Abstract
Objective
Pharmacotherapy for epilepsy is limited with 30% of patients refractory to this approach of suppressing seizures. Current surgical options are invasive and carry significant morbidities including infection, bleeding, and the potential for deleterious neurocognitive effects. As a result, there is a burgeoning need for innovation to develop safer and efficacious interventions.
Methods
Four distinct catheters (2 existing: Cardima catheter, Standard EPT Blazer catheter; 2 new prototypes: balloon catheter, basket catheters) were tested in 12 baboons (21–30 kg, 100% male). For each, we assessed whether or not the catheter was able to be maneuvered safely in various locations of the cerebral venous system, provide adequate cortical tissue contact to record signals, detect these signals as normal or abnormal, successfully stimulate the cortex, and capture the cortical tissue. Locations trialed included the petrosal sinus, straight sinus, vein of Galen, and occipital vein. Pacing cycle length and pacing thresholds varied among experiments.
Results
Successful mapping was conducted in all 12 baboons. The pacing cycle length varied from 75 ms to 650 ms depending on location of the cortex. Pacing threshold was recorded in 4/12 (33%) of the experiments; data is not available for the remaining 8/12 experiments. The threshold values ranged from 0.3 – 20 mAmps. Capture of cortical electrical activity was observed in 11/12 (91.7 %) experiments though the number of successful capture and stimulation attempts varied among experiments. The most reliable and consistent capture occurred with the use of our novel prototyped over-the-wire balloon catheter (9/12; 75%) and basket catheter (3/3; 100%). Necropsy and histology were performed post-experimentation, and only minimal complications were noted (Table 1).
Conclusion
New electrode design can be maneuvered safely in the venous system, provide adequate cortical tissue contact to record signals, detect these signals as normal or abnormal, successfully stimulate the cortex, and capture cortical tissue. These novel devices merit further study in chronic baboons to establish long-term efficacy of continuous seizure recording.
Keywords: Epilepsy, venous pacing, primates, cerebral cortex
Introduction
Epilepsy is a serious network disorder with variable presentation and subpar therapy.9 Currently, 30% of epilepsy patients remain refractory to medical therapy, especially those with mesial temporal lobe epilepsy.5 Invasive techniques, including open resection, have been attempted; however, these can lead to unwanted side effects such as decline in neurocognitive function.5 More recent neurostimulation techniques, including anterior thalamic deep brain stimulation and responsive neurostimulation at seizure foci, have been equivocal in their efficacy - mitigating seizure frequency by 40% immediately after surgery and in 50–69% of patients after several years.4 Apart from inconsistency, these stimulatory techniques lead to many complications, most of which are related to the implantation procedure and hardware, that is, electrode mistargeting, movementm and implantation site infection.4 A combination of these factors has favored movement towards less invasive, non-surgical techniques for the treatment of epilepsy.
Vagal nerve stimulation has been used as a treatment of refractory epilepsy and has led to fewer procedural complications given minimally invasive placement in the neck as opposed to brain but has limited benefit for patients with bilateral interictal epileptiform activity and cortical malformations and may be be subpar to anterior thalamic deep brain stimulation and responsive neurostimulation.2,4 Previously, we have demonstrated successful navigation, mapping, and radiofrequency ablation of the cerebral cortex in porcine, canine, and baboon models through the venous sinuses and cerebral veins.6,7 Here we explore the intra-venous manipulation of novel pacing electrodes. We hope to understand whether these electrodes can provide a safer means to detect cortical signals, determine whether they are normal or abnormal, stimulate the cortex, and capture the cortical tissue since doing so would have significant implications for future epilepsy therapy.
Methods
Animal Preparation
This study was approved by the Mayo Clinic Institutional Animal Care and Use Committee (IACUC). Twelve baboons (21–30 kg, 100% male) were tested under general anesthesia consisting of 1–3% of isoflurane and sodium pentothal. Intravenous heparin was injected periodically to maintain a therapeutic activated clotting time of 250 seconds.
Venous Access and Electrical Mapping
In order to access the animal venous vasculature prior to pacing, a multipurpose 4-French catheter was inserted into either the internal jugular vein or femoral vein. Venograms were obtained at various locations, including the petrosal sinus, straight sinus, vein of Galen, and occipital vein (Table 1). For mapping and subsequent ablation, additional catheters were inserted into the internal carotid artery as described previously.6 Seizures were induced by either electrical stimulation/pacing or injection of penicillin in venous vessels as described previously.6 Mapping of electrical activity was performed at high (200 Hz) and low (50–200 Hz) frequencies.6
Table 1.
Summary of Results. Types of catheters, location of pacing, catheter type used, number of unique sites paced, cycle length, threshold, and whether or not capture was achieved at the respective sites.
| Experiment | Animal Type | Catheter used to obtain venograms | Location of venous stimulation and/or cortical structure stimulated | Catheter used for Pacing | Pacing cycle length (ms) | Threshold (ma) | Capture Obtained? | Complications |
|---|---|---|---|---|---|---|---|---|
| 1 | Baboon | 6-French multipurpose catheter | Petrosal Sinus, Vein of Galen | Cardima 2.7-French decapolar catheter; 6-French 4 mm tipped EPT catheter; our prototyped over-the-wire balloon catheter | 80–600 | – | Yes | No |
| 2 | Baboon | 6-French 4-mm tipped EPT catheter | the occipital lobe, right mesial temporal lobe, petrosal sinus and the vein of Labbe | Cardima 2.7-French decapolar catheter; 6-French 4 mm tipped EPT catheter; our prototyped over-the-wire balloon catheter | 75–300 | – | No | No |
| 3 | Baboon | Cardima 2.7-French decapolar catheter; 6-French 4 mm tipped EPT catheter | petrosal sinus | Cardima 2.7-French decapolar catheter; our prototyped over-the-wire balloon catheter | 500–650 | 11 | Yes (with our prototyped over-the-wire balloon catheter only) | No |
| 4 | Baboon | 6-French 4-mm tipped EPT catheter; our prototyped over-the-wire balloon catheter | Vein of Galen, mid brain, occipital lobe (2 sites) | 6-French 4-mm tipped EPT catheter; our prototyped over-the-wire balloon catheter | 75 | 0.3 – 20 | Yes (with our prototyped over-the-wire balloon catheter only) | Yes (coagulum formation, electrode breakage) |
| 5 | Baboon | our prototyped over-the-wire balloon catheter | Occipital lobe (4 sites), temporal lobe, sagittal sinus | our prototyped over-the-wire balloon catheter | 75 | 0.7 | Yes | No |
| 6 | Baboon | 6-French 4-mm tipped EPT catheter; our prototyped over-the-wire balloon catheter; Basket catheter | Base of brain, petrosal sinus, straight sinus; subdural sinus, temporal lobe (for basket catheter) | 6-French 4-mm tipped EPT catheter; our prototyped over-the-wire balloon catheter; Basket catheter | 75 | – | Yes | No |
| 7 | Baboon | prototyped over-the-wire balloon catheter; Basket catheter | Petrosal sinus, straight sinus; artery (for basket catheter) | prototyped over-the-wire balloon catheter; Basket catheter | 75 | 10 | Yes | Yes (small venous dissection) |
| 8 | Baboon | prototyped over-the-wire balloon catheter; Basket catheter | Occipital lobe, basilar vein (basket catheter) | prototyped over-the-wire balloon catheter | 75 | – | Yes | Yes (breakage of balloon catheter) |
| 9 | Baboon | prototyped over-the-wire balloon catheter | Occipital lobe, straight sinus, straight sinus, temporal fissure | prototyped over-the-wire balloon catheter | 75 | – | Yes | No |
| 10 | Baboon | prototyped over-the-wire balloon catheter | Straight sinus, occipital lobe; sigmoid sinus | prototyped over-the-wire balloon catheter | 75 | – | Yes | No |
| 11 | Baboon | Cardima 2.7-French decapolar catheter; prototyped over-the-wire balloon catheter | Left vein base | Cardima 2.7-French decapolar catheter; prototyped over-the-wire balloon catheter | 75 | – | Yes (with Cardima 2.7-French decapolar catheter only) | No |
| 12 | Baboon | Cardima 2.7-French decapolar catheter; 6-French 4 mm tipped EPT catheter | Occipital lobe, parietal lobe | prototyped over-the-wire balloon catheter; basket catheter | 75 | – | Yes (with basket catheter only) | No |
Pacing
Pacing was conducted using two existing catheters (2.7-Fr octapolar microelectrode catheter [Revelation Cardima™, Fremont CA] & 6-Fr 4-mm tip, deflectable EPT catheter [Blazer Boston Scientific™, Natick, MA]), and two novel minimally invasive pacing catheters (over-the-wire balloon [Figure 1] & basket [Figure 2] catheters). The over-the-wire balloon catheter is lined with polytetrafluoroethylene (PTFE), braided with stainless steel allowing it to be safely manuveured intravascularly, and contains a Pebax outer jacket and consists of six electrodes. There are two rows of electrodes consisting of three electrodes each. Each row of electrodes is 5 mm apart from the other and each electrode is 2 mm apart from the next within the same row allowing for pacing from several different locations without altering catheter position. A detailed schematic of the over-the-wire balloon catheter is shown in Figure 1.6 In contrast, the novel basket catheter, composed of Nitinol, consists of eight 1 mm long, 90% Platinum/10% Iridium electrodes. The electrodes are insulated from Nitinol with Polyimide and are spaced 1.9 mm along the axis and 1.875 mm radially, and the device is designed such that it remains securely in place intravascularly to allow continuous pacing if required. A detailed schematic is shown in Figure 2.
Figure 1. Over-the-wire Balloon Catheter for venous pacing in the CNS.
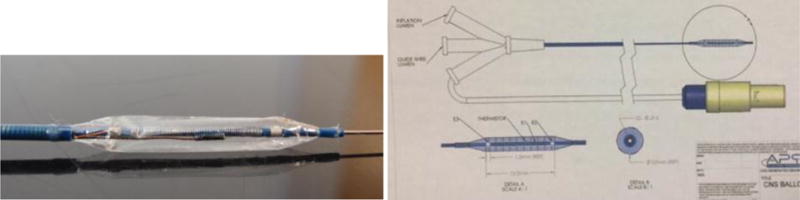
Left: Depicted in this image is the novel over-the-wire balloon catheter, which is lined with polytetrafluoroethylene (PTFE), braided with stainless steel and containing a Pebax outer jacket, consists of 6 electrodes. It consists of 2 rows consisting of 3 electrodes each. Each row of electrodes is 5 mm apart from the other and each electrode is 2 mm apart from the next within the same row, allowing for pacing from several different locations without altering catheter position. Right: Detailed schematic of over-the-wire balloon catheter.
Figure 2. Novel Basket Catheter for venous pacing in the CNS.
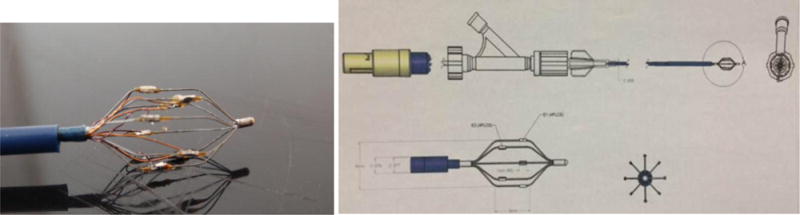
Left: Depicted in this image is the novel Basket catheter used for pacing. It is made up of Nitinol and consists of 90% Platinum/10% Iridium electrodes. The electrodes are insulated from Nitinol with Polyimide. Right: Detailed schematic of basket catheter.
Each electrode was evaluated in various cerebral locations (the mesial temporal lobe and occipital lobe) for its ability to safely be manipulated through the venous system, provide adequate cortical tissue contact to record signals, detect these signals as normal or abnormal, stimulate the cortex, and capture the cortical tissue. (Table 1). Several frequencies were attempted ranging from 30–600 Hz, and various cycle lengths of pacing were implemented. These cycle lengths were adjusted with each stimulation or until electrical capture was obtained. Electrograms before and after stimulation were recorded from the electrodes on each respective intravenous pacing catheter and were documented for normal vs. abnormal activity using a multichannel recording device (Prucka™, General Electric, Milwaukee, USA) with filter settings ranging from 0.5–500 Hz. Stimulation was confirmed by electrogram comparison pre and post pacing shown in Figures 3–5 as well as by the movement of the animal. Capture was characterized by a disruption of normal brain activity and was recorded for each experiment in which it occurred.
Figure 3. Pre- and Post-Capture of cortical tissue after high rate pacing with Cardima 2.7-Fr catheter.
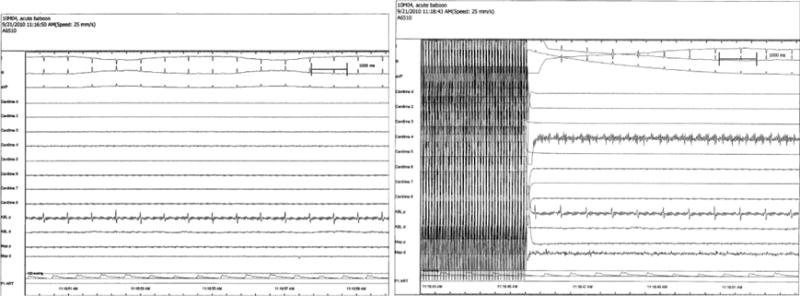
Left: Recording of electrical activity from Cardima 2.7-Fr catheter placed left vein base at a frequency of 30 Hz. Right: Pacing-induced capture of cerebral activity.
Figure 5. Pre- and Post-Capture of cortical tissue after high rate pacing with basket catheter.
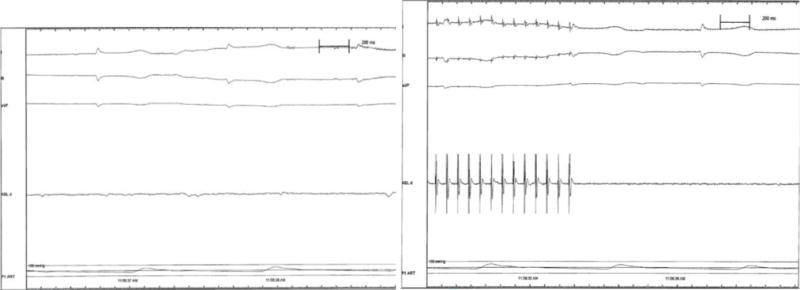
Left: Recording of electrical activity from basket catheter placed in artery at a frequency of 30 Hz. Right: Pacing-induced capture of cerebral activity using basket catheter.
Navigation with magnetic technology
In order to efficiently maneuver the various catheters through the labyrinthine venous sinuses, the NIOBE II system (Stereotaxis, Saint-Louis, MO, USA) was utilized.8 This technology generates a magnetic field which allows for remote control of a steel-tipped, 1.1 Fr-catheter through human vascular structures.
Necropsy
Post-experimentation, animals were euthanized by inducing ventricular fibrillation through direct current applied to the cardiac ventricle. Necropsy was conducted to examine the brain for any grossly abnormal findings from pacing and ablation.
Results
We recorded electrical signals in all tissues tested. We were able to stimulate cortical tissue in a majority of cortical sites and noted capture of cortical tissue when the intravenous catheters were overlying occipital lobe and temporal lobe specifically (Table 1).
Individualized by catheter type, the 2.7-Fr Cardima catheter was tried in four separate experiments. Capture was obtained on 2/4 (50%) occasions, and cycle lengths varied among experiments from 75–650 ms. The 6-Fr 4-mm tip, deflectable EPT catheter was tried in four separate experiments. Capture was obtained on 2/4 (50%) occasions, and cycle lengths varied among experiments from 75–600 ms. The over-the-wire balloon catheter was tried in 12 separate experiments (Figure 1). Capture was obtained on 9/12 (75%) occasions, and cycle lengths varied among experiments from 75–650 ms. Lastly, the basket catheter was tried in three separate experiments (Figure 2). Capture was obtained on 3/3 (100%) occasions. All experiments were conducted with cycle length of 75 ms.
Overall, cycle length during the experiments ranged from 75 ms to 650 ms. Threshold was recorded in 4/12 (33%) experiments; data not recorded for the others. Threshold values ranged from 0.3 – 20 mAmps. Capture of cortical electrical activity was seen in stimulations performed in 11/12 (91.7 %) animal models, the majority of which occurred with use of our novel prototypical over-the-wire balloon catheter (Figure 1). Examples of capture obtained pre- and post-pacing using this catheter are shown in Figure 4 while those obtained by the 2.7-Fr Cardima catheter as well as the basket catheter are depicted in Figures 3 and 5, respectively.
Figure 4. Pre- and Post-Capture of cortical tissue after high rate pacing with over-the-wire balloon catheter.
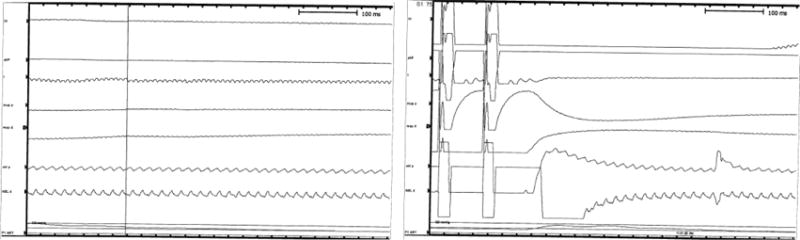
Left: Recording of electrical activity from over-the-wire balloon catheter placed straight sinus at a frequency of 60 Hz. Right: Pacing-induced capture of cerebral activity.
Pathology & Complications
Complications from the procedure were rare. Three of 12 (25%) studies resulted in complications, including coagulum formation, small venous dissection, and catheter breakage (of over-the-wire-balloon catheter during maneuvering into the right distal sigmoid sinus) (Table 1). The catheter breakage was likely related to the specific catheter used. Further iterations of the catheter did not result in breakage due to improved manufacturing.
None of the animal brain specimens examined grossly and histologically showed signs of hemorrhage.
Discussion
Our new intravenous catheters are able to detect, stimulate, and capture cerebral electrical activity. Of the four minimally invasive intravenous catheter-based devices tested in our series of experiments, our novel balloon catheter and basket catheter prototypes were the most successful in achieving consistent capture. In fact, in experiments 1, 3, and 4, only our prototyped over-the-wire balloon catheter (Figure 1) was able to obtain capture, while the Cardima 2.7-French decapolar catheter and the 6-French 4 mm tipped EPT catheter failed to capture cortical activity. The basket catheter (Figure 2) was only tried in three experiments, yet showed successful capture in all three. The 6-Fr 4 mm-tipped EPT catheter was, on numerous occasions, limited in maneuverability, particularly past the petrosal sinus.
In experiment 2, no capture was obtained from either catheter. Possible explanations may be a result of inadequate placement of the catheters in the respective venous drainage sites, preventing solid contact with tissue and resulting in lack of capture. From experiment 4 onwards, we did not use a Cardima 2.7-Fr decapolar catheter (except for once more in experiment 11) since it was felt that we had enough data in terms of mapping using this catheter, and we wanted to focus efforts on testing the newer prototypes. 6-Fr 4 mm-tipped EPT catheter and first-time use of our prototyped over-the-wire balloon catheter were prioritized in these later experiments for pacing.
Current treatment for epilepsy remains subpar. The ability to detect and stimulate cortical tissue intravenously as well as capture these electrical signals may offer a unique manner with which to find epileptic foci. This, coupled with intravenous ablation, which we have described in prior studies, may offer a unique, less invasive, and safer alternative to current options for epilepsy treatment.6,7 Additional studies assessing success of these devices in chronic animal studies and human trials are needed to understand long-term efficacy.
Limitations
There are several limitations to this study. First, our studies are proof-of-concept studies that were performed in the acute setting. Thus, it is unclear as to what the chronic results of implantation of the novel devices will be. Further experiments in animal models will be needed to confirm efficacy. Moreover, all experiments were conducted in animal models. To determine the efficacy in patients, human trials will be crucial if long-term outcomes of this novel device in animal models are successful. Additionally, all of the above studies were conducted with the animals sedated under general anesthesia, which is known to cause lower frequency and higher amplitude of signals on EEG.1 It is therefore possible that these drugs may have had an impact on the capture signals we recorded. While removing such a confounder may not be possible, it is a limitation we must consider.
Lastly, 1 of the 12 experiments (experiment #4) did lead to a complication of coagulum formation on the device. In future studies, we plan to not only have irrigation ability added to the device to preclude this but also apply a negative charge to the electrodes to prevent coagulum formation.10,11 Drug-coated balloon therapy may also be implemented on the catheters to prevent stenosis of devices intravascularly.3 Coupled with anticoagulation therapy, these modifications will minimize the risk of complications in patients implanted.
Conclusion
Of the four catheters tested at the variety of venous sites (including the straight sinus, vein of Galen, etc.) in the cerebral cortex, the novel over-the-wire venous balloon catheter most consistently detected cerebral electrical activity. Stimulation with this device results in local cerebral capture and holds promise for the future development of chronic deep brain and cortical stimulatory devices for the management of epilepsy. Further chronic animal studies and human trials are needed to evaluate such chronic efficacy.
Acknowledgments
Funding: C.V.D. was partially supported by an NIH T32 training grant (HL 007111). This project was funded by the Discovery Translational Fund and the University of MN Partnership grant.
References
- 1.Brown EN, Lydic R, Schiff ND. General anesthesia, sleep, and coma. N Engl J Med. 2010;363:2638–2650. doi: 10.1056/NEJMra0808281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Connor DE, Jr, Nixon M, Nanda A, Guthikonda B. Vagal nerve stimulation for the treatment of medically refractory epilepsy: a review of the current literature. Neurosurg Focus. 2012;32:E12. doi: 10.3171/2011.12.FOCUS11328. [DOI] [PubMed] [Google Scholar]
- 3.De SC, Holmes DR, Jr, Ebrille E, Syed FF, Ladewig DJ, Mikell SB, et al. Direct Pulmonary Vein Ablation With Stenosis Prevention Therapy. J Cardiovasc Electrophysiol. 2015 doi: 10.1111/jce.12732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fisher RS, Velasco AL. Electrical brain stimulation for epilepsy. Nat Rev Neurol. 2014;10:261–270. doi: 10.1038/nrneurol.2014.59. [DOI] [PubMed] [Google Scholar]
- 5.Gross RE, Mahmoudi B, Riley JP. Less is more: novel less-invasive surgical techniques for mesial temporal lobe epilepsy that minimize cognitive impairment. Curr Opin Neurol. 2015 doi: 10.1097/WCO.0000000000000176. [DOI] [PubMed] [Google Scholar]
- 6.Henz BD, Friedman PA, Bruce CJ, Holmes DR, Bower M, Madhavan M, et al. Advances in radiofrequency ablation of the cerebral cortex in primates using the venous system: Improvements for treating epilepsy with catheter ablation technology. Epilepsy Res. 2014;108:1026–1031. doi: 10.1016/j.eplepsyres.2014.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Henz BD, Friedman PA, Bruce CJ, Holmes DR, Jr, Okumura Y, Johnson SB, et al. Successful radiofrequency ablation of the cerebral cortex in pigs using the venous system: possible implications for treating CNS disorders. Epilepsy Res. 2008;80:213–218. doi: 10.1016/j.eplepsyres.2008.03.023. [DOI] [PubMed] [Google Scholar]
- 8.Kara T, Leinveber P, Vlasin M, Jurak P, Novak M, Novak Z, et al. Endovascular brain intervention and mapping in a dog experimental model using magnetically-guided micro-catheter technology. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2014;158:221–226. doi: 10.5507/bp.2012.076. [DOI] [PubMed] [Google Scholar]
- 9.Liao W, Ji GJ, Xu Q, Wei W, Wang J, Wang Z, et al. Functional Connectome before and following Temporal Lobectomy in Mesial Temporal Lobe Epilepsy. Sci Rep. 2016;6:23153. doi: 10.1038/srep23153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lim B, Venkatachalam KL, Henz BD, Johnson SB, Jahangir A, Asirvatham SJ. Prevention of Coagulum Formation With Simultaneous Charge Delivery in Radiofrequency AblationA Canine Model. JACC: Clinical Electrophysiology. 2016 doi: 10.1016/j.jacep.2015.11.007. [DOI] [PubMed] [Google Scholar]
- 11.Lim B, Venkatachalam KL, Jahangir A, Johnson SB, Asirvatham SJ. Concurrent application of charge using a novel circuit prevents heat-related coagulum formation during radiofrequency ablation. J Cardiovasc Electrophysiol. 2008;19:843–850. doi: 10.1111/j.1540-8167.2008.01117.x. [DOI] [PubMed] [Google Scholar]


