Abstract
Background
Normal left anterior descending (LAD) coronary artery as determined by coronary angiography is considered not only to reflect normal angiography but also to correlate with normal anatomy and function. However, subjects who undergo coronary angiography may differ from those who do not need to have invasive evaluation even if their functional noninvasive studies like dobutamine stress echocardiography (DSE) were normal.
Aim
LAD velocities in subjects with normal angiography and those with normal DSE are equal.
Methods
A total of 244 subjects were evaluated, 78 had normal LAD by angiography and 166 had normal LAD by DSE. All had Doppler sampling of LAD velocities by transthoracic echocardiography.
Results
Velocity was higher in the angiographic subgroup in diastole 41 ± 23 vs 33 ± 14 cm/s, p = 0.0078; systole 18 ± 14 vs 13 ± 7 cm/s, p = 0.012; diastolic integral 12.6 ± 5 vs 9.8 ± 3.8 cm, p = 3.15 × 10-5; systolic velocity integral 4 ± 2.9 vs 2.8 ± 1.9, p = 0.0014. While heart rate was similar in both groups, the product of diastolic velocity integral and heart rate of the LAD in the angiographic group was higher: 902 ± 450 vs 656 ± 394, p = 0.00599. Diastolic velocity deceleration time was similar in both groups. Coronary flow reserve defined as diastolic velocity ratio before and immediately after DSE correlated negatively with baseline velocity, r = -0.4.
Conclusions
Mode of defining normality of coronary artery affects velocity behavior of the vessel, reflecting functional differences possibly related to microvasculature and vasodilatation.
Keywords: Coronary angiography, Dobutamine stress echocardiography, Doppler, Left anterior descending coronary artery
Introduction
Coronary atherosclerosis is the most common disease in industrialized countries (1). Therefore, excluding or diagnosing coronary artery disease is of primary importance. Stress tests are frequently performed for the evaluation of coronary artery disease. Dobutamine stress echocardiography (DSE) is an established method for the assessment of coronary artery disease with a sensitivity and specificity of 80-85% (2, 3). Absence of ischemia according to DSE study is of prognostic importance and may be considered as an evidence for absence of the disease or alternatively as an evidence for normal coronary arteries. However, still many patients, for various reasons, reach the catheterization laboratory and are subsequently found to have normal coronary arteriograms (4).
Recent technologic advances in transthoracic echocardiography made Doppler sampling of coronary artery velocities possible (5-6-7-8-9-10). Sampling of coronary artery blood velocities may aid in the diagnosis or exclusion of coronary artery stenosis (11-12-13-14). Therefore, establishing the normal values of coronary artery blood velocity parameters is important. Moreover, since patients still reach the catheterization laboratory to find normal coronary arteries, we questioned whether the method of determining “normality” affects blood velocity in the coronary artery. The purpose of the present study was to determine the normal blood velocities in the left anterior descending (LAD) coronary artery in subjects with normal LAD according to DSE study compared to those with normal LAD according to coronary arteriographic study.
Materials and methods
Population
Two hundred forty-four subjects were evaluated for chest pain and suspected coronary artery disease. Seventy-eight of them were consecutive patients who had normal LAD by coronary angiography and who had Doppler sampling of LAD blood velocities and 166 consecutive patients had normal LAD territory by DSE. Subjects who had abnormal DSE in the LAD area were excluded from the study. Seventy-one patients had ischemia in non-LAD territories by DSE and the LAD was considered to be normal.
Dobutamine stress echocardiography
Siemens’ Acuson Sequoia echocardiographic system, California, equipped with 3.5-7 MHZ transducer was used. The protocol of dobutamine infusion consisted of 3-min stages for each dose, starting with 5 μg/kg/min and increasing to 10, 20, 30 and 40 μg/kg/min. If end-points did not occur or 85% of the age-adjusted heart rate was not achieved, 0.25 mg atropine was injected every 2 minutes up to 1 mg or until the target heart rate was achieved. Blood pressure and 12-lead electrocardiograms were recorded at rest and throughout the DSE study. Horizontal or downsloping >1 mm ST-segment depression at 0.06 s after the J point was considered as evidence for myocardial ischemia.
Sampling of LAD blood velocity
In order to obtain LAD velocities, the color Doppler Nyquist limit was set at 17 cm/s or power Doppler mode with peak velocity 16 cm/s (Fig. 1). Systematic attempts to record LAD color flow were performed. From the low parasternal short axis view, search for diastolic color velocity in the anterior interventricular groove followed by clockwise rotation to achieve alignment of the color jet was performed. Alternatively, from the apical foreshortened two-chamber view LAD diastolic velocity was located in the interventricular groove and counterclockwise rotation of the transducer was performed to optimize alignment with the color jet.
Fig 1 -.
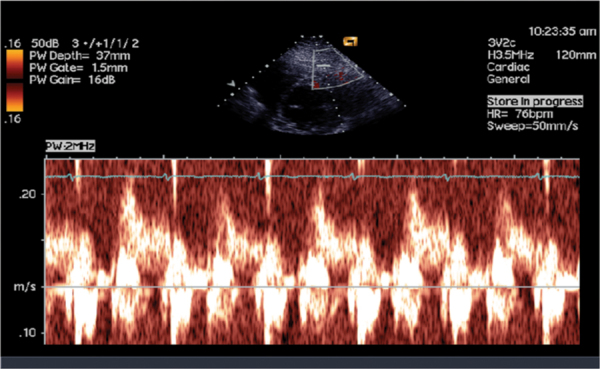
Pulsed Doppler of blood velocity through the left anterior descending coronary artery.
Measurements
Peak diastolic and systolic velocities and their ratios were obtained. In addition time velocity integrals in diastole and systole and their ratios were measured. Pressure half-time was obtained from the diastolic component of the LAD velocity profile. Measurements were averaged from three consecutive beats.
Coronary angiography
All subjects had coronary angiography within 24 hours of the echocardiographic evaluation using Siemens’ system, at 25 frames/s. Severity of stenosis was assessed using quantitative coronary angiography.
Statistical analysis
Mean and standard deviation of parameters were calculated. Comparisons between LAD flow parameters in patients with severe LAD stenosis and subjects with normal and nonsignificant LAD lesions were performed using independent sample Student’s t-test for continuous variables and Pearson’s χ2 test for categorical variables. Multiple regression analysis was performed to examine the effect of some patients’ characteristics (gender, age, heart rate before DSE and left ventricular wall motion score index (LVWMSI) after DSE) on LAD flow parameters. P<0.05 was considered statistically significant. All analyses were performed using SPSS 17.0 software package.
Results
Inter- and intra-observer variability of LAD velocities were 2 ± 0.4 and 1.5 ± 0.2 cm/s, of time velocity integrals 0.4 ± 0.1 and 0.3 ± 0.1 cm, of pressure half-time 10 ± 3 and 8 ± 3 ms and of the diameter of LAD color jet 0.1 ± 0.05 mm, respectively.
Atherosclerotic cardiovascular risk factors
Coronary arteriographic and DSE studies were performed safely in all subjects. No significant obstructive disease was found in the LAD and the vessel was considered to have normal luminogram in all. No ischemia was found in the LAD in all subjects having DSE studies. In Table I, the number of subjects in the DSE and coronary angiography groups are presented in parenthesis. No significant statistical difference was found in the prevalence of the screened atherosclerotic risk factor between the groups.
TABLE I -.
Prevalence in percent of atherosclerotic cardiovascular risk factors
| Arterial hypertension | Hyperlipidemia | Cigarette smoking | Obesity | Family history | Diabetes mellitus | |
|---|---|---|---|---|---|---|
| Angiography (n = 78) | 30.8 (24) | 26.9 (21) | 24.4 (19) | 14.1 (11) | 11.5 (9) | 8.9 (7) |
| Normal DSE (n = 166) | 25.9 (43) | 23.5 (39) | 23.5 (39) | 15.7 (26) | 10.2 (17) | 8.4 (14) |
Comparison of LAD blood velocity parameters according to study modality
As already mentioned all subjects were considered to have a normal LAD either by coronary artriographic or DSE studies. Table II summarizes the comparison between subjects according to study modality. Maximal diastolic and systolic velocities were significantly higher in subjects who had coronary arteriographic studies. Diastolic and systolic time velocity integrals were also significantly higher in the coronary arteriography group. While heart rate was similar in both groups, the product of heart rate and time velocity integrals, both the systolic and diastolic components, which correlate with flow, were significantly higher in subjects having coronary arteriographic studies.
TABLE II -.
LAD velocity parameters in angiographically normal and in subjects without LAD territory ischemia
| VD (cm/s) | VS (cm/s) | TVID (cm) | TVIS (cm) | HR (bpm) | TVID × HR (cm × bpm) | TVIS × HR (cm × bpm) | |
|---|---|---|---|---|---|---|---|
| HR = heart rate; TVID = diastolic time velocity integral; TVIS = systolic time velocity integral; VD = peak diastolic velocity; VS = peak systolic velocity. | |||||||
| Angiography (n = 78) | 41 ± 23 | 18 ± 14 | 12.6 ± 5 | 4 ± 2.9 | 72 ± 12 | 902 ± 450 | 284 ± 245 |
| Normal DSE (n = 166) | 33 ± 14 | 13 ± 7 | 9.8 ± 3.8 | 2.8 ± 1.9 | 75 ± 20 | 656 ± 394 | 178 ± 132 |
| P-value | 0.0078 | 0.012 | 3.15 × 10-5 | 0.0014 | 0.115 | 0.00599 | 0.0005 |
Gender effects on LAD blood velocity parameters
Women were slightly older than but had significantly higher heart rate. Nevertheless, the measured and calculated LAD blood velocities and velocity parameters were not affected by gender as summarized in Table III.
TABLE III -.
Gender effects
| Age (yrs) | HR (bpm) | VD (cm/s) | VS (cm/s) | VD/VS | TVID (cm) | TVIS (cm) | TVID/TVIS | DDT (ms) | P1/2T (ms) | |
|---|---|---|---|---|---|---|---|---|---|---|
| DDT = diastolic deceleration time; HR = heart rate; P1/2T = pressure half time; TVID = diastolic time velocity integral; TVIS = systolic time velocity integral; VD = peak diastolic velocity; VS = peak systolic velocity. | ||||||||||
| Males (n = 101) | 55.2 ± 10.4 | 72.7 ± 15.8 | 32.3 ± 15 | 13 ± 8 | 2.9 ± 1.8 | 9.7 ± 9.7 | 2.7 ± 1.9 | 4.7 ± 3 | 572.7 ± 219 | 177.8 ± 66 |
| Females (n = 65) | 58.6 ± 10.6 | 81.5 ± 22.6 | 35 ± 14 | 13.7 ± 6.5 | 2.9 ± 1.4 | 9.6 ± 3.6 | 3 ± 1.6 | 4 ± 2 | 631 ± 240.6 | 179.5 ± 67 |
| P-value | 0.06 | 0.005 | 0.28 | 0.59 | 0.85 | 0.89 | 0.4 | 0.08 | 0.16 | 0.88 |
Effects of remote ischemia on LAD blood velocity parameters
In Table IV, the effects of remote ischemia, indicated by LVWMSI more than 1, on LAD blood velocity parameters at rest are summarized. As seen no significant difference was found in any measured or calculated blood velocity parameter.
TABLE IV -.
LAD velocity and LAD flow parameters with and without non-LAD DSE ischemia
| VD (cm/s) | VS (cm/s) | HR (bmp) | TVID (cm) | TVIS (cm) | TVID × HR (cm × bpm) | TVIS × HR (cm × bpm) | |
|---|---|---|---|---|---|---|---|
| HR = heart rate; TVID = diastolic time velocity integral; TVIS = systolic time velocity integral; VD = peak diastolic velocity; VS = peak systolic velocity; WMSI = wall motion score index. | |||||||
| WMSI>1 (n = 71) | 34.5 ± 16 | 14 ± 7 | 73 ± 19 | 10 ± 3.7 | 2.8 ± 1.6 | 697 ± 439 | 186 ± 129 |
| WMSI = 1 (n = 95) | 32 ± 11.5 | 12 ± 6 | 77.5 ± 21 | 9 ± 3.3 | 2.6 ± 1.6 | 661 ± 330 | 182 ± 130 |
| P-value | 0.2 | 0.08 | 0.115 | 0.06 | 0.33 | 0.58 | 0.88 |
LAD flow parameters and patient characteristics
As detailed in Table V, gender did not affect LAD velocity parameters. Age had some effect on TVIS at rest. Peak diastolic and systolic LAD blood velocity at rest, DDT, PHT, TVID × HR and TVIS × HR were affected by HR at rest before DSE (Tab. V). LVWMSI after DSE had some significant effect on TVID × HR.
TABLE V -.
Multiple regression analysis (Pearson correlations) against flow parameters before DSE
| Parameter Characteristic | Flow | VD (cm/s) | VS (cm/s) | TVID (cm) | TVIS (cm) | DDT (ms) | P1/2T (ms) | TVID × HR (cm × bpm) | TVIS × HR (cm × bpm) |
|---|---|---|---|---|---|---|---|---|---|
| Flow parameters = the parameters before DSE. | |||||||||
| DDT = diastolic deceleration time; HR = heart rate; P1/2T = pressure half time; TVID = diastolic time velocity integral; TVIS = systolic time velocity integral; VD = peak diastolic velocity; VS = peak systolic velocity. | |||||||||
| Gender | 0.004 | 0.081 | 0.078 | 0.114 | 0.156 | 0.054 | -0.022 | 0.056 | |
| Age | 0.182 | 0.214 | 0.209 | 0.285 (p = 0.002) | -0.8 | -0.041 | 0.173 | 0.0.27 | |
| HRbefore DSE | 0.421 (p<.001) | 0.189 (p = 0.017) | -0.003 | -0.057 | -0.413 (p<0.001) | -0.438 (p<0.001) | 0.543 (p<0.001) | 0.366 (p<0.001) | |
| LVWMSIpost DSE | 0.151 | 0.159 | 0.199 | 0.076 | 0.051 | 0.057 | 0.173 (p = .024) | 0.074 | |
| R (all independent variables) | 0.472 | 0.317 | 0.262 | 0.298 | 0.441 | 0.444 | 0.587 | 0.298 | |
| F P-value | 9.594 <0.001 | 3.703 0.007 | 2.425 0.051 | 3.237 0.014 | 6.643 <0.001 | 7.970 <0.001 | 17.442 <0.001 | 8.514 <0.001 | |
Discussion
In this study, the normal LAD velocity parameters were determined by two subgroups: a) subjects with normal coronary luminograms by coronary angiography, and b) subjects without ischemia in the territory of the LAD by DSE studies. Blood velocities and velocity parameters were significantly higher in those with non-obstructive coronary angiograms compared to those with non-ischemia LAD area with DSE. Thus, the behavior of blood velocity in the normal coronary artery is affected by the mode of defining normality, reflecting functional differences possibly related to microvasculature and vasodilatation.
Coronary blood flow has a distinctive biphasic pattern, with a predominant diastolic component (15). In the absence of coronary artery stenosis, the normal LAD velocity profile is predominantly diastolic and does not reveal a significant velocity gradient or change in velocity pattern along the coronary artery (16-17-18-19). Normal peak diastolic velocities in the present study were similar to those reported previously by invasive Doppler flowires (17). Furthermore, the ratio of diastolic to systolic velocities in subjects without significant LAD stenosis was similar to those reported previously by invasive methods (17).
Despite attempts to improve patient selection, the rate of normal coronary angiography in patients undergoing evaluation for coronary artery disease is 10-20% (20). Normal coronary angiography in subjects with chest pain is five times more common in women than in men (21). A normal coronary angiogram is defined as absence of visible luminal irregularities. The prognosis in these patients is good, although they may continue to suffer from chest pain and may develop cardiac events (22). However, there is evidence of endothelial coronary artery dysfunction in these patients with normal coronary angiograms (23). Moreover, it was shown that patients without focal stenosis on angiography may have diffuse atherosclerosis and exhibit continuous pressure drop along the arterial length with increased resistance to coronary flow which may contribute to ischemia (24). Thus, a normal coronary angiogram does not necessarily mean a normal coronary artery, and our findings of higher LAD velocities and velocity parameters may be explained by coronary arterial dysfunction.
Since stress echocardiography is specific for coronary artery disease, a normal coronary artery is defined when no regional stress-induced regional LV dysfunction is observed. Extent, location and threshold of myocardial ischemia are predictive of outcome (25). An ischemia-positive stress echocardiogram was reported in 9.4% of patients having nonsignificant coronary artery disease on coronary angiography (26). Patients with ischemia by stress echocardiography accounted for 21% of mortality during 7 years’ follow-up and test positivity for ischemia was an independent predictor of mortality. These results confirm the findings of a previous study, showing that women with chest pain in the absence of coronary stenosis had myocardial ischemia with magnetic resonance spectroscopy, and this finding was predictive of subsequent admissions and cost (27). Thus, it seems that coronary artery blood velocities in the absence of myocardial ischemia by stress echocardiographic studies reflect the normal situation more than coronary velocities in subjects with normal coronary luminogram.
Are all the subjects with negative stress echocardiographic studies for myocardial ischemia the same? According to the findings of our study, gender did not affect blood velocity or velocity parameters despite higher heart rates in women. In addition, the presence of remote ischemia did not affect these parameters at rest. Thus, apparently, absence of myocardial ischemia defines a normal coronary artery. However, in a previous study, it was shown that patients with remote ischemia had lower coronary flow reserve compared to subjects without ischemia (28). Therefore, absence of ischemia on stress echocardiography defines a normal coronary artery when confounding conditions associated with vasodilatation of the distal coronary bed and hyperemia are absent.
Limitations
Normal coronary arteries may be defined as those without atherosclerosis. In this study presence or absence of coronary artery atherosclerosis was evaluated only in 78 patients and only by coronary angiography. Intra-coronary ultrasound is most adequate to evaluate coronary atherosclerosis. Alternatively, coronary atheromata may be evaluated by computed tomography. Future studies investigating the Doppler findings in subjects evaluated by intracoronary ultrasound or computed tomography may be helpful. In addition, evaluation of coronary flow reserve as already mentioned may be adequate.
Conclusions
Doppler velocities of the LAD in subjects having normal coronary arteries were higher than those with normal dobutamine stress echocardiographic studies. Thus, normal coronary arteries may differ functionally, and the mode of defining normality affects velocity behavior of the vessel, reflecting functional differences possibly related to microvasculature and vasodilatation.
Disclosures
Financial support: No grants or funding have been received for this study.
Conflict of interest: None.
References
- 1.Hansson GK. Inflammation, atherosclerosis, and coronary artery disease. N Engl J Med. 2005;352(16):1685–1695. doi: 10.1056/NEJMra043430. [DOI] [PubMed] [Google Scholar]
- 2.Geleijnse ML, Fioretti PM, Roelandt JR. Methodology, feasibility, safety and diagnostic accuracy of dobutamine stress echocardiography. J Am Coll Cardiol. 1997;30(3):595–606. doi: 10.1016/s0735-1097(97)00206-4. [DOI] [PubMed] [Google Scholar]
- 3.Picano E. Stress echocardiography: a historical perspective. Am J Med. 2003;114(2):126–130. doi: 10.1016/s0002-9343(02)01427-4. [DOI] [PubMed] [Google Scholar]
- 4.Patel MR, Peterson ED, Dai D et al. Low diagnostic yield of elective coronary angiography. N Engl J Med. 2010;362(10):886–895. doi: 10.1056/NEJMoa0907272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Voci P, Testa G, Plaustro G. Imaging of the distal left anterior descending coronary artery by transthoracic color-Doppler echocardiography. Am J Cardiol. 1998;81(12 12A):74G–78G. doi: 10.1016/s0002-9149(98)00058-7. [DOI] [PubMed] [Google Scholar]
- 6.Caiati C, Montaldo C, Zedda N, Bina A, Iliceto S. New noninvasive method for coronary flow reserve assessment: contrast-enhanced transthoracic second harmonic echo Doppler. Circulation. 1999;99(6):771–778. doi: 10.1161/01.cir.99.6.771. [DOI] [PubMed] [Google Scholar]
- 7.Hildick-Smith DJ, Shapiro LM. Coronary flow reserve improves after aortic valve replacement for aortic stenosis: an adenosine transthoracic echocardiography study. J Am Coll Cardiol. 2000;36(6):1889–1896. doi: 10.1016/s0735-1097(00)00947-5. [DOI] [PubMed] [Google Scholar]
- 8.Higashiue S, Watanabe H, Yokoi Y, Takeuchi K, Yoshikawa J. Simple detection of severe coronary stenosis using transthoracic Doppler echocardiography at rest. Am J Cardiol. 2001;87(9):1064–1068. doi: 10.1016/s0002-9149(01)01462-x. [DOI] [PubMed] [Google Scholar]
- 9.Pizzuto F, Voci P, Mariano E, Puddu PE, Sardella G, Nigri A. Assessment of flow velocity reserve by transthoracic Doppler echocardiography and venous adenosine infusion before and after left anterior descending coronary artery stenting. J Am Coll Cardiol. 2001;38(1):155–162. doi: 10.1016/s0735-1097(01)01333-x. [DOI] [PubMed] [Google Scholar]
- 10.Takeuchi M, Miyazaki C, Yoshitani H, Otani S, Sakamoto K, Yoshikawa J. Assessment of coronary flow velocity with transthoracic Doppler echocardiography during dobutamine stress echocardiography. J Am Coll Cardiol. 2001;38(1):117–123. doi: 10.1016/s0735-1097(01)01322-5. [DOI] [PubMed] [Google Scholar]
- 11.Sharif D, Sharif-Rasslan A, Shahla C, Abinader EG. Detection of severe left anterior descending coronary artery stenosis by transthoracic evaluation of resting coronary flow velocity dynamics. Heart Int. 2010;5(2):e10. doi: 10.4081/hi.2010.e10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ofili EO, Kern MJ, Labovitz AJ et al. Analysis of coronary blood flow velocity dynamics in angiographically normal and stenosed arteries before and after endolumen enlargement by angioplasty. J Am Coll Cardiol. 1993;21(2):308–316. doi: 10.1016/0735-1097(93)90668-q. [DOI] [PubMed] [Google Scholar]
- 13.Hozumi T, Yoshida K, Akasaka T et al. Value of acceleration flow and the prestenotic to stenotic coronary flow velocity ratio by transthoracic color Doppler echocardiography in noninvasive diagnosis of restenosis after percutaneous transluminal coronary angioplasty. J Am Coll Cardiol. 2000;35(1):164–168. doi: 10.1016/s0735-1097(99)00501-x. [DOI] [PubMed] [Google Scholar]
- 14.Saraste M, Vesalainen RK, Ylitalo A et al. Transthoracic Doppler echocardiography as a noninvasive tool to assess coronary artery stenoses—a comparison with quantitative coronary angiography. J Am Soc Echocardiogr. 2005;18(6):679–685. doi: 10.1016/j.echo.2004.09.016. [DOI] [PubMed] [Google Scholar]
- 15.Takeuchi M, Miyazaki C, Yoshitani H, Otani S, Sakamoto K, Yoshikawa J. Assessment of coronary flow velocity with transthoracic Doppler echocardiography during dobutamine stress echocardiography. J Am Coll Cardiol. 2001;38(1):117–123. doi: 10.1016/s0735-1097(01)01322-5. [DOI] [PubMed] [Google Scholar]
- 16.Ofili EO, Kern MJ, Labovitz AJ et al. Analysis of coronary blood flow velocity dynamics in angiographically normal and stenosed arteries before and after endolumen enlargement by angioplasty. J Am Coll Cardiol. 1993;21(2):308–316. doi: 10.1016/0735-1097(93)90668-q. [DOI] [PubMed] [Google Scholar]
- 17.Ofili EO, Labovitz AJ, Kern MJ. Coronary flow velocity dynamics in normal and diseased arteries. Am J Cardiol. 1993;71(14):3D–9D. doi: 10.1016/0002-9149(93)90128-y. [DOI] [PubMed] [Google Scholar]
- 18.Kern MJ, Donohue TJ, Aguirre FV et al. Assessment of angiographically intermediate coronary artery stenosis using the Doppler flowire. Am J Cardiol. 1993;71(14):26D–33D. doi: 10.1016/0002-9149(93)90131-u. [DOI] [PubMed] [Google Scholar]
- 19.Kern MJ. Braunwald’s Heart Disease—A textbook of cardiovascular medicine. Philadelphia: Elsevier Saunders; Coronary blood flow and myocardial ischemia. In: Zipes DP, Libby P, Bonow RO, Braunwald E., eds. 2005; 1103. [Google Scholar]
- 20.Jong P, Mohammed S, Sternberg L. Sex differences in the features of coronary artery disease of patients undergoing coronary angiography. Can J Cardiol. 1996;12(7):671–677. [PubMed] [Google Scholar]
- 21.Sullivan AK, Holdright DR, Wright CA, Sparrow JL, Cunningham D, Fox KM. Chest pain in women: clinical, investigative, and prognostic features. BMJ. 1994;308(6933):883–886. doi: 10.1136/bmj.308.6933.883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kaski JC. Pathophysiology and management of patients with chest pain and normal coronary arteriograms (cardiac syndrome X). Circulation. 2004;109(5):568–572. doi: 10.1161/01.CIR.0000116601.58103.62. [DOI] [PubMed] [Google Scholar]
- 23.Werns SW, Walton JA, Hsia HH, Nabel EG, Sanz ML, Pitt B. Evidence of endothelial dysfunction in angiographically normal coronary arteries of patients with coronary artery disease. Circulation. 1989;79(2):287–291. doi: 10.1161/01.cir.79.2.287. [DOI] [PubMed] [Google Scholar]
- 24.De Bruyne B, Hersbach F, Pijls NH et al. Abnormal epicardial coronary resistance in patients with diffuse atherosclerosis but “normal” coronary angiography. Circulation. 2001;104(20):2401–2406. doi: 10.1161/hc4501.099316. [DOI] [PubMed] [Google Scholar]
- 25.Poldermans D, Arnese M, Fioretti PM et al. Improved cardiac risk stratification in major vascular surgery with dobutamine-atropine stress echocardiography. J Am Coll Cardiol. 1995;26(3):648–653. doi: 10.1016/0735-1097(95)00240-5. [DOI] [PubMed] [Google Scholar]
- 26.Sicari R, Palinkas A, Pasanisi EG, Venneri L, Picano E. Long-term survival of patients with chest pain syndrome and angiographically normal or near-normal coronary arteries: the additional prognostic value of dipyridamole echocardiography test (DET). Eur Heart J. 2005;26(20):2136–2141. doi: 10.1093/eurheartj/ehi408. [DOI] [PubMed] [Google Scholar]
- 27.Buchthal SD, den Hollander JA, Merz CN et al. Abnormal myocardial phosphorus-31 nuclear magnetic resonance spectroscopy in women with chest pain but normal coronary angiograms. N Engl J Med. 2000;342(12):829–835. doi: 10.1056/NEJM200003233421201. [DOI] [PubMed] [Google Scholar]
- 28.Sharif D, Sharif-Rasslan A, Shahla C et al. Coronary flow reserve of the non-ischemia related coronary artery. Cardiol Rev. 2011;2(4):174–180. doi: 10.4021/cr57w. [DOI] [PMC free article] [PubMed] [Google Scholar]


