Supplemental digital content is available in the text.
Background
Hispanic Americans face disparities in access to kidney transplantation, particularly living donor kidney transplantation (LDKT). This study compared characteristics of LDKT recipients before and after implementing the Hispanic Kidney Transplant Program (HKTP) at Northwestern Medicines (NM) and other centers.
Methods
The NM HKTP, initiated in December 2006, delivers culturally and linguistically competent and congruent care. Program-specific data were used to compare the mean ratios of Hispanic to non-Hispanic white LDKTs between pre-HKTP (2001-2006) and post-HKTP (2008-2013), and to compare the characteristics of NM's adult LDKT patients between pre-HKTP and post-HKTP. The same ratio was calculated for transplant centers in regions with a significant Hispanic population (≥25%) and performing in the top tertile of total LDKT volume in the pre-HKTP period. The number of Hispanic and non-Hispanic white patients added to the waiting list were compared between pre-HKTP (2001-2006) and post-HKTP (2008-2013) as a proxy for increased patient referrals and a pathway by which the HKTP may increase LDKTs.
Results
The ratio of Hispanic to non-Hispanic white LDKTs significantly increased by 70% after the implementation of NM's HKTP (pre-HKTP mean = 0.20, post-HKTP mean = 0.34; P= 0.001). None of the other transplant centers experienced a similar increase in their ratio of Hispanic to non-Hispanic white LDKTs. The NM waiting list additions grew by 91% among Hispanics, but grew only 4% for non-Hispanic whites.
Conclusions
These data suggest that the development and implementation of a culturally congruent transplant program can positively affect Hispanic LDKT and thereby reduce Hispanics disparities in LDKT rates. Further studies are needed to prospectively evaluate the generalizability of implementing such culturally competent interventions at other transplant programs.
Hispanics have a disproportionately higher prevalence of end-stage renal disease (ESRD)1 than non-Hispanic whites, resulting in a greater need for kidney transplantation.2 Living donor kidney transplantation (LDKT) is promoted as the best treatment for ESRD because LDKT provides longer graft and patient survival, shorter waiting time, and better quality of life than deceased donor kidney transplantation (DDKT).3,4 However, compared to non-Hispanic whites, disproportionately fewer waitlisted Hispanics received a LDKT in 2014 (4% vs 10%).5 The disparity in LDKT rates will likely increase without intervention as Hispanics are the largest and fastest growing minority group in the United States and have a high prevalence of risk factors for ESRD (e.g., diabetes and hypertension), leading to a greater need for kidney transplantation.6
By “Hispanics,” we refer to a heterogeneous ethnic group in the United States that shares a common language and a pattern of cultural and religious beliefs and values passed down through generations.7,8 Hispanics, as an ethnic group, include diverse subgroups, including Hispanics of Mexican, Puerto Rican, Cuban, Spanish, South and Central American, and other Spanish-speaking countries. Although the preferred use of terms “Hispanic” or “Latino” varies,9,10 in our previous research, we found that both terms used together were preferred, thus, “Hispanic” is used as a proxy for both hereforth.9
Relatively lower living kidney donation (LKD) rates in Hispanics and other ethnic minority groups have been attributed to patient-, provider-, and health care system–related factors.11
Hispanic-specific donor factors include: fear of women not being able to bear children or of men becoming impotent after LKD, concerns that LKD would shorten the donor's life expectancy or require lifelong medication taking,12,13 language barriers,13 legal documentation issues, and preferences for face-to-face, group educational delivery modes.12-15 Moreover, Hispanic transplant candidates believe that few family members could be living donors and are unlikely to ask others to donate.12 In our earlier clinical experience (JCC), Hispanic patients were reluctant to identify and bring potential living donors with them to the transplant education session. Concerns about LDKT that Hispanics share with other minority groups include: lack of knowledge about LKD,13,16-18 fear of surgery,12,17,18 financial concerns,13,17,19 and distrust of the medical establishment.15,17,18 Provider factors include lack of Hispanic health care providers, low rates of preemptive transplantation, and of referral for transplantation.11,20 Health care system factors include the absence of language or literacy-appropriate educational materials.11 Hispanic dialysis patients have reported that dialysis centers provide little information about transplantation or living donation in Spanish.13 The cultural foundations of many of these factors suggest the need for culturally competent education about LKD for Hispanic patients with ESRD, families, and potential living kidney donors.
Culturally competent interventions have been shown to reduce health disparities in transplant and other clinical contexts. Cultural competency refers to: “A set of values, principles, behaviors, attitudes, policies, and structures that enable organizations and individuals to work effectively in cross-cultural situations.”21 Cultural competency includes cultural congruence, when patients and providers share a common ethnic heritage and cultural values,22 and linguistic congruence (e.g., bilingual/bicultural staff).23
Culturally competent interventions can increase LDKT rates.18,24-27 Most interventions focus on African Americans.26-28 Less common are interventions focusing on Hispanics' and their sociocultural concerns,18 such as increasing awareness of LKD as a treatment option,18,24 and willingness to be a LKD through mass media campaigns.18 Two system-based programs delivered in patients' homes have been developed29; the US program was targeted to African Americans.25
Transplant centers are an optimal venue for delivering interventions to increase LDKT rates because they reach patients and their family members who may be key decision makers (e.g., elders), attending transplant education sessions. Including the patient's family in education sessions can facilitate communication about LDKT within the family and with providers.30 To our knowledge, no previous studies have assessed the effectiveness of culturally competent transplant center-based interventions to increase Hispanic LDKT rates. Although many centers provide materials in Spanish,31 there are no published accounts of other comprehensive transplant programs that are tailored to address Hispanics' cultural concerns. The purpose of this study was to assess whether the implementation of a culturally and linguistically competent Hispanic Kidney Transplant Program (HKTP) is associated with increased Hispanic LDKT rates at a single center.
MATERIALS AND METHODS
Setting
Development
Northwestern Medicine (NM) and the Division of Organ Transplantation initiated the HKTP in December 2006 to serve the growing Hispanic population in Chicago and Illinois. The NM HKTP was implemented under the leadership of the Colombian-born Hispanic transplant surgeon, Dr. Juan Carlos Caicedo, in an attempt to increase LKD and kidney transplantation in Hispanics and to reduce the disparity in LDKT among Hispanics. The HKTP was developed based on Dr. Caicedo's Hispanic cultural knowledge and experience in treating the Hispanic patient population.
The HKTP was originally adapted from the English-speaking program. No resources were diverted from the English-speaking program to the HKTP. Rather, a Hispanic social worker was hired and existing Hispanic staff efforts were redirected toward the HKTP within the NM Division of Organ Transplantation. Aside from the HKTP, there were no other major NM programmatic changes in transplantation between 2007 and present. Approximately 75% of Hispanic patients elect to attend the HKTP and about 25% attend the English-speaking program; many patients in the English-speaking program come to interact with Dr. Caicedo because their family members cannot speak English.
Culturally and Linguistically Competent Care
The NM HKTP is culturally competent in its “surface” (superficial) and “deep” structures32 by using Spanish in all interactions and written materials, employing bilingual and bicultural staff, and addressing deep-seated cultural values, beliefs, and information needs of Hispanic kidney patients, their family members, and potential donors in education sessions, as previously described.14 The HKTP places great emphasis on family involvement in the education and evaluation processes given Hispanic cultural value of family in treatment decision making.33 Accordingly, the HKTP's features align well with the National Quality Forum's Framework for Standardizing Measurement and Reporting of High-Quality, Culturally Competent Care,34 as previously described.14
HKTP's Core Features
(A) Integration into Management Systems and Operations: Many people of Hispanic origin (especially those born in the United States) are native speakers of English and may prefer to receive treatment in English.35 Thus, the HKTP asks patients to identify their preference to receive their evaluation in Spanish (HKTP) or English (Standard Program) when scheduling the first visit. Unlike the Standard Program, the HKTP clinical coordinators encourage patients to bring “family members” to the first visit, rather than asking patients to bring along potential “living donors.” The HKTP has found that asking patients to bring “living donors” can reduce their willingness to participate and result in patients not asking their family to donate, which has been observed elsewhere.17,19,30 Further, Hispanic family members often do not realize their potential eligibility to donate, given a lack of knowledge and cultural concerns about LKD and transplantation. Thus, the HKTP, by inviting family members in the education sessions, aims to enhance knowledge about transplantation and donation throughout the family, which increases family members' consideration of becoming a living donor, and plays an important role in moving along treatment decisions because Hispanic family elders (e.g., the grandmother) often influence and guide these decisions.36
(B) Patient-Provider Communication: Before HKTP implementation, the required education sessions were in English only; Spanish-speaking patients were provided with an interpreter. After HKTP implementation, the education sessions were conducted in both the English and Spanish programs and consistently discuss deceased donor waiting times. The educational session content addresses many of the aforementioned Hispanic cultural beliefs and misconceptions about LDKT and transplantation.14
The HKTP delivers two sequential educational sessions in a face-to-face group discussion format in Spanish as the first phase of kidney transplant (KT) and live donor evaluation. The Spanish-speaking Hispanic staff and faculty clinically evaluate patients after the education sessions. The first educational session is delivered to potential recipients, family, and potential donors, and covers general procedures, risks, and benefits in, and cultural misconceptions about kidney transplantation and organ donation. The second information session is delivered to family and potential donors while patients undergo evaluation, and covers specific aspects of the LKD evaluation process. This session reinforces information covered in the first session while providing more details about who can be a donor and acknowledging potential fears with donation, particularly fears generated by the lack of knowledge about transplantation and donation. Additionally, this session discusses the low donation rate among Hispanics and dispels cultural misconceptions about living donation, for example, that people will become disabled, will need lifelong medications, will be unable to work or exercise, and will be unable to have children if they donate.
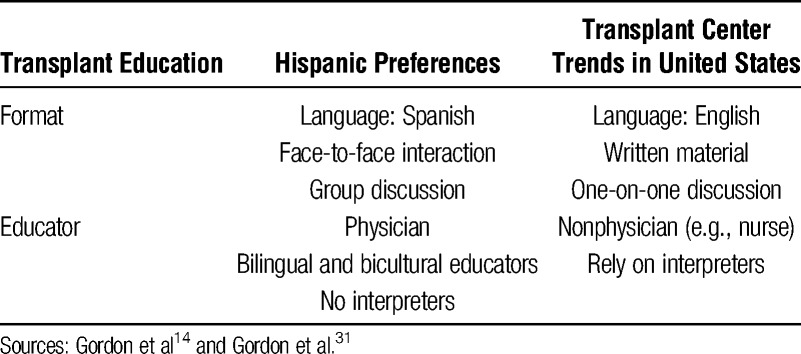
Our evaluation of knowledge gains by HKTP patients and family members from exposure to the education sessions confirms Hispanic preferences for the HKTP's interactive group sessions led by a transplant physician (Table 1).14 In the HKTP, education is provided by a transplant physician given the cultural understanding that many Hispanics feel more comfortable establishing trust with a physician, who is in a traditional position of authority, rather than by another health provider.37 By contrast, our national survey of transplant administrators found that most centers relied on education delivered in English by nonphysicians, with a reliance on written materials.31
TABLE 1.
Hispanic preferences about transplant education and U.S. trends
(C) Community Engagement: The HKTP invests in community engagement of dialysis centers and referring physicians to recruit patients to the HKTP. Specifically, the bilingual Hispanic social worker visits 3 to 4 dialysis centers with large Hispanic patient populations per month, as NM has done with English-speaking patients since 2000. The social worker sets up a booth in the dialysis center lobby to inform Hispanic dialysis patients in Spanish about transplant as an option, addresses concerns, and invites them to the HKTP for evaluation. To facilitate patients' access to the NM HKTP, when patients express interest in transplantation, the social worker immediately obtains their contact information and enters a note in the transplant database. This triggers an email to the clinical coordinator to call the patient to schedule an appointment. Additionally, the HKTP director updates patients' referring physicians by telephone or letter (e.g., at evaluation, after transplantation). The referring physician network includes many primary care providers (PCPs), as Hispanics are often cared for by PCPs rather than nephrologists, perhaps due to the fact that many PCPs speak Spanish. To further engage the Hispanic community, the NM transplant center's website has been translated into Spanish, and Dr. Caicedo provides periodic community education through mass media including public service announcements and interviews broadcast on Hispanic-specific television, radio, and newspapers.
Statistical Analysis
The Organ Procurement and Transplant Network/United Network for Organ Sharing (UNOS) provided data on patient demographics, additions to the waiting list as a proxy for patient referrals, and the ratio of Hispanic to non-Hispanic white LDKTs38 between pre- (2001-2006) and post-HKTP (2008-2013). Data from 2007 were excluded from the main analysis as the HKTP was still in the process of implementation. The ratio of Hispanic to non-Hispanic white LDKTs ([Hispanic LDKT/Total LDKT]/[non-Hispanic white LDKT/Total LDKT]) was used to account for overall growth in transplant center LDKT volume while also providing a comparison to non-Hispanic whites to assess potential disparities in care.
Individual characteristics of NM's adult Hispanic and non-Hispanic white LDKT recipients, pre-HKTP (2001-2006) and post-HKTP (2008-2013), were summarized as percentages and means with standard deviations (SD). χ2 tests were used to compare the pre-HKTP to post-HKTP individual characteristics. The t tests were used to compare the ratio of Hispanic to non-Hispanic white LDKTs and the additions to the waiting list between pre-HKTP and post-HKTP. For the ratio of Hispanic to non-Hispanic white LDKTs, annual ratios were computed and then compared with mean ratios between pre-HKTP and post-HKTP using t tests.
The NM LDKT data were compared to 29 transplant centers, located in regions with a significant Hispanic population (≥25%),39 and performing in the top tertile of adult LDKT volume between 2001 and 2013, except 2007. These transplant centers are in UNOS regions 1, 2, 3, 4, 5, 7, 8, and 9 which will heretofore be referred to as “comparison UNOS regions.” Centers in the top tertile of LDKTs were selected as a proxy measure for the capacity to increase the number of LDKTs, as a result of any new program, such as the HKTP. The LDKT data for NM were also compared with select Illinois transplant centers performing at least 5 adult LDKTs in the same time period to control for regional variation.
To assess whether the HKTP also affected Hispanic DDKTs, the ratio of Hispanic to non-Hispanic white DDKTs at NM was calculated and the ratios between pre-HKTP and post-HKTP were compared, using a t test.
Several sensitivity analyses were performed to determine if factors other than implementation of the HKTP might confound the results. The χ2 test for change in proportion of Hispanic LDKTs in transplant centers listed in Table 2 was performed to compare pre-HKTP and post-HKTP and to put equal weight to each transplant rather than to each year. Characteristics of Hispanic and non-Hispanic white KT recipients in comparison UNOS regions, excluding NM (which represent all transplant centers described in Table 2), were examined pre-HKTP and post-HKTP, using χ2 and t tests. Additionally, data from 2007 were included in the post-HKTP period and the change in ratios of African American LDKTs to non-Hispanic white LDKTs pre-HKTP and post-HKTP was calculated to assess whether the HKTP resulted in an increase in LDKT among Hispanics only or also among other ethnic/racial groups.
TABLE 2.
Ratio of Hispanic to non-Hispanic white living donor kidney transplants by transplant center*

All analyses were performed using SAS software version 9.4 (Cary, NC). A P value less than 0.05 was considered statistically significant. Northwestern University's Institutional Review Board deemed the study exempt because public use and deidentified datasets were used. The clinical and research activities being reported are consistent with the Principles of the Declaration of Istanbul as outlined in the “Declaration of Istanbul on Organ Trafficking and Transplant Tourism.”
RESULTS
Candidate Additions to the KT Waiting List: HKTP versus UNOS Regions
NM waiting list additions pre-HKTP compared to post-HKTP periods grew by 91% from 277 to 529 among Hispanics, but grew by only 4% (1426 to 1485) among non-Hispanic whites. Within UNOS region 7 (excluding NM), the growth was 32% (985 to 1,311) among Hispanics, and 39% (7,544 to 10,497) among non-Hispanic whites (Table S1, SDC, http://links.lww.com/TXD/A9).
Hispanic KT Recipients: HKTP versus Comparison UNOS Regions
At NM, the number of Hispanic KT recipients increased by 70.0% from 150 (pre-HKTP) to 255 (post-HKTP), whereas the number of non-Hispanic white KT recipients increased by 5.0% from 754 (pre-HKTP) to 792 (post-HKTP) (Table S2, SDC, http://links.lww.com/TXD/A9). In the comparison UNOS regions, the number of Hispanic KT recipients increased by 25.2% from 1162 (pre-HKTP) to 12,727 (post-HKTP), whereas the number of non-Hispanic white KT recipients decreased by 3.3% from 35,645 to 34,462 (Table S2, SDC, http://links.lww.com/TXD/A9). Nationally, the number of Hispanic KT recipients increased by 25.5% from 11,220 (pre-HKTP) to 14,078 (post-HKTP), whereas the number of non-Hispanic white KT recipients decreased by 1.3% from 50,881 to 50,211 (Table S2, SDC, http://links.lww.com/TXD/A9).
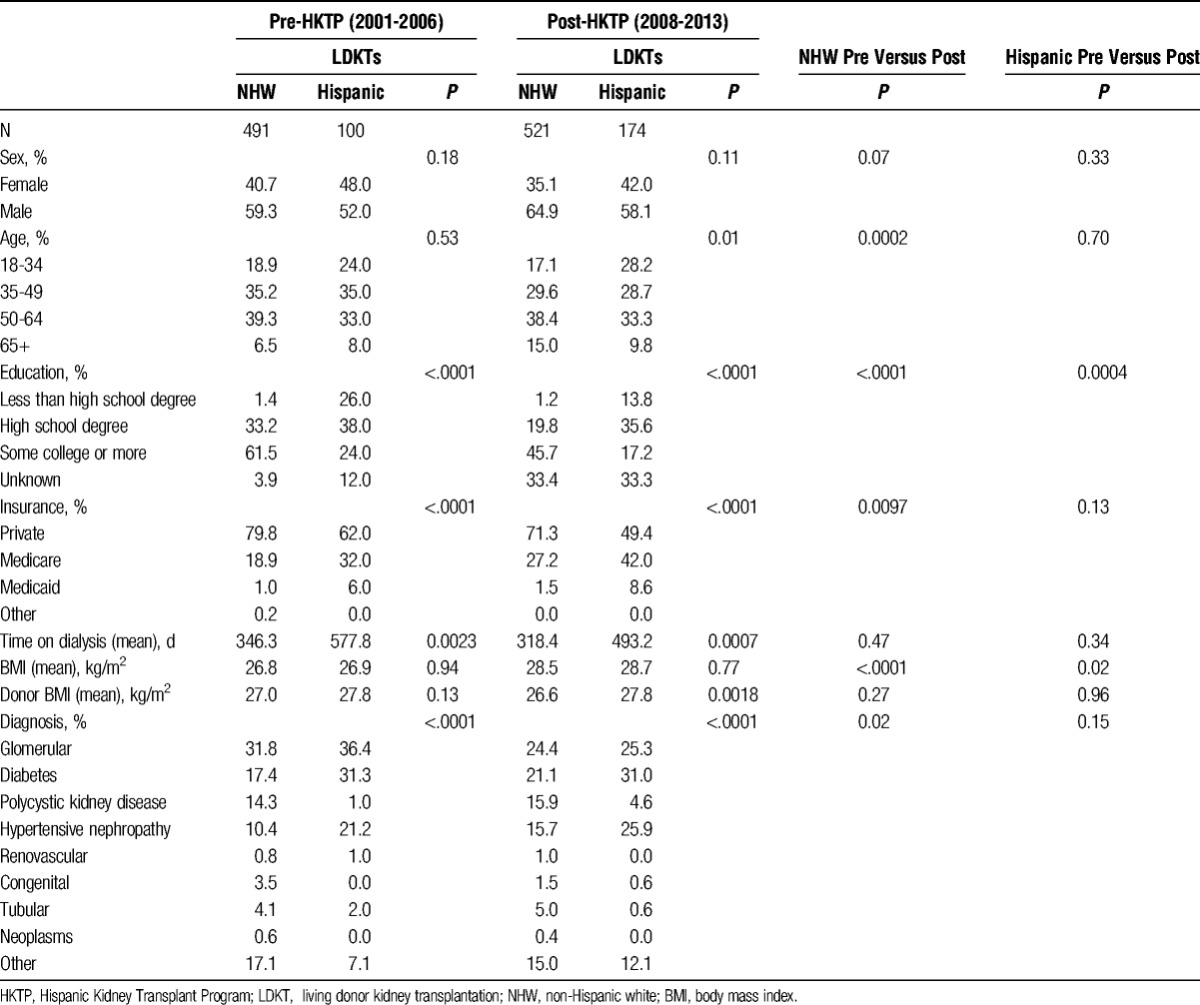
LDKT Recipient Demographics: HKTP Versus Comparison UNOS Regions
At NM, the number of Hispanics receiving LDKTs increased by 74% from 100 (pre-HKTP) to 174 (post-HKTP) (Table 3). By contrast, the number of non-Hispanic whites receiving a LDKT increased by 6.1% from 491 (pre-HKTP) to 521 (post-HKTP). Notably, the number of Hispanic LDKT recipients in the comparison UNOS regions decreased in most of the comparison UNOS regions (2, 5, 6, 7{excluding NM}, 9, 10) with the exception of region 4, which increased by 69% (Table S3, SDC, http://links.lww.com/TXD/A9). Demographic changes within and across pre-HKTP and post-HKTP periods at NM were comparable to changes in the comparison UNOS regions (Table S4, SDC, http://links.lww.com/TXD/A9).
TABLE 3.
Patient-level living donor kidney transplant characteristics at Northwestern Medicine*
LDKT Number and Ratio: HKTP Versus Other Transplant Centers
At NM, the number of Hispanic LDKTs performed grew by 74% from 100 (pre-HKTP) to 174 (post-HKTP). The mean annual ratio of Hispanic to non-Hispanic white LDKTs significantly increased by 70% post-HKTP (pre-HKTP mean = 0.20, post-HKTP mean = 0.34; P = 0.001) (Table 2). This translates to 1 Hispanic for every 5 non-Hispanic whites receiving a LDKT during the pre-HKTP period, whereas 1 Hispanic for every 3 non-Hispanic whites receiving a LDKT in the post-HKTP period.
Note that the mean annual number of non-Hispanic white LDKTs remained stable from pre- to post-HKTP (pre = 82, post = 87; P = 0.32). The increase in Hispanic LDKTs did not appear to occur at the expense of non-Hispanic white LDKTs.
None of the other 29 US transplant centers in the comparison UNOS regions experienced significant increases in their ratio of Hispanic to non-Hispanic white LDKTs from pre- to post-HKTP periods (Table 2).
In sensitivity analyses, the LDKT ratio remained significant for NM but was insignificant for all other centers when including 2007 (implementation period) data to the post-HKTP period. Further, the NM mean ratio of African American to non-Hispanic white LDKTs also did not significantly increase (pre = 0.26, post = 0.32, P = 0.23), further suggesting that the HKTP increased Hispanic LDKTs only. Sensitivity analysis using χ2 analysis found that NM observed a significant increase in Hispanic LDKT rates (P = 0.0004), whereas no other center in Table 2 observed a change in results, except that center 15 also observed a significant increase in Hispanic LDKT rates (P = 0.0003).
HKTP DDKT Rates and Ratio
At NM, the number of Hispanic DDKTs performed grew by 62.0% from 50 (pre-HKTP) to 81 (post-HKTP) (Table 4). By contrast, DDKTs in non-Hispanic whites grew by 1.5% from 263 (pre-HKTP) to 267 (post-HKTP).
TABLE 4.
Ratio of Hispanic to non-Hispanic white deceased donor kidney transplants at Northwestern Medicine
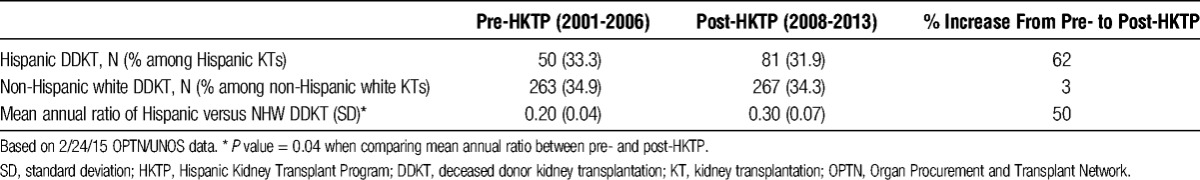
The ratio of Hispanic to non-Hispanic white DDKTs significantly increased by 43.8% after the implementation of NM's HKTP (pre-HKTP mean = 0.21; post-HKTP mean = 0.30; P = 0.04). These data suggest that the HKTP's impact on decreasing disparities between Hispanics and non-Hispanic whites also “spilled over” to also increase DDKTs among Hispanics (Table 4). Similar to LDKT, during the pre-HKTP period (2001-2006), 1 Hispanic for every 5 non-Hispanic whites received a DDKT, whereas in the post-HKTP period (2008-2013), 1 Hispanic for every 3 non-Hispanic whites received a DDKT. In sensitivity analyses, the mean post-HKTP ratio, when including 2007, of Hispanic to non-Hispanic white DDKTs also remained significant (P = 0.03).
DISCUSSION
The NM's HKTP was the only LDKT program that observed a significant increase in the ratio of Hispanic to non-Hispanic white LDKTs (70%), over and above any overall increase in LDKT, among centers in the comparison UNOS regions. Although it may be intuitive that addressing the unique needs of the Hispanic patient population would be associated with increased Hispanic LDKT rates, no study to date has demonstrated this association. This finding is compelling considering the magnitude of the Hispanic LDKT disparity. The fact that Hispanic LDKTs decreased in most regions between the pre- to post-HKTP periods, but increased at NM during the same periods, lends further support to NM's HKTP as a unique phenomenon.
We speculate that factors contributing to an increased rate of Hispanic LDKTs include increased knowledge and positive attitudes toward LKD and LDKT provided through the education sessions offered to Hispanic HKTP participants, and high satisfaction with the HKTP overall.14 By facilitating Hispanic patients' access to the transplant center through culturally competent education about transplantation and LDKT, and community outreach, the HKTP increased the pool of potential LKDs. The HKTP deliberately requests that patients invite their family members, and because Hispanics traditionally have a greater number of extended family members,40 there is a greater chance of increasing the number of potential LKDs per potential recipient.
One might posit that Spanish-speaking countries would have higher LDKT rates given the shared language and possibly awareness of cultural beliefs and values. An international comparison of Spanish-speaking countries reveals much variation in LDKT rates. Based on 2012 data, Hispanics in the United States had 15.5 LDKT per million population (pmp); Mexico had 16.8 LDKT pmp, perhaps owing to larger families.41 Yet Spain had 7.7 LDKT pmp, and Nicaragua, Panama, Paraguay, Peru, Venezuela Argentina, Colombia all had even lower LDKT rates.41 However, just because a country is Spanish-speaking does not necessarily mean that the cultural concerns held by its citizens will be addressed in transplant education. Our English-speaking transplant program does not address the cultural concerns commonly raised in the United States.
There may be alternative explanations for our findings such as: secular changes that were not accounted for in the comparison centers which might have affected the proportion of Hispanic LDKTs performed. However, the effect of the HKTP does not seem to be at the expense of other populations. Because education sessions at NM changed little between the pre-HKTP and post-HKTP periods, and DDKT waiting times were consistently disclosed over time during education sessions, waiting times were unlikely to differentially motivate patients to seek LKDs over study periods. Moreover, the English-speaking program did not experience a drop in patient visits or educational sessions/clinical evaluations comprising the first phase of patient evaluation. Attributing the increase in LDKT to culturally competent care cannot be entirely ascertained without assessing the extent to which comparison centers also implement culturally competent care. Since Organ Procurement and Transplant Network/UNOS data on Hispanic heritage (e.g., Mexican, Puerto Rican, Cuban) are considered to be incomplete, we were unable to assess how LDKTs may vary by subgroup.
Waiting list additions, as a proxy for referrals, increased significantly at NM but also nationally during post-HKTP periods, suggesting that the regional waiting list additions are unlikely to have uniquely contributed to NM's increase in Hispanic LDKT rates. The HKTP's social worker's outreach to Hispanic dialysis patients and to local healthcare providers likely increased referrals of Hispanic patients to the HKTP although it is unclear whether these referrals contributed to the HKTP’s increased Hispanic LDKT rates. Moreover, NM waiting list additions increased for Hispanics and, to a lesser degree, for whites, suggesting that the increase in Hispanic LDKTs was not at the expense of non-Hispanic whites. Even though NM experienced increases in Hispanic additions to the waiting list and in Hispanic LDKTs, when comparing across regions, increases in Hispanic additions to the waiting list do not necessarily translate to increases in Hispanic LDKTs. Thus, while increasing outreach likely helped to increase NM’s Hispanic LDKT rates, other factors (e.g., culturally competent education) likely also play a role in increasing Hispanic LDKT rates.
The HKTP appears to hold great promise as a model for enhancing access to kidney transplantation for Hispanics, thus, improving their health outcomes. Each of the comparison UNOS regions experienced significant increases in additions to the waiting list. However, none of the centers in these regions witnessed similar increases in Hispanic LDKT, suggesting that the additions to the waiting list, as a proxy for referrals, were not a contributing factor to NM’s increase in Hispanic LDKTs. It is likely that the LDKTs resulting from the HKTP occur among new patients rather than those previously on the waiting list.
As the non-Hispanic white LDKT rate remained stable over time, the increase in Hispanic LDKT rate does not appear to have limited access to LDKTs among non-Hispanic whites. Similarly, given that the number of Hispanic DDKTs also grew, the Hispanic LDKT rate also did not appear to occur at the expense of the Hispanic DDKT rate. Moreover, the NM kidney transplant program experienced the same demographic trends over the HKTP periods as did the comparison UNOS regions, suggesting that NM's demographic shifts did not account for the increased ratio of Hispanic LDKTs. The significant increase in the proportion of Hispanic LDKTs in center 15 from pre- to post-HKTP is likely due to the center being abandoned by non-Hispanics at a greater rate than by Hispanics, in contrast to NM, where the LDKT volumes increased among both Hispanics and non-Hispanics in the post-HKTP period.
The HKTP also experienced a significant increase in the ratio of Hispanic to non-Hispanic white DDKTs. The increase may be attributed to efforts by the HKTP to reevaluate Hispanic patients so that they are ready for transplantation and well-educated regarding the different types of donors to optimize the transplantation rate. Although deceased donation is unpredictable and typically requires several years of waiting, the increase in DDKTs should not be solely attributed to HKTP implementation, but may be affected by changes in national kidney allocation policy which deemphasized the HLA-B matching that led to an increase in DDKT for all ethnic minorities.42
Limitations
Because the HKTP was not prospectively designed or evaluated, limited pre-implementation data are available and a causal link between the HKTP and increased LDKT rates cannot be determined. Thus, it is unclear whether the program, specific elements of the program, or other unmeasured factors contributed to the increase in Hispanic LDKT rates. In fact, waiting list additions, used as a proxy for referrals, and patient demographics did not differ over time between patients receiving care at NM and at other transplant centers across the nation, suggesting that these factors likely did not contribute to increased LDKTs post-HKTP; it is unclear what factors contributed to the increase in waiting list additions and LDKTs in region 4. Non-Hispanic patients may also benefit from the features of the HKTP program. As UNOS forms use, but do not define the term “Hispanic,” and as different transplant programs and individuals may variably use and/or interpret the terms “Hispanic” or “Latino,” the reporting of Hispanic individuals to UNOS could be compromised.
Future research is needed to prospectively implement and evaluate the role of a HKTP on Hispanic LDKT rates, and to assess generalizability of our findings at other transplant programs. Specifically, studies should assess whether the HKTP results in transplantation at an earlier ESRD stage, thus shortening dialysis time, which is associated with decreased mortality.43 Accordingly, LDKT recipients would also be in better health at the time of transplantation, having received better quality donor organs, which translate to better posttransplant health outcomes. It remains to be determined whether the HKTP enables patients to get a LDKT sooner and thereby attenuates the onset or worsening of comorbidities associated with ESRD. Studies should also assess which specific programmatic aspects of the HKTP contribute to an increase in LDKT. Moreover, future research should evaluate whether the increase in Hispanic LDKT rates are sustained or change over time. The number of donor evaluations and the subset which do not proceed to donation should also be assessed. Cost analysis for the HKTP should assess whether the greater number of LDKTs performed as a result of the HKTP offsets the costs of program implementation.
CONCLUSIONS
These data suggest that implementation of a culturally competent intervention such as the NM HKTP may result in an increase in the rate of Hispanic LDKTs and the successful reduction in the Hispanic LDKT disparity.
Supplementary Material
ACKNOWLEDGMENTS
This research was initiated by the Informed Consent and Disparities Workgroup of the Northwestern University Transplantation Outcomes Research Collaborative (NUTORC). This work was supported in part by Health Resources and Services Administration contract 234-2005-37011C. The content is the responsibility of the authors alone and does not necessarily reflect the views or policies of the Department of Health and Human Services, nor does mention of trade names, commercial products, or organizations imply endorsement by the U.S. Government.
Footnotes
E.J.G., J.C.C., A.I.S., D.P.L., and J.L.H. participated in research conception and/or design. E.J.G., J.C.C., J.L., and R.K. participated in the writing of the article. E.J.G., J.C.C., J.L., R.K., A.I.S., D.P.L., J.L.H., M.M.A., and D.D.F. participated in a critical revision of the article for important intellectual content. E.J.G., J.C.C., J.L., R.K., A.I.S., and D.P.L. participated in analysis and interpretation of data J.L., R.K., and J.CC. participated in statistical analysis. M.M.A provided administrative, technical, or material support.
Supplemental digital content (SDC) is available for this article. Direct URL citations appear in the printed text, and links to the digital files are provided in the HTML text of this article on the journal’s Web site (www.transplantjournal.com).
This work was supported in part by Health Resources and Services Administration contract 234-2005-37011C.
The authors declare no funding or conflicts of interest.
REFERENCES
- 1. Benabe JE, Rios EV. Kidney disease in the Hispanic population: facing the growing challenge. J Natl Med Assoc. 2004; 96: 789– 798. [PMC free article] [PubMed] [Google Scholar]
- 2. Sung RS, Galloway J, Tuttle-Newhall JE, et al. Organ donation and utilization in the United States, 1997-2006. Am J Transplant. 2008; 8( 4 Pt 2): 922– 934. [DOI] [PubMed] [Google Scholar]
- 3. Lentine KL, Schnitzler MA, Xiao H, et al. Racial variation in medical outcomes among living kidney donors. N Engl J Med. 2010; 363: 724– 732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Terasaki PI, Cecka JM, Gjertson DW, et al. High survival rates of kidney transplants from spousal and living unrelated donors. N Engl J Med. 1995; 333: 333– 336. [DOI] [PubMed] [Google Scholar]
- 5.UNOS/OPTN. U.S. Transplants Performed : January 1, 1988 - December 31, 2014. Based on OPTN data as of March 6, 2015. Website accessed on March 12, 2015. URL [http://optn.transplant.hrsa.gov/converge/latestData/rptData.asp]. 2014.
- 6. Humes KR, Jones NA, Ramirez RR. Overview of Race and Hispanic Origin: 2010. 2011; http://www.census.gov/prod/cen2010/briefs/c2010br-02.pdf.
- 7. Guarnaccia PJ, Rodriguez O. Concepts of culture and their role in the development of culturally competent mental health services. Hisp J Behav Sci. 1996; 18: 419– 443. [Google Scholar]
- 8. DeVos G. Ethnic pluralism: Conflict and accommodation. In: DeVos G, Romanucci-Ross L, eds. Ethnic Identity: Creation, Conflict, and Accommodation. third ed Walnut Creek, CA: Altamira Press; 1995: 15– 47. [Google Scholar]
- 9. Gordon EJ, Feinglass J, Carney P, et al. Development of an interactive, bilingual, culturally targeted website about living kidney donation and transplantation for Hispanics. JMIR Res Protoc. 2015; 4: e42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Centers for Disease Control and Prevention. Cultural Insight – How to Communicate w/ Hispanics/Latinos [http://www.cdc.gov/healthcommunication/Audience/AudienceInsight_CulturalInsights.pdf] Accessed: 2014-09-02. (Archived by WebCite® at http://www.webcitation.org/6SIoxxenK). 2010.
- 11. Purnell TS, Hall YN, Boulware LE. Understanding and overcoming barriers to living kidney donation among racial and ethnic minorities in the United States. Adv Chronic Kidney Dis. 2012; 19: 244– 251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Alvaro EM, Siegel JF, Turcotte D, et al. Living kidney donation among Hispanics: a qualitative examination of barriers and opportunities. Prog Transplant. 2008; 18: 243– 250. [DOI] [PubMed] [Google Scholar]
- 13. Gordon EJ, Mullee JO, Ramirez D, et al. Hispanic/Latino concerns about living kidney donation: a focus group study. Prog Transplant. 2014; 24: 152– 162. [DOI] [PubMed] [Google Scholar]
- 14. Gordon EJ, Reddy E, Gil S, et al. Culturally competent transplant program improves Hispanics' knowledge and attitudes about live kidney donation and transplant. Prog Transplant. 2014; 24: 56– 68. [DOI] [PubMed] [Google Scholar]
- 15. Breitkopf CD. Attitudes, beliefs and behaviors surrounding organ donation among Hispanic women. Curr Opin Organ Transplant. 2009; 14: 191– 195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Siegel JT, Alvaro EM, Lac A, et al. Intentions of becoming a living organ donor among hispanics: a theory-based approach exploring differences between living and nonliving organ donation. J Health Commun. 2008; 13: 80– 99. [DOI] [PubMed] [Google Scholar]
- 17. Shilling LM, Norman ML, Chavin KD, et al. Healthcare professionals' perceptions of the barriers to living donor kidney transplantation among African Americans. J Natl Med Assoc. 2006; 98: 834– 840. [PMC free article] [PubMed] [Google Scholar]
- 18. Alvaro EM, Siegel JT, Crano WD, et al. A mass mediated intervention on Hispanic live kidney donation. J Health Commun. 2010; 15: 374– 387. [DOI] [PubMed] [Google Scholar]
- 19. Boulware LE, Hill-Briggs F, Kraus ES, et al. Identifying and addressing barriers to African American and non-African American families' discussions about preemptive living related kidney transplantation. Prog Transplant. 2011; 21: 97– 104 quiz 105. [DOI] [PubMed] [Google Scholar]
- 20. Joshi S, Gaynor JJ, Bayers S, et al. Disparities among Blacks, Hispanics, and Whites in time from starting dialysis to kidney transplant waitlisting. Transplantation. 2013; 95: 309– 318. [DOI] [PubMed] [Google Scholar]
- 21. U.S. Department of Health and Human Services, Office of Minority Health National Standards for Culturally and Linguistically Appropriate Services in Health Care Final Report. Washington, D.C; 2001. [Google Scholar]
- 22. Leininger M. Culture Care Diversity and Universality: A Theory of Nursing. New York: National League for Nursing; 1991. [PubMed] [Google Scholar]
- 23. Goode T, Jones W. National Center for Cultural Competence, Georgetown University Center for Child & Human Development. http://www11.georgetown.edu/research/gucchd/nccc/documents/Definition%20of%20Linguistic%20Competence.pdf [Accessed 2-18-14]. 2009.
- 24. Alvaro EM, Jones SP, Robles AS, et al. Hispanic organ donation: impact of a Spanish-language organ donation campaign. J Natl Med Assoc. 2006; 98: 28– 35. [PMC free article] [PubMed] [Google Scholar]
- 25. Rodrigue JR, Cornell DL, Kaplan B, et al. A randomized trial of a home-based educational approach to increase live donor kidney transplantation: effects in blacks and whites. Am J Kidney Dis. 2008; 51: 663– 670. [DOI] [PubMed] [Google Scholar]
- 26. Rodrigue JR, Cornell DL, Lin JK, et al. Increasing live donor kidney transplantation: a randomized controlled trial of a home-based educational intervention. Am J Transplant. 2007; 7: 394– 401. [DOI] [PubMed] [Google Scholar]
- 27. Boulware LE, Hill-Briggs F, Kraus ES, et al. Effectiveness of educational and social worker interventions to activate patients' discussion and pursuit of preemptive living donor kidney transplantation: a randomized controlled trial. Am J Kidney Dis. 2013; 61: 476– 486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Rodrigue JR, Pavlakis M, Egbuna O, et al. The "house calls" trial: a randomized controlled trial to reduce racial disparities in live donor kidney transplantation: rationale and design. Contemp Clin Trials. 2012; 33: 811– 818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Ismail SY, Luchtenburg AE, Timman R, et al. Home-based family intervention increases knowledge, communication and living donation rates: a randomized controlled trial. Am J Transplant. 2014; 14: 1862– 1869. [DOI] [PubMed] [Google Scholar]
- 30. Siegel JT, Alvaro EM, Hohman ZP, et al. “Can you spare an organ?”: exploring Hispanic Americans' willingness to discuss living organ donation with loved ones. Health Commun. 2011; 26: 754– 764. [DOI] [PubMed] [Google Scholar]
- 31. Gordon EJ, Caicedo JC, Ladner DP, et al. Transplant center provision of education and culturally and linguistically competent care: a national study. Am J Transplant. 2010; 10: 2701– 2707. [DOI] [PubMed] [Google Scholar]
- 32. Resnicow K, Baranowski T, Ahluwalia JS, et al. Cultural sensitivity in public health: defined and demystified. Ethn Dis. 1999; 9: 10– 21. [PubMed] [Google Scholar]
- 33. Galanti GA. The Hispanic family and male-female relationships: an overview. J Transcult Nurs. 2003; 14: 180– 185. [DOI] [PubMed] [Google Scholar]
- 34. National Quality Forum A Comprehensive Framework and Preferred Practices for Measuring and Reporting Cultural Competency: A Consensus Report. Washington, DC: National Quality Forum; 2009. [URL: http://www.qualityforum.org], [Publications/2009/04/A_Comprehensive_Framework_and_Preferred_Practices_for_Measuring_and_Reporting_Cultural _Competency.aspx.] Accessed December 17, 2013. 2009. [Google Scholar]
- 35. Ryan C., Language Use in the United States: 2011. American Community Survey Reports [URL: http://www.census.gov/prod/2013pubs/acs-22.pdf] Accessed April 28, 2015. U.S. Census Bureau; 2013.
- 36. Centers for Disease Control and Prevention. Cultural Insight – How to Communicate w/ Hispanics/Latinos [http://www.cdc.gov/healthcommunication/Audience/AudienceInsight_CulturalInsights.pdf] Accessed April 16, 2014. 2010.
- 37. Flores G. Culture and the patient-physician relationship: achieving cultural competency in health care. J Pediatr. 2000; 136: 14– 23. [DOI] [PubMed] [Google Scholar]
- 38. Patzer RE, Pastan SO. Measuring the disparity gap: quality improvement to eliminate health disparities in kidney transplantation. Am J Transplant. 2013; 13: 247– 248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. US Census Bureau 2010. State & County QuickFacts URL [http://quickfacts.census.gov/qfd/states/56000.html] Accessed April 17, 2014. 2010.
- 40. US Census Bureau 2010. US Census American Fact Finder: “Average Family Size" (URL: http://factfinder2.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=DEC_10_SF1_P37H&prodType=table) (Accessed 6-18-14).
- 41. International Figures on Donation and Transplantation - 2012 Council of Europe Transplant Newsletter. 2013; 18. [Google Scholar]
- 42. Roberts JP, Wolfe RA, Bragg-Gresham JL, et al. Effect of changing the priority for HLA matching on the rates and outcomes of kidney transplantation in minority groups. N Engl J Med. 2004; 350: 545– 551. [DOI] [PubMed] [Google Scholar]
- 43.U.S. Renal Data System. USRDS 2013 Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2013. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


