Abstract
Background
Person-centered approaches to the study of behavior change, such as repeated measures latent class analysis (RMLCA), can be used to identify patterns of change and link these to later behavior change outcomes.
Methods
Daily smoking status data from three smoking cessation studies (N=287, N=334, and N=403) were submitted to RMLCA to identify latent classes of smokers based on patterns of abstinence across the first 27 days of a quit attempt. Three-month biochemically verified abstinence rates were compared among latent classes with particular patterns of smoking across days. Pharmacotherapy variables and baseline individual differences were added as covariates of latent class membership.
Results
Results of separate and pooled analyses supported a five-class solution that replicated across studies. Latent classes included a large class that achieved immediate stable abstinence, a smaller class of cessation failures, and three classes with partial abstinence that increased, decreased, or remained stable over time. Three-month point-prevalence abstinence rates varied among the latent classes, with 38–55% abstinent among early quitters, 3–20% abstinent among those who smoked intermittently throughout the first 27 days, and fewer than 5% abstinent in the classes marked by little or delayed change in smoking. High-dose nicotine patch and bupropion promoted membership in abstinent classes. Demographics, nicotine dependence, and craving were related to latent class in multiple studies and pooled analyses.
Conclusions
We identified five patterns of smoking behavior in the first weeks of a smoking cessation attempt. These patterns are robust across multiple studies and are related to later point-prevalence abstinence rates.
Keywords: Smoking, Tobacco, Cessation, Repeated Measures Latent Class Analysis
1. INTRODUCTION
1.1 Person-centered approaches to the study of relapse
As with many drugs of abuse, relapse remains the most common outcome of attempts to quit smoking (Fiore et al., 2008). Success in quitting is typically measured in binary terms and at discrete time-points (Hughes et al., 2003). This approach is useful in assessing the health impact of smoking cessation treatments, but masks the pathways by which individuals change. Person-centered analysis of abstinence in the first weeks of quitting may reveal meaningful heterogeneity in responses to treatment and aid in identifying risk and protective factors associated with different paths to abstinence or relapse to smoking.
1.2 Modeling change
Relapse has long been recognized as a nonlinear process (Brandon et al., 2007; Shiffman, 1989) requiring nonlinear analytical approaches. In a recent effort to describe patterns of abstinence during a smoking cessation attempt, a repeated measures latent class analysis (RMLCA) of daily smoking in 1,433 adult smokers from a trial of five active pharmacotherapies and placebo medication (Piper et al., 2009) yielded five latent classes (McCarthy et al., 2015). The most common patterns were stable success or failure in quitting. Less common patterns indicated unstable patterns of behavior during the first 27-days post-quit, with some establishing initially high probabilities of abstinence and then relapsing, others reducing the frequency of smoking early in the quit attempt, and others reporting initial smoking but then markedly increasing abstinence. The latent classes differed in six-month abstinence rates, suggesting that monitoring early smoking patterns may help identify individuals at high risk of longer-term smoking.
1.2.1 Treatment effects on change processes
Modeling change patterns may facilitate treatment evaluation and refinement. Comparing treatments based on their ability to promote early change patterns may tell us more than will the evaluation of distal outcomes. This process approach may also suggest ways to identify individuals who do not initially respond to treatment and who may benefit from adaptive interventions (Rose and Behm, 2014).
1.2.2 Risk and protective factors
Although most smokers who attempt to quit smoking will ultimately relapse, this homogeneity of the distal outcome (relapse) masks considerable heterogeneity of the smoking relapse process (McCarthy et al., 2006). Identifying stable risk and protective factors associated with particular change processes may foster development of treatment-matching protocols to boost cessation success (Witkiewitz et al., 2010). An RMLCA (McCarthy et al., 2015) showed that latent classes of smokers differed in nicotine dependence, smoking history, initial quitting confidence, sleep problems, and ethnic identification. It is important to replicate such findings to identify candidate variables for inclusion in treatment algorithms.
1.3 Study aims
The current study aims to replicate our previous analysis (McCarthy et al., 2015) in three independent smoking cessation studies (Shiffman et al., 1996, 1997; McCarthy et al., 2008) and extend it to new treatment conditions. All studies offered treatment (counseling, patch, and/or bupropion) to smokers motivated to quit and assessed smoking status both in real time using ecological momentary assessment (EMA; Stone and Shiffman, 1994) via palmtop computer, and frequent time-line follow-back (TLFB) assessments. Daily abstinence status in the first 27 days of a quit attempt was analyzed using RMLCA to identify the latent classes of abstinence patterns in each study. Analyses addressed relations between 3-month outcomes, treatments, and relapse-relevant covariates and latent class.
Based on results from the six-arm pharmacotherapy trial (McCarthy et al., 2015), we hypothesized that high-dose nicotine patch treatment would facilitate early quitting, whereas bupropion would support recovery from early smoking. Based on an earlier study of counseling effects on lapse reactions (McCarthy et al., 2010), we expected counseling to promote recovery pattern. We also hypothesized that known relapse risk factors including gender, racial minority status, nicotine dependence, quitting confidence, and baseline craving and affective distress would be associated with membership in latent abstinence classes across studies, but did not make a priori hypotheses about cross-study variation in these relations.
2. METHODS
The design and sample characteristics of each of the three studies are summarized in Tables 1 and 2. Each of these studies has been described previously (e.g., Study 1: Shiffman et al., 1996; Study 2: Shiffman et al., 2006; Study 3: McCarthy et al., 2008a, 2008b). All three studies provided: treatment to adult daily smokers motivated to quit smoking at no-cost, compensation for participation, and palmtop computers to record experiences and behaviors up to nine times per day. In all three studies, latent class membership was defined based on daily smoking status indicators collected via EMA (when available) or TLFB data on daily smoking. All three studies assessed biochemically verified seven-day point-prevalence abstinence between 2.5 and 4 months post-quit.
Table 1.
Summary of study design, sample sizes, and inclusion and exclusion criteria by study.
|
Study
1 (N=287) |
Study
2 (N=334) |
Study
3 (N=407) |
|
|---|---|---|---|
| Study design | Prospective longitudinal study |
Randomized, double-blind nicotine patch |
Randomized, crossed factorial |
| Treatments | Group CBTa | Patchb, Group CBTc |
Bupropiond, Counselinge |
| Days of EMA: pre-quit / post-quit | 16 / 26 | 14 / 56 | 14 /28 |
| Number of clinic visits | 8 | 11 | 11 |
| Number of counseling sessions | 8 | 7 | 8 |
| Payment ($) | 50 | 150 | 200 |
| Distal 7-day abstinence outcome (weeks post-quit) |
6–16 | 11 | 12 |
| Biochemical validation: CO ppm/ cotinine ng/ml |
≤ 8 / < 15 | ≤ 8 / < 15 | ≤ 10 / < 15 |
| Inclusion Criteria | |||
| Age (years) | ≥ 18 | ≥ 21 and ≤65 | ≥ 18 |
| Years of smoking | ≥ 2 | ≥ 5 | |
| Cigarettes/day | ≥ 10 | ≥ 15 | ≥ 10 |
| Baseline CO (ppm) | ≥ 10 | ||
| Exclusion Criteria | Study 1 | Study 2 | Study 3 |
| Use of other tobacco | X | X | |
| Other drug or alcohol abuse | X | X | |
| Contraindications to nicotine patch | X | ||
| Recent bupropion treatment | X | ||
| Body weight < 110 lbs. | X | ||
| Using mood-altering/sedating meds | X | ||
| Reversed/shifted wake-sleep cycle | X | ||
| Serious lung disease | X | ||
| Participation in another study | X | X | |
| Pregnancy or breast feeding | X | X | |
| Living with an enrolled participant | X | X | |
| History of bipolar or psychosis | X | X | |
| Current depression | X | ||
| Contraindications to bupropion use | X | ||
8 60-minute group sessions of cognitive behavior therapy for smoking cessation.
Participants were randomly assigned to wear either 35 mg for 3 weeks, 21 mg for 2 weeks, and placebo for 1 week or placebo patches daily for six weeks post-quit.
All participants were encouraged to attend 7 60-minute group sessions of cognitive behavior therapy for smoking cessation.
Participants were randomly assigned to take active bupropion SR (150 mg for 4 days then 300 mg for 59 days) or placebo pills (63 days) beginning one week pre-quit.
Participants were randomly assigned to receive 8 individual, face-to-face 10-minute smoking cessation counseling sessions or no counseling.
Table 2.
Sample characteristics and covariate values in all three studies and the pooled sample.
| Study 1 (N=287) |
Study 2 (N=334) |
Study 3 (N=407) |
Pooled (N=1028) |
|||||
|---|---|---|---|---|---|---|---|---|
| Covariate | Mean | SD | Mean | SD | Mean | SD | Mean | SD |
| Age in years | 42.4 | 10.0 | 39.5 | 9.4 | 39.0 | 12 | 40.1 | 10.7 |
| Years of educationa | 9.3 | 3.8 | 8.9 | 3.8 | 13.9 | 1.7 | 11.0 | 4.0 |
| FTNDb | 5.9 | 2.2 | 6.5 | 2.0 | 5.0 | 2.3 | 3.7 | 3.2 |
| Cigarettes per day | 27.0 | 11.6 | 24.1 | 8.9 | 21.7 | 10.4 | 24.0 | 10.5 |
| Years Smoked | 22.9 | 12.1 | 22.1 | 9.6 | 21.2 | 11.3 | 22.0 | 11.0 |
| No. past quit attempts | 2.5 | 3.1 | 4.0 | 4.4 | 5.6 | 10.7 | 4.2 | 7.6 |
| Most days abstinent | 330.2 | 665.4 | 97.9 | 90.9 | 116.2 | 137.2 | 167.9 | 368.9 |
| Pre-quit self-efficacyc | 4.0 | 0.8 | 8.9 | 1.6 | 1.5 | 0.9 | 4.6 | 3.4 |
| Pre-quit cravingd | 5.4 | 2.0 | 7.6 | 1.3 | 5.8 | 2.1 | 6.4 | 2.1 |
| Pre-quit sleepe | 2.1 | 0.3 | 5.7 | 0.5 | 5.2 | 0.9 | 4.7 | 1.5 |
| Pre-quit negative affectf | −0.1 | 0.5 | 0.1 | 0.7 | 3.2 | 1.5 | 1.3 | 1.9 |
| Pre-quit positive affectg | 0.1 | 0.7 | 7.4 | 2.0 | ||||
| Pre-quit CES-D-brief formh | 1.5 | 0.5 | 1.9 | 1.2 | 0.2 | 0.4 | 1.1 | 1.1 |
| Pre-quit low arousali | 0.0 | 0.5 | 0.1 | 0.5 | ||||
| Pre-quit inattentionj | −0.1 | 0.6 | 2.6 | 1.3 | ||||
| STAIk | 1.9 | 0.5 | ||||||
| STASl | 3.0 | 2.3 | ||||||
| Demographics | n | % | n | % | n | % | n | % |
| Gender (% Female) | 122 | 42.2% | 162 | 48.5% | 204 | 50.1% | 486 | 47.3% |
| Race | ||||||||
| White | 262 | 91.3% | 284 | 85.0% | 363 | 89.2% | 909 | 88.4% |
| African American | 19 | 6.6% | 37 | 11.1% | 22 | 5.4% | 78 | 7.6% |
| Other | 3 | 1.0% | 12 | 3.6% | 14 | 3.4% | 29 | 2.8% |
| Hispanic | 3 | 1.0% | 1 | 0.3% | 8 | 2.0% | 12 | 1.2% |
Education was a categorical variable transformed into a count of years of education by assigning the value at the midpoint of the range in the category selected (e.g., assigning those who said they had some college but did not earn a college degree a value of 14) years.
FTND=Fagerström Test of Nicotine Dependence (Heatherton, Koslowski, Frecker, & Fagerström, 1991)
In Studies 1 and 2, this is the mean of pre-quit EMA responses to “Confident in ability to abstain?” (on a 1–4 scale in Study 1, and on a 1–11 scale in Study 2 where 1=“NO!!” and 4/11= “YES!!”). In Study 3, this was assessed with a baseline item “If you try to quit smoking within the next 30 days, how likely is it that you will be successful?” on a 7-point scale where 1=“Very successful” and 7=“Not at all successful.”
In Studies 1 and 2, this is the mean of ratings of “Cigarette Craving” (rated on 1–4 scale in Study 1, and on 1–11 scale in Study 2). In Study 3, this is the pre-quit mean of ratings of “Urge(s) to smoke?” and “Bothered by desire to smoke?” rated 1–11 as in Study 2.
In Studies 1 and 2, this is the pre-quit mean of morning EMA items: “Trouble falling asleep?”, “Do you feel well rested?” (reverse coded), “Number of wakenings?”, “Rate how well you slept” (from “very well” to “not well at all”), and “Do you feel tired?” rated on 4-point scales in Study 1 and 10-point scales in Study 2 (except for number awakenings which was entered as 0–99). In Study 3, this was the pre-quit morning EMA mean of “Right now-Well rested?” and “Last night-Trouble falling asleep?” ratings rated on 1–11 scales.
In Studies 1 and 2, this is the pre-quit factor score for the following items: (“How feeling? Happy”, “irritable”, “miserable”, “tense”, “contented”, “frustrated/angry”, “sad”, and “overall feeling”) (see Shiffman et al., 1996 for details). In Study 3, this is the mean of EMA random prompt items “Tense or anxious?” and “Sad or depressed?” rated on a 11-point scale.
In Study 2, this is a factor score defined by happy, contented, calm, and overall feeling items rated on a 11-point scale. In Study 3, this is the mean of PANAS items “Enthusiastic” and “Interested.” rated on 11-point scales.
Mean of pre-quit responses to items from the Center for Epidemiologic Studies-Depression (CES-D) Scale (Radloff, 1977): “Have you felt depressed?”, “Have you felt lonely?”, and “Felt you could not shake off the blues?” rated via EMA in Studies 1 (on a 4-point scale) and 2 (11-point scale) and via pen-and-paper questionnaire in Study 3 (4-point scale).
Low arousal was assessed by taking the factor score on an factor defined by items “Tired” and “Sleepy” rated on a 4-point scale in Study 1 and 11-point scale in Study 2.
Attention problems were assessed by taking the factor score defined by items “Spacey” and “Hard to concentrate” rated on a 4-point scale in Study 1 and 11-point scale in Study 2.
STAI= Spielberger State-Trait Anxiety Inventory (Spielberger, Gorsuch, Lushene, Vagg, & Jacobs, 1983)
STAS=Spielberger State Anger Scale (Spielberger, Jacobs, Russell, & Crane, 1986)
2.1 Data Analysis
We examined the number and correlates of latent classes that emerged based on daily smoking status in the first 27 days of a quit attempt. The RMLCA approach was adopted to capture time-dependent patterns rather than to estimate probabilities of transitions among latent states, as in hidden Markov models (Killeen, 2011). In addition, RMLCA examines latent smoking patterns without imposing restrictions of patterns across time, whereas hidden Markov models impose autoregressive effects of time where the current state is dependent on prior states.
We conducted both separate and pooled analyses, beginning first with unconditional models and then adding distal outcomes, treatment variables, and standardized covariates. All models assume conditional independence of the daily smoking data (i.e., that all covariation in daily smoking status is fully accounted for by the latent class). Models were estimated using SAS 9.3 (SAS Institute Inc., Cary, NC) via Proc LCA using maximum likelihood estimation with 200 random starts.
2.1.1 Unconditional models
Unconditional models with 1–8 classes were fit to each separate study and to pooled data across studies to identify the optimal number of latent classes based on: interpretability, Bayesian Information Criteria (BIC; Nylund et al., 2006; Schwarz, 1978), BIC adjusted for sample size (aBIC, Sclove, 1987), bootstrapped likelihood ratio test (BLRT, a measure of improvement in model fit with each additional class; McLachlan and Peel, 2000; Nylund et al., 2006), and model entropy (a measure of classification precision).
2.1.2 Distal Outcomes
Distal abstinence outcome (biochemically confirmed point-prevalence abstinence 2.5–4 months post-quit) associations with latent class membership were examined by computing the marginal means of abstinence (0=smoking, 1=abstinence) in each class in each study and in a pooled dataset. Individuals cannot be assigned to latent classes with certainty, but each individual is assigned a posterior probability of membership in each class and these can be used to identify the class to which individuals most likely belong.
2.1.3 Treatment
Treatment was coded using a dummy variable (0=placebo, 1=active patch) in Study 2. In Study 3, three dummy indicators were included to capture the effect of each active treatment (counseling alone, bupropion SR alone, or the combination of counseling and bupropion SR) relative to the no counseling, placebo control group.
2.1.4 Covariates
Covariates were added to explore correlates of latent class membership and to estimate treatment effects on latent class membership (in Studies 2–3). Single covariate models were run first to determine whether each candidate predicted class membership at p<.20. Those that did were included in multivariate models. Only covariates that reached significance in stepwise multivariate models (the two predictors with the lowest p values were added, followed by others in ascending order by univariate p value) were retained in the final model. All continuous covariates were standardized within-study. Missing data are not permitted for covariates in RMLCA and there is not yet a program available to reconcile RMLCA results across multiple imputed datasets. As such, some cases [22 (7.7%) in Study 1, 2 (0.6%) in Study 2, 1 (0.2%) in Study 3, 52 (5.1%) in the pooled analysis] were lost in the conditional models.
3. RESULTS
3.1 Unconditional Models
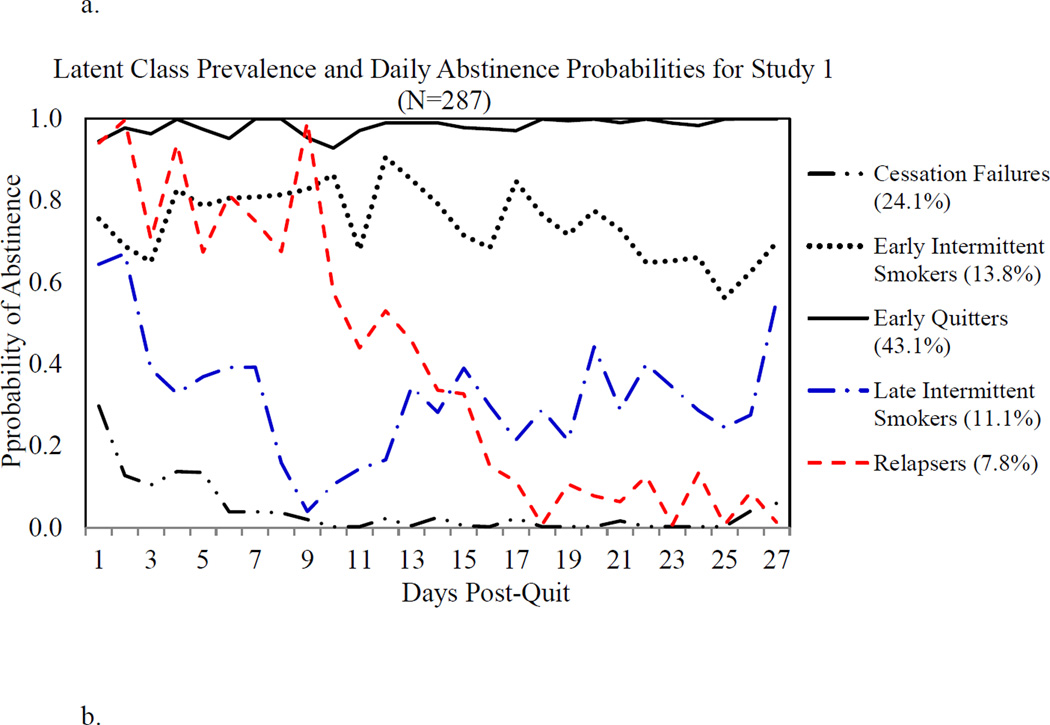
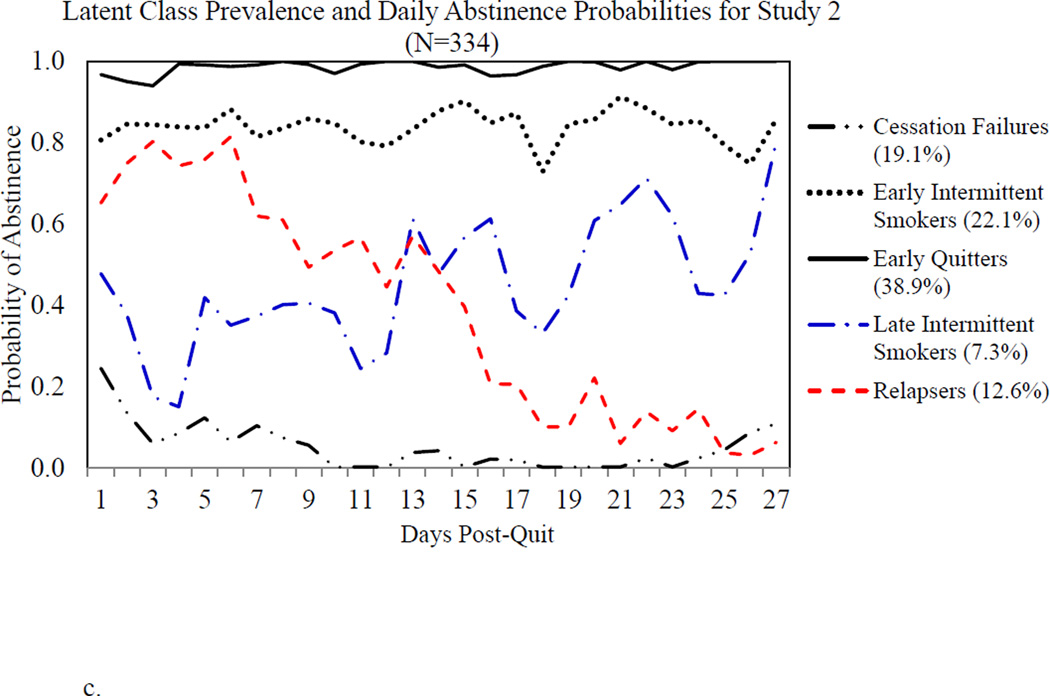
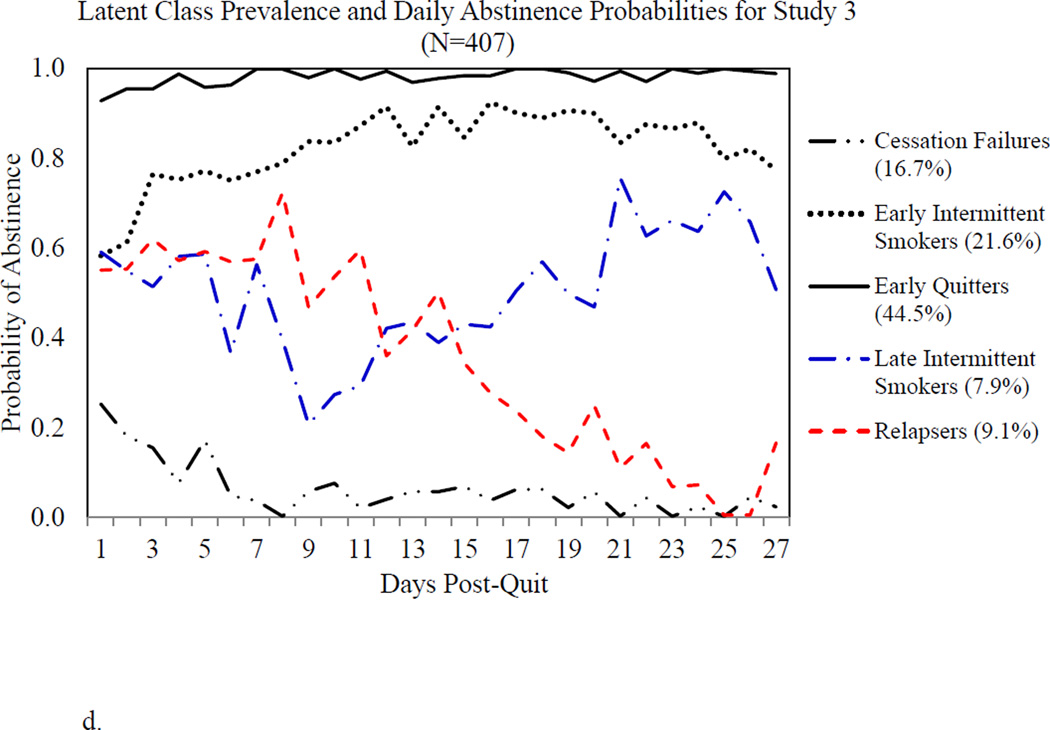
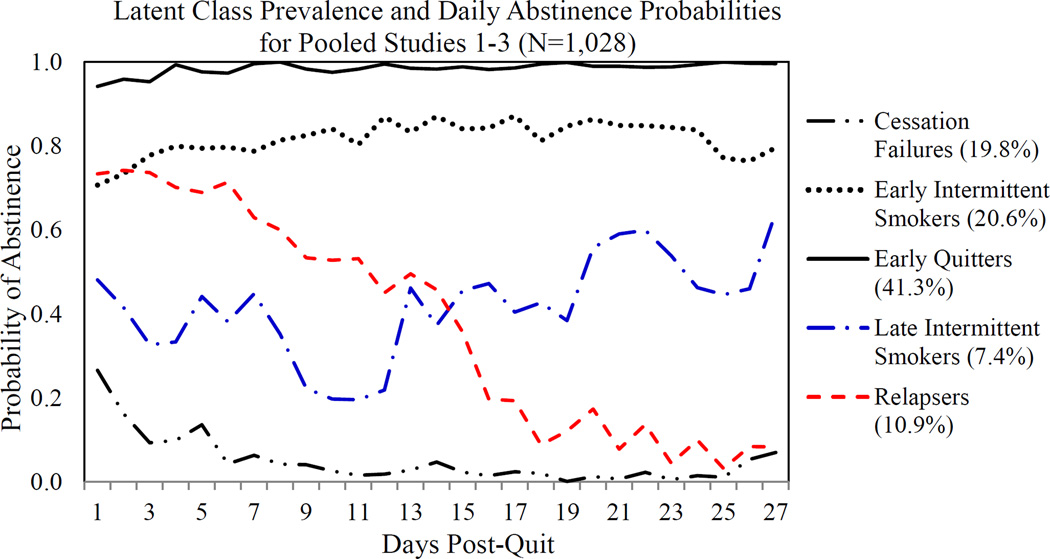
Based on an examination of fit indices, model rho parameters (daily abstinence probabilities within classes), and gamma parameters (latent class prevalences), we retained a 5-class model in all three studies and a pooled analysis (Table 3). Figures 1a–1c display the daily abstinence probabilities and prevalences by latent class for each study and Figure 1d shows the pooled results. As in McCarthy et al. (2015), we have labeled the classes Early Quitters for those who maintain a high probability of abstinence, Cessation Failures for those with near-zero abstinence probabilities, Early Intermittent Smokers for those with intermediate abstinence probabilities, Late Intermittent Smokers for those with initially low abstinence probabilities that increase over days, and Relapsers for those with initially high abstinence probabilities that decline over days. A test of invariance across studies indicated that model fit improved when latent class prevalence and rho parameters were allowed to vary across studies (Δ G2=344.55, df=270, p=.0014), although the nature of the latent classes was strikingly similar across studies (see Figures 1a–c). Tests of invariance are sensitive to minor variations in rho parameters (the analysis considers each day as a separate variable, with no concept of time sequence or adjacency, so even a one-day shift in a smoking transition may appear as a major discrepancy). As an alternative approach to assessing the similarity of the latent class solution across studies, we examined the concordance between assignment of participants to latent classes in the separate versus pooled models. We found a very high rate of concordance (kappa=0.96), confirming the consistency of the latent class solutions across studies.
Table 3.
Pooled and separate model fit indices for unconditional models with 3–6 classes.
| Latent Classes |
Log- likelihood |
df | BIC | BIC | aBIC | aBIC Δ | Entropy | BLRT |
|---|---|---|---|---|---|---|---|---|
| Study 1 | ||||||||
| 3 | −2011 | 134217644 | 2267 | 382 | 2003 | 471 | 0.97 | < 0.001 |
| 4 | −1915 | 134217616 | 2235 | 32 | 1883 | 121 | 0.94 | < 0.001 |
| 5 | −1852 | 134217588 | 2266 | −32 | 1825 | 57 | 0.95 | < 0.001 |
| 6 | −1805 | 134217560 | 2331 | −65 | 1801 | 24 | 0.95 | < 0.001 |
| Study 2 | ||||||||
| 3 | −2865 | 134217644 | 3489 | 424 | 3225 | 513 | 0.96 | < 0.001 |
| 4 | −2747 | 134217616 | 3414 | 74 | 3062 | 163 | 0.93 | < 0.001 |
| 5 | −2665 | 134217588 | 3413 | 1 | 2972 | 90 | 0.93 | < 0.001 |
| 6 | −2610 | 134217560 | 3466 | −53 | 2936 | 36 | 0.93 | < 0.001 |
| Study 3 | < 0.001 | |||||||
| 3 | −3184 | 134217644 | 3585 | 447 | 3321 | 536 | 0.9 | < 0.001 |
| 4 | −3086 | 134217616 | 3557 | 28 | 3205 | 117 | 0.87 | < 0.001 |
| 5 | −3037 | 134217588 | 3626 | −68 | 3185 | 20 | 0.87 | < 0.001 |
| 6 | −2996 | 134217560 | 3712 | −86 | 3182 | 3 | 0.86 | < 0.001 |
| Pooled Analysis: Studies 1–3 | ||||||||
| 3 | −8489 | 134217644 | 7686 | 1445 | 7423 | 1533 | 0.93 | p<.001 |
| 4 | −7886 | 134217616 | 7275 | 411 | 6923 | 500 | 0.90 | p<.001 |
| 5 | −7735 | 134217588 | 7167 | 108 | 6726 | 197 | 0.89 | p<.001 |
| 6 | −7638 | 134217560 | 7167 | 0 | 6636 | 90 | 0.88 | p<.001 |
BIC is the Bayesian information criterion, a measure of model fit; smaller values indicated better fit. aBIC is the BIC adjusted for sample size; smaller values again indicate better fit. Entropy is a measure of the accuracy of classification of participants in latent classes and of class differentiation; higher values indicate better classification. BLRT is the Bootstrap likelihood ratio test, a test of the significance of differences in model fit with the addition of one more latent class; p<.05 indicates a significant change in model fit with a change in the number of latent classes.
Figure 1.
Estimated probability of abstinence from cigarettes by day for the first 27 days of a quit attempt by latent class in Study 1 (panel A), Study 2 (panel B), Study 3 (panel C), and the pooled analysis of Studies 1–3 (panel D). Percentage following each class indicates prevalence of the class.
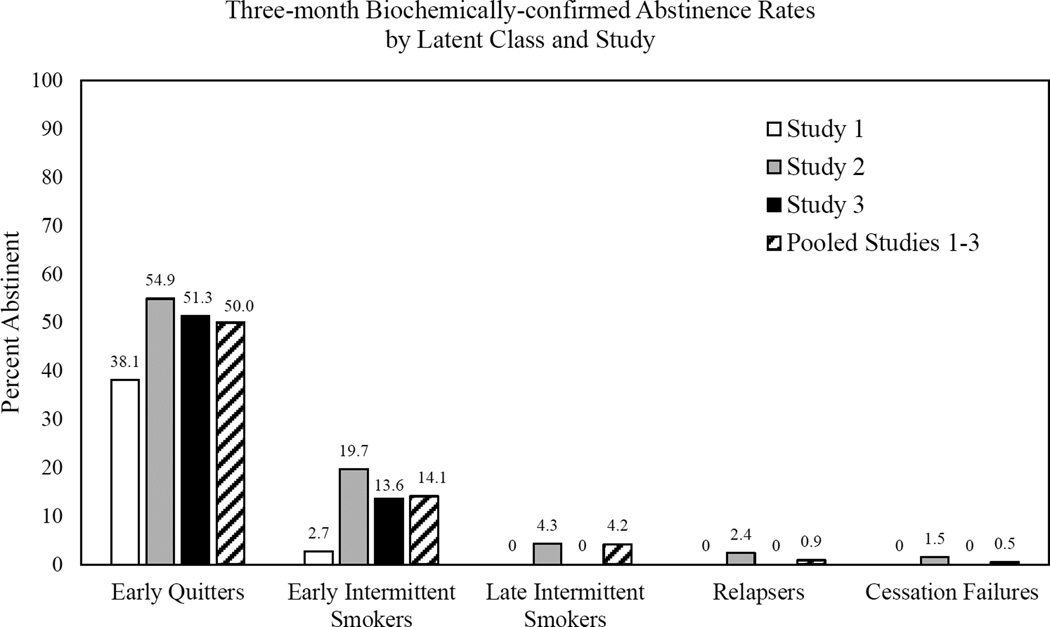
3.2 Distal Outcomes
Confirmed abstinence rates 2.5–4 months post-quit are shown by latent class and study in Figure 2. Only the Early Quitter class had a substantial abstinence rate (38.1%) in Study 1. In Studies 2 and 3, greater than 50% of Early Quitters and nearly 14% (Study 3) and 20% (Study 2) of Early Intermittent Smokers were abstinent three-months post-quit. Abstinence rates were below 5% in all other classes. In the pooled analysis, Early Quitters had significantly higher abstinence rates than all other classes (all ps<=0.001). Early Intermittent Smokers had significantly higher abstinence rates than did Relapsers (p=0.008) or Cessation Failures (p<0.001). Late Intermittent Smokers also had significantly higher abstinence rates than did Cessation Failures (p=0.03).
Figure 2.
Marginal abstinence rates at approximately three months post-target-quit-day by latent class (with participants assigned to a class based on posterior probabilities of membership in each class) by Study. Abstinence was determined by self-report of no smoking in the past seven days at a follow-up interview conducted 2.5 to 4 months post-quit and by carbon monoxide and cotinine.
3.3 Treatment Effects in Studies 2 and 3
Table 4 shows treatment effects on latent class membership in the full final conditional models (i.e., adjusted for the covariates listed in Table 5) for Studies 2 and 3. In Study 2, High-dose patch treatment significantly reduced the odds of being in all transient change classes (Cessation Failure, Relapse, and Late Intermittent Smoking) compared to Early Quitting (Table 4A). Active patch treatment also significantly increased the odds of membership in all change classes compared to Cessation Failure (Table 4B) and increased the odds of sustained Early Intermittent Smoking rather than Relapse (Table 4C). Patch treatment did not differentiate Early and Late Intermittent Smokers (Table 4D).
Table 4.
Odds ratios with 95% Confidence Interval [CI] of latent class membership treatment variables by study.
| Study | Treatment | Early Intermittent | Late Intermittent | Relapse | Cessation Failure |
|---|---|---|---|---|---|
| Panel A: Comparison to Early Quitter Class | |||||
| 2 | Nicotine patch | 0.94 [0.57, 1.56] | 0.50 [0.26, 0.97]* | 0.41 [0.24, 0.68]* | 0.11 [0.07, 0.20]* |
| 3 | Bupropion SR and counseling | 0.73 [0.40, 1.34] | 0.35 [0.17, 0.71]* | 0.56 [0.22, 1.43] | 0.16 [0.08, 0.33]* |
| Bupropion SR alone | 0.48 [0.25, 0.91]* | 0.52 [0.27, 0.98]* | 0.92 [0.40, 2.16] | 0.23 [0.13, 0.43]* | |
| Counseling alone | 0.82 [0.43, 1.57] | 0.88 [0.47, 1.66] | 1.00 [0.41, 2.45] | 0.58 [0.33, 1.03] | |
| Panel B: Comparison to Cessation Failure Class | |||||
| 2 | Nicotine patch | 8.24 [4.49, 15.13]* | 4.37 [2.03, 9.40]* | 3.55 [1.88, 6.70]* | |
| 3 | Bupropion SR and counseling | 4.44 [2.05, 9.61]* | 2.13 [0.91, 4.98] | 3.42 [1.19, 9.88]* | |
| Bupropion SR alone | 2.03 [0.97, 4.21] | 2.20 [1.07, 4.53]* | 3.94 [1.56, 9.97]* | ||
| Counseling alone | 1.41 [0.72, 2.75] | 1.51 [0.78, 2.92] | 1.72 [0.68, 4.35] | ||
| Panel C: Comparison to Relapse Class | |||||
| 2 | Nicotine patch | 2.32 [1.28, 4.22]* | 1.23 [0.57, 2.65] | ||
| 3 | Bupropion SR and counseling | 1.30 [0.48, 3.54] | 0.62 [0.21, 1.84] | ||
| Bupropion SR alone | 0.51 [0.20, 1.33] | 0.56 [0.22, 1.45] | |||
| Counseling alone | 0.82 [0.31, 2.17] | 0.88 [0.33, 2.34] | |||
| Panel D: Comparison to Late Intermittent Smoker Class | |||||
| 2 | Nicotine patch | 1.89 [0.91, 3.94] | |||
| 3 | Bupropion SR and counseling | 2.09 [0.94, 4.64] | |||
| Bupropion SR alone | 0.92 [0.42, 1.99] | ||||
| Counseling alone | 0.94 [0.44, 1.98] | ||||
p < 0.05
Table 5.
Odds ratios with 95% Confidence Interval [CI] of latent class membership by covariate and study.
| Panel A. Gender (1=Female, 0=Male) | |||||
|---|---|---|---|---|---|
| Study | Early Intermittent | Late Intermittent | Relapse | Cessation Failure | |
| Comparison to Early | 1 | 0.90 [0.47, 1.71] | 1.07 [0.56, 2.06] | 1.15 [0.54, 2.43] | 1.76 [0.98, 3.15] |
| Quitter Class | 2 | 2.11 [1.25, 3.57]* | 5.88 [2.38, 14.51]* | 1.33 [0.73, 2.40] | 1.78 [1.05, 3.00]* |
| 3 | 1.55 [1.00, 2.42]* | 2.66 [1.65, 4.28]* | 1.61 [0.87, 30.00] | 2.32 [1.47, 3.65]* | |
| Pooled | 1.46 [1.11, 1.93]* | 2.13 [1.41, 3.22]* | 1.54 [1.10, 2.17]* | 1.80 [1.36, 2.39]* | |
| Comparison to Cessation | 1 | 2.79 [1.08, 7.22]* | 0.84 [0.46, 1.55] | 0.63 [0.32, 1.22] | |
| Failure Class | 2 | 1.19 [0.65, 2.18] | 3.31 [1.27, 8.59]* | 0.75 [0.38, 1.46] | |
| 3 | 0.67 [0.40, 1.13] | 1.15 [0.66, 1.99] | 0.70 [0.35, 1.40] | ||
| Pooled | 0.81 [0.59, 1.12] | 1.19 [0.76, 1.85] | 0.86 [0.59, 1.25] | ||
| Comparison to Relapse | 1 | 0.78 [0.34, 1.83] | 0.94 [0.39, 2.23] | ||
| Class | 2 | 1.59 [0.82, 3.10] | 4.44 [1.64, 12.01]* | ||
| 3 | 0.96 [0.49, 1.90] | 1.65 [0.81, 3.36] | |||
| Pooled | 0.95 [0.65, 1.38] | 1.38 [0.85, 2.26] | |||
| Comparison to Late | 1 | 0.84 [0.39, 1.77] | |||
| Intermittent Smoker Class | 2 | 0.36 [0.14, 0.93]* | |||
| 3 | 0.58 [0.33, 1.02] | ||||
| Pooled | 0.69 [0.44, 1.07] | ||||
| Panel B. Minority (1=Minority, 0=White) | |||||
| Study | Early Intermittent | Late Intermittent | Relapse | Cessation Failure | |
| Comparison to Early | 1 | 0.09 [0.00, 2.02] | 1.96 [0.68, 5.65] | 0.63 [0.14, 2.85] | 1.02 [0.35, 3.02] |
| Quitter Class | 2 | 2.13 [0.98, 4.62] | 4.21 [1.63, 10.89]* | 1.77 [0.73, 4.27] | 2.42 [1.16, 5.07]* |
| 3 | 2.64 [1.44, 4.87]* | 1.09 [0.47, 2.53] | 0.84 [0.26, 2.69] | 1.39 [0.65, 2.95] | |
| Pooled | 1.55 [1.01, 2.37]* | 2.33 [1.34, 4.06]* | 1.01 [0.56, 1.84] | 1.40 [0.88, 2.23] | |
| Comparison to Cessation | 1 | 1.98 [0.72, 5.42] | 1.14 [0.50, 2.59] | 0.83 [0.32, 2.16] | |
| Failure Class | 2 | 0.88 [0.39, 2.00] | 1.74 [0.65, 4.67] | 0.73 [0.29, 1.87] | |
| 3 | 1.91 [0.88, 4.15] | 0.78 [0.30, 2.07] | 0.61 [0.17, 2.22] | ||
| Pooled | 1.10 [0.67, 1.81] | 1.66 [0.90, 3.06] | 0.72 [0.37, 1.39] | ||
| Comparison to Relapse | 1 | 0.14 [0.00, 4.19] | 3.11 [0.61, 15.91] | ||
| Class | 2 | 1.20 [0.46, 3.12] | 2.38 [0.79, 7.22] | ||
| 3 | 3.15 [0.97, 10.25] | 1.29 [0.34, 4.87] | |||
| Pooled | 1.53 [0.82, 2.86] | 2.31 [1.12, 4.78]* | |||
| Comparison to Late | 1 | 0.05 [0.00, 1.08] | |||
| Intermittent Smoker Class | 2 | 0.50 [0.18, 1.38] | |||
| 3 | 2.43 [0.99, 5.99] | ||||
| Pooled | 0.66 [0.37, 1.19] | ||||
| Panel C. Baseline cigarettes/day | |||||
| Study | Early Intermittent | Late Intermittent | Relapse | Cessation Failure | |
| Comparison to Early | 1 | 1.26 [0.85, 1.86] | 0.97 [0.63, 1.48] | 1.43 [0.96, 2.13] | 1.66 [1.19, 2.30]* |
| Quitter Class | 2 | 2.04 [1.42, 2.93]* | 1.23 [0.68, 2.21] | 1.67 [1.11, 2.50]* | 1.39 [0.95, 2.03] |
| 3 | 1.03 [0.78, 1.36] | 0.85 [0.61, 1.18] | 1.14 [0.78, 1.67] | 1.16 [0.89, 1.51] | |
| Pooled | 1.23 [1.05, 1.44]* | 1.06 [0.84, 1.35] | 1.39 [1.16, 1.66]* | 1.32 [1.13, 1.53]* | |
| Comparison to Cessation | 1 | 0.60 [0.33, 1.09] | 0.68 [0.46, 1.01] | 0.82 [0.54, 1.23] | |
| Failure Class | 2 | 1.47 [0.99, 2.18] | 0.89 [0.48, 1.63] | 1.20 [0.77, 1.87] | |
| 3 | 0.89 [0.67, 1.17] | 0.74 [0.52, 1.03] | 0.98 [0.66, 1.45] | ||
| Pooled | 0.94 [0.80, 1.10] | 0.81 [0.63, 1.03] | 1.05 [0.88, 1.27] | ||
| Comparison to Relapse | 1 | 0.88 [0.57, 1.35] | 0.68 [0.42, 1.10] | ||
| Class | 2 | 1.22 [0.81, 1.85] | 0.74 [0.39, 1.38] | ||
| 3 | 0.90 [0.61, 1.35] | 0.75 [0.48, 1.17] | |||
| Pooled | 0.89 [0.74, 1.07] | 0.77 [0.59, 1.00] | |||
| Comparison to Late | 1 | 1.30 [0.82, 2.06] | |||
| Intermittent Smoker Class | 2 | 1.66 [0.91, 3.00] | |||
| 3 | 1.21 [0.85, 1.72] | ||||
| Pooled | 1.16 [0.91, 1.48] | ||||
| Panel D. Baseline FTND | |||||
| Covariate | Study | Early Intermittent | Late Intermittent | Relapse | Cessation Failure |
| Comparison to Early | 1 | 1.04 [0.57, 1.90] | 3.89 [1.95, 7.78]* | 0.76 [0.39, 1.46] | 1.49 [0.87, 2.54] |
| Quitter Class | 2 | 1.07 [0.41, 2.82] | 2.73 [0.58, 12.73] | 1.77 [0.59, 5.27] | 2.29 [0.85, 6.18] |
| 3 | 0.71 [0.49, 1.04] | 1.02 [0.69, 1.53] | 0.58 [0.35, 0.98]* | 1.25 [0.86, 1.82] | |
| Pooled | 1.00 [0.86, 1.16] | 1.45 [1.17, 1.81]* | 1.02 [0.85, 1.23] | 1.47 [1.26, 1.70]* | |
| Comparison to Cessation | 1 | 2.54 [0.49, 13.05] | 2.13 [0.68, 6.65] | 1.65 [0.49, 5.57] | |
| Failure Class | 2 | 0.47 [0.15, 1.47] | 1.19 [0.23, 6.25] | 0.77 [0.22, 2.75] | |
| 3 | 0.57 [0.37, 0.88]* | 0.82 [0.52, 1.29] | 0.47 [0.26, 0.83]* | ||
| Pooled | 0.68 [0.58, 0.81]* | 0.99 [0.79, 1.25] | 0.70 [0.57, 0.85]* | ||
| Comparison to Relapse | 1 | 1.38 [0.66, 2.88] | 5.15 [2.23, 11.89]* | ||
| Class | 2 | 0.61 [0.18, 2.06] | 1.54 [0.27, 8.74] | ||
| 3 | 1.22 [0.69, 2.16] | 1.76 [0.97, 3.18] | |||
| Pooled | 0.98 [0.80, 1.19] | 1.42 [1.10, 1.84]* | |||
| Comparison to Late | 1 | 0.27 [0.12, 0.58]* | |||
| Intermittent Smoker Class | 2 | 0.39 [0.08, 2.02] | |||
| 3 | 0.70 [0.44, 1.10] | ||||
| Pooled | 0.69 [0.55, 0.87]* | ||||
| Panel E. Number of past quit attempts | |||||
| Study | Early Intermittent | Late Intermittent | Relapse | Cessation Failure | |
| Comparison to Early | 1 | 0.51 [0.18, 1.43] | 0.74 [0.30, 1.82] | 2.23 [1.04, 4.78]* | 1.00 [0.46, 2.16] |
| Quitter Class | 2 | 1.20 [0.82, 1.74] | 0.74 [0.35, 1.53] | 0.96 [0.59, 1.56] | 0.55 [0.30, 0.99]* |
| 3 | Did not converge | Did not converge | Did not converge | Did not converge | |
| Pooled | 1.06 [0.93, 1.20] | 1.08 [0.93, 1.26] | 1.10 [0.96, 1.26] | 0.64 [0.48, 0.84]* | |
| Comparison to Cessation | 1 | 0.62 [0.29, 1.30] | 0.46 [0.24, 0.85]* | 0.80 [0.48, 1.35] | |
| Failure Class | 2 | 2.19 [1.18, 4.09]* | 1.35 [0.55, 3.29] | 1.76 [0.88, 3.53] | |
| 3 | Did not converge | Did not converge | Did not converge | ||
| Pooled | 1.66 [1.24, 2.20]* | 1.70 [1.26, 2.29]* | 1.72 [1.28, 2.31]* | ||
| Comparison to Relapse | 1 | 0.23 [0.07, 0.71]* | 0.33 [0.12, 0.92]* | ||
| Class | 2 | 1.25 [0.74, 2.09] | 0.77 [0.34, 1.74] | ||
| 3 | Did not converge | Did not converge | |||
| Pooled | 0.96 [0.83, 1.11] | 0.99 [0.83, 1.17] | |||
| Comparison to Late | 1 | 0.69 [0.21, 2.28] | |||
| Intermittent Smoker Class | 2 | 1.62 [0.77, 3.43] | |||
| 3 | Did not converge | ||||
| Pooled | 0.98 [0.83, 1.15] | ||||
| Panel F. Baseline EMA craving | |||||
| Study | Early Intermittent | Late Intermittent | Relapse | Cessation Failure | |
| Comparison to Early | 1 | 0.72 [0.50, 1.01] | 0.77 [0.55, 1.10] | 1.15 [0.78, 1.69] | 0.89 [0.65, 1.20] |
| Quitter Class | 2 | 0.82 [0.55, 1.21] | 1.58 [0.82, 3.06] | 0.85 [0.55, 1.32] | 1.10 [0.73, 1.65] |
| 3 | 1.95 [1.53, 2.49]* | 2.32 [1.79, 3.00]* | 1.90 [1.37, 2.64]* | 2.31 [1.81, 2.96]* | |
| Pooled | 1.18 [1.02, 1.36]* | 1.45 [1.18, 1.79]* | 1.18 [0.99, 1.41] | 1.52 [1.31, 1.76]* | |
| Comparison to Cessation | 1 | 1.93 [0.96, 3.89] | 1.34 [0.84, 2.14] | 1.04 [0.63, 1.70] | |
| Failure Class | 2 | 0.74 [0.47, 1.18] | 1.44 [0.71, 2.91] | 0.77 [0.46, 1.29] | |
| 3 | 0.84 [0.64, 1.12] | 1.00 [0.75, 1.34] | 0.82 [0.57, 1.18] | ||
| Pooled | 0.78 [0.66, 0.91]* | 0.96 [0.77, 1.20] | 0.78 [0.64, 0.95]* | ||
| Comparison to Relapse | 1 | 0.62 [0.40, 0.98]* | 0.68 [0.43, 1.07] | ||
| Class | 2 | 0.96 [0.59, 1.58] | 1.86 [0.89, 3.88] | ||
| 3 | 1.03 [0.72, 1.47] | 1.22 [0.84, 1.77] | |||
| Pooled | 1.00 [0.82, 1.21] | 1.23 [0.96, 1.59] | |||
| Comparison to Late | 1 | 0.92 [0.61, 1.39] | |||
| Intermittent Smoker Class | 2 | 0.52 [0.26, 1.04] | |||
| 3 | 0.84 [0.63, 1.13] | ||||
| Pooled | 0.81 [0.65, 1.01] | ||||
p < 0.05
In Study 3, relative to the placebo no counseling condition, active bupropion reduced the odds of early smoking (as shown by lower odds of Cessation Failure and Intermittent Smoking versus Early Quitting), and increased odds of Relapse versus Cessation Failure. These effects generally held with or without counseling, although the effect on Early Intermittent Smoking versus Cessation Failure was only significant with counseling, and the effect on Early Intermittent Smoking versus Early Quitting was only significant in the absence of counseling. Bupropion SR also promoted recovery from early smoking (Late Intermittent Smoking versus Cessation Failure), but this was only significant in the absence of counseling. No treatment differentiated Early and Late Intermittent Smokers (Table 4D). Counseling alone had no significant effects.
3.4 Conditional Models (with Covariates)
Covariates that significantly correlate with the likelihood of class-membership in a multivariate multinomial logistic regression model are indicated in Table 5. For each covariate in the final model, a panel of Table 5 depicts the odds ratio of membership in a particular class, relative to a specified reference class. Results for each study and the pooled analyses are shown by row. Covariates that were not significantly related to latent class in any study (pre-quit self-efficacy, affect, sleep disturbance, and depressive symptoms) were dropped from the final models and are not shown.
3.4.1 Gender
Estimated odds ratios (Table 5A.) were significantly above one in the contrast of all early smoking classes (Cessation Failures and both Early and Late Intermittent Smokers) vs. Early Quitters in all but Study 1, indicating that women were more likely than men to continue smoking at the outset of the quit attempt in studies 2, 3, and the pooled analyses. Women were significantly more likely to Relapse than to be Early Quitters only in the pooled analyses, perhaps due to the small numbers of Relapsers in individual studies. In Study 1 only, women were significantly more likely than men to engage in Early Intermittent Smoking rather than daily smoking (Cessation Failure). In Study 2 only, women were more likely than men to be Late Intermittent Smokers relative to all other classes.
3.4.2 Minority Status
Relations between minority status and latent class (Table 5B) suggested greater risk of membership in a smoking class than the Early Quitter class in all but Study 1. In Study 2, members of minority racial/ethnic groups were twice as likely to be Cessation Failures and four times as likely to be Late Intermittent Smokers than Early Quitters, relative to White participants. In Study 3 and the pooled analyses, minority participants were more likely than White participants to be Early Intermittent Smokers than Early Quitters. Minority status was related to greater odds of recovery (Late Intermittent Smoking) versus Relapse than Early Intermittent Smoking only in better powered, pooled analyses.
3.4.3 Baseline Cigarettes per Day
The direction of relations between smoking heaviness and latent abstinence class was largely consistent across studies (Table 5C), despite differences in the magnitude and statistical significance of these effects. Greater smoking heaviness was associated with increased odds of being in higher risk classes rather than the Early Quitting class; in Study 1 and the pooled analyses, greater smoking heaviness was associated with increased odds of Cessation Failure; in Study 2 and the pooled analyses, heavier smoking predicted increased odds of Relapse and Early Intermittent Smoking. These effects were more modest in Study 3 and did not reach significance.
3.4.4 Baseline FTND
Scores on the FTND (Table 5D) were associated with increased risk of initial difficulty quitting in some studies (Late Intermittent Smoking in Study 1 and pooled analyses and Cessation Failure in pooled analyses). Study 3 suggested an unexpected associated between greater dependence and reduced risk of Relapse following cessation (Early Quitting), but this did not replicate across studies. In Study 3 and the pooled analyses, greater dependence was associated with reduced odds of early, partial change in smoking (Early Intermittent Smoking or Relapse) relative to Cessation Failure. More dependent individuals were more likely to be Late Intermittent Smokers vs. Relapsers in Study 1 and the pooled analyses (with similar but non-significant odds ratios in Studies 2 and 3), which may reflect a relation between dependence and difficulty achieving initial abstinence. Greater dependence was associated with lower odds of recovering toward abstinence over days, versus Early Intermittent Smoking across studies; this was significant in Studies 1 and pooled analyses.
3.4.5 Number of Past Quit Attempts
Quitting history was associated with latent class (Table 5E) such that more past quitting was associated with reduced risk of Cessation Failure (in Study 2 and the pooled analyses). Past quitting (which by definition involved past relapsing in the smokers enrolled in this trial) was associated with increased odds of Relapse (vs. Early Quitting in Study 1, vs. Cessation Failure in pooled analyses, and vs. Intermittent Smoking in Study 1). Results generally suggest an association between past quit attempts and a pattern of Relapse in this quit attempt. Study 3 models including number of past quit attempts did not converge.
3.4.6 Baseline EMA Craving
Relations between baseline EMA measures of craving (which varied across studies in terms of items and scaling) and latent class (Table 5F) were highly variable across studies. Although baseline craving was significantly associated with greater odds of membership in a smoking class vs. Early Quitting in Study 3 and pooled analyses, this was not true in Studies 1 and 2. Greater craving was associated with reduced odds of early, partial change (Early Intermittent Smoking or Relapse) versus Cessation Failure in pooled analyses (reflecting similar but non-significant results in Studies 2 and 3). Baseline craving was greater risk of Relapse (versus Early Intermittent Smoking) in Study 1 only.
4. DISCUSSION
The current results replicate a previous RMLCA of smoking status in the first 27 days of a quit attempt (McCarthy et al., 2015) and extend knowledge regarding treatment effects on latent abstinence patterns early in the quitting process. Results of three independent studies converged on a five-class solution: early and stable abstinence, stable reduction, early success followed by relapse, early struggle followed by improvement, or failure to change. Early stable abstinence and reduction are associated with better three-month outcomes. High-dose nicotine patch and bupropion SR appear to promote early abstinence. High-dose patch also appears to promote intermittent smoking, particularly early intermittent smoking, rather than daily smoking. Bupropion SR effects on intermediate classes were dependent on counseling.
4.1 Latent Class Structure
In every study, the largest class (39–45% of smokers) was marked by stable abstinence (Early Quitter), despite the varying sample characteristics and treatments across studies. In all three studies, a smaller group (Cessation Failure, 17–24%) failed to quit, as shown by low abstinence probabilities through 27 days post-quit. The remaining three latent classes had intermediate abstinence probabilities. Early Intermittent Smokers (14–22%) maintained 0.60–0.90 abstinence probabilities across days. Those in a Relapse class (8–13%) established initial abstinence but then returned to consistent smoking. Late Intermittent Smokers (7–11%) showed the opposite pattern, with low or unstable abstinence probabilities initially that increased over weeks. These results are highly concordant with the latent class structure that emerged in an RMLCA of a large trial (McCarthy et al., 2015) and the consistency of the classes across studies is striking.
4.2 Distal Outcomes
Three-month abstinence rates were highest in the Early Quitter latent class, as in McCarthy et al, 2015. In contrast to that study, the only other class with substantial abstinence rates at three months in the present study was the Early Intermittent Smoker class. McCarthy and colleagues (2015) found Late Intermittent Smokers achieved an impressive 23% abstinence rate six months post-quit, whereas Early Intermittent Smokers had only a 10% abstinence rate. Thus, in the current analyses, recovery from initial struggles among Late Intermittent Smokers did not predict later abstinence as in the prior study (McCarthy et al., 2015). Nonetheless, the present results suggest that establishing and maintaining high probabilities of abstinence in the first weeks of a quit attempt marks one for later success.
4.3 Treatment
In Study 2, active high-dose patch with counseling promoted early change (Early Quitting and Early Intermittent Smoking) and prevented Cessation Failure, as hypothesized. High-dose patch also beat our expectations by preventing Relapse relative to those with high initial abstinence probabilities (Early Quitters and Early Intermittent Smokers) and fostering recovery from initial smoking better than did placebo patch. Patch treatment did not differentiate Late Intermittent Smokers from those achieving earlier partial change (Early Intermittent Smoking or Relapse). The lack of effects in comparisons of these smaller, intermediate classes may reflect lower power or may indicate that patch therapy works roughly equally well among these latent classes, despite their different patterns of abstinence.
In Study 3, bupropion SR also appeared to promote early abstinence (Early Quitting or Relapse) rather than initial smoking (Cessation Failure or Late Intermittent Smoking). This benefit of bupropion SR was not dependent on counseling. Bupropion SR effects on intermediate classes were dependent on counseling, however. Bupropion SR with counseling significantly increased the odds of early intermittent smoking (partial change) rather than cessation failure, whereas bupropion alone had a more modest and non-significant benefit. Although active medication was associated with increased odds of recovery from initial smoking (versus continued daily smoking) when offered alone, this effect was not augmented by counseling. As such, the hypothesis that bupropion SR would enhance recovery from initial smoking received only partial support and the hypothesis that counseling would foster recovery for early smoking was not supported. Inconsistencies in medication effects across counseling conditions may reflect low power for comparisons among relatively small classes. The direction of medication effects was consistent across counseling conditions, but differed in magnitude and significance. The failure to detect any benefits of counseling with placebo medication is consistent with earlier logistic regression and survival analyses showing no significant benefit of counseling in this trial (McCarthy et al., 2008a).
4.4 Covariates
The final conditional models contained only those covariates that remained significantly related to latent class membership in at least one study.
4.4.1 Gender
In the larger studies (Studies 2 and 3 and the pooled analyses), women were at greater risk of continued smoking after the target quit day than were men. These data are consistent with prior trials of treatments similar to those tested here that suggested women have more difficulty quitting than do men (Fortmann and Killen, 1994; Perkins and Scott, 2008; Scharf and Shiffman, 2004), but not our earlier RMLCA of early smoking in a 6-arm RCT (McCarthy et al., 2015). These effects were weaker and not significant in the smaller group CBT study in which women were more likely than men to show a significant and stable reduction in smoking days, rather than cessation failure. In the high-dose nicotine patch trial, women were three to four times more likely than men to recover over time rather than continue or return to daily smoking, despite suggestions that nicotine replacement is ineffective in women (Perkins, 2001). This did not occur in the group CBT or bupropion SR and counseling trials. Given the differences among studies, it is difficult to determine the reasons for these inconsistencies. Studies at the population level have found age-specific gender differences, such that women are more likely to quit than are men before age 50 or 60, before the pattern reverses in late life, washing out gender differences in analyses collapsed over age (Jarvis et al., 2013). A larger proportion of participants were over age 50 in Study 1 and the McCarthy et al., 2015 study than in Studies 2 and 3 that showed significant gender differences, however. As such, it is not clear why gender was related to smoking class in only some samples or circumstances.
4.4.2 Minority Status
Epidemiological data suggest that smoking cessation rates are lower among African-American smokers, despite greater interest in quitting and more quit attempts (Malarcher et al., 2011). The current analyses detected greater odds of early smoking in the high-dose nicotine patch RCT, and evidence of lower odds of quitting completely (vs. reducing smoking frequency) in the bupropion SR and counseling RCT among minority (mostly African American) versus non-minority smokers. Similar results were found in our previous RMLCA (McCarthy et al., 2015). When the samples were pooled, there was evidence of greater odds of recovery versus relapse. This effect was in the same direction across all three studies, but only significant when pooled. These data are consistent with both greater difficulty quitting initially and greater motivation to continue trying to quit despite these initial difficulties among minority smokers. The reasons for the inconsistencies across studies are not clear. Research with enriched sampling of specific racial or ethnic subpopulations is needed to resolve these discrepancies across studies.
4.4.3 Nicotine Dependence
Results indicated that cigarettes per day, FTND scores, and the number of past quit attempts were significantly related to less favorable latent smoking classes. The patterns of covariate relations with class contrasts varied across studies, but generally supported a relation between greater dependence and greater risk of smoking. Heavier smokers were less likely to be Early Quitters than in a smoking class in two of the three studies. In pooled analyses, higher scores on the FTND were also related to lower odds of sustained abstinence and greater odds of both cessation failure and relapse, as in our previous RMLCA (McCarthy et al., 2015). Although these effects were not significant in the high-dose patch study, they were generally in the same direction. There was an unexpected association between higher FTND scores and lower risk of relapse among early quitters in the bupropion SR and counseling trial, but not in the other studies, including the 6-arm RCT (McCarthy et al., 2015). More past quit attempts were associated with reduced risk of Cessation Failure in the group-CBT and high-dose patch studies, as in the 6-arm RCT (McCarthy et al., 2015). In addition, more past quitting was associated with greater risk of Relapse, an effect not observed in the previous RMLCA (McCarthy et al., 2015). These data suggest that more experience quitting is helpful in initiating cessation, but that a history of multiple past relapses are associated with greater relapse risk in an index attempt, although the extent of this association may vary by sample, treatment, or situation
4.4.4 Baseline Craving
Baseline craving was associated with lower odds of sustained abstinence in only the bupropion SR and counseling RCT, although greater pre-quit craving was also associated with greater relapse risk relative to sustained intermittent smoking in the group CBT study. Craving was not significantly related to latent class in our earlier RMLCA (McCarthy et al., 2015), in which baseline self-efficacy and sleep were more robustly related to class. The items and scales used to assess craving differed across studies, which may contribute to the varying results. The lack of robustness in these relations across studies suggests they have limited potential to serve as markers of early smoking patterns.
4.5 Limitations
Both a limitation and a strength of the current study is the diversity of the studies included. The datasets were collected using different screening criteria, research designs, and assessment batteries by two investigative teams. As such, study is likely a potent source of variance reflecting the influence of many factors. Despite this, the latent class structure was replicated across studies, although many specific covariate relations with latent classes did not. The relatively small size of the samples in the individual studies may have limited power and contributed to inconsistencies in the pattern of covariate relations across studies. Also, results may not replicate among self-quitters, as all participants in the current studies were screened for high levels of motivation and volunteered for relatively demanding intervention studies. Complementary Markov modeling approaches that provide more specific information about particular transition probabilities (i.e., relapse), such as that developed by Killeen (2011) will enhance our understanding of treatment and covariate effects on smoking cessation outcome.
4.6 Conclusions
Five common patterns of daily smoking at the outset of a smoking cessation attempt have been identified in four independent samples of adult smokers in smoking cessation studies. Tobacco dependence and smoking history are associated with these patterns, and smoking cessation therapies, particularly pharmacotherapies, influence smoking patterns in the early phases of quitting. Early patterns of smoking in the first weeks of a quit attempt presage later abstinence outcomes.
Highlights.
Replicated 5 latent classes of daily smoking patterns during a stop smoking attempt
First-month latent smoking classes differ in 3-month point-prevalence abstinence
High-dose nicotine patch protects against promotes early, sustained abstinence
Bupropion SR protects against early smoking and relapse
Nicotine dependence is a risk factor for membership in less abstinent classes
Acknowledgments
Conflict of Interest
GlaxoSmithKline donated active and placebo medication for the randomized clinical trial of bupropion SR and counseling and the high-dose patch study re-analyzed in the present paper. Dr. McCarthy has received discounts on nicotine lozenge purchases from GlaxoSmithKline in the past. GlaxoSmithKline played no role in the design, implementation, analysis, or reporting of the studies. Dr. Shiffman has consulted to GlaxoSmithKline on smoking and smoking cessation, and currently consults with Niconovum on smoking cessation and Reynolds American Incorporated on tobacco harm minimization. No one from GlaxoSmithKline, Niconovum, or Reynolds American Incorporated were involved in any way in the conceptualization, implementation, analysis, or reporting for this project.
Role of Funding Source
This work was supported by National Institute on Drug Abuse Grant R01DA033303 awarded to Drs. McCarthy and Shiffman. The data for this study were collected as part of previously reported studies and clinical trials (Shiffman et al., 1996 supported by grant R01DA6084 from the National Institute on Drug Abuse; Shiffman et al., 1997 supported by grant R01DA6084 from the National Institute on Drug Abuse; McCarthy et al., 2008 supported by grants P50CA084724 from the National Cancer Institute and P50DA19706 from the National Institute on Drug Abuse). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Drug Abuse, the National Cancer Institute, or the National Institutes of Health.
We wish to thank Timothy B. Baker, Michael C. Fiore, and the staff at the Center for Tobacco Research and Intervention in the Department of Medicine at the University of Wisconsin School of Medicine and Public Health for sharing data for this project.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributors
D. E. McCarthy contributed to the conceptualization of the project, prepared data for analysis, and drafted the manuscript. L. Ebssa conducted data analyses, prepared tables and figures, and assisted in the writing of the manuscript. K. Witkiewitz contributed to the conceptualization of the project, provided expert guidance regarding data analysis, and assisted in writing the manuscript. S. Shiffman contributed to the conceptualization of the project, contributed two datasets for analysis, guided data analytic choices, and contributed to the writing of the manuscript. All authors have approved the final manuscript.
Contributor Information
Danielle E. McCarthy, Email: demccart@rci.rutgers.edu.
Lemma Ebssa, Email: lemma@rci.rutgers.edu.
Katie Witkiewitz, Email: katiew@unm.edu.
Saul Shiffman, Email: shiffman@pinneyassociates.com.
REFERENCES
- Brandon TH, Vidrine JI, Litvin EB. Relapse and relapse prevention. Ann. Rev. Clin. Psychol. 2007;3:257–284. doi: 10.1146/annurev.clinpsy.3.022806.091455. [DOI] [PubMed] [Google Scholar]
- Fiore MC, Jaén CR, Baker TB, Bailey WC, Benowitz NL, Curry SJ, Wewers ME. Clinical Practice Guideline. Rockville, MD: U.S. Department of Health and Human Services, Public Health Service; 2008. Treating Tobacco Use and Dependence: 2008 Update. [Google Scholar]
- Fortmann SP, Killen JD. Who shall quit? Comparison of volunteer and population-based recruitment in two minimal contact smoking cessation studies. Am. J. Epidemiol. 1994;140:39–51. doi: 10.1093/oxfordjournals.aje.a117157. [DOI] [PubMed] [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker RC, Fagerstrom KO. The Fagerstrom Test for Nicotine Dependence: a revision of the Fagerstrom Tolerance Questionnaire. Br. J. Addiction. 1991;86:1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- Hughes JR, Keely J, Niaura R, Ossip-Klein D, Richmond R, Swan G. Measures of abstinence from tobacco in clinical trials: issues and recommendations. Nicotine Tob. Res. 2003;5:13–25. [PubMed] [Google Scholar]
- Jarvis MJ, Cohen JE, Delnevo CD, Giovino GA. Dispelling myths about gender differences in smoking cessation: population data from the USA, Canada, and Britain. Tob. Control. 2013;22:356–360. doi: 10.1136/tobaccocontrol-2011-050279. [DOI] [PubMed] [Google Scholar]
- Killeen PR. Markov model of smoking cessation. PNAS. 2011;108:S3. doi: 10.1073/pnas.1011277108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malarcher A, Dube S, Shaw L, Babb, Kaufmann R. Quitting smoking among adults—United States, 2001–2010. MMWR. 2011;60:1513–1519. [PubMed] [Google Scholar]
- McCarthy DE, Ebssa L, Witkiewitz K, Shiffman S. Paths to tobacco abstinence: a repeated measures latent class analysis. J. Consult. Clin. Psychol. 2015;83:696–708. doi: 10.1037/ccp0000017. doi: http:dx.doi.org/10.1037/jccp0000017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCarthy DE, Piasecki TM, Fiore MC, Baker TB. Life before and after quitting smoking: an electronic diary study. J. Abnorm. Psychol. 2006;115:454–466. doi: 10.1037/0021-843X.115.3.454. [DOI] [PubMed] [Google Scholar]
- McCarthy DE, Piasecki TM, Lawrence DL, Jorenby DE, Shiffman S, Fiore MC, Baker TB. A randomized, controlled clinical trial of bupropion SR and individual smoking cessation counseling. Nic. Tobac. Res. 2008a;10:717–729. doi: 10.1080/14622200801968343. [DOI] [PubMed] [Google Scholar]
- McCarthy DE, Piasecki TM, Lawrence DL, Jorenby DE, Shiffman S, Baker TB. Psychological mediators of bupropion SR treatment for smoking cessation. Addiction. 2008b;103:1521–1533. doi: 10.1111/j.1360-0443.2008.02275.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLachlan GJ, Peel D. Finite Mixture Models. New York: John Wiley; 2000. [Google Scholar]
- Nylund KL, Asparouhov T, Muthen BO. Deciding On The Number Of Classes In Latent Class Analysis And Growth Mixture Modeling: A Monte Carlo Simulation Study. 2006 Retrieved from http://www.statmodel.com/recpapers.shtml. [Google Scholar]
- Perkins KA. Smoking cessation in women: apecial considerations. CNS Drugs. 2001;15:391–411. doi: 10.2165/00023210-200115050-00005. [DOI] [PubMed] [Google Scholar]
- Perkins KA, Scott J. Sex differences in long-term smoking cessation rates due to nicotine patch. Nicotine Tob. Res. 2008;10:1245–1250. doi: 10.1080/14622200802097506. [DOI] [PubMed] [Google Scholar]
- Piper ME, Smith SS, Schlam TR, Fiore MC, Jorenby DE, Fraser D, Baker TB. A randomized placebo-controlled clinical trial of five smoking cessation pharmacotherapies. Arch. Gen. Psychiatry. 2009;66:1253–1262. doi: 10.1001/archgenpsychiatry.2009.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl. Psychol. Measure. 1977;1:385–401. [Google Scholar]
- Rose JE, Behm FM. Combination treatment with varenicline and bupropion in an adaptive smoking cessation paradigm. Am. J. Psychiatry. 2014;171:1199–1205. doi: 10.1176/appi.ajp.2014.13050595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scharf D, Shiffman S. Are there gender differences in smoking cessation, with and without bupropion? Pooled- and meta-analyses of clinical trials of bupropion SR. Addiction. 2004;99:1462–1469. doi: 10.1111/j.1360-0443.2004.00845.x. [DOI] [PubMed] [Google Scholar]
- Schwarz, Gideon E. Estimating the dimension of a model. Annal. Stats. 1978;6:461–464. [Google Scholar]
- Sclove LS. Application of model-selection criteria to some problems in multivariate analysis. Psychometrika. 1987;52:333–343. [Google Scholar]
- Shiffman S. Conceptual issues in the study of relapse. In: Gossop M, editor. Relapse and Addictive Behavior. New York: Routledge; 1989. pp. 149–179. [Google Scholar]
- Shiffman S, Engberg JB, Paty JA, Perz WG, Gnys M, Kassel JD, Hickcox M. A day at a time: predicting smoking lapse from daily urge. J. Abnorm. Psychol. 1997;106:104–116. doi: 10.1037//0021-843x.106.1.104. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Paty JA, Gnys M, Kassel JA, Hickcox M. First lapses to smoking: within subjects analysis of real time reports. J. Consult. Clin. Psychol. 1996;64:366–379. doi: 10.1037//0022-006x.64.2.366. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Scharf D, Shadel W, Gwaltney C, Dang Q, Paton S, Clark D. Analyzing milestones in smoking cessation: an illustration from a randomized trial of high-dose nicotine patch. J. Consult. Clin. Psychol. 2006;74:276–285. doi: 10.1037/0022-006X.74.2.276. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Waters AJ, Hickcox M. The Nicotine Dependence Syndrome Scale: a multidimensional measure of nicotine dependence. Nicotine Tob. Res. 2004;6:327–348. doi: 10.1080/1462220042000202481. [DOI] [PubMed] [Google Scholar]
- Spielberger CD, Gorsuch RL, Lushene R, Vagg PR, Jacobs GA. Manual for the State-Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologists Press; 1983. [Google Scholar]
- Spielberger CD, Jacobs G, Russell S, Crane RS. Assessment of anger: the state-trait anger scale. In: Butcher JN, Spielberger CD, editors. Advances in Personality Assessemnt. Vol. 2. New York: Routledge; 1986. pp. 161–190. [Google Scholar]
- Stone AA, Shiffman S. Ecological momentary assessment (EMA) in behavioral medicine. Ann. Behav. Med. 1994;16:199–202. [Google Scholar]
- Witkiewitz K, Hartzler B, Donovan DM. Matching Motivation Enhancement Treatment to client motivation: re-examining the Project MATCH motivation matching hypothesis. Addiction. 2010;105:1403–1413. doi: 10.1111/j.1360-0443.2010.02954.x. [DOI] [PMC free article] [PubMed] [Google Scholar]