Abstract
Background:
The incidence of cesarean section is increased. About 3–30% of the women who undergo cesarean experience surgical site infections (SSIs). Many methods, have been used to decrease the incidence of SSIs, but despite much effort, no definite efficacious method has been suggested.
Materials and Methods:
In this parallel, single-blinded, randomized control trial, 56 women with post-surgical superficial wound dehiscence were divided into two groups in a 1:1 ratio. One group was irrigated with normal saline for irrigation and Firooz® baby soapand the other with normal saline for irrigation and povidone-iodine. Formation of granulation tissue was monitored in both groups. Also, the reason for surgery, length of wound dehiscence, and duration of hospitalization and wound union after were compared in both group's.
Results
The soap group patients were irrigated for 4.18 ± 1.96 days compared to 5.36 ± 2.83 days for the patients in povidone-iodine group (P = 0.414). The granulation tissue was formed after 3.88 ± 1.94 days in the soap group compared to 4.48 ± 2.92 days in the other group (P = 0.391), and the duration of hospitalization was 5.48 ± 2.04 days in the soap group compared to 6.3 ± 2.95 days in the other group (P = 0.423). So, no differences were observed between the two groups.
Conclusion:
It can be concluded since there is no difference between the results of two groups, irrigation with normal saline and soap is safe, easy and causes no harm or allergy compared with povidone iodine and normal saline.
Keywords: Iran, randomized controlled trial, surgical wound dehiscence, therapeutic irrigation
INTRODUCTION
The incidence of cesarean section has increased during the past decades. In the United States, about 29.1% of the births occur by cesarean.[1] About 3–30% of the women who undergo cesarean experience surgical site infections (SSIs).[2,3,4,5] Maternal obesity, many pelvic examinations, diabetes mellitus, internal monitoring, and infections such as chorioamnionitis increase the risk of SSIs.[6,7,8] As the incidence of these risk factors increases, the incidence of complications of surgical wounds, such as infection, seroma, hematoma, and wound dehiscence also increases.[6,9,10,11] Many methods, including administering antibiotics for prophylaxis before surgery, skin preparation techniques, and subcutaneous drainages, have been used to decrease the incidence of SSIs.[6,12,13,14] Wound dehiscence refers to the wounds that open more than 1 cm and those form hematoma or seroma getting infected.[2,9] An open wound should be evaluated for signs of bacterial growth, exudates, necrotic tissues, or opened sutures. Many wound protection methods that create a proper condition for wound healing exist. These methods include using nontoxic detergent solutions, enzymes that remove necrotic tissues, and absorbent materials that control drainage.[15] However, another problem is that this kind of treatment is time consuming[16] because povidone-iodine delays granulation tissue formation. it should not remain in the wound, the wound needs to be debrided every time, and a second person is required, unlike the soap method that needs debridement only for the first cleaning and no one's help is required. One of the methods that has been used to treat a reopened wound is cleansing with water and soap.[7,17] A benefit of this method is that a reliable patient can perform it at home using soap without needing another person. The wound will be closed if granulation tissue forms. This method does not need long-term hospitalization and reduces the expenses. Soap is an antiseptic substance and there is no soap-related harm reported until now. No complications have been reported with water and soap.[7] Since no studies have compared these two methods (we really tried, but could not find any study similar to this research), we decided to compare the effects of water and soap irrigation with betadine and normal saline irrigation in patients who experienced wound dehiscence after episiotomy, laparotomy, and cesarean section, in order to find an easier and more effective method.
MATERIALS AND METHODS
This was a parallel, single-blinded (patients), randomized control trial that was conducted in Shariati Hospital of Bandar Abbas, Iran in 2012. In this study, 56 women were enrolled from all the women between 10 and 60 years of age who attended Shariati Hospital due to wound dehiscence after laparotomy, episiotomy, and cesarean section. To determine the sample size, the formula of  was used. Based on the available data
was used. Based on the available data  prevalence of SSI (6.4%), and d = 0.05], the sample size was calculated as 93 patients. Convenience sampling was used to select patients. Later, 37 patients were excluded from the study because of inappropriate follow-up. The patients who were not willing to participate, had inappropriate follow-up, or had a history of steroidusewereexcluded.
prevalence of SSI (6.4%), and d = 0.05], the sample size was calculated as 93 patients. Convenience sampling was used to select patients. Later, 37 patients were excluded from the study because of inappropriate follow-up. The patients who were not willing to participate, had inappropriate follow-up, or had a history of steroidusewereexcluded.
Only if a patient had fever, we administered antibiotics. We explained about the risk factors of wound dehiscence to the patients. Blocked randomization was used to allocate the patients in two groups in a 1:1 ratio because this method ensures equal treatment allocation within each block if the complete block is used. The wounds of patients of the control group were irrigated by normal saline and povidone iodine while normal saline for irrigation and Firooz ® baby soap were used to irrigate the subjects’ wounds. This study was approved by the ethics committee of Hormozgan University of Medical Sciences and all the participants gave an informed written consent. Every patient was visited by a certified, blinded gynecologist and the wound dehiscence was scored based on the amount of dehiscence as follows: 1 point for dehiscence less than a third of the length of the wound, 2 points for two thirds, and 3 points for a full dehiscence. In the water and soap group, after wound debridement, the wound was in contact with soaps for 15 min and then washed with water. This task was done every 8 h. The wounds were evaluated every day by a gynecologist, and after the formation of a granulation tissue, the patients were transferred to the operating room to close the wound. The treatment was changed to povidone-iodine and normal saline if no improvement was seen. In the other group the wounds were irrigated with betadine and 500 ml of normal saline for three times, and after the formation of granulation tissue, the wounds were closed in the same operating room. Necessary data were collected based on a self-constructed checklist that contained demographic and clinical findings (pregnancy history, number of children living, length of the wound dehiscence, granulation tissue formation, etc.). After data collection, SPSS 16 software was used for description and analysis. Independent sample t-test was used to compare the scores of the patients on the first, third, and fifth days and (because we could not find similar studies, and also, healing of wound is usually expected during these days) to compare the hospitalization length. Also, demographic data were compared using Chi-square and t-tests.
RESULTS
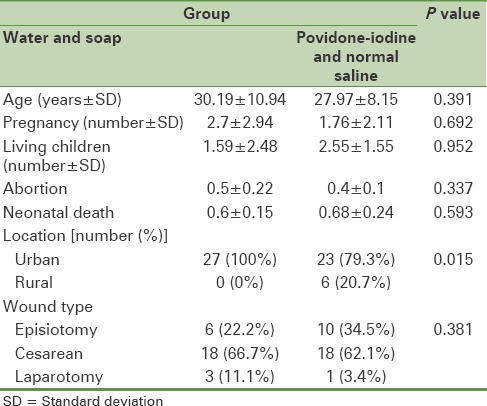
In this study, 56 participants were enrolled of whom 27 (48.2%) participants were in the water and soap group and 29 participants (51.8%) were in the povidone-iodine and normal saline group. As shown in Table 1, the difference between the baseline characteristics of the two groups was not significant. Previous cesarean was the most common reason for surgery among patients of the two groups. Because of lack of the patient's cooperation, BMI in some of the patients’ couldn’t be calculated, so this index couldn’t be compared in the two groups The length of the wound dehiscence was less than two thirds in 7 cases (25.9%) and the wound was totally open in 20 cases (74.1%) in the water and soap group. In the povidone-iodine and normal saline group, the amount of wound dehiscence was below a third of the wound in one patient (3.4%), whereas it was totally open in 20 patients (69%) and was in between in 8 cases (27.6%). The difference between the amounts of wound dehiscence was not statistically significant (P = 0.608). The wound of the patients in the water and soap group was irrigated for 4.18 ± 1.96 days versus 5.36 ± 2.83 days for patients in the betadine group. This difference was not significant (P = 0.414). The granulation tissue formed after 4.48 ± 2.92 days in the betadine and normal saline group and after 3.88 ± 1.94 days in the water and soap group. This difference also was not significant (P = 0.391). The duration of hospitalization was 6.3 ± 2.95 days in the normal saline group and 5.48 ± 2.04 days in the water and soap group. The difference between the duration of hospitalization in the two groups was not significant (P = 0.423). None of the patients in the water and soap group experienced wound dehiscence, while the wounds of two patients (7.4%) in the normal saline group opened again and had to be closed for the third time. This difference was not statistically significant (P = 0.49).
Table 1.
Comparison of the baseline characteristics of the patients between two groups
DISCUSSION AND CONCLUSION
We used an alternative method for the management of wound dehiscence after cesarean, laparotomy, and episiotomy and compared it to the traditional treatment (using betadine and normal saline irrigation) in this randomized clinical trial. Betadine is an effective antiseptic[18] which is routinely used for irrigation of dehiscent wounds. Despite antibiotic prophylaxis, different surgical techniques, and preventive recommendations, wound dehiscence is still a major problem after surgeries. Infection, obesity, and uncontrolled diabetes are the main risk factors for wound dehiscence. Therefore, there is a need for safer, more effective, and less expensive treatments. Most studies have focused on the risk factors of wound dehiscence and how to prevent them. The results of our study reveal that normal saline forirrigation and Firooz ® baby soap is as effective as povidone iodine and normal saline. It is safe, easy, and causes no harm or allergy. According to our findings, this new treatment does not change the prognosis or the duration of hospitalization. However, it leads to faster recovery. The success obtained may be related to the antiseptic effects of soap. Other studies showed that the length of the wound and steroid use prior to surgery are the major risk factors for SSIs in patients who undergo cesarean.[19] In this study, there was no difference between the lengths of the wounds of the two groups. Also, no patients reported any history of steroid use.
In this study, all the wounds closed after irrigation. It has been shown that wound closure improves after obstetrics and gynecology surgeries.[20] Closing opened wounds is safe and decreases the recovery time.[21] Also, new guidelines recommend secondary wound closure of the dehiscent wounds.[15] It has been reported that early closure of dehiscent wounds is effective and safe.[22,23] Using water and soap for wound irrigation is a safe and effective method for the treatment of dehiscent wounds after cesarean, episiotomy, and laparotomy. Some of the patients of the water and soap group were not willing to follow their course at home and wanted to finish their treatment in the hospital, and the benefit of this method is that the patients could be followed on an outpatient basis. The limitation of this study was its small sample size. If this clinical trial is carried out in phase 3 or 4 and includes larger number of patients, more accurate results would be obtained, and for our hospital, it would be beneficial in decreasing the length of stay and decreasing the expenses of the patients. Thus, further studies need to be performed to compare the impact of soap and water in the treatment of wound dehiscence with that of normal saline plus povidone-iodine.
Financial support and sponsorship
This study was funded by Hormozgan University of Medical Sciences.
Conflicts of Interest
There are no conflicts of interest.
Acknowledgment
This study was extracted from the thesis of a medical student. The authors would like to thank all medical staff who were involved in the study and helped them during the study.
REFERENCES
- 1.Martin JA, Hamilton BE, Menacker F, Sutton PD, Mathews T. Preliminary births for 2004: Infant and maternal health. Health E-stats. National Center for Health Statistics. 2005 [PubMed] [Google Scholar]
- 2.Jain S, Jain M, Purwar S, Jain V, Jain P. Negative pressure wound therapy for post-cesarean, post-hysterectomy dehisced abdominal wounds. J Med Soc. 2012;26:171–4. [Google Scholar]
- 3.Bagnall NM, Vig S, Trivedi P. Surgical-site infection. Surgery (Oxford) 2009;27:426–30. [Google Scholar]
- 4.Bärwolff S, Sohr D, Geffers C, Brandt C, Vonberg RP, Halle H, et al. Reduction of surgical site infections after Caesarean delivery using surveillance. J Hosp Infect. 2006;64:156–61. doi: 10.1016/j.jhin.2006.06.009. [DOI] [PubMed] [Google Scholar]
- 5.Nuthalapaty FS, Rouse DJ. The impact of obesity on obstetrical practice and outcome. Clin Obstet Gynecol. 2004;47:898–913. doi: 10.1097/01.grf.0000135358.34673.48. [DOI] [PubMed] [Google Scholar]
- 6.Owens CD, Stoessel K. Surgical site infections: Epidemiology, microbiology and prevention. J Hosp Infect. 2008;70(Suppl 2):3–10. doi: 10.1016/S0195-6701(08)60017-1. [DOI] [PubMed] [Google Scholar]
- 7.Leaper DJ. Surgical-site infection. Br J Surg. 2010;97:1601–2. doi: 10.1002/bjs.7275. [DOI] [PubMed] [Google Scholar]
- 8.Biondo S, Kreisler E, Fraccalvieri D, Basany EE, Codina-Cazador A, Ortiz H. Risk factors for surgical site infection after elective resection for rectal cancer. A multivariate analysis on 2131 patients. Colorectal Dis. 2012;14:e95–102. doi: 10.1111/j.1463-1318.2011.02798.x. [DOI] [PubMed] [Google Scholar]
- 9.Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and TRends in obesity among US adults, 1999-2008. JAMA. 2010;303:235–41. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 10.Davies GA, Maxwell C, McLeod L, Gagnon R, Basso M, Bos H, et al. SOGC Clinical Practice Guidelines: Obesity in pregnancy. No. 239, February 2010. Int J Gynaecol Obstet. 2010;110:167–73. doi: 10.1016/j.ijgo.2010.03.008. [DOI] [PubMed] [Google Scholar]
- 11.Olsen MA, Butler AM, Willers DM, Devkota P, Gross GA, Fraser VJ. Risk factors for surgical site infection after low transverse cesarean section. Infect Control Hosp Epidemiol. 2008;29:477–84. doi: 10.1086/587810. [DOI] [PubMed] [Google Scholar]
- 12.Anderson DJ, Kaye KS, Classen D, Arias KM, Podgorny K, Burstin H, et al. Strategies to prevent surgical site infections in acute care hospitals. Strategies. 2008;29:S51–61. doi: 10.1086/591064. [DOI] [PubMed] [Google Scholar]
- 13.Bratzler DW, Houck PM. Surgical Infection Prevention Guideline Writers Workgroup. Antimicrobial prophylaxis for surgery: An advisory statement from the National Surgical Infection Prevention Project. Am J Surg. 2005;189:395–404. doi: 10.1016/j.amjsurg.2005.01.015. [DOI] [PubMed] [Google Scholar]
- 14.Opøien HK, Valbø A, Grinde-Andersen A, Walberg M. Post-cesarean surgical site infections according to CDC standards: Rates and risk factors. A prospective cohort study. Acta Obstet Gynecol Scand. 2007;86:1097–102. doi: 10.1080/00016340701515225. [DOI] [PubMed] [Google Scholar]
- 15.Sarsam SE, Elliott JP, Lam GK. Management of wound complications from cesarean delivery. Obstet Gynecol Surv. 2005;60:462–73. doi: 10.1097/01.ogx.0000166603.43959.aa. [DOI] [PubMed] [Google Scholar]
- 16.Wechter ME, Pearlman MD, Hartmann KE. Reclosure of the disrupted laparotomy wound: A systematic review. Obstet Gynecol. 2005;106:376–83. doi: 10.1097/01.AOG.0000171114.75338.06. [DOI] [PubMed] [Google Scholar]
- 17.Nthumba PM, Stepita-Poenaru E, Poenaru D, Bird P, Allegranzi B, Pittet D, et al. Cluster-randomized, crossover trial of the efficacy of plain soap and water versus alcohol-based rub for surgical hand preparation in a rural hospital in Kenya. Br J Surg. 2010;97:1621–8. doi: 10.1002/bjs.7213. [DOI] [PubMed] [Google Scholar]
- 18.Durani P, Leaper D. Povidone–iodine: Use in hand disinfection, skin preparation and antiseptic irrigation. Int Wound J. 2008;5:376–87. doi: 10.1111/j.1742-481X.2007.00405.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.De Vivo A, Mancuso A, Giacobbe A, Priolo A, De Dominici R, Maggio Savasta L. Wound length and corticosteroid administration as risk factors for surgical site complications following cesarean section. Acta Obstet Gynecol Scand. 2010;89:355–9. doi: 10.3109/00016340903568175. [DOI] [PubMed] [Google Scholar]
- 20.Boesch CE, Umek W. Effects of wound closure on wound healing in gynecologic surgery: A systematic literature review. J Reprod Med. 2009;54:139–44. [PubMed] [Google Scholar]
- 21.Wechter ME, Pearlman MD, Hartmann KE. Reclosure of the disrupted laparotomy wound: A systematic review. Obstet Gynecol. 2005;106:376–83. doi: 10.1097/01.AOG.0000171114.75338.06. [DOI] [PubMed] [Google Scholar]
- 22.Rose CH, Blessitt KL, Araghizadeh F, Morrison JC. Episiotomy dehiscence that required intestinal diversion. Am J Obstet Gynecol. 2005;193:1759–60. doi: 10.1016/j.ajog.2005.08.037. [DOI] [PubMed] [Google Scholar]
- 23.Jovanovic NS, Kocijancic DM, Terzic MM. Current approach to episiotomy: Inevitable or unnecessary? Cent Eur J Med. 2011;6:685–90. [Google Scholar]


