Abstract
Purpose
The aim of this study was to analyze clinical characteristics of skeletal metastasis in epidermal growth factor receptor (EGFR) mutant non-small cell lung cancer (NSCLC) and treatment outcomes of continued EGFR tyrosine kinase inhibitor (TKI) therapy in patients presenting with skeletal metastasis progression.
Materials and Methods
Of the 216 patients treated with EGFR-TKI for management of stage III-IV NSCLC between 2006 and 2012 in Seoul St. Mary’s Hospital, 76 patients with confirmed EGFR-mutated NSCLC with skeletal metastases during therapy were analyzed retrospectively.
Results
Of 76 patients with EGFR mutant lung cancer with skeletal metastasis, 37 patients developed first progressive disease (PD) in skeletal regions. EGFR-TKI was continued in these 37 patients after first PD in skeletal regions. Median time to first PD of skeletal regions was 8.9 months (95% confidence interval [CI], 4.8 to 13.0). Median time of continued EGFR-TKI after first PD of skeletal regions was 8.0 months (95% CI, 2.9 to 13.0) in patients with disease progression of preexisting regions, 5.6 months (95% CI, 4.5 to 6.7) in patients showing new localized regions, and 3.3 months (95% CI, 1.1 to 5.5) in patients with multiple new metastatic regions (p=0.006). Median time of postskeletal metastasis progression survival was 23.0 months (95% CI, 13.5 to 32.5), 15.0 months (95% CI, 3 to 34.7), and 7.0 months (95% CI, 6.0 to 8.0) (p=0.004) in the above described patient groups, respectively. Overall, seven patients (18.9%) had more than one episode of skeletal progression of disease without extraskeletal PD.
Conclusion
Continued EGFR-TKI treatment with adequate local treatment after progression of skeletal metastasis may be considered for patients who show disease progression in preexisting regions or local progression.
Keywords: EGFR, Non-small cell lung carcinoma, EGFR tyrosine kinase inhibitor, Bone metastasis, Response Evaluation Criteria in Solid Tumors
Introduction
Epidermal growth factor receptor tyrosine kinase inhibitors (EGFR-TKI) represent standard first-line treatment for patients with advanced and metastatic non-small cell lung cancer (NSCLC) harboring somatic sensitizing mutations in EGFR [1]. However, patients who initially respond to treatment often develop acquired resistance. According to a previous study, 23% of patients experience symptomatic flares after termination of TKI treatment and EGFR-TKI exerts minimal toxicity, compared to cytotoxic chemotherapy [2]. Therefore, some patients continue EGFR-TKI after Response Evaluation Criteria in Solid Tumors (RECIST)-based progression, particularly when the disease is controllable with local therapy options, such as radiotherapy or surgery or both [3,4]. Currently, continued EGFR-TKI after RECIST progressive disease (PD) could be considered as a treatment option for cases of localized or gradual PD in patients without EGFR exon 20 T790 mutations or those unable to participate in clinical trials [5].
Skeletal metastasis is considered the predominant cause of hospital morbidity and impaired quality of life among NSCLC patients with symptomatic flares [6]. Historically, development of skeletal metastasis occurs in 30%-40% of patients with advanced NSCLC. This percentage is expected to increase with the application of newer and more sensitive screening/imaging technologies for metastatic disease and prolongation of patient survival [7,8]. Continued EGFR-TKI could be considered after RECIST PD of skeletal metastasis, compared to other systemic progression, because of the limitation in efficacy of systemic cytotoxic chemotherapy in the management of skeletal metastasis, and skeletal related adverse events (SREs) related to disease progression are generally treated using local radiotherapy and surgical intervention.
Based on this clinical practice, we retrospectively analyzed the clinical characteristics of progressive skeletal metastasis in cases of EGFR-mutated NSCLC treated with EGFR-TKI, with the aim of identifying the patient populations that may benefit from continued EGFR-TKI therapy after RECIST PD of skeletal metastasis.
Materials and Methods
1. Patients
A total of 216 patients treated with EGFR-TKI for management of recurrent or unresectable stage III-IV NSCLC between March 2006 and 2012 in Seoul St. Mary’s Hospital were identified from the cancer registry. Of these, 76 patients with confirmed EGFR-mutated NSCLC presenting with skeletal metastasis during EGFR-TKI therapy were further distinguished. Patients diagnosed with skeletal metastasis just prior to commencement of EGFR-TKI therapy were included, as well as those who developed metastasis during therapy. Patients who developed skeletal metastasis after completing EGFR-TKI therapy or those with bone metastasis and completely regressed before starting EGFR-TKI therapy and did not progress during EGFR-TKI therapy were excluded. Skeletal metastasis was diagnosed using positron emission tomography (PET)–computed tomography (CT) or magnetic resonance imaging (MRI).
Collection of clinical information from patients with somatic EGFR mutations was approved by the institutional review board. Written informed consent to allow genetic screening for EGFR-sensitizing mutations was obtained from each patient at the time of diagnosis or prior to EGFR-TKI treatment.
2. Mutational analysis
Tumor specimens for each patient were obtained using diagnostic or surgical procedures. Samples were paraffinembedded and DNA extracted analyzed for EGFR mutations EGFR exons 18 to 21 were amplified using polymerase chain reaction (PCR), and analyzed bidirectionally via direct sequencing to confirm the presence of somatic mutations. Mutations were confirmed with multiple independent PCR reactions using previously reported criteria [9]. The following EGFR mutations were considered sensitizing: deletion in exon 19, duplication in exon 19, deletion-insertion of exon 19, L858R and L861Q point mutations, and the G719 missense point mutation [9].
3. Treatment and response evaluation
During EGFR-TKI treatment, tumor measurement and response assessment were performed by a thoracic radiologist, musculoskeletal radiologist, and nuclear medicine physician separately at baseline and follow-up, using RECIST 1.1 at each follow-up scan.
According to our lung cancer multidisciplinary team protocol, regarding chest and abdomen CT scan, chest and abdomen CT scan was performed every 6 weeks. If the patient was diagnosed as having skeletal metastasis based on initial diagnostic imaging (chest CT scan, abdomen CT, brain MRI, PET-CT scan, and bone scan), bone scan imaging was performed every 6 weeks when the patient underwent chest and abdominal CT scan. PET-CT and MRI were additionally performed every 6 months and where clinically indicated, to confirm suspicious regions.
Radiotherapy was usually performed at 30-40 Gy for 2-3 weeks with palliative intent. Surgery was performed in cases of PD at a previous radiation site and high-risk pathologic fractures. During radiotherapy for skeletal metastasis, EGFR-TKI was continued for all patients who tolerated the treatment.
4. Analysis of skeletal metastasis
In terms of analysis of PET-CT scan, all fluorodeoxyglucose (FDG) PET-CT images were reviewed using fusion software (Syngo, Siemens Medical Solutions, Knoxville, TN), which provided multiplanar reformatted images and displayed PET images with attenuation correction, CT images, and PET-CT fusion images. Two nuclear-medicine physicians reviewed the images and reached a consensus. For semiquantitative analysis, the regions of interest were delineated on transaxial images around the areas with increased FDG uptake, and the maximum standardized uptake value (SUVmax), which is widely used to quantify FDG uptake compared to mean liver SUV value and normal surrounding tissue, was calculated.
Findings of PET- and CT-imaging studies were analyzed separately. For further analysis of CT images, we searched for evidence of involvement of soft tissue, presence of osteoblastic or osteolytic lesions, and evidence of fracture in lesions that demonstrated FDG uptake. The presence of fracture lines or callus formation was interpreted as evidence of fracture. CT images were analyzed in the bone-setting window [10].
Response evaluation of skeletal metastasis was based mainly on RECIST criteria 1.1 of non-target regions, however we considered response evaluation of target regions for a soft tissue mass larger than 1 cm. In detail, complete response (CR) of skeletal metastatic regions was defined as normalization of tracer uptake by bone scan, complete sclerotic fill-in of lytic lesions and the restoration of normal bone density on CT scan and normalization of all lesions to SUV signal less than mean liver SUV and equal to normal surrounding tissue SUV by PET-CT scan [11].
In terms of bone flare phenomenon, to differentiate the patients with bone flare phenomenon from true PD, for patients who developed new regions in bone scan (especially first 6 weeks scan) who showed clinical symptoms, the MRI and PET-CT scan were checked to exclude true progression and patients who showed no symptoms and no evidence of PD in the MRI and PET-CT scan were followed up for the next 6 weeks with bone scan because most cases of bone flare phenomenon after EGFR-TKI therapy are reported to occur within the first 3 months [12].
5. Statistical analysis
Differences in baseline characteristics between groups were compared using Fisher exact test for categorical data and Wilcoxon signed-rank test for continuous data. The Kaplan-Meier method was used to estimate time-to-event distribution and follow-up. All tests were two-sided, with a significance level of 0.05.
In patients who continued EGFR-TKI therapy beyond first PD in skeletal metastasis, median time to first PD was defined as date of initiation of EGFR-TKI therapy to first PD in skeletal regions. The duration of continued EGFR-TKI was defined as the date from first PD in skeletal regions to termination of therapy. Postskeletal metastasis survival was defined as the date of first PD in skeletal regions to death from any cause. Overall time-to-progression was defined as the date of initiation of therapy to EGFR-TKI termination. No patients died prior to RECIST PD, but those who did not experience PD were censored at the last follow-up. Log-rank test was used for comparison of survival curves among the patient groups. Rate ratios and their 95% confidence intervals (CIs) were calculated. The SPSS ver. 15.0 (SPSS, Inc., Chicago, IL) was used for analysis.
Results
1. Comparison of clinical characteristics between patients with first PD in skeletal and extraskeletal regions
Among the 216 patients treated with EGFR-TKI, 76 had skeletal metastasis. Within this patient group, 73 (96.1%) were diagnosed with skeletal metastasis via PET-CT scan only and three with MRI only. Thirty-six patients (47.3%) were diagnosed using both MRI and PET scan.
Thirty-seven patients developed first PD in skeletal regions only, and 39 in extraskeletal and/or skeletal regions. Multiple bone metastases was more prevalent in patients with first PD in skeletal regions, compared to those with first PD in extraskeletal regions (Table 1).
Table 1.
Clinical characteristics of patients with EGFR mutant NSCLC with skeletal metastasis according to first progression sites
| Clinical characteristic | Skeletal region only (n=37) | Extraskeletal±skeletal regions (n=39) | p-value |
|---|---|---|---|
| Age, mean (yr) | 58.2 | 62.6 | 0.061 |
| Sex | |||
| Male | 15 (40.5) | 13 (33.3) | - |
| Female | 22 (59.5) | 26 (66.7) | |
| ECOG | |||
| 0/1 | 20 (54.1) | 22 (56.4) | - |
| ≥ 2 | 17 (45.9) | 17 (43.6) | |
| Smoking | |||
| Never | 24 (62.2) | 29 (74.4) | - |
| Current/former | 13 (37.8) | 10 (25.6) | |
| EGFR mutation | |||
| Exon 19 del | 19 (51.4) | 17 (43.6) | - |
| Exon 21 L858R | 12 (32.4) | 19 (48.7) | |
| Exon 18 G719X | 3 (8.1) | 1 (2.6) | |
| Exon 21 L861Q | 2 (5.4) | 2 (5.1) | |
| Exon 19 insertion | 1 (2.7) | ||
| No. of bone metastases | |||
| Single | 4 (10.8) | 12 (30.8) | 0.048 |
| Multiple | 33 (89.2) | 27 (69.2) | |
| Brain metastasis | |||
| No | 20 (54.1) | 16 (41.0) | - |
| Yes | 17 (45.9) | 23 (59.0) | |
| Extrathoracic metastasis (except bone and brain) | |||
| No | 28 (75.7) | 27 (69.2) | - |
| Yes | 9 (24.3) | 12 (30.8) | |
| Management of skeletal metastasis before EGFR-TKIs | |||
| No | 17 (48.5) | 26 (65.1) | 0.068 |
| Yes | 20 (51.5) | 13 (34.9) | |
| Sort of EGFR-TKI | |||
| Gefitinib | 25 (67.6) | 21 (53.8) | - |
| Erlotinib | 12 (32.5) | 17 (43.6) | |
| Line of EGFR-TKI | |||
| 1st line | 25 (67.6) | 21 (53.8) | - |
| 2nd/3rd line | 12 (32.4) | 18 (46.2) | |
| Response to EGFR-TKIs | |||
| CR/PR | 31 (84.8) | 34 (80.0) | - |
| SD | 6 (15.2) | 4 (11.6) | |
| PD | 1 (2.3) | ||
| Progression sites at the time of stopping EGFR-TKI | 31 | 29 | |
| Extraskeletal regions only | 4 (12.9) | 19 (67.9) | 0.001 |
| Skeletal and extraskeletal regions | 19 (61.3) | 10 (32.1) | |
| Skeletal regions only | 8 (25.8) | ||
| Disease flare at stopping EGFR-TKI | 7 (22.5) | 4 (14.3) | 0.147 |
| Overall TTP, median (95% CI, mo) | 17.2 (13.1-21.1) | 10.4 (7.4-14.4) | 0.031 |
| OS, median (95% CI, mo) | 37.2 (14.1-61.2) | 37.3 (28.1-46.1) | 0.639 |
Values are presented as number (%) unless otherwise indicated. EGFR, epidermal growth factor receptor; NSCLC, non-small cell lung cancer; ECOG, Eastern Cooperative Oncology Group; TKI, tyrosine kinase inhibitor; CR, complete response; PR, partial response; SD, stable disease; PD, progressive disease; TTP, time to progression; CI, confidence interval; OS, overall survival.
At the time of stopping EGFR-TKI, 27 of 31 patients (88.1%) in the first PD in skeletal regions group developed PD in skeletal regions, compared with 10 patients (32.1%) in the extraskeletal regions PD group (p=0.001). Among the 27 patients, eight patients still had skeletal PD at the time of EGFR-TKI termination. Of the 11 patients admitted to hospital at the time of termination of EGFR-TKI therapy, seven patients (22.5%) were in the first PD in skeletal regions group. Five of these patients were admitted due to SREs (pathologic fractures and cord compressions) (Table 1).
No significant difference in median overall survival (OS) was observed between the two groups. Overall, 11 patients underwent postprogression biopsy at the time of EGFR-TKI termination for evaluation of the presence of resistant EGFR exon 20 T790M mutations. Our data showed that five patients had acquired this EGFR mutation.
In terms of OS between patients who continued EGFR-TKI beyond PD and patients who discontinued EGFR-TKI after PD, overall 41 patients continued EGFR-TKI after RECIST PD including 37 patients with skeletal metastasis only progression and four patients with PD with extraskeletal and/or skeletal metastasis. No significant difference in median OS between patients who continued EGFR-TKI and patients who discontinued EGFR-TKI after PD was observed (34.6 months vs. 35.5 months, p=0.905) (Fig. 1).
Fig. 1.
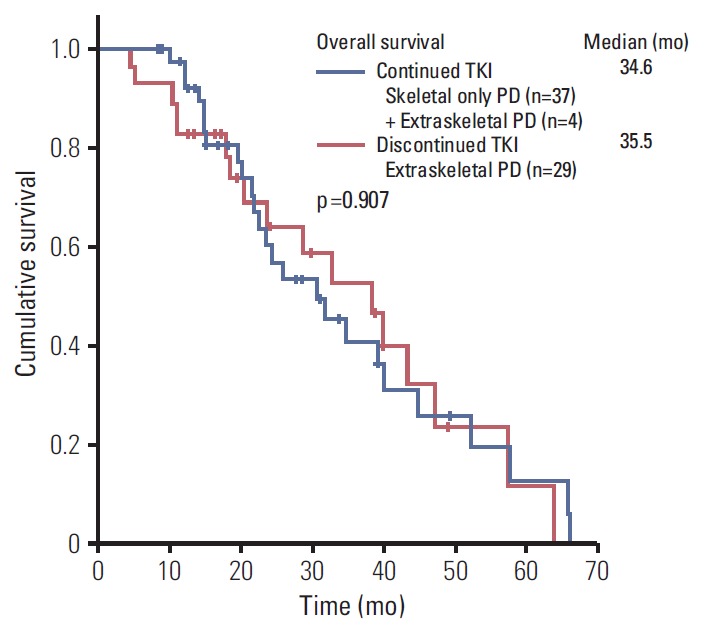
Median overall survival time of patients who continued epidermal growth factor receptor tyrosine kinase inhibitor (EGFR-TKI) therapy and patients who discontinued EGFR-TKI therapy after progressive disease (PD).
2. Clinical disease progression patterns of patients continuing EGFR-TKI after first PD in skeletal regions
No symptoms were evident in 15 of the 37 patients (40.5%) who developed first PD in skeletal regions only. These asymptomatic patients, as well as eight patients who experienced pain without pathologic fracture were diagnosed with PD via routine evaluation of skeletal regions.
Patients were categorized according to three groups based on clinical characteristics of skeletal progression. The first group showed reappearance of metastasis in skeletal regions after having achieved CR, confirmed using PET-CT scan or MRI, following either local or EGFR-TKI therapy. The second group had localized progression of skeletal metastasis limited to one segment of vertebra or less than three sites in other skeletal regions according to the scope of the radiation field. The third group showed newly developed multiple skeletal metastases (Tables 2 and 3).
Table 2.
Classification of skeletal metastasis progression in EGFR mutant NSCLC after EGFR-TKI therapy based on clinical characteristics
| Classifications of progression in skeletal metastasis | |
|---|---|
| Progression of preexisting regions | Reappearance of metastasis in skeletal regions after having achieved CR |
| New localized regions | Localized progression of skeletal metastasis limited to one segment of vertebra or less than 3 sites in other skeletal regions |
| Multiple new regions | Multiple new regions more than one segment of vertebrae and more than 3 sites in skeletal regions |
EGFR, epidermal growth factor receptor; NSCLC, non-small cell lung cancer; TKI, tyrosine kinase inhibitor; CR, complete response.
Table 3.
Clinical characteristics of patients who progressed only skeletal regions according to patterns of skeletal metastasis progression
| Overall (n=37) | Progression of preexisting regions after CR (n=12) | New localized regions (n=13) | Multiple new regions (n=12) | |
|---|---|---|---|---|
| Symptom | ||||
| Asymptomatic new regions | 15 | 2 | 9 | 4 |
| Pain without pathologic fracture | 18 | 10 | 1 | 7 |
| Pathologic fracture | 2 | - | 1 | 1 |
| Cord compression | 2 | - | 2 | - |
| Treatment of skeletal metastasis | ||||
| Surgery | 6 | - | 3 | 3 |
| Radiotherapy | 25 | 11 | 7 | 7 |
| No. of patients with > 1 episode of PD in skeletal regions | 7 | 4 | 3 | - |
| Response to EGFR-TKI at the time of first PD (except skeletal region) | ||||
| Respondinga) | 31 | 10 | 12 | 10 |
| Impending PDb) | 6 | 2 | 1 | 2 |
| Progression site at the time of stopping EGFR-TKI | ||||
| Skeletal regions | 8 | 1 | 3 | 4 |
| Skeletal+extraskeletal regions | 19 | 8 | 6 | 5 |
| Extraskeletal regions | 4 | 2 | - | 2 |
CR, complete response; PD, progressive disease; EGFR, epidermal growth factor receptor; TKI, tyrosine kinase inhibitor.
No increase compared to nadir assessment in target region and stable disease (SD) in non-target region,
Overall SD but increase (< 20% of summation of long diameter and < absolute 5 mm compared to nadir assessment) in target region and SD in non-target region.
In 12 patients, bone regions reappeared after CR, just progressed preexisting regions without new regions. Ten patients experiencing pain and one with no symptoms received radiotherapy to skeletal metastasis regions. Overall, five patients who had achieved CR with EGFR-TKI alone received radiotherapy and re-irradiation therapy was administered to the remaining six patients. Four patients had more than two episodes of subsequent progression of skeletal metastasis. Two of these patients experienced three episodes of subsequent progression without PD of extraskeletal regions before termination of EGFR-TKI. Among the 11 patients who stopped EGFR-TKI because of subsequent PD, eight showed disease progression to both skeletal and extraskeletal regions. Development of new brain metastasis occurred in two patients and leptomeningeal seeding metastasis in one patient. Two patients were admitted because of bone pain.
Thirteen patients showed localized disease progression in skeletal regions. Nine patients had no symptoms, and three patients experienced more than two episodes of subsequent skeletal metastasis. One patient developed new brain metastasis, and one was admitted because of cord compression at the time of EGFR-TKI termination.
Twelve patients developed multiple new skeletal metastases. Seven patients received local radiotherapy for symptomatic sites; however, the duration of radiation was not extended to more than 1 month, and the radiation field was less than three sites. One patient switched to systemic chemotherapy immediately after completing radiotherapy, due to subsequent PD. Among the 11 patients who stopped EGFR-TKI, four showed disease progression in skeletal regions only. New brain metastasis was reported in one patient. Two patients were admitted due to skeletal-related adverse events and two due to malignant pleural effusion.
In terms of other SREs, no patients had hypercalcemia, and only three received bisphosphonate.
3. Clinical outcomes of continued EGFR-TKI after first PD in skeletal regions
Median time to first PD of skeletal regions was 8.9 months (95% CI, 4.8 to 13.0), the duration of continued EGFR-TKI beyond PD was 5.6 months (95% CI, 3.2 to 7.9), and postskeletal metastasis survival was 14.0 months (95% CI, 10.1 to 17.9). According to the clinical characteristics of progression in skeletal regions, median time to first PD differed significantly among the three groups (p=0.037) (Table 4). Median time of continued EGFR-TKI after first PD was 8.0 months (95% CI, 2.9 to 13.0) in patients with bone regions reappeared of preexisting regions after CR, 5.6 months (95% CI, 4.5 to 6.7) in patients with new localized regions, and 3.3 months (95% CI, 1.1 to 5.5) in those with newly developed multiple metastatic regions (p=0.006) (Table 4, Fig. 2A). Postskeletal metastasis survival was 23.0 months (95% CI, 13.5 to 32.5), 15.0 months (95% CI, 3 to 34.7), and 7.0 months (95% CI, 6.0 to 8.0) (p=0.004) in the three groups, respectively (Table 4, Fig. 2B). Median OS was 39.0 months (95% CI, 21.1 to 56.9), 33.0 months (95% CI, 14.0 to 51.9), and 14.0 months (95% CI, 8.2 to 19.8) (p=0.003), respectively (Table 4, Fig. 2B).
Table 4.
Clinical outcomes of continued EGFR-TKI therapy according to patterns of progression in skeletal metastasis
| Progression of preexisting regions | New localized regions | Multiple new regions | p-value | |
|---|---|---|---|---|
| Median time to first PD (95 % CI, mo) | 13.0 (9.9-16.0) | 9.2 (5.5-12.9) | 6.7 (6.2-7.2) | 0.037 |
| Median duration of continued EGFR-TKI after first PD (95 % CI, mo) | 8.0 (3.4-13.0) | 5.6 (4.5-6.7) | 3.3 (1.1-5.5) | 0.006 |
| Postskeletal metastasis survival (95 % CI, mo) | 23.0 (13.5-32.5) | 15.0 (3-34.7) | 7.0 (6.0-8.0) | 0.004 |
| Median overall TTP (95 % CI, mo) | 26.9 (11.3-36.2) | 17.5 (14.0-21.0) | 9.2 (1.7-16.7) | < 0.001 |
| Median OS (95 % CI, mo) | 39.0 (21.1-56.9) | 33.0 (14.0-51.9) | 14.0 (8.2-19.8) | 0.003 |
EGFR, epidermal growth factor receptor; TKI, tyrosine kinase inhibitor; PD, progressive disease; CI, confidence interval; TTP, time to progression; OS, overall survival.
Fig. 2.
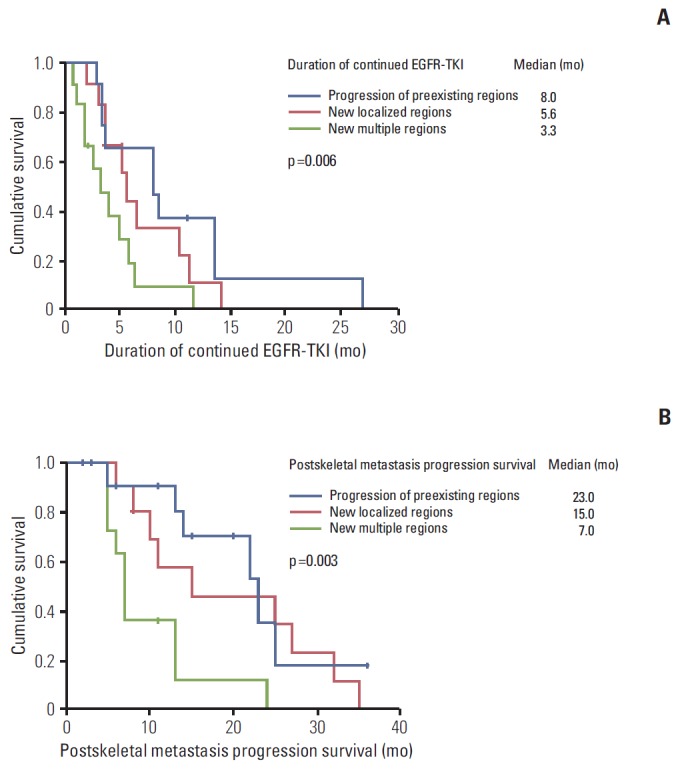
(A) Median time of continued epidermal growth factor receptor tyrosine kinase inhibitor (EGFR-TKI) after first progressive disease for patient groups according to patterns of progression in skeletal metastasis. (B) Postskeletal metastasis progression survival for patient groups according to patterns of progression in skeletal metastasis.
According to clinical symptoms and response to EGFR-TKI, median time of continued EGFR-TKI was 6.4 months (95% CI, 4.2 to 8.6) in asymptomatic patients, 3.7 months (95% CI, 1.0 to 6.4) in symptomatic patients (p=0.462), 5.6 months (95% CI, 2.5 to 8.4) in responding patients, and 5.2 months (95% CI, 2.4 to 8.6) in patients with signs of impending disease progression.
Discussion
The overall incidence of skeletal metastasis in EGFR-mutated NSCLC does not appear to be higher, compared to other wild-type or K-ras mutated NSCLC, although post-metastatic bone disease survival is longer [13]. In our study, survival after first skeletal PD was 14.0 months. Thus, patients with skeletal metastasis had a greater chance of developing new skeletal metastases and SREs. In addition, seven patients (18.9%) experienced more than two episodes of PD. Management of skeletal metastasis should be a priority in patients developing first PD in skeletal regions.
To prevent skeletal-related adverse events and morbidity, early detection and treatment with bisphosphonate is generally recommended. In our study, due to limitations in accessibility to zoledronic acid, only three patients could receive bisphosphonate. However, PET-CT scanning every 6 months facilitated the early detection of new skeletal metastasis before development of symptoms. Overall, development of asymptomatic new skeletal metastasis occurred in 40.5% of patients. Although new skeletal metastasis without PD of the extraskeletal region is considered PD according to RECIST criteria, continued EGFR-TKI could be considered because of the feasibility of combination with radiotherapy and limited efficacy of the other systemic treatment in management of skeletal metastasis [14]. EGFR-TKI therapy has shown favorable outcomes in prevention of SREs, since these agents inhibit differentiation of bone marrow stromal cells to osteoclasts and promote osteoblastic activity in the metastatic bone region [15]. An earlier small-scale Japanese study reported prolonged benefits of continued EGFR-TKI after bone metastasis progression [16].
In terms of benefit in continued EGFR-TKI therapy after PD, no differences in OS were observed between patients who continued EGFR-TKI and patients who discontinued EGFR-TKI in the overall population (Fig. 1). However, we could not make any conclusion about the benefit of EGFR-TKI therapy because most patients who continued EGFR-TKI therapy were in the skeletal only PD group and development of multiple new skeletal metastases occurred in 12 patients of that group, considered the dramatic progression group who had the poor outcome. These patients only continued EGFR-TKI for 3.3 months. Several different criteria are employed for classifying patterns of progression in EGFR-mutated lung cancer for selection of patients who might benefit from continued treatment [3-5,17-19].
Duration of disease control, tumor growth rate, changes in overall tumor volume, and subjective symptoms are important predictors of the length of continued EGFR-TKI beyond RECIST PD [3,5,17]. CT or MRI scans, standard methods of assessment of RECIST criteria, can only be applied for evaluation of skeletal regions with identifiable soft tissue components [20]. The majority of skeletal metastasis regions are considered non-target areas, and PD is defined by new regions or unequivocal progression of preexisting skeletal metastasis [11,20]. Adjustment of RECIST PD in skeletal metastasis to previous classifications of progression patterns in EGFR-mutated NSCLC is difficult. Compared to previous studies, our study showed no differences in the duration of continued EGFR-TKI according to the presence of symptoms and changes or overall response of other extraskeletal or target regions [5,19]. Our data showed pain symptoms in 10 out of 12 patients in the group with disease progression of preexisting regions after CR, because patients who had previously experienced pain in the skeletal metastatic regions were thought to be more sensitive to pain in the same regions. Thus, we classified skeletal metastasis as disease progression of preexisting regions after CR, localized progression, and multiple new metastases groups. Patients with progression in preexisting regions or localized progression could be considered to benefit from continued EGFR-TKI therapy and adequate local treatment such as radiotherapy after PD in skeletal regions. These groups could be classified as gradual or localized progression of skeletal metastasis, as suggested previously [3,5,17].
In addition, patients with the secondary T790M mutation are reported to benefit from EGFR-TKI treatment beyond disease progression, compared to those without the mutation [21]. Only 11 patients could be evaluated for secondary mutations at the time of terminating EGFR-TKI. Due to the insufficient number of patients in the current analysis, we could not conclusively show benefits of continuing EGFR-TKI in the subgroup with the T790M mutation. In practice, it is difficult to obtain the appropriate tissue specimens for molecular studies after progression of EGFR-TKI therapy, particularly in cases of bone metastasis. A previous study reported the lowest yield of 40% for decalcified material in bone samples (4/10), even using a new assay, due to alterations in DNA after the procedure of decalcification with acid [22]. In cases of rebiopsy after progression of EGFR-TKI, relatively small samples and association with non-neoplastic cells can lead to false-negative results [22]. In cases where skeletal metastasis is the only progression site, the cell-free plasma DNA assay for EGFR T790M may be an effective option for detection of resistant mutations [23,24].
It is important to note that our study has several limitations. Major weaknesses include its retrospective design, small sample size, and evaluation of bone metastasis. Bone metastasis was assessed every 6 weeks using a whole-body bone scan and every 6 months PET-CT and MRI, and suspicious regions were further confirmed with MRI or PET scans. Due to the considerable incidence of false-negative results of Bone scan, the window period should be considered between the date of false-negative bone scan and true positive subsequent PET-CT scan [11,25]. Practically, establishment of an effective standard method for response assessment in skeletal metastasis is needed. Differences in specificities and sensitivities among imaging modalities should also be considered in response evaluation of skeletal metastasis [25]. Detection of skeletal metastasis progression with newly developing imaging modalities should be more rapid than that achieved in the current study.
Conclusion
In conclusion, continued EGFR-TKI with adequate local treatment such as radiation therapy may be an option in patients showing disease progression to preexisting regions after CR or local progression of skeletal metastasis. Considering the difficulties in response evaluation and re-biopsy for molecular analysis as well as the influence of skeletal metastasis on morbidity, investigation of different evaluation methods and treatment strategies is required for future applications.
Acknowledgments
This study is supported by the Cancer Research Institute, The Catholic University of Korea, Seoul, Korea.
Footnotes
Conflict of Interest relevant to this article was not reported.
References
- 1.Maemondo M, Inoue A, Kobayashi K, Sugawara S, Oizumi S, Isobe H, et al. Gefitinib or chemotherapy for non-small-cell lung cancer with mutated EGFR. N Engl J Med. 2010;362:2380–8. doi: 10.1056/NEJMoa0909530. [DOI] [PubMed] [Google Scholar]
- 2.Chaft JE, Oxnard GR, Sima CS, Kris MG, Miller VA, Riely GJ. Disease flare after tyrosine kinase inhibitor discontinuation in patients with EGFR-mutant lung cancer and acquired resistance to erlotinib or gefitinib: implications for clinical trial design. Clin Cancer Res. 2011;17:6298–303. doi: 10.1158/1078-0432.CCR-11-1468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Conforti F, Catania C, Toffalorio F, Duca M, Spitaleri G, Barberis M, et al. EGFR tyrosine kinase inhibitors beyond focal progression obtain a prolonged disease control in patients with advanced adenocarcinoma of the lung. Lung Cancer. 2013;81:440–4. doi: 10.1016/j.lungcan.2013.05.019. [DOI] [PubMed] [Google Scholar]
- 4.Nishie K, Kawaguchi T, Tamiya A, Mimori T, Takeuchi N, Matsuda Y, et al. Epidermal growth factor receptor tyrosine kinase inhibitors beyond progressive disease: a retrospective analysis for Japanese patients with activating EGFR mutations. J Thorac Oncol. 2012;7:1722–7. doi: 10.1097/JTO.0b013e31826913f7. [DOI] [PubMed] [Google Scholar]
- 5.Yang JJ, Chen HJ, Yan HH, Zhang XC, Zhou Q, Su J, et al. Clinical modes of EGFR tyrosine kinase inhibitor failure and subsequent management in advanced non-small cell lung cancer. Lung Cancer. 2013;79:33–9. doi: 10.1016/j.lungcan.2012.09.016. [DOI] [PubMed] [Google Scholar]
- 6.Coleman RE. Skeletal complications of malignancy. Cancer. 1997;80(8 Suppl):1588–94. doi: 10.1002/(sici)1097-0142(19971015)80:8+<1588::aid-cncr9>3.3.co;2-z. [DOI] [PubMed] [Google Scholar]
- 7.Coleman RE. Metastatic bone disease: clinical features, pathophysiology and treatment strategies. Cancer Treat Rev. 2001;27:165–76. doi: 10.1053/ctrv.2000.0210. [DOI] [PubMed] [Google Scholar]
- 8.Bury T, Barreto A, Daenen F, Barthelemy N, Ghaye B, Rigo P. Fluorine-18 deoxyglucose positron emission tomography for the detection of bone metastases in patients with non-small cell lung cancer. Eur J Nucl Med. 1998;25:1244–7. doi: 10.1007/s002590050291. [DOI] [PubMed] [Google Scholar]
- 9.Lynch TJ, Bell DW, Sordella R, Gurubhagavatula S, Okimoto RA, Brannigan BW, et al. Activating mutations in the epidermal growth factor receptor underlying responsiveness of nonsmall-cell lung cancer to gefitinib. N Engl J Med. 2004;350:2129–39. doi: 10.1056/NEJMoa040938. [DOI] [PubMed] [Google Scholar]
- 10.Choi HS, Yoo IR, Park HL, Choi EK, Kim SH, Lee WH. Role of (1)(8)F-FDG PET/CT in differentiation of a benign lesion and metastasis on the ribs of cancer patients. Clin Imaging. 2014;38:109–14. doi: 10.1016/j.clinimag.2013.11.011. [DOI] [PubMed] [Google Scholar]
- 11.Costelloe CM, Chuang HH, Madewell JE, Ueno NT. Cancer response criteria and bone metastases: RECIST 1.1, MDA and PERCIST. J Cancer. 2010;1:80–92. doi: 10.7150/jca.1.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chao HS, Chang CP, Chiu CH, Chu LS, Chen YM, Tsai CM. Bone scan flare phenomenon in non-small-cell lung cancer patients treated with gefitinib. Clin Nucl Med. 2009;34:346–9. doi: 10.1097/RLU.0b013e3181a344df. [DOI] [PubMed] [Google Scholar]
- 13.Hendriks LE, Smit EF, Vosse BA, Mellema WW, Heideman DA, Bootsma GP, et al. EGFR mutated non-small cell lung cancer patients: more prone to development of bone and brain metastases? Lung Cancer. 2014;84:86–91. doi: 10.1016/j.lungcan.2014.01.006. [DOI] [PubMed] [Google Scholar]
- 14.Scagliotti GV, Hirsh V, Siena S, Henry DH, Woll PJ, Manegold C, et al. Overall survival improvement in patients with lung cancer and bone metastases treated with denosumab versus zoledronic acid: subgroup analysis from a randomized phase 3 study. J Thorac Oncol. 2012;7:1823–9. doi: 10.1097/JTO.0b013e31826aec2b. [DOI] [PubMed] [Google Scholar]
- 15.Normanno N, Gullick WJ. Epidermal growth factor receptor tyrosine kinase inhibitors and bone metastases: different mechanisms of action for a novel therapeutic application? Endocr Relat Cancer. 2006;13:3–6. doi: 10.1677/erc.1.01185. [DOI] [PubMed] [Google Scholar]
- 16.Inomata M, Shukuya T, Takahashi T, Ono A, Nakamura Y, Tsuya A, et al. Continuous administration of EGFR-TKIs following radiotherapy after disease progression in bone lesions for non-small cell lung cancer. Anticancer Res. 2011;31:4519–23. [PubMed] [Google Scholar]
- 17.Nishino M, Dahlberg SE, Cardarella S, Jackman DM, Rabin MS, Ramaiya NH, et al. Volumetric tumor growth in advanced non-small cell lung cancer patients with EGFR mutations during EGFR-tyrosine kinase inhibitor therapy: developing criteria to continue therapy beyond RECIST progression. Cancer. 2013;119:3761–8. doi: 10.1002/cncr.28290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nishino M, Cardarella S, Dahlberg SE, Jackman DM, Ramaiya NH, Hatabu H, et al. Radiographic assessment and therapeutic decisions at RECIST progression in EGFR-mutant NSCLC treated with EGFR tyrosine kinase inhibitors. Lung Cancer. 2013;79:283–8. doi: 10.1016/j.lungcan.2012.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Asami K, Okuma T, Hirashima T, Kawahara M, Atagi S, Kawaguchi T, et al. Continued treatment with gefitinib beyond progressive disease benefits patients with activating EGFR mutations. Lung Cancer. 2013;79:276–82. doi: 10.1016/j.lungcan.2012.11.022. [DOI] [PubMed] [Google Scholar]
- 20.Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1) Eur J Cancer. 2009;45:228–47. doi: 10.1016/j.ejca.2008.10.026. [DOI] [PubMed] [Google Scholar]
- 21.Li W, Ren S, Li J, Li A, Fan L, Li X, et al. T790M mutation is associated with better efficacy of treatment beyond progression with EGFR-TKI in advanced NSCLC patients. Lung Cancer. 2014;84:295–300. doi: 10.1016/j.lungcan.2014.03.011. [DOI] [PubMed] [Google Scholar]
- 22.Arcila ME, Oxnard GR, Nafa K, Riely GJ, Solomon SB, Zakowski MF, et al. Rebiopsy of lung cancer patients with acquired resistance to EGFR inhibitors and enhanced detection of the T790M mutation using a locked nucleic acid-based assay. Clin Cancer Res. 2011;17:1169–80. doi: 10.1158/1078-0432.CCR-10-2277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Oxnard GR, Paweletz CP, Kuang Y, Mach SL, O'Connell A, Messineo MM, et al. Noninvasive detection of response and resistance in EGFR-mutant lung cancer using quantitative next-generation genotyping of cell-free plasma DNA. Clin Cancer Res. 2014;20:1698–705. doi: 10.1158/1078-0432.CCR-13-2482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang Z, Chen R, Wang S, Zhong J, Wu M, Zhao J, et al. Quantification and dynamic monitoring of EGFR T790M in plasma cell-free DNA by digital PCR for prognosis of EGFR-TKI treatment in advanced NSCLC. PLoS One. 2014;9: doi: 10.1371/journal.pone.0110780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lecouvet FE, Talbot JN, Messiou C, Bourguet P, Liu Y, de Souza NM, et al. Monitoring the response of bone metastases to treatment with Magnetic Resonance Imaging and nuclear medicine techniques: a review and position statement by the European Organisation for Research and Treatment of Cancer imaging group. Eur J Cancer. 2014;50:2519–31. doi: 10.1016/j.ejca.2014.07.002. [DOI] [PubMed] [Google Scholar]


