Abstract
Background
Aspects of U.S. clinical abortion service provision such as gestational age limits, charges for abortion services, and anti-abortion harassment can impact the accessibility of abortion; this study documents changes in these measures between 2008 and 2012.
Methods
In 2012 and 2013, we surveyed all known abortion-providing facilities in the United States (n = 1,720). This study summarizes information obtained about gestational age limits, charges, and exposure to anti-abortion harassment among clinics; response rates for relevant items ranged from 54% (gestational limits) to 80% (exposure to harassment). Weights were constructed to compensate for nonresponding facilities. We also examine the distribution of abortions and abortion facilities by region.
Findings
Almost all abortion facilities (95%) offered abortions at 8 weeks’ gestation; 72% did so at 12 weeks, 34% at 20 weeks, and 16% at 24 weeks in 2012. In 2011 and 2012, the median charge for a surgical abortion at 10 weeks gestation was $495, and $500 for an early medication abortion, compared with $503 and $524 (adjusted for inflation) in 2009. In 2011, 84% of clinics experienced at least one form of harassment, only slightly higher than found in 2009. Hospitals and physicians’ offices accounted for a substantially smaller proportion of facilities in the Midwest and South. Clinics in the Midwest and South were exposed to more harassment than their counterparts in the Northeast and West.
Conclusions
Although there was a substantial decline in abortion incidence between 2008 and 2011, the secondary measures of abortion access examined in this study changed little during this time period.
Between 2008 and 2011, the abortion rate in the United States dropped 13%, from 19.4 to 16.9 abortions per 1,000 women aged 15 to 44 (Jones & Jerman, 2014). The number of abortion clinics declined by only 1% during this same time period (Jones & Jerman, 2014), suggesting that clinic closures alone did not account for most of the drop in abortion incidence. In fact, several trends—including a parallel decline in birth rates (National Center for Health Statistics, 2009, 2013) and increased reliance on long-acting reversible contraception (Finer, Jerman, & Kavanaugh, 2012)—suggest that the decline in abortion is at least partially owing to fewer women experiencing unintended pregnancies (Jones & Jerman, 2014).
Although access to abortion is primarily defined by the presence of a health care facility that provides abortion care, secondary measures of access can influence women’s ability to obtain care at these facilities, and include factors such as fees charged, gestational age limits, and harassment. If abortion services became more expensive, if fewer facilities were performing abortions at various gestational ages, or if increased harassment made women reluctant to go to a clinic, access to services may have been reduced.
In 2009, the median charge for a surgical abortion at 10 weeks was $470, and the comparable charge for early medication abortion, which accounted for 17% of all nonhospital abortion procedures, was $490 (Jones & Kooistra, 2011). These costs can be significant, especially in consideration of the fact that the majority of abortion patients are low income, and most pay out of pocket (Jones, Finer, & Singh, 2010; Upadhyay, Weitz, Jones, Barar, & Foster, 2013). Additionally, some women must travel to access services, which can introduce additional costs. In 2008, abortion patients traveled an average of 30 miles one way (or 60 miles roundtrip) to the facility at which they obtained their abortion, but women who lived in a state with a 24-hour waiting period, women obtaining second-trimester abortions, those who crossed state lines, and, in particular, those who lived in rural areas were more likely to travel greater distances (Jones & Jerman, 2013). Both costs and facility gestational age limits can result in delays in accessing services (Van Bebber, Phillips, Weitz, Gould, & Stewart, 2006). In 2009, 95% of facilities offered abortion services at 8 weeks’ gestation, but only 23% did so at 20 weeks, and 11% at 24 weeks (Jones & Kooistra, 2011). During this same year, an estimated 4,000 women were unable to obtain abortions because they were past facilities’ gestational age limits by time they made it there (Upadhyay et al., 2013). If the proportion of facilities offering abortions in the second trimester declined since 2009, it is possible that an even greater number of women were unable to access services in more recent years.
Although information on regional variations in abortion access is available, it has not been systematically examined in prior research. Abortion rates and facility distributions vary by region; in 2011, the Midwest and the South had lower abortion rates (11.7 and 15.2, respectively) than the Northeast and the West (24.6 and 18.5), and 53% and 49% of women in the Midwest and the South, respectively, lived in a county without a clinic, compared with 24% and 16% in the Northeast and West (Jones & Jerman, 2014). Almost all states in the Midwest and South prohibit Medicaid coverage of abortions for low-income women (Guttmacher Institute, 2013b), and women in these regions have to travel significantly farther to access abortion services (Jones & Jerman, 2013). Access to services in these regions may be further reduced by antiabortion attitudes and harassment. In 2009, 85% of nonhospital facilities in the Midwest and 75% in the South experienced any harassment, compared with 48% Northeast and 44% in the West (Jones & Kooistra, 2011). Moreover, almost all of the 106 laws related to abortion restrictions adopted between 2008 and 2011 were in the Midwest and South (Jones & Jerman, 2014).
This article documents several measures of access to abortion services in the United States—cost, gestational age limits, and harassment—using data from the Guttmacher Institute’s most recent Abortion Provider Census. For the first time, we also assess regional differences in abortion access.
Methods
Data used in this analysis come from the Guttmacher Institute’s 16th census of all known abortion-providing facilities in the United States, a series dating back to 1973. The results of this survey produce the most complete data available on abortion incidence and service providers in the United States. The current analysis assesses several indicators: Gestational age limits in 2012, average charges for abortion services in 2011 and 2012, and whether the facility experienced any of seven forms of harassment in 2011. Survey items about harassment referred specifically to 2011. The survey methodology has been described in detail elsewhere (Jones & Jerman, 2014), but we provide a brief overview of relevant issues herein.
In April 2012, paper questionnaires collecting information on number of abortions and various aspects of abortion services were sent to all known abortion providing facilities in the United States, and data collection efforts continued through May 2013. Hospital surveys had fewer questions and, for example, did not ask about harassment or charges for procedures because individuals completing the surveys in these types of facilities sometimes do not have access to this information. Approximately 81% of nonhospital facilities responded to the survey, with varying degrees of survey completeness. Information about issues such as gestational age limits and charges was available on many clinic web sites and was sometimes used for facilities that did not return the survey or did not answer these questions. Only 25% of hospital facilities known to provide abortions responded to the survey; however, many of our analyses are limited to nonhospital facilities, because the overwhelming majority of abortion procedures (96%) take place in nonhospital settings.
All facilities, including hospitals, were asked the minimum and maximum gestational age—defined as the number of weeks since a woman’s last menstrual period (LMP)—at which they provided three types of abortions: Early medication abortion, surgical abortion, and induction abortion. The survey referred to early medication abortion as occurring before 10 weeks LMP and involving mifepristone, misoprostol, or methotrexate; induction abortions were not defined, per se, but the category included parenthetical information indicating that they occurred in the second trimester or later. Importantly, prior surveys only asked about medication and surgical abortions, and did not have a separate item for induction abortion; in the past it was assumed that these procedures were considered to be surgical abortions. However, we found that 133 facilities listed a higher maximum gestational age limit for the induction procedure item than was listed for surgical procedures. In some instances the difference was greater by 3 or more weeks. Thus, the current study may result in higher, but more accurate, estimates of gestational age limits. Items about gestational age limits were assumed to be answered in reference to the time the survey was filled out, typically in 2012.
Nonhospital facilities were asked the usual charges a self-paying patient would incur for surgical abortions at 10 and 20 weeks and for early medication abortions, and we used this information to estimate the average amount charged for each procedure. Items asking about costs referred to charges in 2011, but information obtained from abortion facilities’ web sites was for the year in which the data were obtained, and for some facilities this was 2012; as such, cost information is presented here for 2011 and 2012. To account for the fact that more women obtain abortions at larger facilities or seek out facilities with lower charges, we weighted the charge data by the number of abortions at each facility in 2011 to estimate the mean out-of-pocket expenditure for patients.
Nonhospital facilities were asked how frequently they had experienced any of seven types of harassment in 2011: Picketing, picketing with physical contact or blocking, vandalism, picketing of homes of staff members, bomb threats, harassing phone calls, and noise disturbances. The four response categories ranged from never to 20 or more times per year. Our analysis examines never versus any exposure, as well as frequent exposure, or 20 or more times per year. Clinics that provide abortion services advertise their services and are easy to find, whereas many physicians’ offices that provide these services have a lower profile. For this reason, we restricted our analysis of exposure to harassment to clinic facilities.
We obtained at least some information on gestational age limits from 54% of all facilities (this indicator included hospitals, many of which did not respond to the survey); among nonhospital facilities, 68% had information on charges (including facilities for which we obtained information from their web sites), and 80% of clinics provided information about exposure to harassment. We constructed weights that accounted for these differences, and they were used in relevant analyses. The weights were constructed based on facility type and caseload and assume that nonresponding facilities resembled those that responded.
We distinguish between four types of facilities: Abortion clinics, nonspecialized clinics, hospitals, and physicians’ offices. Abortion clinics are defined as nonhospital facilities in which half or more of patient visits were for abortion services. Non-specialized clinics are sites in which fewer than half of patient visits were for abortion services; these include physicians’ offices that provide 400 or more abortions per year. Physicians’ offices are facilities that perform fewer than 400 abortions per year and have names suggesting that they are physicians’ private practices. We also distinguish among four caseload groups: Fewer than 30 abortions, 30 to 399 abortions, 400 to 999 abortions, and 1,000 or more per year.
Findings
Gestational Age Limits
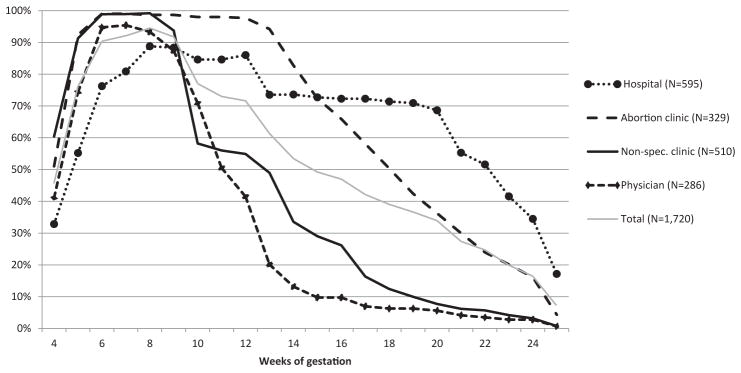
Almost all abortion facilities (95%) offered abortions at 8 weeks’ gestation in 2012 (Figure 1), and the proportion of facilities offering abortion services at 9 weeks or later declined steadily, with 72% performing abortions at 12 weeks, 34% at 20 weeks, and 16% at 24 weeks. Fewer than half (46%) offered abortions at 4 weeks’ gestation or earlier.
Figure 1.
Percentage of facilities performing abortions, by gestational age at which abortions were performed, according to type of facility, 2012.
There were important variations in gestational age limits by facility type. After 9 weeks’ gestation, there was a sharp drop of both nonspecialized clinics and physicians’ offices performing abortions, perhaps because these types of facilities were more likely to offer only early medication abortion (Jones & Jerman, 2014). For example, 93% of abortion-providing physicians offered services at 8 weeks, but this percentage dropped to 71% at 10 weeks. Almost all abortion clinics offered abortion services through the first trimester, but availability steadily declined after 12 weeks, gestation. Slightly more than two thirds of hospitals provided abortions at 20 weeks’ gestation. Although lower than hospitals, a substantial minority of abortion clinics (36%) also performed abortions at 20 weeks’ gestation.
Cost
In 2011 and 2012, the median charge for a surgical abortion at 10 weeks gestation was $495 (range, $10–$2,908; Table 1). (The unusually low minimum was listed by one facility that did relatively few abortions and likely reflects a sliding scale or reduced fee.) By comparison, the infiation-adjusted charge for the same procedure in 2009 was $503 (Bureau of Labor Statistics, 2013; Jones & Kooistra, 2011), suggesting little to no change. The cost of abortion varied by facility type and gestational age. Abortion clinics charged the least for a surgical abortion at 10 weeks’ gestation ($450); abortions were most expensive at physicians’ offices ($550). Following this pattern, facilities with the largest caseloads charged the least ($450), and those that performed fewer than 30 procedures per year charged the most ($650).
Table 1.
Charges for Nonhospital Surgical Abortion at 10 Weeks of Gestation, According to Type of Facility and Charges for Nonhospital Early Medical Mifepristone Abortions, 2011–2012
| Provider Type and Caseload | Surgical Abortion at 10 Weeks (U.S.$)
|
Paid, Mean | Early Medical Abortion before 10 Weeks (U.S.$)
|
Paid, Mean | ||||
|---|---|---|---|---|---|---|---|---|
| Mean | Median | Range | Mean | Median | Range | |||
| All | 558 | 495 | 10–2,908 | 480 | 527 | 500 | 20–1,655 | 504 |
| Provider type | ||||||||
| Physician | 636 | 550 | 10–2,500 | 529 | 558 | 500 | 20–1,655 | 484 |
| Nonspecialized clinic | 569 | 485 | 100–2,908 | 518 | 525 | 500 | 290–1,250 | 528 |
| Abortion clinic | 472 | 450 | 195–1,500 | 457 | 503 | 494 | 295–1,250 | 492 |
| Caseload | ||||||||
| <30 | 738 | 650 | 150–2,739 | 647 | 592 | 535 | 28–1,655 | 553 |
| 30–399 | 554 | 485 | 10–2,908 | 523 | 513 | 500 | 20–1,250 | 504 |
| 400–999 | 519 | 480 | 100–1,400 | 515 | 534 | 500 | 290–1,250 | 532 |
| ≥1,000 | 483 | 450 | 220–1,250 | 472 | 504 | 495 | 295–1,250 | 500 |
Adjusting for the fact that more women obtained abortions at facilities that charged less, we found that women paid $480 (mean) for a surgical abortion at 10 weeks’ gestation in 2011 and 2012, and patterns by facility type and caseload mirrored those of amount charged. In 2009, the inflation-adjusted cost was $483 (Bureau of Labor Statistics, 2013; Jones & Kooistra, 2011), once again suggesting little to no change.
In 2011, approximately 23% of nonhospital abortions were early medication procedures (Jones & Jerman, 2014). The median charge for early medication abortion was similar to surgical abortions at 10 weeks’ gestation at $500, although the average amount women paid was slightly higher than that for a surgical abortion at 10 weeks ($504). Adjusting for inflation, the median charge for early medication abortion in 2009 was $524 (Bureau of Labor Statistics, 2013; Jones & Kooistra, 2011). The median charge for an early medication procedure varied little by facility type, but as with surgical abortion, smaller facilities charged slightly more and prices decreased as caseload increased. The average amount women paid for a medication abortion did not always follow the same patterns as amount charged. For example, women paid slightly less for them at physicians’ offices than at other facilities.
Abortions at 20 weeks’ gestation typically take 2 or more days to complete, and involve greater skill and resources. The median charge for an abortion at 20 weeks’ gestation in 2011 and 2012 was $1,350 (range, $750–$5,000; data not shown).
Harassment
A majority of clinics (84%) experienced at least one form of antiabortion harassment in 2011 (Table 2). Exposure to picketing was most common (80%) followed by receiving harassing phone calls (47%). Additionally, just over one quarter of facilities reported picketing with physical contact or blocking of patients.
Table 2.
Percentage of Abortion and Nonspeciality Clinic Providers Experiencing Harassment, by Provider Type, Caseload, and Region, According to Type of Harassment, 2011
| Provider | n | Any Harassment
|
Picketing
|
Harassing Phone Calls
|
Picketing with Physical Contact/Blocking of Patients
|
Noise Disturbances
|
Vandalism
|
Picketing of Homes of Staff Members
|
Bomb Threats
|
|---|---|---|---|---|---|---|---|---|---|
| % | % | % | % | % | % | % | % | ||
| All 2011 | 84 | 80 | 47 | 28 | 21 | 15 | 6 | 3 | |
| Type | |||||||||
| Abortion clinic | 327 | 91 | 88 | 64 | 41 | 33 | 19 | 12 | 4 |
| Nonspecialized clinic | 508 | 79 | 74 | 36 | 20 | 14 | 13 | 2 | 2 |
| Size | |||||||||
| <30 | 36 | 39 | 26 | 26 | 0 | 0 | 0 | 0 | 0 |
| 30–399 | 247 | 72 | 66 | 27 | 12 | 9 | 14 | 2 | 1 |
| 400–999 | 184 | 85 | 80 | 46 | 26 | 19 | 15 | 7 | 1 |
| ≥1,000 | 367 | 96 | 94 | 62 | 43 | 33 | 17 | 9 | 5 |
| Region | |||||||||
| Midwest | 124 | 95 | 88 | 77 | 45 | 27 | 20 | 11 | 4 |
| Northeast | 194 | 78 | 75 | 42 | 21 | 14 | 13 | 4 | 3 |
| South | 234 | 89 | 85 | 57 | 35 | 33 | 15 | 11 | 3 |
| West | 283 | 79 | 74 | 28 | 20 | 14 | 15 | 1 | 1 |
Note: Midwest states include Illinois, Indiana, Iowa, Kansas, Michigan, Minnesota, Missouri, Nebraska, North Dakota, Ohio, South Dakota, and Wisconsin. Northeast states include Connecticut, Maine, Massachusetts, New Hampshire, New Jersey, New York, Pennsylvania, Rhode Island, and Vermont. South states include Alabama, Arkansas, Delaware, District of Columbia, Florida, Georgia, Kentucky, Louisiana, Maryland, Mississippi, North Carolina, Oklahoma, South Carolina, Tennessee, Texas, Virginia, and West Virginia. West states include Alaska, Arizona, California, Colorado, Hawaii, Idaho, Montana, Nevada, New Mexico, Oregon, Utah, Washington, and Wyoming.
Abortion clinics were more likely than nonspecialized clinics to report experiencing each form of harassment, as were larger facilities when compared with smaller ones. Almost all facilities with abortion caseloads of 1,000 patients or more each year had experienced picketing (94%). Despite their low abortion caseload, slightly more than one quarter of clinics with fewer than 30 abortion patients each year reported picketing.
When examined by region, exposure was highest in the Midwest, where 95% of clinics experienced at least one type of harassment, followed by the South (89%). Levels of harassment were also substantial in the Northeast (78%) and the West (79%). These regional patterns pertained to most types of harassment, although a greater proportion of clinics in the Midwest were exposed to harassing phone calls (77%) compared with other regions.
Harassment was not an infrequent occurrence for many clinics; 53% reported that they were picketed 20 or more times in 2011, with increased exposure more common among abortion clinics (73%) and facilities performing 1,000 or more abortions (78%; data not shown). The majority of clinics in the Midwest and the South experienced picketing 20 or more times per year (66% and 58%), compared with just under one half in the Northeast (48%) and the Midwest (47%). Higher frequency exposure to other types of harassing activities was less common, although 17% of abortion clinics were exposed to harassing phone calls and 18% to noise disturbances 20 or more times in 2011.
Published figures for levels of harassment in 2008 were not restricted to clinics and included fewer activities; specifically, receiving harassing phone calls and noise disturbances were not included in the prior survey. We generated comparable tabulations of both the 2008 and 2011 datasets using only the five overlapping indicators and found a slight increase in exposure to any of the harassing activities assessed on both surveys: 80% of clinics in 2011 compared with 75% in 2008 (data not shown).
Regional Distributions of Facilities and Abortions
Even though the South accounted for the largest share of U.S. abortions (34%), there were more abortion-providing facilities in the Northeast (453) and West (737) than in the South (357; Table 3). Hospitals made up the largest percentage of abortion-providing facilities in the Northeast and the West (36% and 42%, respectively), whereas abortion clinics made up the largest portion of facilities in the South (40%). A slightly higher proportion of facilities in the Midwest were nonspecialized clinics (37%), compared with abortion clinics (35%). Fewer than 1 in 10 facilities in the Midwest and South were physicians’ offices, but these facilities accounted for approximately one in five facilities in the Northeast and the West.
Table 3.
Distribution of Abortions and Women of Reproductive Age; Type of Abortion Facilities and Number of Abortions by Facility Type; All by Region, 2011
| % of All Abortions | Northeast
|
Midwest
|
South
|
West
|
Total
|
|---|---|---|---|---|---|
| 26 | 14 | 34 | 26 | 100 | |
| Distribution of facilities | |||||
| Total no. of facilities | 453 | 173 | 357 | 737 | 1,720 |
| Facility type (%) | 100 | 100 | 100 | 100 | 100 |
| Abortion clinic | 12 | 35 | 40 | 10 | 19 |
| Nonspecialized clinic | 29 | 37 | 29 | 29 | 30 |
| Hospital | 36 | 22 | 24 | 42 | 35 |
| Physicians’ offices | 23 | 6 | 7 | 20 | 17 |
| Distribution of abortions | |||||
| Total no. of abortions | 272,020 | 153,380 | 356,790 | 276,300 | 1,058,490 |
| Facility type (%) | 100 | 100 | 100 | 100 | 100 |
| Abortion clinic | 51 | 69 | 76 | 57 | 64 |
| Nonspecialized clinic | 38 | 28 | 22 | 38 | 31 |
| Hospital | 9 | 2 | 1 | 3 | 4 |
| Physicians offices | 2 | 0 | 0 | 2 | 1 |
| Women 15–44 (%) | 18 | 21 | 37 | 24 | 100 |
Note: Abortion clinics are defined as nonhospital facilities in which half or more of patient visits were for abortion services; non-specialized clinics are sites in which fewer than half of patient visits were for abortion services, including physicians’ offices that provide 400 or more abortions per year. Physicians’ offices are facilities that perform fewer than 400 abortions per year.
Although there were regional differences in facility type, abortion clinics provided the majority of abortions in all regions and physicians’ offices provided the fewest. In the West, for example, abortion clinics made up only 10% of all facilities, but accounted for 57% of the region’s total abortions; the 20% of physicians’ offices accounted for only 2% of abortions. Hospitals accounted for fewer than 10% of abortions in all regions.
Regional differences also existed in population distributions of abortions. The Northeast accounted for 18% of all women of reproductive age, but 26% of abortions (Table 3). By contrast, the Midwest accounted for 21% of all women of reproductive age but 14% of abortions.
Discussion
We found relatively few changes in gestational age limits, charges for abortion services or harassment experienced by abortion providing facilities between 2008 and 2009 compared with 2011 and 2012. Similar to previous years (Jones & Kooistra, 2011; Jones, Zolna, Finer, & Henshaw, 2008), virtually all facilities offered abortion services at 8 weeks’ gestation. A higher proportion of facilities reported providing later second-trimester abortions in 2012 compared with 2009 (in 2012, 34% provided at 20 weeks and 16% provided at 24 weeks, compared with 23% and 11%, respectively, in 2009). This increase is likely owing to a change in the wording of the survey item asking about second-trimester abortions by induction as opposed to an actual increase in the proportion of facilities offering this service.
In 2011 and 2012, on average, women paid $480 for a surgical abortion at 10 weeks, and $504 for an early medication abortion. Given prior research finding that most low-income women pay for the procedure out of pocket (Jones, Upadhyay, & Weitz, 2013; Jones et al., 2010), these costs are not insignificant. But, after adjusting for inflation, women in 2011 and 2012 seemed to be paying about the same amount as abortion patients in 2009. That the number of early medication abortions increased during this period (Jones & Jerman, 2014) could be a both a cause and a consequence of the small ($24) drop in the cost of this procedure; greater demand may have resulted in a lower cost, or it could also be that lowering the cost made it more affordable for more women. Median charges for abortion also showed little to no change over time. This may represent an effort on the part of providers to keep services affordable, in spite of increases in both restrictions and concomitant costs of health care provision in many areas.
The majority of clinics experienced at least one type of harassment; although exposure was highest among clinics that specialized in abortion services (91%) and those with annual caseloads of 1,000 or more (96%), it was still experienced by more than three quarters of nonspecialized clinics. We found that clinics in the Midwest and the South were more likely to experience harassment than those in the Northeast and the West, and, moreover, they were more likely to experience harassment more frequently (i.e., >20 times per year).
We identified several interesting patterns in abortion provision by region. There was a greater concentration of services in abortion and nonspecialized clinics in the Midwest and South—in particular, a substantially smaller share of facilities was accounted for by physicians’ offices in these areas. Notably, clinics—both abortion and nonspecialized—accounted for the overwhelming majority of abortions in all regions (89%–98%). Relative to the Northeast and the West, women in the Midwest and, to a lesser extent, the South were underrepresented among abortion patients, and harassment was also more common. It is possible that women in these regions have a harder time accessing abortion services owing to greater distances (Jones & Jerman, 2014), reduced access to providers (Jones & Jerman, 2014), and greater stigma; inability to overcome these barriers may contribute to their relatively lower abortion rates. Cultural factors may also play a role. For example, recent research found greater levels of opposition to legal abortion in the Midwest and the South (Pew Research Center for People and the Press, 2013). As such, when confronted with an unintended pregnancy, women in these regions may be less inclined to seek an abortion.
We are aware of several shortcomings of this study. Some facilities did not answer all (or any) of the questions. For example, only a minority of hospitals provided us with information on gestation; it is possible that our estimates of gestational limits for these facilities is imprecise, especially if nonresponding hospitals differ from those that did participate in the survey. We expect that some facilities that perform a small number of abortions per year—in particular hospitals and physicians’ offices—are not captured in our survey. Smaller providers in the Midwest and the South may have been more reluctant to respond to our survey than small providers in the Northeast and the West, and, if this were the case, the regional variations in provider types that we identified may be less pronounced.
Implications for Policy and/or Practice
Abortion is an integral component of comprehensive reproductive health care, but legal availability does not guarantee access to services. Although this study suggests that changes in gestational age limits and cost did not change substantially from 2008 and 2009 compared with 2011 and 2012, it is possible that a number of factors impacting access to services have changed since the study period. In 2012, 42 abortion restrictions were enacted (Guttmacher Institute, 2013a), and another 70 abortion restrictions were enacted in 2013—mostly in the South and the Midwest (Guttmacher Institute, 2014). As services become more restricted in the these regions and, potentially, more concentrated within facilities vulnerable to anti-abortion harassment and state regulations, barriers may mount. Ongoing monitoring of abortion indicators is necessary to address disparities in access to reproductive health services. Ideally, policymakers will use this information to remove barriers to abortion care and proactively protect all women’s access to reproductive health care.
Acknowledgments
The authors thank Alyssa Browne, Amelia Bucek, Carolyn Cox, Marjorie Crowell, Michelle Eilers, Vivian Gor, Fran Linkin, Tsuyoshi Onda, Stina Rosenquist, Zoe Unger, and Emily Zahn for research assistance, and Elizabeth Nash and Lawrence Finer for reviewing early versions of this article.
References
- Bureau of Labor Statistics. [Accessed November 30, 2013];Consumer price index inflation calculator. 2013 Available: http://www.bls.gov/data/inflation_calculator.htm.
- Finer LB, Jerman J, Kavanaugh ML. Changes in use of long-acting contraceptive methods in the United States, 2007–2009. Fertility and Sterility. 2012;98:893–897. doi: 10.1016/j.fertnstert.2012.06.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guttmacher Institute. [Accessed November 30, 2013];Laws affecting reproductive health and rights: 2012 state policy review. 2013a Available: http://www.guttmacher.org/statecenter/updates/2012/statetrends42012.html.
- Guttmacher Institute. [Accessed March 20, 2014];Laws affecting reproductive health and rights: 2013 state policy review. 2014 Available: http://www.guttmacher.org/statecenter/updates/2013/statetrends42013.html.
- Guttmacher Institute. Restricting insurance coverage of abortion. Washington, DC: Author; 2013b. [Google Scholar]
- Jones RK, Jerman J. How far did US women travel for abortion services in 2008? Journal of Women’s Health. 2013;22:706–713. doi: 10.1089/jwh.2013.4283. [DOI] [PubMed] [Google Scholar]
- Jones RK, Kooistra K. Abortion incidence and access to services in the United States, 2008. Perspectives on Sexual and Reproductive Health. 2011;43(1):41–50. doi: 10.1363/4304111. [DOI] [PubMed] [Google Scholar]
- Jones RK, Finer LB, Singh S. Characteristics of US abortion patients, 2008. New York: Guttmacher Institute; 2010. [Google Scholar]
- Jones RK, Jerman J. Abortion incidence and service availability in the United States, 2011. Perspectives on Sexual and Reproductive Health. 2014;46(1) doi: 10.1363/46e0414. http://dx.doi.org/10.1363/46e0414. [DOI] [PubMed] [Google Scholar]
- Jones RK, Zolna MR, Finer LB, Henshaw SK. Abortion in the United States: Incidence and Access to Services, 2005. Perspectives on Sexual and Reproductive Health. 2008;40(1):6–16. doi: 10.1363/4000608. [DOI] [PubMed] [Google Scholar]
- Jones RK, Upadhyay UD, Weitz TA. At what cost? Payment for abortion care by U.S. women. Women’s Health Issues. 2013;23(6):e173–e178. doi: 10.1016/j.whi.2013.03.001. [DOI] [PubMed] [Google Scholar]
- National Center for Health Statistics. Births, marriages, divorces, and deaths: provisional data for 2008. National Vital Statistics Reports. 2009;57(19) Table B. [PubMed] [Google Scholar]
- National Center for Health Statistics. [Accessed September 30, 2013];Vintage 2012 bridged-race postcensal population estimates. 2013 Available: http://www.cdc.gov/nchs/nvss/bridged_race/data_documentation.htm#vintage2012.
- Pew Research Center for People and the Press. [Accessed November 30, 2013];Widening regional divide over abortion laws. 2013 Available: http://www.people-press.org/2013/07/29/widening-regional-divide-over-abortion-laws/
- Upadhyay UD, Weitz TA, Jones RK, Barar RE, Foster DG. Denial of abortion because of provider gestational age limits in the United States. American Journal of Public Health. 2013 Aug 15; doi: 10.2105/AJPH.2013.301378r. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Bebber SL, Phillips KA, Weitz TA, Gould H, Stewart F. Patient costs for medication abortion: Results from a study of five clinical practices. Women’s Health Issues. 2006;16(1):4–13. doi: 10.1016/j.whi.2005.07.006. [DOI] [PubMed] [Google Scholar]