||
| Married | 1.4 | 1.0–2.1 | ||
| Cohabitating | 1.5† | 1.0–2.2 | ||
| Education | ||||
| No high school diploma | — | |||
| High school or high school equivalency certificate | 1.1 | 0.6–1.9 | ||
| Some college | 1.1 | 0.6–2.0 | ||
| College graduate | 1.0 | 0.6–1.9 | ||
| Employment | ||||
| Not working full-time | — | |||
| Working full-time | 1.0 | 0.7–1.3 | ||
| Current insurance coverage | ||||
| Private | — | |||
| Medicaid | 1.0 | 0.7–1.4 | ||
| Other‖ | 1.3 | 0.8–2.2 | ||
| None | 1.2 | 0.8–1.8 | ||
| Religious affiliation | ||||
| No religion | — | |||
| Catholic | 1.1 | 0.7–1.8 | ||
| Protestant | 1.1 | 0.8–1.7 | ||
| Other religions | 1.7 | 1.0–2.9 | ||
| No. of male sexual partners in previous year | ||||
| Fewer than 2 | — | |||
| 2 or more | 0.6† | 0.4–0.9 | ||
| Ever experienced unwanted pregnancy | ||||
| No | — | |||
| Yes | 1.2 | 0.8–1.8 | ||
| Total no. of live births | ||||
| 0 | — | — | ||
| 1–2 | 3.2§ | 2.0–5.0 | 5.5§ | 3.1–9.6 |
| 3 or more | 1.9† | 1.1–3.5 | 4.3§ | 2.0–9.4 |
| Intentions for future birth(s) | ||||
| No | — | |||
| Yes | 1.2 | 0.9–1.7 | ||
| Ever stopped using non-LARC hormonal method due to dissatisfaction? | ||||
| No | — | — | ||
| Yes | 2.1§ | 1.6–2.9 | 1.9§ | 1.4–2.6 |
OR, odds ratio; CI, confidence interval; LARC, long-acting reversible contraception.
Population includes all female respondents who reported current contraceptive method use weighted to reflect the U.S. female civilian population of the United States. The final multivariable model included the following variables: race–ethnicity, income as a percent of federal poverty level, age, born outside the United States, region, total number of live births, and ever having stopped using a non-LARC hormonal method as a result of dissatisfaction.
Possible significant difference at P<.05, needs further study.
Significant difference at P<.01.
Significant difference at P<.001.
Other types of insurance include Medicare, military health care, or other forms of government health care (not including Indian Health Service).
Among LARC users in 2012, most used an IUD (89%), and the rest used an implant (11%) (Fig. 1). When examining associations between key demographic characteristics and type of LARC method used, a clear pattern emerged between method type and user race, income, and age. Significantly higher proportions of younger females (aged 15–24 years, P<.001), black females (P=.005), and females not in the highest income level (P=.018) used implants than their counterparts. In contrast, older women (ages 30 years and older), white females and females in the highest income level used IUDs in greater proportions than their counterparts.
Fig. 1.
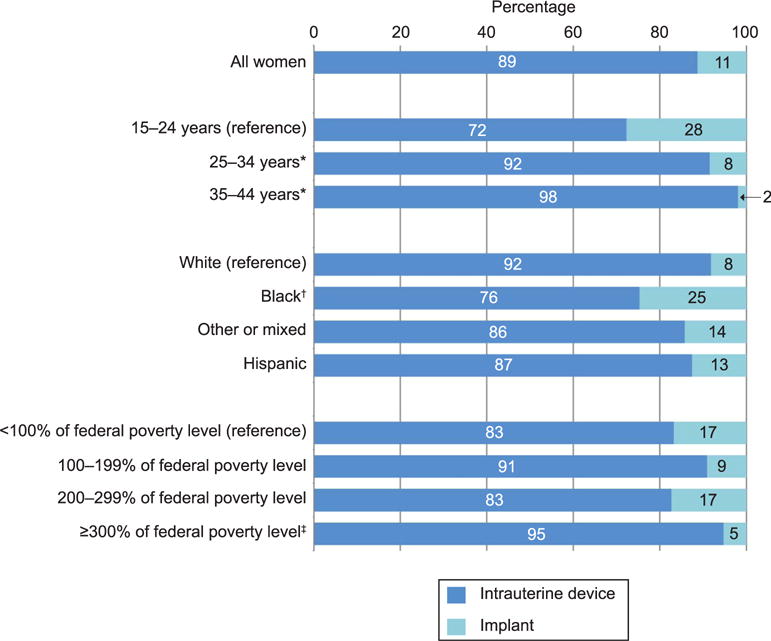
Use of intrauterine device compared with implant by demographic characteristics among all current long-acting reversible contraceptive users (n=444). *P<.001; †P<.01; ‡P<.05.
Kavanaugh. Intrauterine Device and Implant Use in the United States. Obstet Gynecol 2015.
Among IUD users in 2012, almost three fourths used a hormonal IUD, and the rest used the nonhormonal IUD (Fig. 2). There were no significant differences in type of IUD used by age or income level. Most notably, although fewer than one fourth of white, black, and females of other or mixed race used the nonhormonal IUD, Hispanic female’s use was significantly different than white female’s use (P=.009) and was split almost evenly between the hormonal and nonhormonal IUD.
Fig. 2.
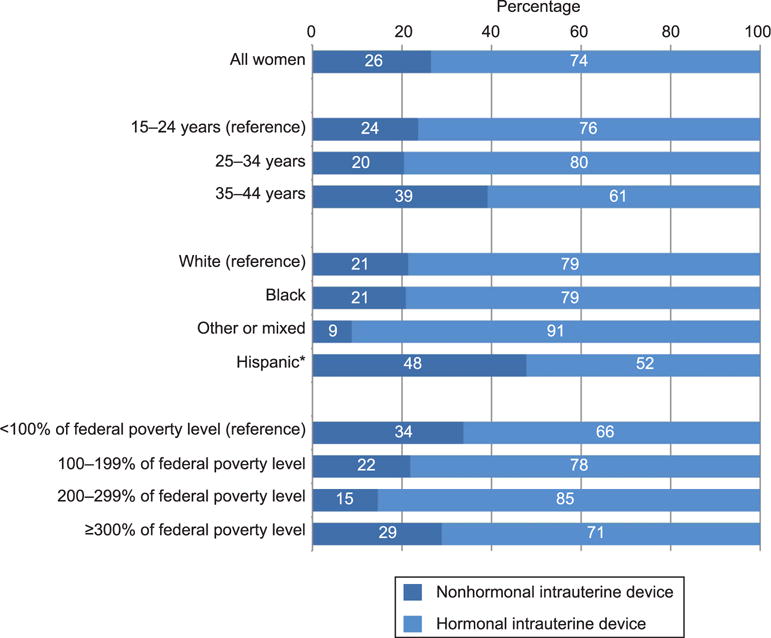
Use of nonhormonal and hormonal intrauterine device (IUD) by demographic characteristics. Of current contraceptive users, 375 women reported using either the hormonal or nonhormonal IUD in the previous 2 months; six current contraceptive users reported using an IUD in the previous 2 months but did not specify the type; an additional 14 women reported using an IUD in the previous 2 months but were not current contraceptive users at the time of the survey and were excluded from this analysis. *P<.01.
Kavanaugh. Intrauterine Device and Implant Use in the United States. Obstet Gynecol 2015.
When examining discontinuation of LARC methods as a result of dissatisfaction among the 16% of females using contraception who had ever used a LARC method, we found no significant associations among the key characteristics of race, income, or age with discontinuation (Table 3). Women with other types of insurance (OR 1.9, P=.037) and no insurance (OR 2.0, P=.025) both had increased odds of discontinuing LARC methods as a result of dissatisfaction as compared with females with private insurance and females living in the South (OR 0.4, P=.031) and Midwest (OR 0.4, P=.025) had decreased odds of doing so compared with females in the Northeast. Those with at least a college education (OR 0.4, P=.02) had decreased odds of discontinuing LARC methods as a result of dissatisfaction compared with females with less than a high school education. No other demographic or sexual and reproductive health characteristics were associated with either greater or less discontinuation of LARC methods resulting from dissatisfaction.
Table 3.
Percentages, Unadjusted Odds Ratios, and 95% Confidence Intervals From Simple Logistic Regression Analyses of Women Who Have Ever Discontinued a Long-Acting Reversible Contraception Method as a Result of Dissatisfaction Among Those Women Who Have Ever Used Long-Acting Reversible Contraception by Selected Demographic Characteristics, 2012 (n=848)
| Demographic Characteristic | % Discontinued | OR | 95% CI |
|---|---|---|---|
| All | 28 | ||
| Race–ethnicity | |||
| White, non-Hispanic | 27 | — | |
| Black, non-Hispanic | 20 | 0.7 | 0.4–1.2 |
| Other or multiple races, non-Hispanic | 37 | 1.6 | 0.6–4.4 |
| Hispanic | 31 | 1.2 | 0.8–2.0 |
| Income as a % of federal poverty level | |||
| Less than 100% | 29 | — | |
| 100–199% | 38 | 1.5 | 0.8–2.7 |
| 200–299% | 34 | 1.2 | 0.6–2.4 |
| 300% or higher | 17 | 0.5* | 0.2–1.0 |
| Age (y) | |||
| 15–24 | 30 | — | |
| 25–34 | 32 | 1.1 | 0.7–1.8 |
| 35–44 | 22 | 0.6 | 0.3–1.2 |
| Region | |||
| Northeast | 42 | — | |
| South | 24 | 0.4* | 0.2–0.9 |
| Midwest | 23 | 0.4* | 0.2–0.9 |
| West | 29 | 0.6 | 0.3–1.1 |
| Education | |||
| No high school diploma | 32 | — | |
| High school or high school equivalency certificate | 38 | 1.3 | 0.6–2.8 |
| Some college | 25 | 0.7 | 0.4–1.3 |
| College graduate | 14 | 0.4* | 0.2–0.8 |
| Current insurance coverage | |||
| Private | 21 | — | |
| Medicaid | 36 | 2.1 | 1.0–4.5 |
| Other | 34 | 1.9* | 1.0–3.5 |
| None | 35 | 2.0* | 1.1–3.7 |
OR, odds ratio; CI, confidence interval.
Although associations between all characteristics identified in Tables 1 and 2 and the outcome of discontinuation of long-acting reversible contraception method resulting from dissatisfaction were examined, only the key characteristics of race, income, and age as well as the significant associations are presented. “Other” types of insurance include Medicare, military health care, or other forms of government health care (not including Indian Health Service).
Significant difference at P<.05.
DISCUSSION
Women’s use of LARC methods has been steadily increasing for approximately a decade; during the most recent time period, use of LARC methods, particularly IUDs, increased almost uniformly across the population of users with significant increases documented among some of the groups of females who are typically at highest risk for unintended pregnancy,8 namely young adults and poor females. Increased clinical emphasis on IUDs and implants as first-line options for females of all ages9 and policy and programmatic efforts10,11 to eliminate access barriers to LARC methods by providing them free of charge to females may have helped to drive their increased uptake regionally in sites where these programs were in place.12–14
Despite increases in LARC use among black females earlier in the decade,2 our findings may reduce concern about promotion of LARC methods specifically to black females, because there was no continued increase in LARC use among black females between 2009 and 2012; use did continue to increase among females of other races and ethnicities. In fact, after accounting for other demographic characteristics, black females were less likely than white females to use LARC methods. Similarly, there was no difference in LARC use by poverty status, and there were no differences in discontinuation of LARC methods resulting from dissatisfaction between minority women and non-Hispanic white women.
However, the lower level of LARC use among black females may reflect unequal access to these methods15,16 or continued higher levels of medical mistrust among females in the black community, among other factors.17 For poor females of color in particular, acknowledging the well-documented legacy of racism and population control as it relates to contraception–and especially health care provider-controlled methods–is important, because although contraceptive methods alone cannot fully address the underlying causes of existing disparities driving unintended pregnancy (eg, racism, classism, etc), reproductive health professionals should strive to enable adolescents and women to avail themselves of the full method mix and freely choose the method that best suits their personal needs.4,18,19
Accordingly, more research into the removal of LARC methods is warranted, because we know little about the levels of access and reasons behind removal trends. More disadvantaged females may exhibit similar levels of discontinuation as a result of dissatisfaction as their counterparts, but potentially for very different reasons. Although some females may not discontinue because they are satisfied LARC users, others may have experienced pressure from, or barriers to or within, the medical establishment to avoid removal, including the denial of removal coverage under state Medicaid law.20–22
Although LARC use overall does not appear to be concentrated among any one demographic group, use of the IUD and implant individually may be. Implant users consist of many more young, low-income, and black females, which may be driven by method demand (user preference) or supply (inequitable access). Differentials in IUD and implant use among groups should continue to be monitored as these methods gain popularity.
Our analyses indicate that more females not traditionally considered to be eligible candidates for LARC methods such as young females and nulliparous females are adopting them. However, given that females who have ever discontinued a non-LARC hormonal method as a result of dissatisfaction are twice as likely to be currently using LARC, it may still be the case that LARC methods are more likely to be adopted only after females have tried and rejected other methods.
Some of the largest increases in LARC use documented between 2009 and 2012 were observed among nulliparous females and females intending a future or subsequent child, indicating that these methods are being used by some women to delay or space pregnancies rather than limit them. Nonetheless, nulliparous females are still much less likely to use LARC methods than females who have had a child, suggesting that there may be a lack of awareness of updated clinical guidelines indicating LARC methods as suitable or first-line choices for females at all stages in their reproductive lives.9,23 Similarly, younger females are increasingly using LARC methods, but use among the youngest age group15–19 remains much lower than all other age groups. When these young females do use LARC methods, they tend to use the implant more than the IUD. Research indicates that this may be the result of health care provider perceptions of patient preferences, pain, or pelvic examination avoidance and a higher likelihood of early removal as a result of dissatisfaction.10 However, these data indicate that, nationally, young females are not more likely to discontinue these methods as a result of dissatisfaction than older women, a finding supported by a study of discontinuation among a large group of females using LARC.24
Although these data predate the implementation of the Affordable Care Act’s contraceptive mandate, significant increases in LARC use were also documented among females employed full-time and those with private insurance coverage. Since the Affordable Care Act’s enactment, females are increasingly paying $0 out of pocket for their contraception,25 but barriers to obtaining full coverage for methods remain,20,22 which may affect LARC use in the future.
Several limitations are inherent in the analysis of cross-sectional data. Associations observed between respondent characteristics and contraceptive method use do not necessarily imply a causal relationship. In addition, given multiple hypothesis testing, our chosen threshold for significance of P<.05 may have resulted in some spuriously significant associations. Nonetheless, given our aim to describe broad trends in use, we present unadjusted P values and highlight those below the traditional threshold to enable the reader to differentiate those characteristics with greatest evidence of change.
During the same study period, unintended pregnancy rates fell in many states in the United States with double-digit declines in some states where public health professionals have made proactive efforts to improve access to long-acting methods in particular.26 Although LARC methods are now more proportionately utilized in the United States, it is still important for health care providers to consider the historical and cultural context in which method choices are made. Long-acting reversible contraception methods may present many females with an option that effectively meets their specific needs at a particular time in their reproductive lives, but there is no single “best” method of contraception. By both providing accurate information about methods and prioritizing each individual woman’s stated preferences, health care providers can support all females in achieving their childbearing goals.
Acknowledgments
The authors thank Rachel Jones, Laura Lindberg, and Adam Sonfield for reviewing and commenting on this manuscript and Meghan Ingerick for research assistance.
Supported by a grant from an anonymous donor.
Footnotes
Financial Disclosure
The authors did not report any potential conflicts of interest.
LEVEL OF EVIDENCE: III
References
- 1.Hatcher R, Trussell J, Nelson A, Cates W. Contraceptive technology. Atlanta (GA): Bridging the Gap Communications; 2011. [Google Scholar]
- 2.Finer LB, Jerman J, Kavanaugh ML. Changes in use of long-acting contraceptive methods in the United States, 2007–2009. Fertil Steril. 2012;98:893–7. doi: 10.1016/j.fertnstert.2012.06.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Secura G. Long-acting reversible contraception: a practical solution to reduce unintended pregnancy. Minerva Ginecol. 2013;65:271–7. [PubMed] [Google Scholar]
- 4.Gold RB. Guarding against coercion while ensuring access: a delicate balance. Guttmacher Policy Rev. 2014;17:8–14. [Google Scholar]
- 5.Gomez AM, Fuentes L, Allina A. Women or LARC first? Reproductive autonomy and the promotion of long-acting reversible contraceptive methods. Perspect Sex Reprod Health. 2014;46:171–5. doi: 10.1363/46e1614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Higgins JA. Celebration meets caution: LARC’s boons, potential busts, and the benefits of a reproductive justice approach. Contraception. 2014;89:237–41. doi: 10.1016/j.contraception.2014.01.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.U.S. Department of Health and Human Services. National Survey of Family Growth User’s Guide. Hyattsville (MD): HHS; 2014. Centers for Disease Control and Prevention and National Center for Health Statistics. Public use data file documentation: 2011–2013. [Google Scholar]
- 8.Finer LB, Zolna MR. Shifts in intended and unintended pregnancies in the United States, 2001–2008. Am J Public Health. 2014;104(suppl 1):S43–8. doi: 10.2105/AJPH.2013.301416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Long-acting reversible contraception: implants and intrauterine devices. Practice Bulletin No. 121. American College of Obstetricians and Gynecologists. Obstet Gynecol. 2011;118:184–96. doi: 10.1097/AOG.0b013e318227f05e. [DOI] [PubMed] [Google Scholar]
- 10.Kavanaugh ML, Frohwirth L, Jerman J, Popkin R, Ethier K. Long-acting reversible contraception for adolescents and young adults: patient and provider perspectives. J Pediatr Adolesc Gynecol. 2013;26:86–95. doi: 10.1016/j.jpag.2012.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McNicholas C, Madden T, Secura G, Peipert JF. The contraceptive CHOICE project round up: what we did and what we learned. Clin Obstet Gynecol. 2014;57:635–43. doi: 10.1097/GRF.0000000000000070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Biggs MA, Rocca CH, Brindis CD, Hirsch H, Grossman D. Did increasing the use of highly effective contraception contribute to declining abortions in Iowa? Contraception. 2015;91:167–73. doi: 10.1016/j.contraception.2014.10.009. [DOI] [PubMed] [Google Scholar]
- 13.Postlethwaite D, Trussell J, Zoolakis A, Shabear R, Petitti D. A comparison of contraceptive procurement pre- and post-benefit change. Contraception. 2007;76:360–5. doi: 10.1016/j.contraception.2007.07.006. [DOI] [PubMed] [Google Scholar]
- 14.Ricketts S, Klingler G, Schwalberg R. Game change in Colorado: widespread use of long-acting reversible contraceptives and rapid decline in births among young, low-income women. Perspect Sex Reprod Health. 2014;46:125–32. doi: 10.1363/46e1714. [DOI] [PubMed] [Google Scholar]
- 15.Dehlendorf C, Foster DG, de Bocanegra HT, Brindis C, Bradsberry M, Darney P. Race, ethnicity, and differences in contraception among low-income women: methods received by Family PACT Clients, California, 2001–2007. Perspect Sex Reprod Health. 2011;43:181–7. doi: 10.1363/4318111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Downing RA, LaVeist TA, Bullock HE. Intersections of ethnicity and social class in provider advice regarding reproductive health. Am J Public Health. 2007;97:1803–7. doi: 10.2105/AJPH.2006.092585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Frost JJ, Lindberg LD, Finer LB. Young adults’ contraceptive knowledge, norms, and attitudes: associations with risk of unintended pregnancy. Perspect Sex Reprod Health. 2012;44:107–16. doi: 10.1363/4410712. [DOI] [PubMed] [Google Scholar]
- 18.Gordon L. Woman’s body, woman’s right: a social history of birth control in America. New York (NY): Penguin; 1990. [Google Scholar]
- 19.Roberts D. Killing the black body: race, reproduction, and the meaning of liberty. New York (NY): Vintage; 1998. [Google Scholar]
- 20.National Women’s Law. State of birth control coverage: health plan violations of the Affordable Care Act. Washington, DC: National Women’s Law Center; 2015. pp. 1–34. [Google Scholar]
- 21.Division of Medical Services. South Dakota Medicaid: family planning billing manual. Pierre (SD): Department of Social Services; 2015. [Google Scholar]
- 22.Salganicoff A, Ranji U, Beamesderfer A, Kurani N. Women and health care in the early years of the ACA: key findings from the 2013 Kaiser Women’s Health Survey. Menlo Park (CA): The Henry J. Kaiser Family Foundation; 2014. [Google Scholar]
- 23.Committee on Adolescence, American Academy of Pediatrics. Contraception for adolescents. Pediatrics. 2014;134:e1244–56. [Google Scholar]
- 24.Rosenstock JR, Peipert JF, Madden T, Zhao Q, Secura GM. Continuation of reversible contraception in teenagers and young women. Obstet Gynecol. 2012;120:1298–305. doi: 10.1097/aog.0b013e31827499bd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sonfield A, Tapales A, Jones RK, Finer LB. The impact of the federal contraceptive coverage guarantee on out-of-pocket payments for contraceptives: 2014 update. Contraception. 2015;91:44–8. doi: 10.1016/j.contraception.2014.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kost K. Unintended pregnancy rates at the state level: estimates for 2010 and trends since 2002. New York (NY): Guttmacher Institute; 2015. [Google Scholar]


